Abstract
Aims
Septic arthritis (SA) of the native knee joint is associated with significant morbidity. This review compared post-operative functional outcomes (patient-reported outcome measures (PROMs) and range of movement (ROM)) following arthroscopic washout (AW) and open washout (OW) amongst adult patients with SA of the native knee. The need for further operative intervention was also considered.
Methods
Electronic databases of PubMed, MEDLINE, Embase, Cochrane, Web of Science and Scopus were searched between 16 February 2023 and 18 March 2023. Randomised controlled trials (RCTs) and comparative observational analytic studies comparing function (reflected in PROMs or ROM) at latest follow-up following AW and OW were included. A narrative summary was provided concerning post-operative PROMs. Pooled estimates for mean ROM and re-operation rates were conducted using the random-effects model. The risk of bias was assessed using the Cochrane risk-of-bias assessment tool-2 for RCTs and the Risk of Bias in Non-Randomized Studies of Interventions tool for observational analytic studies.
Results
Of 2580 retrieved citations, 7 articles (1 RCT and 6 cohort studies) met the inclusion criteria. Of these, five had some concerns/moderate risk of bias, and two had serious risk. There was a slight tendency for superior mean PROMs following AW compared with OW, but due to small effect sizes, this was unlikely clinically relevant. Additionally, the use of four different PROMs scales made direct comparisons impossible. AW was associated with superior ROM (mean difference 20.18° (95% CI 14.35, 26.02; p < 0.00001)), whilst there was a tendency for lower re-operation requirements following AW (OR 0.64, 95% CI 0.26, 1.57, p = 0.44).
Conclusions
AW was associated with equivalent to superior post-operative function and lower requirement for further intervention compared with OW. Results need to be interpreted cautiously, taking into consideration the methodological and clinical heterogeneity of the included studies.
Systematic review registration
PROSPERO 2022, CRD42022364062.
Similar content being viewed by others
Introduction
Septic arthritis (SA) of the native knee joint is an orthopaedic emergency, with treatment delays potentially resulting in significant cartilage disruption, or even life-threatening sepsis [1,2,3]. The incidence is approximately 2–10 per 100,000 persons in the UK [3, 4]. Risk factors include rheumatoid arthritis, skin infections, increasing age, bacteraemia, diabetes mellitus, liver disease, immunosuppression, and joint penetration [5, 6]. In adults, typical micro-organisms include Staphylococcus aureus (S. aureus) and streptococci [3, 4, 7].
Diagnosis of SA requires consideration of clinical and laboratory features. Patients typically report knee pain, swelling, erythema, restricted range of movement, and decreased weight bearing [6]. White blood cell counts and C-reactive protein levels may be elevated, whilst joint fluid aspirate reveals a causative micro-organism in approximately 50–75% cases [3, 6]. Culture-negative SA may arise due to sampling after antimicrobial therapy, rare micro-organisms not grown on regular culture media, and other technical factors [8,9,10]. Such absence of micro-organisms may be falsely reassuring, delaying treatment, and hindering ability to target antimicrobial therapy [10].
Management of native knee SA typically involves irrigation and debridement of the joint, commonly known as a ‘washout’. This can be performed arthroscopically (‘keyhole’) or via arthrotomy (‘open’) [6]. Removal of the synovial lining of the joint, synovectomy, may be undertaken as part of an arthroscopic or open washout and is thought to maximise the reduction of the bacterial burden, although the evidence for this is limited [11]. Antimicrobial therapy typically is recommended for up to 6-week post-washout [12] but may vary according to clinical and microbiological findings.
To our knowledge, no systematic review has compared post-operative function (reflected in patient-reported outcome measures (PROMs) and range of movement (ROM)) as a primary outcome following arthroscopic washout (AW) or open arthrotomy washout (OW) of native knee SA. Additionally, the literature varies regarding requirement for subsequent intervention, a potential complication of both AW and OW. Two recent meta-analyses explored this as their primary outcome [13, 14]. Liang found that AW and OW were associated with comparable rates of reinfection (odds ratio (OR) = 0.85) [13], whilst Panjwani et al. reported a lower pooled relative risk (RR) of reoperation following AW (RR = 0.69) [14].
