Abstract
Background
The widely accepted prevalence of traditional medicine (TM) in Ethiopia was about 80 %, of which 95 % were sourced from plants. The purpose of this study was to update knowledge of the prevalence of herbal medicine or TM in Ethiopia and describe the characteristics of the population mostly relying on herbal medicine or TM to inform health policy-makers.
Methods
PubMed, Google Scholar, Hinari, Scopus, and the Directory of Open Access Journals (DOAJ) were searched. The methodological quality of each included study was assessed using the quality assessment checklist for prevalence studies. Meta-analysis was conducted using STATA version 17, and the heterogeneity between studies was assessed using I2 test statistics based on the random effect model. Forest and funnel plots were used to present the data. Subgroup analysis was done by the study population, region, and setting.
Results
Thirty-six studies with a total of 16,288 participants met the inclusion criteria. Meta-analysis of the study revealed that the prevalence of herbal medicine use in Ethiopia is 46 % (95 % CI, 37–54 %), with significant heterogeneity among the studies (I2 = 99.19 %). Egger’s test for publication bias of herbal medicine use revealed significant results (Egger, P = 0.002) which indicates possible missing of small sample size studies. The prevalence of TM use in Ethiopia is 65 % (95 % CI, 52–77 %) with significant heterogeneity among the studies (I2 = 99.18 %). Egger’s test for publication bias of TM use revealed non-significant results (Egger, P = 0.275). The subgroup analysis by the study setting and the region revealed variability amongst the studies. Community-based studies and Oromia National Regional State showed higher prevalence. By population type, a higher prevalence of TM use was observed amongst children and lowest amongst malaria suspects.
Conclusions
The current study revealed that TM/herbal medicine utilization remained an important source of primary healthcare in Ethiopia. In comparison to the commonly reported prevalence of TM/herbal medicine, there is a considerable decline in TM/herbal medicine prevalence. High TM/herbal medicine use tendency during pregnancy necessitates safety studies to optimize the utilization.
Similar content being viewed by others
Background
The World Health Organization (WHO) defines traditional medicine (TM) as “the sum total of the knowledge, skill, and practices based on the theories, beliefs, and experiences indigenous to different cultures, whether explicable or not, used in the maintenance of health as well as in the prevention, diagnosis, improvement or treatment of physical and mental illness” [1]. For a number of reasons, TM is highly valued and widely used around the world. The TM/herbal medicines with strong scientific evidence on their safety profiles, sufficient efficacy, and quality contribute to the goal of ensuring that all people have access to standard health care. This made TM/herbal medicines highly valued assets [1, 2].
Herbal medicine according to WHO is a practice which includes herbs, herbal materials, herbal preparations, and finished herbal products, that contain active ingredients parts of plants, or other plant materials, or combinations [3]. It encompasses the combination of practices of indigenous systems of medicine and several therapeutic experiences of many previous generations [4]. Main plant parts used in herbal medicine include leaves, stems, flowers, roots, and seeds [5]. Herbal medicines are asserted to cure diabetes, jaundice, hypertension, tuberculosis, mental disorders, Acquired Immunodeficiency Syndrome (AIDS), cancer, skin diseases, and many other infectious diseases [4].
The use of medicinal plants as a fundamental component of the African traditional healthcare system is the oldest with a long track record and is widely acknowledged among all therapeutic systems. In many parts of rural Africa, traditional healers prescribing medicinal plants are the most easily accessible and affordable health resource available to the local community and at times the only treatment modality that exists [6]. The TM in Africa is holistic involving both the body and the mind and traditional healers offer information, counseling, and treatment to patients and their families in a personal manner [6]. Patients’ preference, the low ratio of medical doctors to the total population, and the lack of effective modern medical treatment for some ailments in Africa are additional factors for the wider practice of traditional medicines.
According to the WHO, 70–80 % of Africans today depend either totally or partially on TM [1]. Traditional medicine is widely practiced in Ethiopia. It is used to treat diverse forms of human diseases including cancer, hypertension, diabetes, bacterial infections, parasitic infections, and many more [7,8,9,10,11]. Over 80 % of the Ethiopian population also relies on TM according to a report as old as 1986 [12], and more than 95% of the preparations are made from plant origin [13]. This represents the majority of the rural population and sectors of the urban population where there is little or no access to modern health care [14].
The recent study in 2016 by the WHO’s Study on Global Ageing and Adult Health (SAGE) revealed that the widely accepted notion that 80 % of Africans and Asians rely on TM stands no more [15]. For instance, it was <3 % in Ghana and <2 % in South Africa, which is much less than what previous reports claimed [15]. The present systematic review and meta-analysis aimed to update knowledge of the prevalence of TM/herbal medicine in Ethiopia. In addition, it aims to point out the characteristics of the population mostly relying on TM/herbal medicine to inform health policy-makers to harness its potential contribution to health, wellness, and people-centered healthcare and promote safe and effective use through the regulation of products, practices, and practitioners as indicated in the WHO TM strategy 2014–2023 [1].
