Abstract
Background
The health effects of dietary fats are a controversial issue on which experts and authoritative organizations have often disagreed. Care providers, guideline developers, policy-makers, and researchers use systematic reviews to advise patients and members of the public on optimal dietary habits, and to formulate public health recommendations and policies. Existing reviews, however, have serious limitations that impede optimal dietary fat recommendations, such as a lack of focus on outcomes important to people, substantial risk of bias (RoB) issues, ignoring absolute estimates of effects together with comprehensive assessments of the certainty of the estimates for all outcomes.
Objective
We therefore propose a methodologically innovative systematic review using direct and indirect evidence on diet and food-based fats (i.e., reduction or replacement of saturated fat with monounsaturated or polyunsaturated fat, or carbohydrates or protein) and the risk of important health outcomes.
Methods
We will collaborate with an experienced research librarian to search MEDLINE, EMBASE, CINAHL, and the Cochrane Database of Systematic Reviews (CDSR) for randomized clinical trials (RCTs) addressing saturated fat and our health outcomes of interest. In duplicate, we will screen, extract results from primary studies, assess their RoB, conduct de novo meta-analyses and/or network meta-analysis, assess the impact of missing outcome data on meta-analyses, present absolute effect estimates, and assess the certainty of evidence for each outcome using the GRADE contextualized approach. Our work will inform recommendations on saturated fat based on international standards for reporting systematic reviews and guidelines.
Conclusion
Our systematic review and meta-analysis will provide the most comprehensive and rigorous summary of the evidence addressing the relationship between saturated fat modification for people-important health outcomes. The evidence from this review will be used to inform public health nutrition guidelines.
Trial registration
PROSPERO Registration: CRD42023387377.
Similar content being viewed by others
Background
Non-communicable diseases, including cardiovascular disease (CVD), cancer, and diabetes are responsible for 4 of 5 deaths worldwide [1]. Modifying dietary habits may reduce the incidence of non-communicable diseases, though what constitutes an optimal fat intake and dietary pattern is highly debated.
The health effects of dietary fats are a controversial issue on which experts and authoritative organizations have often disagreed [2, 3]. While some guidelines, for example, have recommended restricting dietary fats to less than 30–35% of total energy intake, others have concluded that reduction of total dietary fats has little effect on improving health outcomes [4,5,6,7]. The relationship between saturated fats and cardiovascular disease is another case in point, about which authoritative organizations and experts continue to disagree [8, 9].
Care providers, guideline developers, policy-makers, and researchers use systematic reviews to advise patients on optimal dietary habits, formulate dietary recommendations and policies, and to plan future research [10,11,12]. While a plethora of systematic reviews on the health effects of dietary fats have been published to date [13], existing reviews have serious limitations. Most systematic reviews, for example, have addressed only one or a few health-related outcomes, whereas dietary recommendations and related policy implementation require consideration of all people-important outcomes (e.g., all-cause, cardiovascular, and cancer mortality, non-fatal stroke and myocardial infarction, cancer incidence, type 2 diabetes, dementia, and quality of life), as well as patient or public health-related values and preferences that bear on dietary recommendations [11, 12, 14]. Further, existing reviews often contain substantial deficiencies. For example, reviews often fail to present absolute effect estimates, which can lead to misinterpretation of findings [15,16,17,18,19,20]. Equally important, only a handful of reviews have formally and comprehensively evaluated the certainty of evidence for each outcome—a critical step in contextualizing review findings and generating dietary recommendations [15, 19,20,21], and aside from one dietary guideline on red and processed meat [22], none have used a contextualized approach, as recently recommended by the Grading of Recommendations, Assessment, Development and Evaluations (GRADE) working group [23,24,25]. Finally, the extent to which risk of bias (RoB) associated with missing participant outcome data reduces the certainty in results [26, 27] also represents a key issue in contextualizing review findings and the generation of dietary recommendations [15]. For instance, evidence suggests that almost one in every three trials with statistically significant results lose significance when making plausible assumptions about the outcomes of participants with missing data [26].
