Abstract
Background
Global epidemiological data indicates that despite implementation of multiple interventions and significant financial investment, the HIV/AIDS epidemic remained inadequately controlled as of 2020. E-health presents a novel approach in delivering health information and health care and has gained popularity in HIV prevention worldwide. However, evidence on the effectiveness of e-health interventions on HIV prevention among diverse populations remains inadequate. Our study aims to systematically evaluate the effectiveness of varying e-health interventions on HIV prevention, with the objective of providing data support and guidance for the development of future e-health HIV intervention strategies.
Methods
A systematic search of electronic English databases, including MEDLINE through PubMed, Embase, Scopus, and Web of Science, along with three Chinese databases, including National Knowledge Infrastructure (CNKI), Chinese Wanfang Digital Periodicals (WANFANG), and Chinese Science and Technology Periodicals (VIP) database, will be conducted for the period of 1 January 1980 to 31 December 2022. Additionally, gray literature and unpublished trials in trial registers will be searched. Studies aimed at HIV prevention through e-health interventions, with full-text publications available in either English or Chinese, will be included. Study types will be limited to RCT, cluster RCT, and quasi-experiment study. The risk of bias in individual studies will be assessed following the guideline highlighted by the Cochrane Handbook for Systematic Reviews of Interventions. The outcomes will cover cognitive, behavioral, psychological, management, and biological measures of individuals involved in e-health interventions. The quality of evidence will be assessed by the Grading of Recommendations, Assessment, Development, and Evaluation (GRADE) approach. Ultimately, a systematic review with meta-analysis will be conducted to compare the effectiveness of e-health interventions among diverse populations.
Discussion
This systematic review seeks to establish novel insights into the effectiveness of e-health interventions in diverse populations worldwide. It will inform the design and use of e-health interventions to optimize HIV-related strategies.
Systematic review registration
PROSPERO CRD42022295909.
Similar content being viewed by others
Background
The HIV epidemic has presented significant global challenges, prompting a major focus on HIV prevention as a public health priority. In this context, the United Nations has established ambitious goals, including the end of the AIDS epidemic by 2030 [1], as well as the objective of reducing new HIV infections to fewer than 500,000 annually [2]. Despite the efforts of the international health community, these goals remain elusive. To illustrate, the United Nations Program on HIV and AIDS (UNAIDS) has reported that, as of 2021, approximately 38.4 million people worldwide are living with HIV [3]. Moreover, there were about 1.5 million new HIV infections in 2021, which was a number far exceeding the targeted goal and has threatened not only global public health but also society and the economy [3].
Despite the implementation of numerous intervention strategies such as immediate start of antiretroviral therapy (ART), promotion of condom uses, opioid drug substitution, needle and syringe exchange program, and the provision of voluntary consultation and testing (VCT) services, targeted interventions for key populations, school-based awareness campaigns, promotion of HIV self-testing [4, 5], the decline in new HIV infections remains insufficient for achieving established targets. Moreover, HIV transmission patterns have recently shifted from high-risk populations to the general population worldwide [6,7,8]. Given the increasing public health burden of HIV and the pressing need to end the epidemic by 2030, innovative interventions must be integrated into traditional approaches due to changes in people’s lifestyle and behaviors of seeking sexual partners.
The proliferation of the Internet and the increasing emergence of dating apps or websites have significantly enhanced the ease and privacy of meeting and approaching causal sexual partners, potential romantic partners, one-night stand partners, and Internet partners [9,10,11,12]. Internet friendship platforms, such as some geosocial networking applications (GSN apps) especially dating apps (e.g., Tinder, Grindr), have made communication and interaction with other users in close proximity extremely convenient [13]. While public venues such as bars and parks were traditionally popular haunts for seeking causal sexual partners in the past, the use of GSN apps or dating apps has increasingly replaced these means of courtship in recent years [14]. Gravningen K. et al.’s study showed that 30% of Norwegian adolescents reported Internet partner seeking by using dating apps (e.g., Tinder, Bumble, Hinge) and social media networks (e.g., Facebook, Twitter, Instagram) [12]. Studies have shown that a significant number of men who have sex with men (MSM) in the USA, ranging from 36.0 to 63.6%, and mainland China (40.6%) used GSN apps to seek male partners [15,16,17,18]. Furthermore, HIV incidence among GSN apps’ users was found to be 4 times higher than that of nonusers (8.5 vs 2.0 per 100 person-years) [19]. Therefore, there is an urgent need for targeted HIV prevention measures through Internet.