Materials and methods
Search strategy
Published and unpublished research papers (e.g., MSc/PhD thesis) reporting the prevalence of TM/herbal medicine in different settings: during pregnancy, for infants (children), for adults, in urban settings, and in rural settings even involving health professionals at the institution or community level were included. The search domains included Google Scholar, local university repositories—for unpublished research, international abstracting, and indexing databases such as SCOPUS, PubMed, Hinari, ScienceDirect, Web of Science, EBSCO, and Directory of Open Access Journals (DOAJ).
In designing the search strategy, participants, intervention, comparator, and outcome (PICO) were used. The participants of this study were the Ethiopian population. The intervention is TM including herbal medicine. Since this is the prevalence comparator, the outcome was not used in designing the search term.
The key terms/phrases used for searching were Ethiopia, plants, medicinal plants, traditional medicine, traditional knowledge, herbs, indigenous knowledge, folk medicine, ethnobotany, ethnopharmacology, ethnomedicine, medico-cultural, prevalence, proportion, and use rate. Based on the information above, the following search terms were applied in different databases. (1) Traditional medicine OR medicinal plant* OR herb* OR indigenous knowledge OR traditional knowledge OR folk medicine OR folk remedies OR home remedies OR ethnobotan* OR ethnopharmacolog* OR ethnomedicin* ethnopharmaceutic* OR medico-cultural; (2) Prevalence OR proportion OR Use rate; and (3) Ethiopia*. The search maps used in PubMed were as follows: ((traditional medicine OR medicinal plant* OR herb* OR indigenous knowledge OR traditional knowledge OR folk medicine OR folk remedies OR home remedies OR ethnobotan* OR ethnopharmacolog* OR ethnomedicin* ethnopharmaceutic* OR medico-cultural) AND (prevalence OR proportion OR use rate)) AND (Ethiopia*).
First, the titles and abstracts were screened and then suitable articles were downloaded and examined against the inclusion criteria. Published and unpublished ethnobotanical and ethnomedicinal surveys reporting the prevalence or proportion of the population using herbal medicine or TM in Ethiopia were included. Review articles, historical documents, experimental studies, data lacking information on study areas, prevalence of use, and not reporting information about traditional medicinal plants were excluded.
Risk of bias assessment
The methodological quality of each included study was assessed using the quality assessment tool for prevalence studies developed by Leboueuf-Yde and Lauritsen and then modified by Hoy and colleagues [16, 17]. Graphs of the summary of the risk of bias were developed using RevMan 5.3 (Cochrane Informatics and Knowledge Management Department, London, UK).
Data extraction
Data were extracted using a Microsoft Excel spreadsheet. The characteristics of extracted data in each study include first author name, year of publication, area of study (region), study setting (community or institution-based), number of study participants, response rate, characteristics of study participants (population type), age of study participants, frequency of herbal medicine use, frequency of TM use, and most frequently used herbal medicine.
Data analysis
Statistical analyses were conducted using STATA version 17.0 (StataCorp, LP, College Station, TX). The prevalence was pooled using the MetaProp command in STATA. The heterogeneity of the studies was assessed using the I2 statistic, and significance was declared at I2 > 50 %. Because of significant heterogeneity among the studies, the random-effects model (REM) was used to estimate the pooled prevalence and 95 % CI using the DerSimonian and Laird methods. The Freeman-Turkey double arcsine transformation was used to avoid missing prevalence near or at 0 and 1 from the meta-analysis. Subgroup analysis was done by region, study setting, and population type. The presence of publication bias was tested using Egger’s test. Forest and funnel plots were constructed to display the individual studies and pooled results. The data were computed by Cochrane Collaboration’s software, RevMan 5.3.
Results
Characteristics of included studies
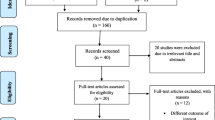
Database and other relevant source searching resulted in 790 articles of which 36 met the inclusion criteria, enrolling a total of 16,288 participants. The included studies published were for 20 years from 2002 to 2022 (Fig. 1).