We hypothesised that AW would be associated with favourable post-operative PROMs and ROM, owing to smaller incisions and reduced scarring. We also hypothesised that AW would be associated with as good, or superior, rates of infection eradication, in keeping with previous meta-analyses [13, 14]. Therefore, the primary aim of this review was to compare post-operative function following AW and OW. Secondary aims were to compare rates of reoperation in the early post-operative phase (30 days) and following typical cessation of antimicrobial therapy (90 days).
Materials and methods
Data sources and study selection
This systematic review was registered with PROSPERO (CRD42022364062) and was conducted based on a predefined protocol and in accordance with Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines [15].
We searched for studies that compared functional outcomes following AW and OW as the index procedure for native knee SA in adult patients (> 18 years).
The online databases PubMed, MEDLINE, Embase, Cochrane, Web of Science, and Scopus through OvidSP were searched independently by two authors (G. K., A. T.) between 16 February 2023–18 March 2023, according to the agreed search strategies, using combined text and MeSH headings (Table 1). Databases were searched from database inception with no date range imposed on the retrieval of studies.
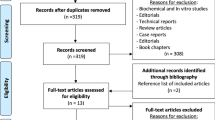
Article titles and abstracts, and then full manuscripts of potentially relevant studies, were independently reviewed by two authors (G. K., A. T.) who discussed and resolved any disagreements regarding inclusion, without needing to consult the senior authors (S. K., J. E.). The reference lists of relevant publications were also hand-searched for additional relevant studies.
Studies were included if they were interventional or comparative observational analytic studies (randomised controlled trials (RCTs), cohort studies, case–control studies) involving human subjects. We excluded narrative reviews, case reports, letters to the editor, and studies describing prosthetic joint infections or noninfectious arthritis.
Data extraction
One author (G. K.) used a standardised form to extract data. A second reviewer (A. T.) independently checked these data against those in original articles.
Data were extracted on the following: geographical location, publication year, study design, level of evidence [16], participants (age, sex), sample size, duration of follow-up, risk factors, microbiological findings, post-operative PROMs and ROM, re-operation requirements, and synovectomy at index procedure.
In publications where data were inadequate, we contacted the authors to request the information needed. Where no response was obtained, the study was excluded from analysis.
Outcomes
The primary outcomes were post-operative PROMs and ROM (at latest follow-up) following AW and OW. The secondary outcomes were rates of reoperation for persistent or recurrent infection within 30 and 90 days of index procedure. We also aimed to present an overview of microbiological findings, risk factors, and whether synovectomy was undertaken during the index procedure.
Assessment of risk of bias and evidence quality
The risk of bias was independently assessed by two authors (G. K., A. T.) who discussed and resolved any disagreements. The Cochrane risk-of-bias assessment tool-2 (RoB2) [17] was used for RCTs and the Risk of Bias in Non-Randomized Studies of Interventions (ROBINS-I) tool [18] for observational studies.
The Grading of Recommendations Assessment, Development and Evaluation (GRADE) criteria were used to assess the quality of the evidence for each outcome [19].
Data synthesis and analysis
A narrative summary was provided concerning PROMs, microbiological features, risk factors, and undertaking of synovectomy. Regarding ROM and reoperation, summary measures were presented as mean differences and odds ratios (OR) with 95% confidence intervals (95% CI). The random-effects model was used to obtain pooled estimates for each outcome, to account for interstudy heterogeneity and provide a more conservative evaluation of the significance of the association [20]. The extent of interstudy heterogeneity was assessed with the I2 statistic [21], with values of 30–60% representing moderate heterogeneity [22].
Statistical analysis was conducted using Review Manager (RevMan Web), version 5.4, the Cochrane Collaboration 2020, available at revman.cochrane.org.