E-health is defined as a collection of electronic technologies that utilize the Internet to provide healthcare services, thereby improving the quality of life and facilitating healthcare delivery [20, 21]. These technologies encompass a variety of practices such as electronic medical records (eMRs), electronic health records (eHRs), mobile health (m-health) applications for health practice, remote service provision through telecommunications (telehealth and telemedicine), electronic health information systems (eHIS), medication systems, and social media platforms [22]. The World Health Organization (WHO) recognizes that e-health has the potential to strengthen preventive medical care, enhance healthcare quality, reduce costs for healthcare institutions and users, and increase access to healthcare services for poor, underserved, vulnerable populations and people in marginalized areas [20]. Furthermore, e-health has the potential to transform healthcare service access and quality and help contain costs [23]. The WHO emphasizes that e-health plays a key role in achieving universal health coverage [24].
Currently, there is increasing academic interest in the effectiveness of e-health interventions for HIV prevention worldwide. For example, Marhefka, Turner, and Lockhart [25] utilized an e-health video conference program for women living with HIV (WLH), investigating the feasibility of group-based e-health interventions. Michael Argenyi et al. [26] utilized social media in HIV screening outreach for deaf and hard-of-hearing adults, demonstrating its effectiveness in mitigating technological or linguistic barriers. David Loutfi et al. [27] analyzed a pilot social media intervention for HIV prevention among marginalized young women in Botswana, revealing that while social media could enhance reach to hard-to-reach populations, its acceptance was lower than that of face-to-face interventions. Furthermore, Brooks, Nieto, Swendeman, Myers, Lepe, Cabral, Kao, Donohoe, and Comulada [28] reported that social media and mobile technology (SMMT) interventions were well accepted in managing HIV care among youth and young adults aged 13–34 living with HIV. Overall, previous studies on e-health HIV interventions were varied in terms of population and intervention tools, and the findings were often contradictory across studies. Therefore, there is a critical need to synthesize and integrate the existing evidence to establish more robust conclusions.
Nevertheless, previous systematic reviews on this topic have provided incomplete evidence. On one hand, most reviews have only focused on promoting treatment among persons living with HIV, disregarding the effectiveness of e-health in preventing HIV infection [29,30,31]. On the other hand, previous relevant systematic reviews have predominantly concentrated on key populations, such as MSM [32, 33], African countries with a high burden of HIV epidemic [34,35,36], and HIV-related outcomes, while disregarding other outcomes such as psychological health [37]. To end the AIDS pandemic by 2030, all population strategies must be considered. However, globally, there is a paucity of systematic summaries and classification of previous evidence regarding e-health intervention effectiveness for all populations. Hence, the objective of this study is to systematically summarize and quantitatively integrate different types of e-health interventions’ effectiveness across various populations and regions, enabling the selection for more effective prevention measures to end AIDS by 2030.
Methods
Protocol and registration
A systematic review with meta-analysis will be implemented in this study. This protocol of meta-analysis will be performed on the basis of the Preferred Reporting Items for Systematic review and Meta-Analysis Protocol (PRISMA-P) statement (Additional file 1) [38], and the reporting of the following systematic review with meta-analysis will use the PRISMA extension statement as a guide. This study has been registered at PROSPERO with registration number CRD42022295909.