Of these studies, 16 were from the Amhara National Regional State; nine from Oromia National Regional State; three from Addis Ababa City Administration; three from Harari Peoples’ National Regional State; two from South Nations, Nationalities and Peoples Regional State; and one each from Southwest Ethiopia National Regional State, Benshangul-Gumuz National Regional State and in health centers from Addis Ababa and Bati, North Central Ethiopia. Twenty of the studies were conducted at institutions such as hospitals and health centers, and the remaining 16 studies were community-based studies. Twelve studies were conducted on pregnant women; nine in the general population, four in parents with children, three among HIV/AIDS patients, two among diabetic patients, two among hypertensive patients, and one each in HIV/AIDS and TB co-infected patients, cancer patients, malaria suspected patients, and among older adults. The general characteristics of included studies; regions where the studies were conducted, population type, the study setting, sample size, response rate, age groups, prevalence of herbal medicine, and TM use; and most frequently used herbal medicines were depicted in Table 1.
Quality assessment of the included studies
A low risk of bias was observed in all of the included studies in terms of the source of data collection as all of them were directly collected from the participants. In terms of non-response bias, acceptable case definition, and instrument used, almost all studies have shown a low risk of bias. About half of the included studies have shown a high risk of bias in terms of representing the national population, sampling frame, and random sampling technique. The risk of bias assessment summary and the graph are presented in Fig. 2A and B.
Prevalence of herbal medicine use in Ethiopia
Meta-analysis of the study revealed that the prevalence of herbal medicine use in Ethiopia is 46 % (95 % CI, 37–54 %), and there was significant heterogeneity among the studies, I2=99.19 % (Fig. 3). Egger’s test for publication bias revealed significant result (Egger, P= 0.002) which indicates possible missing of small sample size studies.
The studies included were significantly heterogeneous as the statistical test revealed; visual inspection of the funnel also revealed the scatted distribution of the prevalence values (Fig. 4).
Subgroup analysis of the study by region revealed that there is heterogeneity among studies as indicated in Table 2. The mixed (Addis Ababa and Bati) showed a higher prevalence of herbal medicine use compared to all other regions while Addis Ababa showed the lowest prevalence. Community-based studies showed a higher prevalence of herbal medicine use compared to institutional-based studies. More studies were conducted among pregnant women, higher prevalence of use of herbal medicine was observed amongst cancer patients and lowest among malaria suspects.
The trends analysis revealed that most of the studies (91.7 %) were conducted between 2014 and 2022. The heterogeneity was visible regardless of the year of the study (Fig. 5).
Prevalence of traditional medicine use in Ethiopia
Meta-analysis of the study revealed that the prevalence of TM use in Ethiopia is 65 % (95 % CI, 52–77 %). There was significant heterogeneity among the studies, I2=99.18% (Fig. 6). Egger’s test for publication bias revealed non-significant results (Egger, P=0.275).
The studies included were significantly heterogeneous as it was for the prevalence of herbal medicine use; visual inspection of the funnel also reveals a scatted distribution of the prevalence values (Fig. 7).
Subgroup analysis of TM use by region revealed that there is variability among studies as indicated in Table 3. Community-based studies showed a higher prevalence of TM use compared to institutional-based studies though non-significant. The Oromia National Regional State showed a higher prevalence of TM use compared to all other regions while Southwest Ethiopia showed the lowest use prevalence. A higher prevalence of TM was observed among children and lowest among malaria suspects.
Trends in traditional medicine use in Ethiopia
Trends analysis revealed that most of the studies were conducted between 2016 and 2022. Heterogeneity is visible regardless of the year of study (Fig. 8).
Discussion
The present finding revealed that the prevalence of 65 % (95 CI %, 52–77 %) TM and that of the herbal medicine prevalence of 46 % (95 CI %, 38–56 %) are much less than the previously established prevalence. The long-standing value that 80 % of Ethiopians rely on TM and of which 95 % is sourced from herbal medicine is far from the present truth. Traditional medicine is an integral part of healthcare as an alternative healthcare delivery system especially in low- and middle-income countries encompassing Latin America, Africa, and Asia [1, 54, 55]. In Ethiopia, according to the official population projection of the Central Statistical Agency (CSA) 2019, 79.77 % of the Ethiopian population lives in rural parts of the country [56]. The rural area is characterized by poor infrastructural settings with scarce or no modern facilities to provide primary healthcare. The TM is sometimes the only accessible and affordable alternative primary healthcare among such rural communities [1]. African TM/herbal medicine is used for various human ailments such as cancer, hypertension, HIV, and use during pregnancy follows similar trends to that of Ethiopian TM/herbalism [57,58,59,60].
Among the herbal medicines reported in the present study, there are ubiquitously used herbs as foods or dyes by the general population in daily lives. For instance, Zingiber officinale (Ginger), Ruta chalepensis (Tena Adam), Allium sativa (Garlic), Ocimum lamiifolium (Damakase), Thymus vulgaris (Tosign), Lepidium sativum (Feto), Trigonella foenum-graecum L. (Absh (fenugreek), and Linum usitatissimum (telba (Flax seeds)) are among the reported herbal medicines and further contributed to the increase in the prevalence [61, 62]. These are common dietary supplements/spices and are also commonly used herbs for medicinal purposes.