Results
Article selection
In total, 2580 potentially relevant citations were identified, 2573 of which were subsequently excluded (Fig. 1). Seven eligible studies were included.
Study characteristics
Table 2 outlines characteristics of the seven studies (one RCT, six cohort studies) reporting functional outcomes after AW and OW. In total, 394 patients (243 arthroscopic, 151 open) were included.
Key microbiological findings are outlined in Table 3. Staphylococcus aureus was the most common micro-organism (96, 24.4%), whilst over 15% were culture negative (66, 16.5%). Where described, antimicrobial regimes were typically administered for a total of 4–6 weeks [23,24,25,26,27, 29]. No risk factors were present in at least 24.4% of patients (Table 3).
Regarding disease severity, of the three studies [24, 26, 29] reporting Gächter stage [30], there was a tendency for patients with earlier changes (stages I/II) to be managed arthroscopically and more advanced changes (III/IV) to be managed with OW.
Assessment of risk of bias
Moderate risk of bias was present in five studies and serious risk in two studies (Table 4). Bias in participant selection was mostly considered moderate because there may have been an association between the interventions and outcomes (patients with more severe symptoms were more likely to undergo OW). Bias relating to measurement of interventions, outcomes, and departures from intended interventions was judged low because the intervention and outcomes were objective and insusceptible.
Patient-reported outcome measures
Four studies reported on post-operative PROMs using four different scales (Table 5). Due to heterogeneity of constructs measured, study design, and one study describing categorical results, PROMs were not pooled and synthesised quantitatively using standardised mean difference [31]. Overall, there was weak evidence of a slightly favourable effect of AW on PROMs. However, the small mean differences were likely not clinically significant, and overlapping confidence intervals would suggest no real difference in effect estimates.
Range of movement
Four cohort studies described ROM at latest follow-up (Table 6). The mean difference in ROM was 20.18° (95% CI 14.35, 26.02; p < 0.00001), favouring AW (Fig. 2). No significant heterogeneity was observed (I2 = 14%). Findings by Kalem et al. [27] were excluded from this meta-analysis, as necessary information regarding the interquartile range was neither reported nor provided when requested from the corresponding author.
On age-adjusted subgroup analysis, Böhler et al. [25] found the difference in mean ROM between AW and OW groups persisted (p = 0.008).
Secondary outcomes
Table 7 details the requirements for re-operation and whether synovectomy was performed during the index procedure. Re-operation was necessary in 31.7% (77/243) of patients following AW and 33.8% (51/151) of patients following OW. Practice regarding synovectomy varied. Owing to inconsistency in reporting, we were unable to look for association between synovectomy and re-operation requirements.
As the timeframe from index to second procedure was often not specified, we were unable to report 30- and 90-day re-operation rates. The second procedure typically paralleled the index; 53 AW patients (68.5%) underwent further AW, and 33 OW patients (64.7%) underwent further OW. The nature of subsequent procedure(s) was not specified for 21 patients.
Additionally, it was often not reported whether single or multiple repeat procedures were necessary. Johns et al. [26] reported that fewer irrigation procedures were required following AW (1.79 ± 0.96) than following OW (2.42 ± 1.5) (p = 0.010).
Meta-analysis of the six cohort studies suggested a tendency for lower re-operation requirement following AW (OR 0.64, 95% CI 0.26–1.57, p = 0.44) (Fig. 3). Moderate interstudy heterogeneity was observed (I2 = 52%). Data from Peres et al. [23] were not included in this model owing to the difference in study design; however, the authors reported no difference in effectiveness of treatment.
After age adjustment, Böhler [25] found the difference in re-operation requirements between groups persisted (p = 0.008). Similarly, Johns [26] found that the superiority of AW persisted after adjustment for age, sex, comorbidity, and positive joint culture (OR 2.56, 95% CI 1.1, 5.9; p = 0.027).