Eligibility criteria and type of study
The optimal study design for inclusion in this systematic review is randomized controlled trials (RCTs). However, considering the inherent characteristics of public health interventions, individualized randomization may be impractical in some circumstances. Therefore, cluster RCTs and quasi-experimental studies with self-control will also be considered for inclusion. Cross-sectional studies utilizing only online surveys will not be incorporated in this analysis. Studies that meet the following inclusion criteria will be included: (1) focused on HIV prevention, (2) the study conducting an e-health intervention originally, (3) written in English and retrieved from electronic English databases or in Chinese and retrieved from electronic Chinese databases with full-text access, and (4) published within the timeframe of January 1, 1980, to December 31, 2022, as the first documented case of HIV was reported in Los Angeles in 1981 [39].
Participants
In this study, participants who received an e-health intervention will be included. The subgroup analysis will primarily concentrate on evaluating the effectiveness of e-health interventions among university students, women, adolescents, and HIV key populations (i.e., men who have sex with men, sex workers, people who inject drugs, transgender individuals, and individuals confined in correctional facilities).
Type of interventions
Original researches conducting e-health interventions on HIV prevention will be included. E-health interventions are defined as those implemented through the Internet, such as m-health and telehealth, which utilize electronic technologies to provide healthcare resources, services, and information. Studies that solely conducted online surveys without any intervention will be excluded from the analysis.
Outcomes of interest
We will consider the systematic reviews with the following outcomes; the details of these outcomes are shown in Table 1.
Data sources and search strategy
Electronic searches
We plan to conduct a comprehensive and systematic search of various electronic English databases, including MEDLINE, PubMed, Embase, Scopus, and Web of Science, as well as three Chinese databases, which are National Knowledge Infrastructure (CNKI), Chinese Wanfang Digital Periodicals (WANFANG), and Chinese Science and Technology Periodicals (VIP) database. The detail of these search strategies is shown in Additional file 2. This search strategy has been collaboratively developed by a medical librarian and all authors and is based on key terms from previous literature. In addition to this, we will perform a thorough examination of the reference lists of identified relevant RCTs and reviews, contact experts in the field of HIV e-health interventions to identify any additional trials or results, and scrutinize ClinicalTrials.gov, Chinese Clinical Trial Registry (ChiCTR), and International Clinical Trials Registry Platform (ICTRP) to identify planned, ongoing, or unpublished trials. In order to retrieve any gray literature, we will also search Google Scholar and Baidu Scholar.
Study selection
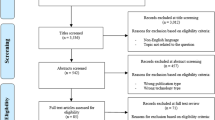
Two reviewers (L. W. and X. Y.) will independently assess the titles and abstracts that meet the initial retrieval criteria. Studies that do not satisfy the eligibility criteria will be excluded. Subsequently, the remaining publications will undergo a full-text screening by both investigators (L. W. and X. Y.) according to the same inclusion criteria. In the event of any disagreements, discussion will be employed to seek consensus. Any discrepancy that cannot be resolved will be referred to a third reviewer to determine the final decision. Furthermore, excluded publications and their respective reasons for elimination will be confirmed by a third reviewer. A PRISMA 2009 flow chart (Fig. 1) will be used to show the process of study selection. The extracted references will be managed using EndNote software (version X9 Windows). A pilot test using articles published in 2022 will be conducted, and necessary adjustments will be made based on the results.
Data extraction
The studies selected through the study selection process will undergo data extraction, wherein information from the studies will be extracted after a thorough reading of the full text, and presented in Table 2. The data extraction form will be created using Microsoft Excel 2016.
Data extraction will be conducted by two independent reviewers (L. W. and X. Y.) utilizing the designed data extraction form. Following this process, the records extracted by the reviewers will be cross-checked, and any disputed points will be resolved through a third reviewer who will make the final decision. Upon completion of the extraction process, the data records will be sorted by region and year. This will result in a dataset of included studies for data analysis. A pilot test will be conducted on selected studies published in 2022 with adjustments made as necessary thereafter.
Risk-of-bias assessment
The Cochrane Collaboration risk-of-bias (ROB) tool or Cochrane risk-of-bias tool for cluster-randomized control trials (RoB2.0) will be used by two independent authors (L. W. and X. Y.) to assess the risk of bias in the included studies [40,41,42]. In the event of any disagreements, they will be resolved through discussion, and any unresolved disagreement will be referred to the third reviewer for a final decision. Each criteria of RoB or RoB2.0 will be classified into low risk (meet the standard), unclear risk (specific details or descriptions were not reported), or high risk (not fulfilling the criteria). The quality assessment results will be presented using the Cochrane risk-of-bias assessment chart [43].
