Abstract
Background
Distal gastrectomy (DG) is a commonly used surgical procedure for gastric cancer (GC), with three reconstruction methods available: Billroth I, Billroth II, and Roux-en-Y. In 2018, our team published a systematic review to provide guidance for clinical practice on the optimal reconstruction method after DG for GC. However, since then, new evidence from several randomized controlled trials (RCTs) has emerged, prompting us to conduct an updated systematic review and network meta-analysis to provide the latest comparative estimates of the efficacy and safety of the three reconstruction methods after DG for GC.
Method
This systematic review and network meta-analysis update followed the PRISMA-P guidelines and will include a search of PubMed, Embase, and the Cochrane Library for RCTs comparing the outcomes of Billroth I, Billroth II, or Roux-en-Y reconstruction after DG for patients with GC. Two independent reviewers will screen the titles and abstracts based on predefined eligibility criteria, and two reviewers will assess the full texts of relevant studies. The Bayesian network meta-analysis will evaluate various outcomes, including quality of life after surgery, anastomotic leakage within 30 days after surgery, operation time, intraoperative blood loss, major postoperative complications within 30 days after surgery, incidence and severity of bile reflux, and loss of body weight from baseline.
Ethics and dissemination
The review does not require ethical approval. The findings of the review will be disseminated through publication in an academic journal, presentations at conferences, and various media outlets.
INPLASY registration number
INPLASY2021100060.
Similar content being viewed by others
Introduction
Description of the condition
Gastric cancer (GC) is a significant cause of cancer-related mortality, accounting for 5.6% of all cancer cases and 7.7% of cancer-related deaths worldwide, with a mortality number of 768,793 in 2020 [1]. Although multidisciplinary gastric cancer care has improved survival rates through chemotherapy, radiotherapy, and molecular targeted therapy [2], radical surgical resection remains the only definitive therapeutic treatment for individuals with localized GC [3, 4]. For most GC in the lower two-thirds of the stomach, distal gastrectomy (DG) is the recommended surgery. However, the choice of reconstruction method after DG is still controversial, with various methods introduced since Billroth conducted the first subtotal gastrectomy in 1881 [5]. Billroth I (B-I), Billroth II (B-II), and Roux-en-Y (R-Y) are all valid reconstruction methods [6].
Description of the intervention
B-I and B-II reconstructions are widely used in Asia due to their procedural simplicity [7], but they also have complications. For instance, Billroth I reconstruction may increase anastomotic tension and the incidence of fistula, despite having physiological advantages [8]. Billroth II reconstruction avoids anastomotic tension to some extent, but it cannot be applied to all patients because it may lead to postoperative alkaline reflux gastritis, dumping syndrome, esophagitis, and anastomotic ulcers [9,10,11]. R-Y reconstruction prevents alkaline reflux gastritis and reflux esophagitis, and reduces anastomotic tension [12]. Despite these advantages, patients who have undergone R-Y reconstruction often experience Roux stasis syndrome [13,14,15]. Therefore, finding an appropriate digestive tract reconstruction method to reduce postoperative complications and improve quality of life is crucial.
Why it is important to do this review
Our team conducted a Bayesian network meta-analysis to investigate the comparative evidence of B-I, B-II, and R-Y reconstruction for patients with GC after DG, combining direct and indirect comparisons [16]. In 2019, two additional meta-analyses also investigated this question [17, 18]. However, they included observational studies as well as randomized controlled trials (RCTs), potentially leading to bias. Furthermore, Min et al. conducted a meta-analysis on this topic in 2022 but only searched the PubMed database [19]. Relevant publications may have been missed as a result. Moreover, these studies [17,18,19] did not evaluate the confidence in the findings from network meta-analyses. As several RCTs have been published in recent years, potentially providing clinical efficacy evidence for the three reconstruction methods after DG for GC, we plan to conduct a systematic review and network meta-analysis update to expand our previous work [16] and provide more robust clinical evidence. In this updated review, we will adjust primary outcomes of interest to include quality of life after surgery and major postoperative complications within 30 days after surgery. Additionally, we will update the literature search as well as include a broader range of study types and adjust the effect sizes.
Method
This review will update a previously published systematic review and meta-analysis by our team.