We propose a methodologically innovative systematic review to summarize existing evidence on reducing or replacing dietary saturated fat with other nutrients (mono- or polyunsaturated fat, carbohydrates, protein) and important health outcomes. This work will improve upon the limitations of previous reviews and guidelines by addressing a comprehensive list of people-important single outcomes that patients and members of the public can better understand (rather than composite outcomes), analyze RoB using a nutrition specific assessment [14, 28] as well as tools for assessing missing data [27, 29], and calculating absolute effect estimates and evaluating the certainty of these estimates using the GRADE fully contextualized approach [15, 24].
Methods
Research question
Among adult patients and members of the public with or without cardiometabolic conditions, what is the impact of modifying dietary fat intake (lowering saturated fat intake, or lowering saturated fat while increasing polyunsaturated fat and/or increasing monounsaturated fat and/or protein and/or complex carbohydrates) on the risk of critically important health outcomes (e.g., mortality, stroke, myocardial infarction, quality of life)?
Scope
Our systematic review will summarize foods and diets addressing reduced saturated fats, and the replacement or modification of saturated fats with monounsaturated, polyunsaturated fats (e.g., omega-3 and omega-6), carbohydrates or protein and the relationship with all-cause mortality; cardiovascular mortality; cancer mortality; cardiovascular disease including coronary heart disease and myocardial infarctions; stroke; total cancer incidence; type 2 diabetes; dementia including Alzheimer’s disease; satisfaction with diet; and quality of life in patients with or without cardiometabolic conditions (e.g., previous history of cardiovascular events such as myocardial infarction or stroke, diabetes, hypertension) but without other chronic (e.g., cancer) or infectious conditions.
Inclusion criteria
We will include randomized controlled trials (RCTs) of individuals or groups (six or more clusters). Randomized trials have to state an intention to reduce saturated fat (SFA) intake via appropriate food or nutrient-based aims, or trial reports have to provide a dietary aim in general, such as reducing total fat or improving heart health (reduced saturated fats and encouraged fruit and vegetables), while also achieving a statistically significant (p < 0.05) reduction in saturated fat reduction between the the intervention arm and control arm during the trial period. Eligible interventions have to be low fat dietary advice, supplementation with naturally occurring oils or fats (e.g., food based olive oil or fish), or provision of modified or low-fat foods, as compared to an intake of a higher saturated fat diet, placebo or a control diet higher in fat (e.g., usual diet). Our intended time-point of interest for the duration of the diet intervention will be 2 years (24 months) or more.
We will exclude trials that are formula based (e.g., weight-loss formulas such a NutriSystem), have a pharmacological intervention for weight-loss (e.g., Olestra), or the primary aim to assess weight-loss (experimental arm is calorie restricted while the control arm is ad libitum). If trials employ active interventions such cardiometabolic or smoking cessation medications (e.g., statins, Metformin, Chantix), the study will be eligible if both groups are provided drugs, active intervention. If a trial demonstrated a statistically significant between group reduction in SFA and encouraged active interventions such as physical exercise, or cardiovascular medications in one arm (intervention) with no exercise or medication in the alternative arm (control), we will exclude. We will also exclude observational studies given that over 50,000 patients have been randomized to SFA reduction and replacement interventions, and the available trials have captured all of our people-important outcomes. For the purpose of informing SFA dietary guidelines, we will use the most recent, high-quality systematic reviews of cohort studies (e.g., [30, 31]).
Search strategy
We will collaborate with an experienced research librarian to search MEDLINE, EMBASE, CINAHL, and registers for reviews including PROSPERO and the Cochrane Database of Systematic Reviews (CDSR) for systematic reviews of RCTs. For reviews, we will run an updated search from the date of the last comprehensive systematic review (e.g., [32]) for new primary studies. Since questions addressed by older reviews are likely to have been also addressed in more recent reviews, we will restrict the search to reviews published from 2015 onward. We will also search the reference lists of included reviews, related publications on PubMed and Google Scholar, clinicaltrials.gov and contact content and research experts in this area to further augment our search. We will also search included studies from previous systematic reviews to ensure the subsequent studies have not been reported with longer follow-up data.