Statistical analysis
The extracted data will be reported using descriptive statistics. Meta-analysis will be employed to generate pooled estimates. Relevant indicators will utilize the standardized mean difference (SMD) [44] for continuous variables (e.g., knowledge score, scale score) and relative risk (RR) or odds ratio (OR) for categorical variables (e.g., HIV testing, condom use). All statistical analyses will be conducted using meta-analysis package in R software version 4.2.2 (R Core Team). Inconsistency (I2) based on the chi-squared test will be utilized to assess overall heterogeneity, classified into three levels: I2 ≤ 50%, low heterogeneity; I2 > 50% to I2 < 75%, moderate heterogeneity; and I2 ≥ 75%, high heterogeneity. A random-effects model is preferable, particularly when I2 > 50% [45, 46]. Outcomes will be considered statistically significant when p < 0.05. Furthermore, for studies investigating various types of e-health interventions for the same outcome, network meta-analysis using the Bayesian approach will be utilized to compare the effectiveness among different types of e-health interventions if possible. For outcomes that cannot be quantitatively synthesized due to too few studies available or high heterogeneity in intervention methods or study populations, a narrative synthesis will be conducted.
If feasible, subgroup analysis will be conducted to evaluate intervention effects in various subpopulations, including (1) target populations, such as key populations (e.g., MSM, people who inject drugs, people in prisons and other closed settings, sex workers, and transgender people) and other focused population subgroups (e.g., adolescents, women, university students); (2) sex (male, female); (3) age groups; (4) types of e-health interventions; (5) types of countries, encompassing western or eastern countries and developing or developed countries; (6) prevalence states of countries, including those with the highest, moderate, and lowest rates of HIV prevalence; and (7) interactive and noninteractive e-health interventions.
Sensitivity analysis will be conducted to assess the stability and reliability of the study by excluding studies with special characteristics, such as those of lower quality (e.g., before-after studies conducted in the same population). Furthermore, we will perform additional sensitivity analyses by iteratively excluding each study to gauge its impact on overall estimates and to ascertain the stability of results.
Publication bias will be assessed by using a funnel plot (suggested in cases where no less than 10 studies are included in the meta-analysis) and Egger’s test [47]. To test asymmetry in the funnel plot, a rank correlation test or regression analysis will be employed. In circumstances where data is accessible for the analysis from no less than 10 trials, meta-regression techniques will also be employed to investigate the association of trial characteristics with effect sizes.
If cluster-randomized trials are incorporated, we will perform sample size adjustment utilizing estimates to evaluate covariance with cluster-level adjustment for participants with measurements at both baseline and final follow-up. Furthermore, interaction terms will be employed to examine the consistency of effects among subgroups [48, 49].
Certainty of evidence
The Grading of Recommendations Assessment, Development, and Evaluation (GRADE) will be utilized to assess the level of certainty of evidence [50]. A rating of high, moderate, low, or very low quality will be assigned to each piece of evidence based on its performance across five domains, comprising of risk of bias, inconsistency, indirectness, imprecision, and other relevant considerations [51, 52]. The GRADE-based determination of evidence certainty will be carried out by two independent authors (L. W. and X. Y.), with any disagreements resolved through discussion. For cases where an agreement is not reached, the matter will be referred to a third reviewer for final adjudication.