The trend analysis of the studies revealed that the majority of the studies with proportions of herbal medicine use were conducted between 2014 and 2022, the last 8 years (Table 4). This finding further signifies that the old figures of TM/herbal medicine prevalence needed updating and hence the present finding can be referred to as the current prevalence of TM/herbal medicine in Ethiopia.
The present finding that a lower socio-economic status, unemployment, and rural residence where access to modern health facilities is scarce were associated with high TM/herbal medicine use is in agreement with other reports [63, 64]. The WHO’s study on Global Ageing and Adult Health (SAGE) also determined that the TM prevalence in six populous middle-income countries such as China, Ghana, India, Mexico, Russia, and South Africa is much lower than has previously been reported and those who do make use of TM are more likely to be socio-economically disadvantaged corroborates the present finding [15].
The most regularly cited reasons for TM/herbal medicine use in the present finding disclosed are closeness to residency, cultural acceptability, trust by the general population, ease of access, affordability, and dissatisfaction with modern medicine also supported by other reports elsewhere [15, 63,64,65]. In some high-income countries, the TM usage is reported to be high. For instance, Australia (48 %), Canada (70 %), France (75 %), the UK (51.8 %), and the USA (42%) of the population use TM [66,67,68]. In those countries, unlike the low- and middle-income countries, the reason for high TM usage is due to the assumption that TMs are safer than allopathic medicines [69].
The most frequently cited TM other than herbal medicine included bone setting, use of the spiritual water (“tsebel”), prayer (faith healing), massage, cauterization, traditional birth attendance, and tooth extraction. This finding is in agreement with reports from other African countries [70].
In our report, most of the TM/herbal medicines were used to treat health conditions experienced during pregnancy, malaria, TB, HIV/AIDS, hypertension, cancer, and the like. Among the users, pregnant women are commonly practicing. As pregnant mothers are more likely to risk groups for potential toxicity derived from herbal remedies which eventually affect the fetus, creating awareness of general use and potential risks of herbal remedies need to be addressed through the health policy system [18].
The current study is highly heterogeneous as observed from I2. The source of this heterogeneity could be from the methodological quality, geographic and cultural variations, smallness of the included studies, intrinsic variability in the population, and formal synthesis of comparable data. Moreover, eligible studies included in the current study were from some of the administrative regions in Ethiopia and thus may not comprehensively represent the national TM or herbal medicine use. Therefore, to determine the prevalence of TM or herbal medicine at the national level, the large-scale prospective study which represents all administrative regions and city councils should be considered.
In this study, we have collected, compared, and interrogated the dataset of herbal and TM prevalence using systematic reviews and meta-analysis of currently available evidence. Although the studies included may not be from all over Ethiopia, all published TM or herbal medicine prevalence reporting studies from Ethiopia were thoroughly analyzed. Significant heterogeneity observed may be a reflection of the poor methodological quality of included studies and geographical and cultural variations. In addition, all of the included studies were conducted in small particular localities and non-representative convenient sampling techniques were also employed. Therefore, the limitations of the current study arose inherently from the characteristics of the included studies.
Conclusion
In conclusion, the study revealed that TM/herbal medicine utilization remained an integral source of primary healthcare in Ethiopia. In comparison to the commonly reported prevalence of TM/herbal medicine, there is a considerable decline in TM/herbal medicine prevalence. This might be due to improved access to modern healthcare facilities which could be related to rapid urbanization, slight improvements in rural infrastructures, and public awareness of allopathic medicine. The vast majority who still rely on TM/herbal medicine basically is due to a lack of access to these allopathic medicines with affordable prices. Therefore improving the livelihood of the majority poor and making modern medicines easily accessible with low or affordable prices is highly recommended. The high tendency of TM/herbal medicine use during pregnancy is a finding that is of concern. This calls for urgent regulatory measures from the government and needs to be supported by robust scientific studies for the safety of both the mother and the fetus.
Availability of data and materials
All data generated or analyzed are included in the manuscript.
Abbreviations
- CAM:
-
Complementary and Alternative Medicine
- CI:
-
Confidence Interval
- HIV/AIDS:
-
Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome
- TM:
-
Traditional Medicine
- SNNPR:
-
Southern Nations, Nationalities and Peoples Region
- WHO:
-
World Health Organization
References
WHO. WHO traditional medicine strategy: 2014-2023. Geneva: World Health Organization; 2013.
Yuan H, Ma Q, Ye L, Piao G. The traditional medicine and modern medicine from natural products. Molecules. 2016;21(5):559. https://doi.org/10.3390/molecules21050559.