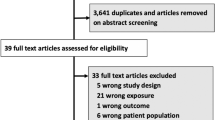
Screening and study selection
Pairs of reviewers will complete calibration exercises, after which they will perform screening of search results independently and in duplicate. Reviewers will resolve discrepancies by discussion or by adjudication by an expert research methodologist. To start, we will search for systematic reviews that include one or more RCTs that address the association between dietary fats and important health outcomes (above) in adults with or without cardiometabolic conditions, but without other chronic or infectious conditions. In cases in which two or more systematic reviews reporting on the same exposure and outcome have overlapping searches within three months of one another, we will select the systematic review that is the most comprehensive (i.e., includes the most eligible studies). To identify RCTs published after the end of the search used in the most comprehensive systematic review identified, we will run an updated search of MEDLINE, EMBASE, CINAHL, and CDSR from the date of the last comprehensive systematic review.
Data extraction
Following calibration exercises, reviewers, working independently, in duplicate and using a standardized, piloted tested data extraction form, will extract data from included reviews and primary studies. Reviewers will resolve discrepancies by discussion or by adjudication by an expert research methodologist.
From each original study, we will extract information on the study characteristics (population, intervention, comparator, outcomes) and results. For event (dichotomous) data we will extract numbers of events in each study arm at the last reported time point available during the intervention period, and the number of participants included in each arm. For continuous data, we will extract means, standard deviations (or other variance data), and numbers in each arm at the last reported time point during the intervention period. We will also extract planned dietary composition in both study arms, assessed dietary composition in both arms, longest duration of the intervention, whether the intervention consists of dietary advice, advice plus some food provision, or provision of most foods, cointerventions (pharmaceutical and non-pharmaceutical), data on compliance in both arms, and surrogate outcomes including total serum cholesterol and low density lipoprotein (LDL) cholesterol in both arms at the latest available date during the intervention (during the randomized period) [32].
Risk of bias
Following calibration exercises, reviewers, working independently and in duplicate, will assess the RoB of eligible primary studies. Reviewers will resolve discrepancies by discussion or by adjudication by an expert research methodologist.
Systematic reviews often have important limitations related to their assessment of RoB, such as the application of tools that do not address all important sources of bias, tools that include constructs unrelated to RoB (e.g., generalizability), or apply RoB tools inconsistently [33]. Hence, in duplicate we will assess the RoB of primary studies de novo using a modification of the Cochrane risk of bias 1.0 instrument for RCTs [34, 35]. Based on our previous use of the tool, it has been modified in a standardized way in order to make the assessment more manageable and specific to nutrition studies [28]. For instance, our modified Cochrane RoB instrument for RCTs uses more comprehensive instructions for all RoB items with clear definitions and examples for low and high RoB, and uses four response options [36]. In particular, to evaluate sequence generation, allocation concealment and blinding, we will first assess if these items were adequately reported (i.e., clearly reported, mostly reported, mostly not reported, clearly not reported) and second, we will evaluate how serious the RoB is using an index of suspicion (i.e., 1 = definitely low risk, 2 = probably low risk, 3 = probably high risk, 4 = definitely high risk). For example, a study may report “double-blinded” without details as to which of the five possible study team members of an RCT where specifically blinded. For both data analysts and data adjudicators we would answer “clearly not reported” and “probably high risk of bias”. We will also modify the selective outcome reporting item to avoid confounding “outcome reporting bias” with “publication bias”, and use the more comprehensive and specific item for selective reporting used in the Cochrane RoB 2.0 tool [37]. Our team has previously successfully used similar modified instruments for the assessment of RoB for nutrition RCTs [28, 38].