Discussion
Based on the protocol of this study, a pioneering systematic review with meta-analysis will be conducted to summarize and assess the impact of e-health interventions on HIV prevention across various outcome indicators and populations worldwide. Although several factors, including imperfect e-health implementation and demographic factors such as gender, residence, income, education, and culture, can influence the adoption of e-health, it still holds significant potential in promoting people’s health status [53]. Our findings will highlight the diverse contributions made by e-health interventions and aid in the development and decision-making of public health strategies for HIV prevention. However, e-health interventions may not show advantages over traditional methods in some aspects, because it changes the communication mode between the intervention implementers and recipients. Hence, it is crucial to capitalize on the advantages while avoiding potential disadvantages. Ultimately, the intended outcome is a range of policy options that employ e-health interventions, promoting an accelerated end to the AIDS pandemic. One limitation of the current study is the inclusion of studies written exclusively in English and Chinese, hence leading to the possibility of missing relevant studies written in other languages. To enhance the comprehensiveness of our study, we will incorporate evidence generated from different types of studies (e.g., RCT, cluster RCT, and quasi-experiment study). Furthermore, we recommend users to adapt or translate the framework within their respective contexts, considering other relevant characteristics such as subgroups, cultural factors, and potential barriers. In summary, this systematic review will bring a novel concept and direction that exploits e-health to achieve the aspirational goal of ending AIDS by 2030.
Availability of data and materials
Not applicable.
Abbreviations
- UNAIDS:
-
The United Nations Program on HIV and AIDS
- RCTs:
-
Randomized controlled trials
- ART:
-
Antiretroviral therapy
- VCT:
-
Voluntary consultation test
- GSN apps:
-
Geosocial networking applications
- MSM:
-
Men who have sex with men
- eMRs:
-
Electronic medical records
- eHRs:
-
Electronic health records
- m-health:
-
Applications for health practice for mobile health
- eHIS:
-
Electronic health information systems
- WHO:
-
World Health Organization
- SMMT:
-
Social media and mobile technology
- PRISMA-P:
-
Preferred Reporting Items for Systematic review and Meta-Analysis Protocol
- PrEP:
-
Pre-exposure prophylaxis
- PEP:
-
Postexposure prophylaxis
- ROB:
-
The Cochrane Collaboration risk-of-bias (ROB) tool
- RoB2.0:
-
Cochrane risk-of-bias tool for cluster-randomized control trials
- SMD:
-
Standardized mean difference
- SD:
-
Standard deviation
- SE:
-
Standard error
- RR:
-
Relative risk
- OR:
-
Odds ratio
- GRADE:
-
Grading of Recommendations Assessment, Development, and Evaluation
- ChiCTR:
-
Chinese Clinical Trial Registry
- ICTRP:
-
International Clinical Trials Registry Platform
References
United Nations. Transforming our world: the 2030 Agenda for Sustainable Development. 2015. https://sustainabledevelopment.un.org/post2015/transformingourworld/publication.
The Joint United Nations Programme on HIV/AIDS. Political declaration on HIV and AIDS: on the fast-track to accelerate the fight against HIV and to end the AIDS epidemic by 2030. 2016. https://www.unaids.org/en/resources/presscentre/pressreleaseandstatementarchive/2016/june/20160608_PS_HLM_PoliticalDeclaration.
UNAIDS. Global HIV & AIDS statistics — fact sheet. 2021. https://www.unaids.org/en/resources/fact-sheet.
Piot P, Abdool Karim SS, Hecht R, Legido-Quigley H, Buse K, Stover J, Resch S, Ryckman T, Møgedal S, Dybul M, Goosby E, Watts C, Kilonzo N, Mcmanus J, Sidibé M. UNAIDS–Lancet Commission. Defeating AIDS–advancing global health. Lancet. 2015;386(9989):171–218.
Harries AD, Suthar AB, Takarinda KC, Tweya H, Kyaw NT, Tayler-Smith K, Zachariah R. Ending the HIV/AIDS epidemic in low- and middle-income countries by 2030: is it possible? F1000Res. 2016;5:2328.
Tang WM, Lyu P. Conducting implementation research of HIV self-testing for overall achievement of HIV/AIDS prevention and treatment goal in China. Zhonghua Liu Xing Bing Xue Za Zhi. 2021;42:215–8.
World Health Organization. Consolidated guidelines on HIV prevention, diagnosis, treatment and care for key populations. 2014. https://www.who.int/publications/i/item/9789241511124.