WHO. General guidelines for methodologies on research and evaluation of traditional medicine. World Health Organization; Geneva; 2000.
Khan MSA, Ahmad I, Chattopadhyay D. New look to phytomedicine: advancements in herbal products as novel drug leads: Academic Press. 2019. https://doi.org/10.1016/C2017-0-01165-5.
Bent S. Herbal medicine in the United States: review of efficacy, safety, and regulation: grand rounds at University of California, San Francisco Medical Center. J Gen Int Med. 2008;23:854–9. https://doi.org/10.1007/s11606-008-0632-y.
Tabuti JR, Hassen IE, Pateh UU, Mahomoodally MF. Recent advances towards validating efficacy and safety of African traditional medicines. Evid Based Complement Alternat Med. 2014;260567:2. https://doi.org/10.1155/2014/260567.
Getachew S, Medhin G, Asres A, Abebe G, Ameni G. Traditional medicinal plants used in the treatment of tuberculosis in Ethiopia: a systematic review. Heliyon. 2022;8(5):e09478. https://doi.org/10.1016/j.heliyon.2022.e09478.
Tuasha N, Petros B, Asfaw Z. Plants used as anticancer agents in the Ethiopian traditional medical practices: a systematic review. Evid Based Complement Alternat Med. 2018;6274021:28. https://doi.org/10.1155/2018/6274021.
Teka A, Maryo M. Ethiopian medicinal plants used for respiratory tract disorders: ethnomedicinal review. Evid Based Complement Alternat Med. 2023;7612804. https://doi.org/10.1155/2023/7612804.
Asnake S, Teklehaymanot T, Hymete A, Erko B, Giday M. Survey of medicinal plants used to treat malaria by Sidama people of Boricha District, Sidama Zone, South Region of Ethiopia. Evid Based Complement Alternat Med. 2016. https://doi.org/10.1155/2016/9690164:9690164.
Birhan W, Giday M, Teklehaymanot T. The contribution of traditional healers’ clinics to public health care system in Addis Ababa, Ethiopia: a cross-sectional study. J Ethnobiol Ethnomed. 2011;7(1):39. https://doi.org/10.1186/1746-4269-7-39.
Abebe D. Traditional medicine in Ethiopia: the attempts being made to promote it for effective and better utilization. SINET Eth J Sci. 1986;9:61–9.
Kefalew A, Asfaw Z, Kelbessa E. Ethnobotany of medicinal plants in Ada’a District, East Shewa Zone of Oromia regional state Ethiopia. J Ethnobiol Ethnomed. 2015;11:25. https://doi.org/10.1186/s13002-015-0014-6.
Bishaw M. Promoting traditional medicine in Ethiopia: a brief historical review of government policy. Soc Sci Med. 1991;33(2):193–200. https://doi.org/10.1016/0277-9536(91)90180-k.
Oyebode O, Kandala N-B, Chilton PJ, Lilford RJ. Use of traditional medicine in middle-income countries: a WHO-SAGE study. Health Policy Plan. 2016;31(8):984–91. https://doi.org/10.1093/heapol/czw022.
Leboeuf-Yde C, Lauritsen JM. The prevalence of low back pain in the literature. Spine. 1995;20(19):2112–8.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, Baker P, Smith E, Buchbinder R. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65(9):934–9. https://doi.org/10.1016/j.jclinepi.2011.11.014.
Abeje G, Admasie C, Wasie B. Factors associated with self medication practice among pregnant mothers attending antenatal care at governmental health centers in Bahir Dar city administration, Northwest Ethiopia, a cross sectional study. Pan Afr Med J. 2015; 20:276. https://doi.org/10.11604/pamj.2015.20.276.4243.
Addis GT, Workneh BD, Kahissay MH. Herbal medicines use and associated factors among pregnant women in Debre Tabor town, north West Ethiopia: a mixed method approach. BMC Complemen Med Ther. 2021;21(1):268. https://doi.org/10.1186/s12906-021-03439-3.
Ahmed SM, Sundby J, Aragaw YA, Abebe F. Self-Medication and safety profile of medicines used among pregnant women in a tertiary teaching hospital in Jimma, Ethiopia: a cross-sectional study. Int J Environ Res Public Health. 2020;17(11):3993. https://doi.org/10.3390/ijerph17113993.
Ahmed SM, Sundby J, Aragaw YA, Nordeng H. Medicinal plants used among pregnant women in a tertiary teaching hospital in Jimma, Ethiopia: a cross-sectional study. BMJ Open. 2021;11(8):e046495. https://doi.org/10.1136/bmjopen-2020-046495.
Asrat D, Alle A, Kebede B, Dessie B. Factors associated with parental traditional medicine use for children in Fagita Lekoma Woreda Northwest Ethiopia: a cross-sectional study. SAGE Open Med. 2020;8:2050312120978008. https://doi.org/10.1177/2050312120978008.