Risk of bias related to missing participant outcome data
Following calibration exercises, reviewers, working independently and in duplicate and using a standardized and piloted tested data extraction form will extract data on missing participant outcome data (MPOD) from included RCTs that address the association between dietary fats and all people-important outcomes. Reviewers will resolve discrepancies by discussion or by adjudication by an expert research methodologist. As needed, we will contact the trialists to ask for available but unreported MPOD in the primary study report.
We will define participant outcome data as ‘‘missing’’ if they are unavailable to the reviewers; that is, unavailable to investigators of the primary studies, or available to the primary study investigators but not included in published reports and not provided after inquiry.
For our primary analysis, we will use a complete-case analysis (sometimes referred to as an available-case analysis) where participants with missing participant outcome data are excluded from both the numerator and denominator when calculating relative and absolute risks. We will subsequently compare the complete-case analysis to a series of sensitivity analysis to explore the impact of missing data on our outcomes and assess the robustness of the effect estimates as suggested using GRADE 17 guidance [26, 27, 29, 39, 40]. To do so, we will assume that the event rate for those participants in the control group who had missing data was the same as the event rate for those participants in the control group who were successfully followed. For the intervention group, we will calculate effects using the following assumed ratios of event rates in those with missing data in comparison to those successfully followed: 1.5:1, 2:1, 3:1, and 5:1 [26].
Data synthesis and analysis
For our review of RCTs, for each dietary fat and health outcome of interest, based on guidance from the Cochrane Handbook we will conduct de novo meta-analyses comparing lower versus higher intake of saturated fats, and saturated fats replaced or modified with polyunsaturated fatty acids (PUFA), monounsaturated fatty acids (MUFA), protein and complex carbohydrates. Replacement trials will be those wherein participants are asked to reduce their fat or SFA, and authors report evidence of significant decrease in SFA with a corresponding increase in other nutrients (e.g., SFA is reduced by ~ 6% of daily calories [energy], while there is an increase in energy from PUFA (e.g., 4%) and/or MUFA (e.g., 2%). Replacement trials, while more robust if they provide known quantities of specific food interventions to participants, may or may not provide the intervention (e.g., nuts, olive oil). Depending the types of trials and intervention arms (reduction; replacement; modification of fat and macronutrients), we may conduct both standard pairwise comparisons and a network meta-analysis.
For each outcome reported in each review, we will present the intervention, comparator, number of studies and participants, the baseline risk, the absolute and relative effects and the corresponding certainty of evidence. We will use data from GLOBOCAN [41] and the Emerging Risk Factors Collaboration [42] to estimate the baseline and absolute risks for major cardiometabolic and cancer outcomes, respectively. Absolute risks for cardiometabolic outcomes will be estimated over 10.8 years, while cancer outcomes will be estimated over a lifetime [41, 42]. Using these baseline risks, we will calculate the absolute risk reductions for our respective outcomes [43]. Since our review will inform a dietary guideline, wherein decision-makers need to consider evidence from all people-important outcome data, we will use a fully contextualized approach and we will categorize the magnitude of effects as trivial, small but important, moderate or large using guidance from GRADE [24, 25] and the Cochrane Collaboration [44]. Using thresholds for the magnitude of importance developed in consultation with an international dietary guideline panel on red and processed meat [22], we will use the following categorization. For fatal outcomes, ≤ 10 events per 1000 will be considered a trivial (unimportant) effect size, 11–25 per 1000 will be considered a small but important effect, and 26–40 per 1000 will be considered moderate. For non-fatal outcomes, ≤ 20 per 1000 will be considered trivial, 21–40 per 1000 will be considered small but important, and 41–60 per 1000 will be considered moderate. For mixed fatal and non-fatal outcomes, ≤ 15 per 1000 will be considered trivial, 16–30 per 1000 will be considered small but important, and 31–45 per 1000 will be considered moderate in size. For continuous patient-reported quality of life measures, will search the literature for anchor-based minimal important difference (MID) estimates, and if no MID is identified we will use half the baseline standard deviation from normative data for the quality of life measure [45,46,47]. As per GRADE guidance, we will present our data in summary of findings tables [43].