Protocol and registration
This protocol is written in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis Protocols (PRISMA-P) (Supplementary file 1) [20]. Any amendments to this protocol will be recorded in an updated version of the INPLASY registration. The updated work will be conducted in accordance with the PRISMA guidelines and the standard methodology recommended by the Cochrane Collaboration [21, 22].
Inclusion criteria
Types of participants
We will include studies with patients who had histologically proven gastric cancer located in the distal stomach and without evidence of distant metastasis.
Types of studies
We will include randomized controlled trials (RCTs) and quasi-experimental studies, wherein the method for allocating participants to different interventions was not strictly random (e.g., by date of birth, day of the week, month of the year, medical record number, or order of inclusion in the study). Sensitivity analyses will be conducted, excluding quasi-randomized trials, to assess the robustness of the results. The studies considered for inclusion will have been published before February 1st, 2024.
Types of interventions
We will include RCTs that compare two or more of the following reconstruction methods after DG for GC: B-I, B-II, or R-Y reconstruction.
Types of outcome measures
The primary outcomes will be as follows:
-
1)
Quality of life after surgery (measured by validated questionnaires) (at least six months).
-
2)
Major postoperative complications within 30 days after surgery (grade III to V according to Clavien‐Dindo Classification) [23].
The secondary outcomes will be as follows:
-
1)
Operation time
-
2)
Hospital stays
-
3)
Incidence of anastomotic leakage within 30 days after surgery.
-
4)
Incidence and severity of bile reflux according to endoscopic examination or according to the criteria of the original studies (at least 6 months).
-
5)
Loss of body weight (kg) from baseline (at least 6 months).
Exclusion criteria
-
1)
Studies with overlapping data.
-
2)
Full-text articles are not available after exhaustive searches to locate the texts.
Information sources and search strategy
One reviewer will perform a systematic literature search in PubMed, Ovid Embase, and the Cochrane Central Register of Controlled Trials databases for eligible studies from their inception. Medical subject headings terms (Mesh) combined with text words and synonyms will be performed in our search course. In addition, the manual search and reference search will be performed to enlarge the search range. The reference list of relevant publications will also be hand-searched to identify additional potential studies. A sample PubMed search strategy is described in detail in online Supplementary file 2. In PubMed search strategy, we combined the subject-specific strategy with the sensitivity and precision-maximizing version of the Cochrane highly sensitive search strategy for identifying randomized trials, 2008 revision [21].
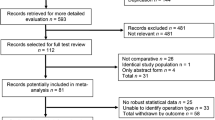
Study selection and data extraction
Two reviewers will independently screen titles and abstracts to exclude obvious irrelevant reports, using the reference management software Endnote X20. They will then independently examine the full text of all potentially eligible articles. Disagreements will be resolved through a team discussion. We will record the excluding reasons and generate a PRISMA flow diagram for the network meta-analysis [24].
Two reviewers will extract data independently using a standardized data collection form. The following data will be extracted from the included studies: the first author, publication year, country, study design, participant characteristics, inclusion/exclusion criteria, intervention details, and outcome data. If multiple studies are conducted on the same subjects, only the study with the highest methodological quality, the most complete results, or the most recent published date will be included [25]. The authors of the trials will be contacted to provide missing data if needed. Disagreements will be resolved through a team discussion.
Dealing with missing data
For missing data, we will attempt to obtain more information from the original authors. In the absence of a reply, we will try to calculate the data through the available coefficients according to the Cochrane Handbook for Systematic Reviews [21]. For continuous outcomes, SDs will be estimated by stand errors, p values, or CIs, depending on how the original research is provided. Otherwise, SDs will be evaluated based on the median or IQR. The potential impact of these missing data will be assessed by sensitivity analysis. We will not exclude the studies with insufficient data, we will describe these studies in the supplementary and explain the reasons why they will not be included in meta-analysis.
Risk of bias assessment
Two reviewers will independently assess the quality and risk of bias of the included studies by using the Cochrane Risk of Bias Tool (RoB I) in the following domains [26]: random sequence generation, allocation concealment, blinding of participants and personnel, missing outcome data, selective outcome reporting, and other bias. The risk of bias in each domain, as well as the overall risk of bias, will be rated as ‘low risk’, ‘high risk’, or ‘unclear’. Disagreements will be resolved through a team discussion. When inadequate information is available from the studies to rate a risk of bias item, we will contact the corresponding authors for additional information.