Quality of evidence
The summary of the GRADE assessment [19] for each outcome is outlined in Table 8. The evidence certainty ranged from moderate to very low for all outcomes assessed in this systematic review. This was mostly because of starting with a low rating because the data were mostly from observational studies, and the certainty of the evidence was further downgraded for risk of bias or inconsistency.
Publication bias
We were unable to undertake Egger’s test for publication bias, as Egger’s test has insufficient power to distinguish chance from real funnel plot asymmetry with fewer than 10 studies [36].
Discussion
Septic arthritis of the native knee can be joint- and life-threatening; thus, prompt, effective management is paramount. Our findings suggest that AW has a tendency for favourable functional outcomes and re-operation rates compared with OW. However, the evidence is uncertain due to moderate-serious risk of bias and inter-study heterogeneity.
Comparison with other studies
The present study represents the first systematic review focusing primarily on function following AW and OW. Our findings agree with PROMs and ROM described in reviews by Panjwani [14] and Liang [13], respectively. This was predictable, as we retrieved just one additional study reporting PROMs [28], and none further reporting ROM. Findings by Kalem [27], which did not show a difference regarding ROM, were not included in the meta-analysis because information required for pooling of the data was not provided.
Our findings suggested that AW may be associated with lower re-operation rates, given the direction and magnitude of the risk estimate (OR 0.64). However, the confidence intervals were imprecise suggesting heterogeneity, so the results should be interpreted cautiously. In keeping with our findings, Liang [13] showed a possible trend for lower rates of reinfection following AW (OR = 0.85; p = 0.44), whilst Panjwani [14] reported substantially reduced risk of reoperation (RR = 0.69; p = 0.0006). Both these reviews included additional studies in their pooled analyses which were excluded from the present study due to omission of PROMs [37,38,39,40,41]. Additionally, Panjwani [14] combined effect estimates from randomised and non-randomised studies, which is generally inappropriate [42].
Explanation of findings
It could be suggested that the less-invasive AW is associated with superior post-operative function, owing to smaller surgical incisions and shorter post-operative recovery. The reported difference in mean ROM (20.18°) is likely highly clinically significant; whilst not previously studied in the septic arthritis setting, in the setting of stroke, the minimum clinically important difference (MCID) was under 10° [43]. However, given the observational nature of six of the included studies, there is the risk of confounding. We noted that patients with higher Gächter-stage disease [24, 25, 29], mean preoperative temperature [23], and more risk factors for SA development [26] were selected for OW. Such preference for OW in higher Gächter-stage disease has been described elsewhere [44]. Thus, poorer functional outcomes might be expected.
Requirement for reoperation may be confounded by patient factors, including Gächter stage, pyrexia at presentation, body mass index > 45 kg/m2, elevated inflammatory markers, and immunosuppression [5, 44,45,46]. Of the included studies, only Böhler [25] and Johns [26] adjusted for confounders. Similarly, re-operation requirement may be influenced by intervention factors, including time from presentation to index and subsequent procedures, total number of procedures, and individual surgeons’ thresholds for synovectomy and reoperation. Due to inconsistent reporting, we were unable to stratify or adjust for these factors which may have affected outcomes in the pooled analysis; thus, one should interpret these results with caution.
It is also possible that the observed associations may have arisen due to underpowering, as no prior sample size calculation was undertaken. Post hoc analysis suggested adequate power in the RCT [23] and two cohort studies [25, 26]; however, this may not be the case for the remaining studies.
Implications of findings
We suggest that AW is acceptable to patients and efficacious in the treatment of native knee SA and thus should be routinely used in the management of this condition. We have presented strong evidence in favour of AW regarding ROM and weak evidence regarding PROMs.
As AW was associated with a tendency for reduced re-operation requirement, this may decrease healthcare costs, and we suggest further investigation is warranted. We note, however, that none of the studies utilised a generic health-related quality-of-life assessment tool, which has been recommended to be used in combination with condition-specific scales to facilitate economic assessment [47].