We will conduct subgroup analyses or meta-regression, if appropriately powered, with a chi-square test of interaction to assess the following anticipated effect modifiers:
-
i)
We will consider the primary macronutrient replacing the dietary fat under investigation (e.g., replacement of saturated fatty acid (SFA) with PUFA, MUFA, protein or carbohydrates). We anticipate that, for instance, replacing SFA with PUFA or MUFA will reduce the risk of cardiovascular events [32, 48] more than SFA reduction alone, or replacement with CHO or protein.
-
ii)
We will conduct subgroups among RCTs that provide food (e.g., nuts, olive oil, fish) or fat supplementation versus those with dietary advice only, anticipating larger treatment effects in trials that provide food/supplementation interventions [32, 49].
-
iii)
We will explore co-interventions as an effect modifier (e.g., statins, blood pressure lowering agents, exercise, or behavioral support groups), anticipating larger treatment effects in trials that provide active co-interventions [50, 51].
-
iv)
We will use meta-regression to examine the association between the change in low density lipoprotein (LDL) and total cholesterol, surrogates for SFA reduction, and the log relative risk changes for each of our outcomes. We anticipate that participants with lower cholesterol levels will have a lower risk of stroke, myocardial infarction, coronary heart disease, and cardiovascular mortality.
-
v)
Based on a modified version of the Cochrane risk of bias 1.0 instrument [28], we explore if studies at lower RoB have estimates of effect that differ significantly from studies at higher RoB, anticipating that studies at higher risk of bias will have larger treatment effects [52].
We will conduct a number of sensitivity analysis including (a) for primary studies that report on measures of dietary fats from participant-reported dietary intake surveys (i.e., dietary records or recalls, food frequency questionnaires) versus those that report tissue biomarkers (adipose polyunsaturated linoleic acid levels, subcutaneous fat aspirate, plasma fatty acid concentration) with or without participant-reported dietary intake assessments. While the number of established nutritional biomarkers is small, biomarkers may be applied directly in disease association analyses as has been done successfully for dairy fats [53] and alpha linolenic acid [54] based on valid markers for omaga 3 fatty acids [55], and may be used to calibrate self-report assessments to reduce systematic and random measurement error [56]. We will also conduct sensitivity analysis for (b) studies that report results corresponding to intake of dietary fats in absolute quantities (i.e., g/day) and those that report results from energy density models (i.e., % energy).
We will conduct pairwise meta-analyses using Revman 5.0, the meta package [57] and R version 3.5.1 (R Foundation for Statistical Computing).
Evaluation of the certainty of evidence
We will assess the certainty of the evidence using the GRADE fully contextualized approach [24, 25] approach and present results for reducing and replacing/modifying saturated fat separately in a summary of findings table [43].
Discussion
Our systematic review will provide a comprehensive and rigorous summary of the evidence addressing the relationship between dietary saturated and unsaturated fats and important health outcomes, including an estimate of the magnitude of effect, and the certainty of evidence.
This work represents a novel and efficient approach to evidence synthesis in fields in which many evidence syntheses have been previously published on dietary fats and health outcomes. Our systematic reviews will begin by utilizing the search strategies and selection of relevant studies done by existing well conducted systematic literature reviews (e.g., [32]), and subsequently we will search for primary studies from the date of the last systematic review forward.
Implications
Our findings will be used towards the development of dietary guidelines addressing saturated fats and the risk of cardiovascular and cancer outcomes, including recommendations for those at very low, low, and high risk of a cardiovascular event.
Dissemination
We will disseminate our findings by publication in a peer reviewed journal and by presentation at national and international conferences. Based on the findings of our overview, we will make GRADE summary of findings tables, plain language summaries, and infographics in user-friendly and open-access outputs for clinicians and patients and community members.