Data analysis
(1) Geometry of the network
We will use Hiplot (available at hiplot-academic.com) to draw network plots to describe and present the geometry of types of interventions including B-I, B-II, and R-Y reconstruction for patients with GC after DG for each outcome. Each node will be a treatment. An edge will connect two nodes when at least one trial compares the two corresponding treatments. The size of the nodes will be proportional to the number of patients, while the weight of each edge will be proportional to the number of studies per treatment comparison.
(2) Assessment of transitivity
We will use a narrative summary to describe the characteristics of each included study. To assess transitivity, we will compare the distributions of baseline participant characteristics across studies and treatments to confirm that they are parallel among different comparisons. If differences are found, then these will be addressed in subgroup and sensitivity analyses.
(3) Network meta-analysis
We will apply all NMAs using a Bayesian Markov chain Monte Carlo framework and fitted in R [27] using the gemtc [28], and rjags [29] package. For NMAs, we will report the estimated weighted mean differences (WMDs) for continuous outcomes, whereas the estimated risk ratios (RRs) for dichotomous outcomes, as well as the 95% credible interval (95% CrI). This is in preference to the odds ratio (OR) since ORs (when interpreted as RR) can markedly exaggerate the effect size when event rates are high [30,31,32]. To rank the efficacy for each intervention, we will calculate the ranking probabilities for all treatments, the surface under the cumulative ranking curve (SUCRA) [33].
(4) Heterogeneity assessment
When multiple trials are available for comparison, heterogeneity within each pair-wise comparison will be assessed using the Cochran Q test with I2 statistic [34]. We will interpret the I2 statistic according to the guidelines in the Cochrane Handbook [30, 35] as follows: 0 to 40% might not be important; 30 to 60% may represent moderate heterogeneity; 50 to 90% may represent substantial heterogeneity; 75 to 100% represents considerable heterogeneity. The Chi2 test will be interpreted where a P value less than or equal to 0.10 will indicate evidence of statistical heterogeneity. For network meta‐analysis, we will assess statistical heterogeneity in the entire network by considering the magnitude of the between‐study variance parameter (Tau2) derived from the network meta‐analysis models. We will compare the magnitude of the heterogeneity variance with empirical distribution for dichotomous outcomes, as proposed by Turner 2012 [36]. Both pairwise meta-analysis and network meta-analysis (NMA) will be conducted using random-effects models [34].
(5) Assessment of inconsistency
We will use the node-splitting method, which involves splitting mixed evidence into direct and indirect evidence in each node for comparison, to assess inconsistency [37]. If a discrepancy is not found, this network meta-analysis can be considered to fit the consistency model. Otherwise, when a significant difference between direct and indirect evidence occurs, an inconsistency model will be utilized, and potential reasons for inconsistency will be discussed [38].
Meta-biases and confidence in the findings from network meta-analysis
To assess small-study effects, we will visually explore the comparison-adjusted funnel plot for each outcome when at least 10 studies are available. The confidence in the findings from network meta-analysis will be evaluated based on the latest version of the Confidence In Network Meta-Analysis (CINeMA) web tool [39, 40] (available at cinema.ispm.unibe.ch). CINeMA is based on a methodological framework that considers six domains: within-study bias, reporting bias, indirectness, imprecision, heterogeneity, and incoherence [39].
Discussion
This updated systematic review and network meta-analysis aims to comprehensively evaluate the latest evidence regarding the optimal reconstruction method for patients with GC after DG. Our analysis will consider various clinical outcomes such as quality of life after surgery and major postoperative complications within 30 days. Additionally, we will provide recommendations for future research directions in this area and highlight the clinical implications of our findings for informing treatment decisions.
Availability of data and materials
Not applicable.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2021;71(3):209–49.
Johnston FM, Beckman M. Updates on management of gastric cancer. Curr Oncol Rep. 2019;21(8):67.
Cai Z, Yin Y, Shen C, Wang J, Yin X, Chen Z, et al. Comparative effectiveness of preoperative, postoperative and perioperative treatments for resectable gastric cancer: a network meta-analysis of the literature from the past 20 years. Surg Oncol. 2018;27(3):563–74.