Additionally, the use of four different PROMs scales has rendered direct comparison between studies impossible, and with the data provided, it was not possible to calculate standardised mean difference. Of the scales used, only the BBFS has been described in SA of the native knee [33], and the MCID has been established in the SA context for none of the scales. Such use of unvalidated tools may render results less reliable, and differences observed may not be clinically relevant. Furthermore, it is possible that the scales used do not actually reflect what is pertinent to the patient population; to our knowledge, this has not been explored qualitatively. Additionally, we have considered PROMs and ROM at latest follow-up. As average follow-up duration varied, and it was often unclear when measurements were obtained, these functional results may not be directly comparable.
Strengths and limitations
A robust search of multiple databases and rigorous approach to study selection was employed. This ensured that all available relevant citations were identified and outcomes extracted. However, owing to the lack of high-quality studies, the findings should be interpreted with caution. Limitations of the six cohort studies include their retrospective nature, typically small sample sizes, and no blinding of outcome assessors, whilst the small, single-centre nature of the RCT may limit the external validity of their findings. Furthermore, owing to the small number of studies included, we were unable to test for publication bias.
As SA represents an increasing clinical concern, a definitive RCT is warranted. In contrast to the RCT by Peres [23], this should be multicentre and with prior sample size calculation, in order to improve external validity and ensure sufficient power to capture the outcomes of interest. Subgroup analysis may also wish to consider the appropriateness for AW or OW by disease severity, association between disease severity and functional outcomes, and the role of synovectomy at initial washout. Despite RCTs being the gold standard for clinical research, their use in assessing the effectiveness of orthopaedic interventions has limitations. They are labour intensive, expensive, and need large sample sizes. Real-world evidence, such as nesting analysis within arthroplasty registries, may represent better investigative avenues.
Conclusion
Based on the available evidence, we conclude that AW results in favourable post-operative ROM, similar PROMs, and a tendency for lower re-operation rates compared with OW. Thus, AW is acceptable for use in the treatment of native knee SA. However, as OW tended to be used in those with more severe disease, there may be confounding by indication. Therefore, there is no evidence to suggest that OW should not be used, for example, should arthroscopic treatment be unavailable.
Despite SA being a growing area of clinical concern, higher-quality evidence is lacking. Clinical and methodological heterogeneity of the included studies limits one’s ability to make meaningful comparisons. This systematic review highlights the need for more definitive large clinical trials, with a particular focus on patient-reported and functional outcomes.
References
Mathews CJ, Weston VC, et al. Bacterial septic arthritis in adults. The Lancet. 2010;375(9717):846–55.
Perry CR. Septic arthritis. Am J Orthop (Belle Mead NJ). 1999;28(3):168–78.
Weston VC, Jones AC, et al. Clinical features and outcome of septic arthritis in a single UK Health District 1982–1991. Ann Rheum Dis. 1999;58(4):214–9.
Rutherford AI, Subesinghe S, et al. A population study of the reported incidence of native joint septic arthritis in the United Kingdom between 1998 and 2013. Rheumatology. 2016;55(12):2176–80.
Lu V, Zhou A, et al. Risk factors for septic arthritis and multiple arthroscopic washouts: minimum 2-year follow-up at a major trauma centre. Clin Rheumatol. 2022;41(8):2513–23.
Elsissy JG, Liu JN, et al. Bacterial septic arthritis of the adult native knee joint: a review. JBJS Rev. 2020;8(1):e0059.
Long B, Koyfman A, Gottlieb M. Evaluation and management of septic arthritis and its mimics in the emergency department. West J Emerg Med. 2019;20(2):331–41.
Hindle P, Davidson E, Biant LC. Septic arthritis of the knee: the use and effect of antibiotics prior to diagnostic aspiration. The Annals of The Royal College of Surgeons of England. 2012;94(5):351–5.
Yoon HK, Cho SH, et al. A review of the literature on culture-negative periprosthetic joint infection: epidemiology, diagnosis and treatment. Knee Surg Relat Res. 2017;29(3):155–64.