Tran BX, Do HP, Hall B, Latkin CA, Nguyen TQ, Nguyen CT, Ho CSH, Ho RCM. The use of health behavioral theories in HIV/AIDS research: a bibliometric analysis (gap research). AIDS Rev. 2019;21(2):93–107.
Mao YX, Xiao CC, Wang T, Li SY, Yan H. One-night-stand behavior and associated factors among young men who have sex with men in Wuhan, China. Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38(6):746–9.
Watchirs Smith L, Guy R, Degenhardt L, Yeung A, Rissel C, Richters J, Liu B. Meeting sexual partners through Internet sites and smartphone apps in Australia: national representative study. J Med Internet Res. 2018;20(12): e10683.
Castro Á, Barrada JR, Ramos-Villagrasa PJ, Fernández-Del-Río E. Profiling dating apps users: sociodemographic and personality characteristics. Int J Environ Res Public Health. 2020;17(10):3653.
Gravningen K, Aicken CR, Schirmer H, Mercer CH. Meeting sexual partners online: associated sexual behaviour and prevalent chlamydia infection among adolescents in Norway: a cross-sectional study. Sex Transm Infect. 2016;92(2):97–103.
Barrada JR, Castro Á, Fernández Del Río E, Ramos-Villagrasa PJ. Do young dating app users and non-users differ in mating orientations? PLoS ONE. 2021;16(2): e0246350.
Castro Á, Barrada JR. Dating apps and their sociodemographic and psychosocial correlates: a systematic review. Int J Environ Res Public Health. 2020;17:6500.
Phillips G 2nd, Magnus M, Kuo I, Rawls A, Peterson J, Jia Y, Opoku J, Greenberg AE. Use of geosocial networking (GSN) mobile phone applications to find men for sex by men who have sex with men (MSM) in Washington. DC AIDS Behav. 2014;18(9):1630–7.
Beymer MR, Weiss RE, Bolan RK, Rudy ET, Bourque LB, Rodriguez JP, Morisky DE. Sex on demand: geosocial networking phone apps and risk of sexually transmitted infections among a cross-sectional sample of men who have sex with men in Los Angeles County. Sex Transm Infect. 2014;90(7):567–72.
Lehmiller JJ, Ioerger M. Social networking smartphone applications and sexual health outcomes among men who have sex with men. PLoS ONE. 2014;9: e86603.
Bien CH, Best JM, Muessig KE, Wei C, Han L, Tucker JD. Gay apps for seeking sex partners in China: implications for MSM sexual health. AIDS Behav. 2015;19(6):941–6.
Xu J, Yu H, Tang W, Leuba SI, Zhang J, Mao X, Wang H, Geng W, Jiang Y, Shang H. The effect of using geosocial networking apps on the HIV incidence rate among men who have sex with men: eighteen-month prospective cohort study in Shenyang, China. J Med Internet Res. 2018;20(12): e11303.
Tebeje TH, Klein J. Applications of e-Health to support person-centered health care at the time of COVID-19 pandemic. Telemed J E Health. 2021;27:150–8.
Mauco KL, Scott RE, Mars M. Validation of an e-Health readiness assessment framework for developing countries. BMC Health Serv Res. 2020;20:575.
World Health Organization. Regional action agenda on harnessing e-Health for improved health service delivery in the Western Pacific. 2019. https://www.who.int/publications/i/item/9789290618959.
World Health Organization. Harnessing e-Health for improved service delivery. https://apps.who.int/iris/bitstream/handle/10665/280002/WPR-RC069-08-eHealth-2018-en.pdf?sequence=1&isAllowed=y.
World Health Organization. Strengthening health workers capacities through digital health. 2019. https://www.who.int/news/item/09-07-2019-strengthening-health-workers-capacities-through-digital-health.
Marhefka SL, Turner D, Lockhart E. Understanding women’s willingness to use e-Health for HIV-related services: a novel application of the technology readiness and acceptance model to a highly stigmatized medical condition. Telemed J E Health. 2019;25:511–8.
Argenyi M, Kushalnagar P. Social media use and HIV screening uptake among deaf adults in the United States: cross-sectional survey study. JMIR Public Health Surveill. 2019;5: e13658.