Smyth EC, Nilsson M, Grabsch HI, van Grieken NC, Lordick F. Gastric cancer. Lancet. 2020;396(10251):635–48.
Hu Y, Zaydfudim VM. Quality of life after curative resection for gastric cancer: survey metrics and implications of surgical technique. J Surg Res. 2020;251:168–79.
Hirao M, Takiguchi S, Imamura H, Yamamoto K, Kurokawa Y, Fujita J, et al. Comparison of Billroth I and Roux-en-Y reconstruction after distal gastrectomy for gastric cancer: one-year postoperative effects assessed by a multi-institutional RCT. Ann Surg Oncol. 2013;20(5):1591–7.
Nunobe S, Sasako M, Saka M, Fukagawa T, Katai H, Sano T. Symptom evaluation of long-term postoperative outcomes after pylorus-preserving gastrectomy for early gastric cancer. Gastric Cancer. 2007;10(3):167–72.
Hoya Y, Mitsumori N, Yanaga K. The advantages and disadvantages of a Roux-en-Y reconstruction after a distal gastrectomy for gastric cancer. Surg Today. 2009;39(8):647.
Choi CI, Baek DH, Lee SH, Hwang SH, Kim DH, Kim KH, et al. Comparison between Billroth-II with Braun and Roux-en-Y reconstruction after laparoscopic distal gastrectomy. J Gastrointest Surg. 2016;20(6):1083–90.
Shim JH, Oh SI, Yoo HM, Jeon HM, Park CH, Song KY. Roux-en-Y gastrojejunostomy after totally laparoscopic distal gastrectomy: comparison with Billorth II reconstruction. Surg Laparosc Endosc Percutan Tech. 2014;24(5):448–51.
Shirbeigi L, Halavati N, Leila A, Aliasl J. Dietary and medicinal herbal recommendation for management of primary bile reflux gastritis in traditional Persian medicine. Iran J Public Health. 2015;44(8):1166–8.
Nishizaki D, Ganeko R, Hoshino N, Hida K, Obama K, Furukawa TA, et al. Roux-en-Y versus Billroth-I reconstruction after distal gastrectomy for gastric cancer. Cochrane Database Syst Rev. 2021;9(9):CD012998.
Mon RA, Cullen JJ. Standard Roux-en-Y gastrojejunostomy vs. “uncut” Roux-en-Y gastrojejunostomy: a matched cohort study. J Gastrointest Surg. 2000;4(3):298–303.
Xiong J-J, Altaf K, Javed MA, Nunes QM, Huang W, Mai G, et al. Roux-en-Y versus Billroth I reconstruction after distal gastrectomy for gastric cancer: a meta-analysis. World J Gastroenterol: WJG. 2013;19(7):1124.
Zong L, Chen P. Billroth I vs. Billroth II vs. Roux-en-Y following distal gastrectomy: a meta-analysis based on 15 studies. Hepatogastroenterology. 2011;58(109):1413–24.
Cai Z, Zhou Y, Wang C, Yin Y, Yin Y, Shen C, et al. Optimal reconstruction methods after distal gastrectomy for gastric cancer: a systematic review and network meta-analysis. Medicine (Baltimore). 2018;97(20):e10823.
Liu XF, Gao ZM, Wang RY, Wang PL, Li K, Gao S. Comparison of Billroth I, Billroth II, and Roux-en-Y reconstructions after distal gastrectomy according to functional recovery: a meta-analysis. Eur Rev Med Pharmacol Sci. 2019;23(17):7532–42.
Ma Y, Li F, Zhou X, Wang B, Lu S, Wang W, et al. Four reconstruction methods after laparoscopic distal gastrectomy: a systematic review and network meta-analysis. Medicine (Baltimore). 2019;98(51):e18381.
Min JS, Kim RB, Seo KW, Jeong SH. Comparison of the clinical outcomes of reconstruction methods after distal gastrectomy: a systematic review and meta-analysis based on randomized controlled trials. J Gastric Cancer. 2022;22(2):83–93.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349.
Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA, editors. Cochrane Handbook for Systematic Reviews of Interventions. 2nd ed. Chichester: John Wiley & Sons; 2019.
Hutton B, Salanti G, Caldwell DM, Chaimani A, Schmid CH, Cameron C, et al. The PRISMA extension statement for reporting of systematic reviews incorporating network meta-analyses of health care interventions: checklist and explanations. Ann Intern Med. 2015;162(11):777–84.
Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009;250(2):187–96.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Duchaine CS, Aubé K, Gilbert-Ouimet M, Gralle APBP, Vezina M, Ndjaboue R, et al. Effect of psychosocial work factors on the risk of depression: a protocol of a systematic review and meta-analysis of prospective studies. BMJ Open. 2019;9(11):e033093.
Higgins JP, Sterne JA, Savovic J, Page MJ, Hróbjartsson A, Boutron I, et al. A revised tool for assessing risk of bias in randomized trials. Cochrane Database Syst Rev. 2016;10(Suppl 1):29–31.
Team RC. R: A language and environment for statistical computing. MSOR connections. 2014. p. 1.
van Valkenhoef G, Lu G, de Brock B, Hillege H, Ades AE, Welton NJ. Automating network meta-analysis. Res Synth Methods. 2012;3(4):285–99.
Plummer M. rjags: Bayesian graphical models using MCMC. R package v. 4–8. 2018.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10(10):Ed000142.
Balasubramanian H, Ananthan A, Rao S, Patole S. Odds ratio vs risk ratio in randomized controlled trials. Postgrad Med. 2015;127(4):359–67.
Rombach I, Knight R, Peckham N, Stokes JR, Cook JA. Current practice in analysing and reporting binary outcome data-a review of randomised controlled trial reports. BMC Med. 2020;18(1):147.
Salanti G, Ades A, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Cai Z, Liu C, Chang C, Shen C, Yin Y, Yin X, et al. Comparative safety and tolerability of approved PARP inhibitors in cancer: a systematic review and network meta-analysis. Pharmacol Res. 2021;172:105808.
Lewis SR, Macey R, Stokes J, Cook JA, Eardley WG, Griffin XL. Surgical interventions for treating intracapsular hip fractures in older adults: a network meta-analysis. Cochrane Database Syst Rev. 2022;2(2):Cd013404.
Turner RM, Davey J, Clarke MJ, Thompson SG, Higgins JP. Predicting the extent of heterogeneity in meta-analysis, using empirical data from the Cochrane Database of Systematic Reviews. Int J Epidemiol. 2012;41(3):818–27.
Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7–8):932–44.
Higgins JP, Jackson D, Barrett JK, Lu G, Ades AE, White IR. Consistency and inconsistency in network meta-analysis: concepts and models for multi-arm studies. Res Synth Methods. 2012;3(2):98–110.
Nikolakopoulou A, Higgins JPT, Papakonstantinou T, Chaimani A, Del Giovane C, Egger M, et al. CINeMA: An approach for assessing confidence in the results of a network meta-analysis. PLoS Med. 2020;17(4):e1003082.
Papakonstantinou T, Nikolakopoulou A, Higgins JPT, Egger M, Salanti G. CINeMA: Software for semiautomated assessment of the confidence in the results of network meta-analysis. Campbell Syst Rev. 2020;16(1):e1080.
Acknowledgements
None.
Patient and public involvement statement
Patient and Public Involvement Statement is not applicable because the essence of meta-analysis is the reanalysis of published data.
Funding
None.
Author information
Authors and Affiliations
Contributions
Bo Zhang, Jing Liao, and Zhaolun Cai conceived the original idea of this research. Zhou Zhao, Chaoyong Shen, Hancong Li, and Xiangcheng Pan designed the protocol and drafted the manuscript. Hancong Li, Mingchun Mu, Zhaolun Cai, and Xiangcheng Pan participated in developing the eligibility criteria, search strategy, data extraction methods, and data summary plan. Bo Zhang and Jing Liao reviewed the manuscript. All authors approved the last version of this manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Ethical approval is not required for this protocol since the study will be conducted using the previously published studies. The reporting of this protocol did not involve individual patients and public agencies.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Supplementary 1.
PRISMA-P 2015 checklistR1.
Additional file 2: Supplementary 2.
PubMed search strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhao, Z., Li, H., Pan, X. et al. Optimal reconstruction methods after distal gastrectomy for gastric cancer: a protocol for a systematic review and network meta-analysis update. Syst Rev 13, 19 (2024). https://doi.org/10.1186/s13643-023-02445-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02445-5