Goh GS, Parvizi J. Diagnosis and treatment of culture-negative periprosthetic joint infection. J Arthroplasty. 2022;37(8):1488–93.
Lui TH. Complete arthroscopic synovectomy in management of recalcitrant septic arthritis of the knee joint. Arthrosc Tech. 2017;6:e467–75.
Earwood JS, Walker TR, Sue GJC. Septic arthritis: diagnosis and treatment. Am Fam Physician. 2021;104(6):589–97.
Liang Z, Deng X, Li L, Wang J. Similar efficacy of arthroscopy and arthrotomy in infection eradication in the treatment of septic knee: a systematic review and meta-analysis. Front Surg. 2022;8:801911.
Panjwani T, Wong KL, et al. Arthroscopic debridement has lower re-operation rates than arthrotomy in the treatment of acute septic arthritis of the knee: a meta-analysis. Journal of ISAKOS. 2019;4:307–12.
Moher D, Liberati A, et al. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA statement. BMJ. 2009;339:b2535.
Wright JG, Swiontkowski MF, Heckman JD. Introducing levels of evidence to the journal. J Bone Joint Surg Am. 2003;85(1):1–3.
Sterne JAC, Savović J, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366:l4898.
Sterne JA, Hernán MA, et al. ROBINS-I: a tool for assessing risk of bias in non-randomised studies of interventions. BMJ. 2016;355:i4919.
Guyatt G, Oxman AD, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Fleiss JL. The statistical basis of meta-analysis. Stat Methods Med Res. 1993;2(2):121–45.
Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539–58.
Higgins JPT, Chandler J,. Chapter 10: Analysing data and undertaking meta-analyses. Cochrane Handbook for Systematic Reviews of Interventions version 6.3 (updated February 2022) 2022 [Online] Available from: www.training.cochrane.org/handbook. Accessed 5th May 2023
Peres LR, Marchitto RO, et al. Arthrotomy versus arthroscopy in the treatment of septic arthritis of the knee in adults: a randomized clinical trial. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3155–62.
Balabaud L, Gaudias J, et al. Results of treatment of septic knee arthritis: a retrospective series of 40 cases. Knee Surg Sports Traumatol Arthrosc. 2007;15(4):387–92.
Böhler C, Dragana M, et al. Treatment of septic arthritis of the knee: a comparison between arthroscopy and arthrotomy. Knee Surg Sports Traumatol Arthrosc. 2016;24(10):3147–54.
Johns BP, Loewenthal MR, Dewar DC. Open compared with arthroscopic treatment of acute septic arthritis of the native knee. J Bone Joint Surg Am. 2017;99(6):499–505.
Kalem M, şahin E. Comparison of three surgical treatment methods in acute septic arthritis of the knee in adults. Flora Infeksiyon Hastalıkları ve Klinik Mikrobiyoloji Dergisi. 2018;23:1-9.
Sabater-Martos M, Garcia Oltra E, et al. Arthrotomic debridement of arthrotic septic arthritis of the knee is more effective than arthroscopic debridement and delays the need for prosthesis despite progression. Revista Española de Cirugía Ortopédica y Traumatología (English Edition). 2021;65(1):3–8.
Wirtz DC, Marth M, et al. Septic arthritis of the knee in adults: treatment by arthroscopy or arthrotomy. Int Orthop. 2001;25(4):239–41.
Gächter A. Arthroskopische Spülung zur Behandlung infizierter Gelenke. Oper Orthop Traumatol. 1989;1(3):196–9.
Zeng L, Yao L, et al. Presentation approaches for enhancing interpretability of patient-reported outcomes in meta-analyses: a systematic survey of Cochrane reviews. J Clin Epidemiol. 2023;158:119–26.
Tegner Y, Lysholm J. Rating systems in the evaluation of knee ligament injuries. Clin Orthop Relat Res. 1985;198:43–9.