Loutfi D, Andersson N, Law S, Kgakole L, Salsberg J, Haggerty J, Cockcroft A. Reaching marginalized young women for HIV prevention in Botswana: a pilot social network analysis. Glob Health Promot. 2020;27(2):74–81.
Brooks RA, Nieto O, Swendeman D, Myers J, Lepe RM, Cabral A, Kao U, Donohoe T, Comulada WS. Qualitative evaluation of social media and mobile technology interventions designed to improve HIV health outcomes for youth and young adults living with HIV: a HRSA SPNS initiative. Health Promot Pract. 2020;21(5):693–704.
Cho H, Iribarren S, Schnall R. Technology-mediated interventions and quality of life for persons living with HIV/AIDS. A systematic review Appl Clin Inform. 2017;8:348–68.
Njoroge M, Zurovac D, Ogara EA, Chuma J, Kirigia D. Assessing the feasibility of eHealth and mHealth: a systematic review and analysis of initiatives implemented in Kenya. BMC Res Notes. 2017;10(1):90.
Meiksin R, Melendez-Torres GJ, Falconer J, Witzel TC, Weatherburn P, Bonell C. eHealth interventions to address sexual health, substance use, and mental health among men who have sex with men: systematic review and synthesis of process evaluations. J Med Internet Res. 2021;23(4): e22477.
Kudrati SZ, Hayashi K, Taggart T. Social media & PrEP: a systematic review of social media campaigns to increase PrEP awareness & uptake among young Black and Latinx MSM and women. AIDS Behav. 2021;25:4225–34.
Santos VDF, Costa AKB, Lima ICV, Alexandre HO, Gir E, Galvão MTG. Use of the telephone for accessing people living with HIV/AIDS to antiretroviral therapy: systematic review. Cien Saude Colet. 2019;24(9):3407–16.
Cheng LJ, Kumar PA, Wong SN, Lau Y. Technology-delivered psychotherapeutic interventions in improving depressive symptoms among people with HIV/AIDS: a systematic review and meta-analysis of randomised controlled trials. AIDS Behav. 2020;24(6):1663–75.
Demena BA, Artavia-Mora L, Ouedraogo D, Thiombiano BA, Wagner N. A systematic review of mobile phone interventions (SMS/IVR/Calls) to improve adherence and retention to antiretroviral treatment in low-and middle-income countries. AIDS Patient Care STDS. 2020;34(2):59–71.
Manby L, Aicken C, Delgrange M, Bailey JV. Effectiveness of eHealth interventions for HIV prevention and management in sub-Saharan Africa: systematic review and meta-analyses. AIDS Behav. 2022;26(2):457–69.
Moher D, Shamseer L, Clarke M, Ghersi D, Liberati A, Petticrew M, Shekelle P, Stewart LA, PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst Rev. 2015;4(1):1.
Bailey JV, Wayal S, Aicken CRH, Webster R, Mercer CH, Nazareth I, Rait G, Peacock R, Murray E. Interactive digital interventions for prevention of sexually transmitted HIV. AIDS. 2021;35(4):643–53.
Feroze KB, Wang J. Ocular manifestations of HIV. In: StatPearls. Treasure Island: StatPearls Publishing; 2021. PMID: 28722955.
Wolff RF, Moons KGM, Riley RD, Whiting PF, Westwood M, Collins GS, Reitsma JB, Kleijnen J, Mallett S, PROBAST Group†. PROBAST: a tool to assess the risk of bias and applicability of prediction model studies. Ann Intern Med. 2019;170(1):51–8 PMID: 30596875.
Lyu XZ, Sun F, Zhan SY. Risk related to bias assessment: (4) Revised Cochrane risk of bias tool for cluster-randomized control trials (RoB2.0). Zhonghua Liu Xing Bing Xue Za Zhi. 2018;39(2):240–4. Chinese. PMID: 29495213.
Yang ZR, Sun F, Zhan SY. Risk on bias assessment: (2) Revised Cochrane risk of bias tool for individually randomized, parallel group trials (RoB2.0). Zhonghua Liu Xing Bing Xue Za Zhi. 2017;38(9):1285–91. Chinese. PMID: 28910948.