Ayele AA, Tegegn HG, Haile KT, Belachew SA, Mersha AG, Erku DA. Complementary and alternative medicine use among elderly patients living with chronic diseases in a teaching hospital in Ethiopia. Complement Ther Med. 2017;35:115–9. https://doi.org/10.1016/j.ctim.2017.10.006.
Bantie GM, Meseret Z, Bedimo M, Bitew A. The prevalence and root causes of delay in seeking healthcare among mothers of under five children with pneumonia in hospitals of Bahir Dar city, North West Ethiopia. BMC Pediatrics. 2019;19(1):482. https://doi.org/10.1186/s12887-019-1869-9.
Bayisa B, Tatiparthi R, Mulisa E. Use of herbal medicine among pregnant women on antenatal care at Nekemte Hospital, Western Ethiopia. Jundishapur J Nat Pharm Prod. 2014;9(4):e17368. https://doi.org/10.17795/jjnpp-17368.
Emiru YK, Adamu BA, Erara M, Chanie T, Gurmu AE. Complementary and alternative medicine use in a pregnant population, Northwest Ethiopia. Int J Reprod Med. 2021; 8829313. https://doi.org/10.1155/2021/8829313.
Erku DA, Basazn Mekuria A. Prevalence and correlates of complementary and alternative medicine use among hypertensive patients in Gondar town, Ethiopia. Evid Based Complement Alternat Med. 2016; 6987636. https://doi.org/10.1155/2016/6987636.
Erku DA. Complementary and alternative medicine use and its association with quality of life among cancer patients receiving chemotherapy in Ethiopia: a cross-sectional study. Evid Based Complement Alternat Med. 2016;2809875. https://doi.org/10.1155/2016/2809875.
Feyissa M, Gedif Fenta T, Asres K, Gebremariam T. Prevalence, perception and predictors of concomitant herbal medicine use among HIV/AIDS and tuberculosis patients in metekel zone, Northwest Ethiopia: a cross-sectional study. Evid Based Complement Alternat Med. 2022; 8235229. https://doi.org/10.1155/2022/8235229.
Gedif T, Hahn HJ. Epidemiology of herbal drugs use in Addis Ababa Ethiopia. Pharmacoepidemiol Drug Saf. 2002;11(7):587–91. https://doi.org/10.1002/pds.729.
Gedif T, Hahn H-J. The use of medicinal plants in self-care in rural central Ethiopia. J Ethnopharmacol. 2003;87(2–3):155–61. https://doi.org/10.1016/s0378-8741(03)00109-0.
Endale Gurmu A, Teni FS, Tadesse WT. Pattern of traditional medicine utilization among HIV/AIDS patients on antiretroviral therapy at a university hospital in northwestern Ethiopia: a cross-sectional study. Evid Based Complement Alternat Med. 2017; 1724581. https://doi.org/10.1155/2017/1724581.
Haile KT, Ayele AA, Mekuria AB, Demeke CA, Gebresillassie BM, Erku DA. Traditional herbal medicine use among people living with HIV/AIDS in Gondar, Ethiopia: do their health care providers know? Complement Ther Med. 2017;35:14–9. https://doi.org/10.1016/j.ctim.2017.08.019.
Shiferaw A, Baye AM, Amogne W, Feyissa M. Herbal medicine use and determinant factors among HIV/AIDS patients on antiretroviral therapy in Tikur Anbessa specialized hospital, Addis Ababa, Ethiopia. HIV AIDS (Auckl). 2020;12:941. https://doi.org/10.2147/HIV.S283810.
Tizazu D, Workineh Y, Ayalew Y. Parental traditional medicine use for children and associated factors in North Mecha district, North West Ethiopia. Pediatric Health Med Ther. 2020;11:505. https://doi.org/10.2147/PHMT.S275249.
Tesfaye M, Solomon N, Getachew D, Biru YB. Prevalence of harmful traditional practices during pregnancy and associated factors in Southwest Ethiopia: a community-based cross-sectional study. BMJ Open. 2022;12(11):e063328. https://doi.org/10.1136/bmjopen-2022-063328.
Nigussie S, Godana A, Birhanu A, Abdeta T, Demeke F, Lami M, Gemechu K, Eyeberu A, Bogale K, Dechasa DB. Practice of traditional medicine and associated factors among residents in Eastern Ethiopia: a community-based cross-sectional study. Front Public Health. 2022;10:915722. https://doi.org/10.3389/fpubh.2022.915722.
Nega SS, Bekele HM, Meles GG, Nordeng H. Medicinal plants and concomitant use with pharmaceutical drugs among pregnant women. J Altern Complement Med. 2019;25(4):427–34. https://doi.org/10.1089/acm.2018.0062.