Bussière F, Beaufils P. Role of arthroscopy in the treatment of pyogenic arthritis of the knee in adults Report of 16 cases. Rev Chir Orthop Reparatrice Appar Mot. 1999;85(8):803–10.
Bellamy N, Buchanan WW, et al. Validation study of WOMAC: a health status instrument for measuring clinically important patient relevant outcomes to antirheumatic drug therapy in patients with osteoarthritis of the hip or knee. J Rheumatol. 1988;15(12):1833–40.
Larson KR, Cracchiolo A 3rd, Dorey FJ, Finerman GA. Total knee arthroplasty in patients after patellectomy. Clin Orthop Relat Res. 1991;264:243–54.
Sterne JA, Sutton AJ, et al. Recommendations for examining and interpreting funnel plot asymmetry in meta-analyses of randomised controlled trials. BMJ. 2011;343:d4002.
Dave OH, Patel KA, et al. Surgical procedures needed to eradicate infection in knee septic arthritis. Orthopedics. 2016;39(1):50–4.
Jaffe D, Costales T, et al. Methicillin-resistant Staphylococcus aureus infection is a risk factor for unplanned return to the operating room in the surgical treatment of a septic knee. J Knee Surg. 2017;30(9):872–8.
Bovonratwet P, Nelson SJ, et al. Similar 30-day complications for septic knee arthritis treated with arthrotomy or arthroscopy: an American College of Surgeons National Surgical Quality Improvement Program Analysis. Arthroscopy. 2018;34(1):213–9.
Faour M, Sultan AA, et al. Arthroscopic irrigation and debridement is associated with favourable short-term outcomes vs. open management: an ACS-NSQIP database analysis. Knee Surg Sports Traumatol Arthrosc. 2019;27(10):3304–10.
Johnson DJ, Butler BA, et al. Arthroscopy versus arthrotomy for the treatment of septic knee arthritis. J Orthop. 2020;19:46–9.
Sarri G, Patorno E, et al. Framework for the synthesis of non-randomised studies and randomised controlled trials: a guidance on conducting a systematic review and meta-analysis for healthcare decision making. BMJ Evidence-Based Medicine. 2022;27(2):109–19.
Guzik A, Drużbicki M, et al. Estimating minimal clinically important differences for knee range of motion after stroke. J Clin Med. 2020;9(10):3305.
Straub J, Lingitz M-T, et al. Early postoperative laboratory parameters are predictive of initial treatment failure in acute septic arthritis of the knee and shoulder joint. Sci Rep. 2023;13(1):8192.
Radhamony NG, Walkay S, et al. Predictors of failure after initial arthroscopic washout in septic arthritis of native knee joint- a retrospective analysis. Annals of Medicine and Surgery. 2022;74:103269.
Aïm F, Delambre J, et al. Efficacy of arthroscopic treatment for resolving infection in septic arthritis of native joints. Orthop Traumatol Surg Res. 2015;101(1):61–4.
Al Sayah F, Jin X, Johnson JA. Selection of patient-reported outcome measures (PROMs) for use in health systems. J Patient Rep Outcomes. 2021;5(Suppl 2):99.
Author information
Authors and Affiliations
Contributions
GK undertook the PROSPERO registration, literature search, data extraction, quality grading, results collation, manuscript preparation. AT served as second reviewer in manuscript retrieval, data extraction and quality grading, and assisted in results collation and manuscript preparation. JRAP assisted in proof-reading and manuscript preparation. JTE oversaw the project and assisted in data presentation and manuscript preparation. SKK oversaw the project and assisted in PROSPERO registration, meta-analysis, data presentation and manuscript preparation.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kennedy, G.E.M., Tharmaseelan, A., Phillips, J.R.A. et al. Does arthroscopic or open washout in native knee septic arthritis result in superior post-operative function? A systematic review and meta-analysis of randomised controlled trials and observational studies. Syst Rev 13, 106 (2024). https://doi.org/10.1186/s13643-024-02508-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-024-02508-1