Mills K, Marchand G, Sainz K, Azadi A, Ware K, Vallejo J, Anderson S, King A, Osborn A, Ruther S, Brazil G, Cieminski K, Hopewell S, Rials L, Klipp A. Salpingectomy vs tubal ligation for sterilization: a systematic review and meta-analysis. Am J Obstet Gynecol. 2021;224(3):258–65.
Cuijpers P, Weitz E, Cristea IA, Twisk J. Pre-post effect sizes should be avoided in meta-analyses. Epidemiol Psychiatr Sci. 2017;26(4):364–8.
Tleyjeh IM, Kashour Z, Damlaj M, Riaz M, Tlayjeh H, Altannir M, Altannir Y, Al-Tannir M, Tleyjeh R, Hassett L, Kashour T. Efficacy and safety of tocilizumab in COVID-19 patients: a living systematic review and meta-analysis. Clin Microbiol Infect. 2021;27(2):215–27.
Borenstein M, Hedges LV, Higgins JP, Rothstein HR. A basic introduction to fixed-effect and random-effects models for meta-analysis. Res Synth Methods. 2010;1(2):97–111.
Yadav V, Jain A, Dabar D, Goel AD, Sood A, Joshi A, Agarwal SS, Nandeshwar S. A meta-analysis on the prevalence of depression in perimenopausal and postmenopausal women in India. Asian J Psychiatr. 2021;57: 102581.
Smaill FM, Vazquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database Syst Rev. 2019;2019(11):CD000490.
Yin X, Rodgers A, Perkovic A, Huang L, Li KC, Yu J, Wu Y, Wu JHY, Marklund M, Huffman MD, Miranda JJ, Di Tanna GL, Labarthe D, Elliott P, Tian M, Neal B. Effects of salt substitutes on clinical outcomes: a systematic review and meta-analysis. Heart. 2022;108(20):1608–15.
Gonzalez-Padilla DA, Dahm P. Evidence-based urology: understanding GRADE methodology. Eur Urol Focus. 2021;7:1230–3.
Zeng L, Brignardello-Petersen R, Hultcrantz M, Siemieniuk RAC, Santesso N, Traversy G, Izcovich A, Sadeghirad B, Alexander PE, Devji T, Rochwerg B, Murad MH, Morgan R, Christensen R, Schünemann HJ, Guyatt GH. GRADE guidelines 32: GRADE offers guidance on choosing targets of GRADE certainty of evidence ratings. J Clin Epidemiol. 2021;137:163–75.
Hultcrantz M, Rind D, Akl EA, Treweek S, Mustafa RA, Iorio A, Alper BS, Meerpohl JJ, Murad MH, Ansari MT, Katikireddi SV, Östlund P, Tranæus S, Christensen R, Gartlehner G, Brozek J, Izcovich A, Schünemann H, Guyatt G. The GRADE Working Group clarifies the construct of certainty of evidence. J Clin Epidemiol. 2017;87:4–13.
Alanezi F. Factors affecting the adoption of e-health system in the Kingdom of Saudi Arabia. Int Health. 2021;13:456–70.
Funding
This work is supported by the National Natural Science Foundation of China (72104008). The funding sources have no role in the study design, analysis, reporting, or the decision to publish the study.
Author information
Authors and Affiliations
Contributions
WL, YXY, ML, ZB, JZW, HRG, and XJH, participated in the conception and design of the study, including search strategy development. WL, YXY, ML, ZB, and JZW, tested the feasibility of the study. WL, wrote the manuscript. YXY, improved the manuscript. All the authors critically reviewed this manuscript and approved the final version.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
PRISMA-P 2015 Checklist.
Additional file 2.
Search strategy.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wang, L., Yan, Xy., Mei, L. et al. Effect of e-health interventions on HIV prevention: a protocol of systematic review and meta-analysis. Syst Rev 12, 106 (2023). https://doi.org/10.1186/s13643-023-02274-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02274-6