Mekuria AB, Erku DA, Gebresillassie BM, Birru EM, Tizazu B, Ahmedin A. Prevalence and associated factors of herbal medicine use among pregnant women on antenatal care follow-up at University of Gondar referral and teaching hospital, Ethiopia: a cross-sectional study. BMC Complement Altern Med. 2017;17(1):86. https://doi.org/10.1186/s12906-017-1608-4.
Mekuria AB, Belachew SA, Tegegn HG, Ali DS, Netere AK, Lemlemu E, Erku DA. Prevalence and correlates of herbal medicine use among type 2 diabetic patients in Teaching Hospital in Ethiopia: a cross-sectional study. BMC Complement Altern Med. 2018;18(1):85. https://doi.org/10.1186/s12906-018-2147-3.
Jambo A, Mengistu G, Sisay M, Amare F, Edessa D. Self-medication and contributing factors among pregnant women attending antenatal care at public hospitals of Harar town Ethiopia. Front Pharmacol. 2018;9:1063. https://doi.org/10.3389/fphar.2018.01063.
Kebede B, Gedif T, Getachew A. Assessment of drug use among pregnant women in Addis Ababa Ethiopia. Pharmacoepidemiol Drug Saf. 2009;18(6):462–8. https://doi.org/10.1002/pds.1732.
Kifle ZD, Yimenu DK, Kidanu BB. Complementary and alternative medicine use and its associated factors among hypertensive patients in Debre Tabor General Hospital Ethiopia. Metabol Open. 2021;12:100132. https://doi.org/10.1016/j.metop.2021.100132.
Kifle ZD, Bayleyegn B, Tadesse TY, Woldeyohanins AE. Prevalence and associated factors of herbal medicine use among adult diabetes mellitus patients at government hospital, Ethiopia: an institutional-based cross-sectional study. Metabol Open. 2021;11:100120. https://doi.org/10.1016/j.metop.2021.100120.
Kovalev V, Wells ML. Self-treatment practices for perceived symptoms of malaria in Ethiopia. Cureus. 2020;12(7):e9359. https://doi.org/10.7759/cureus.9359.
Laelago T, Yohannes T, Lemango F. Prevalence of herbal medicine use and associated factors among pregnant women attending antenatal care at public health facilities in Hossana Town, Southern Ethiopia: facility based cross sectional study. Arch Public Health. 2016;74(1):7. https://doi.org/10.1186/s13690-016-0118-z.
Hailu F, Cherie A, Gebreyohannis T, Hailu R. Determinants of traditional medicine utilization for children: a parental level study in Tole District, Oromia, Ethiopia. BMC Complement Med Ther. 2020;20(1):125. https://doi.org/10.1186/s12906-020-02928-1.
Aragaw TJ, Afework DT, Getahun KA. Assessment of knowledge, attitude, and utilization of traditional medicine among the communities of Debre Tabor Town, Amhara Regional State, North Central Ethiopia: a cross-sectional study. Evid Based Complement Altern Med. 2020;6565131. https://doi.org/10.1155/2020/6565131.
Belachew N, Tadesse T, and Gube AA. Knowledge, attitude, and practice of complementary and alternative medicine among residents of Wayu town, Western Ethiopia. J Evid Based Complementary Altern Med. 2017;22(4):929–35. https://doi.org/10.1177/2515690X17746547.
Bussa NF, Gemeda AS. Assessment of traditional medicine utilization in Harar town, eastern Ethiopia. J Ayu Herb Med. 2018;4(4):158–64.
Chali BU, Hasho A, Koricha NB. Preference and practice of traditional medicine and associated factors in Jimma Town, Southwest Ethiopia. Evid Based Complement Altern Med. 2021;9962892. https://doi.org/10.1155/2021/9962892.
Gari A, Yarlagadda R, Wolde-Mariam M. Knowledge, attitude, practice, and management of traditional medicine among people of Burka Jato Kebele, West Ethiopia. J Pharm Bioallied Sci. 2015;7(2):136. https://doi.org/10.4103/0975-7406.148782.
Misha G, Raghavendra Y, Messay W-M. Knowledge, attitude, practice and management of traditional medicine among people of Shopa Bultum, Southeast Ethiopia. Res J Pharmaceut Biol Chem Sci. 2014;5(5):152–70.
Ampomah IG, Malau-Aduli BS, Seidu A-A, Malau-Aduli AE, Emeto TI. Integrating traditional medicine into the Ghanaian health system: perceptions and experiences of traditional medicine practitioners in the Ashanti region. Int Health. 2022;15(4):414–27. https://doi.org/10.1093/inthealth/ihac059.
CSA. Population projection of ethiopia for all regions at wereda level from 2014–2017. Central Statistical Agency (CSA). Federal Democratic Republic of Ethiopia, Addis Ababa. 2019:118.
Asiimwe JB, Nagendrappa PB, Atukunda EC, Kamatenesi MM, Nambozi G, Tolo CU, Ogwang PE, Sarki AM. Prevalence of the use of herbal medicines among patients with cancer: a systematic review and meta-analysis. Evid Based Complement Alternat Med. 2021;9963038:1–18. https://doi.org/10.1155/2021/9963038.
El Hajj M, Holst L. Herbal medicine use during pregnancy: a review of the literature with a special focus on sub-Saharan Africa. Front Pharmacol. 2020;11:866. https://doi.org/10.3389/fphar.2020.00866.
Hughes GD, Aboyade OM, Clark BL, Puoane TR. The prevalence of traditional herbal medicine use among hypertensives living in South African communities. BMC Complement Altern Med. 2013;13(1):38. https://doi.org/10.1186/1472-6882-13-38.
Namuddu B, Kalyango JN, Karamagi C, Mudiope P, Sumba S, Kalende H, Wobudeya E, Kigozi BK, Waako P. Prevalence and factors associated with traditional herbal medicine use among patients on highly active antiretroviral therapy in Uganda. BMC Pub Health. 2011;11(1):855. https://doi.org/10.1186/1471-2458-11-855.
Boy HIA, Rutilla AJH, Santos KA, Ty AMT, Alicia IY, Mahboob T, Tangpoong J, Nissapatorn V. Recommended medicinal plants as source of natural products: a review. Digit Chin Med. 2018;1(2):131–42. https://doi.org/10.1016/S2589-3777(19)30018-7.
Jiang TA. Health benefits of culinary herbs and spices. J AOAC Int. 2019;102(2):395–411. https://doi.org/10.5740/jaoacint.18-0418.
Sato A. Does socio-economic status explain use of modern and traditional health care services? Soc Sci Med. 2012;75(8):1450–9. https://doi.org/10.1016/j.socscimed.2012.05.032.
Awiti JO. Poverty and health care demand in Kenya. BMC Health Serv Res. 2014;14(1):560. https://doi.org/10.1186/s12913-014-0560-y.
James PB, Wardle J, Steel A, Adams J. Traditional, complementary and alternative medicine use in Sub-Saharan Africa: a systematic review. BMJ Glob Health. 2018;3(5):e000895. https://doi.org/10.1136/bmjgh-2018-000895.
Payyappallimana U. Role of traditional medicine in primary health care. Yok J Soc Sci. 2010;14(6):57–75.
Herbreteau J-B, Tavernier E, Joly A, Marchand A, Édée A-É, Tauveron V, Maruani A. Traditional healers or bonesetters (“rebouteux”) in France: a survey of their practice, profile, and customers. Ann Dermatol Venereol. 2023;150(2):89–94. https://doi.org/10.1016/j.annder.2022.11.006.
Posadzki P, Watson LK, Alotaibi A, Ernst E. Prevalence of use of complementary and alternative medicine (CAM) by patients/consumers in the UK: systematic review of surveys. Clin Med. 2013;13(2):126. https://doi.org/10.7861/clinmedicine.13-2-126.
Mensah M, Komlaga G, Forkuo AD, Firempong C, Anning AK, Dickson RA. Toxicity and safety implications of herbal medicines used in Africa. Herbal Med. 2019;63:1992–0849. https://doi.org/10.5772/intechopen.72437.
Gyasi RM, Poku AA, Boateng S, Amoah PA, Mumin AA, Obodai J, Agyemang-Duah W. Integration for coexistence? Implementation of intercultural health care policy in Ghana from the perspective of service users and providers. J Integ Med. 2017;15(1):44–55. https://doi.org/10.1016/S2095-4964(17)60312-1.
Bernstein N, Akram M, Yaniv-Bachrach Z, Daniyal M. Is it safe to consume traditional medicinal plants during pregnancy? Phytother Res. 2021;35(4):1908–24. https://doi.org/10.1002/ptr.6935.
Acknowledgements
Not applicable.
Funding
The authors declare that they did not receive funding for this research from any source.
Author information
Authors and Affiliations
Contributions
NT conceived and designed the study, curated and extracted the data, and drafted the manuscript. SF extracted the data and conducted the quality and trend analysis. SD conducted the data analysis, interpreted the results, and assess the methodological quality. All authors revised, edited, and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tuasha, N., Fekadu, S. & Deyno, S. Prevalence of herbal and traditional medicine in Ethiopia: a systematic review and meta-analysis of 20-year studies. Syst Rev 12, 232 (2023). https://doi.org/10.1186/s13643-023-02398-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02398-9