Strengths and limitations
The strengths of this systematic review will include an extensive search for relevant systematic reviews of RCTs and RCTs; duplicate screening and extraction of data; the assessment of the RoB of studies using rigorous criteria aligned with advances in the methodology of bias assessment [28, 35, 37] including the assessment of the impact of missing participant outcome data on the RoB [27], and the transparent assessment of the magnitude and certainty of estimates for each of our outcomes using GRADE criteria [24, 25]. The GRADE approach to assessing the certainty of estimates is based on comprehensive methodology that has been described in detail in a series of eight BMJ publications and over 30 publications in the Journal of Clinical Epidemiology and has been adopted by over 110 international organizations, including the Cochrane Collaboration, Joanna Briggs Institute and the World Health Organization, each of which regularly apply GRADE to nutritional questions [11, 21]. The application of the GRADE approach will facilitate the consideration of important criteria that bear on the certainty of evidence on the relationship between saturated fats and health outcomes, including RoB, inconsistency, indirectness, imprecision, and publication bias. All this will serve to improve public transparency in making and communicating judgments about the magnitude and certainty of evidence on dietary fat and health outcomes.
Conclusions
Our review will provide a comprehensive and rigorous summary of the evidence addressing the relationship between saturated, polyunsaturated and monounsaturated fats, and important health outcomes, including absolute estimates of the magnitude of effect and the certainty of evidence for these effects. Our findings will be used to establish dietary recommendations on saturated fat consumption, including reduction versus replacement of SFA with PUFA, MUFA, CHO, and protein.
Availability of data and materials
No additional data available.
References
World Health Organization. Global status report on noncommunicable diseases 2014. World Health Organization; 2014. https://apps.who.int/iris/handle/10665/148114. Accessed 12 Mar 2023.
Teicholz N. The scientific report guiding the US dietary guidelines: is it scientific? BMJ. 2015;351: h4962.
Forouhi NG, Krauss RM, Taubes G, Willett W. Dietary fat and cardiometabolic health: evidence, controversies, and consensus for guidance. BMJ. 2018;361: k2139.
US Department of Agriculture, US Department of Health & Human Services. Dietary guidelines for Americans 2015–2020: Skyhorse Publishing Inc.; 2015.
Department of Health and Human Services, Agriculturem USDo. Scientific Report of the 2015 Dietary Guidelines Advisory Committee. 2015.
Herforth A, Arimond M, Alvarez-Sanchez C, Coates J, Christianson K, Muehlhoff E. A global review of food-based dietary guidelines. Adv Nutr. 2019;10(4):590–605.
National Health Services. The Eatwell Guide. UK; 2016. https://www.nhs.uk/live-well/eat-well/food-guidelines-and-food-labels/the-eatwell-guide/. Accessed 12 Mar 2023.
Demasi M. US nutritionists call for dietary guideline limits on saturated fat intake to be lifted. BMJ. 2020;371: m4226.
Astrup A, Magkos F, Bier DM, Brenna JT, de Oliveira Otto MC, Hill JO, et al. Saturated fats and health: a reassessment and proposal for food-based recommendations: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020;76(7):844–57.
Brannon PM, Taylor CL, Coates PM. Use and applications of systematic reviews in public health nutrition. Annu Rev Nutr. 2014;34:401–19.
Johnston BC, Alonso-Coello P, Bala MM, Zeraatkar D, Rabassa M, Valli C, et al. Methods for trustworthy nutritional recommendations NutriRECS (Nutritional Recommendations and accessible Evidence summaries Composed of Systematic reviews): a protocol. BMC Med Res Methodol. 2018;18(1):162.
Zeraatkar D, Johnston BC, Guyatt G. Evidence collection and evaluation for the development of dietary guidelines and public policy on nutrition. Annu Rev Nutr. 2019;39:227–47.
Schwingshackl L, Zähringer J, Beyerbach J, Werner SW, Heseker H, Koletzko B, et al. Total dietary fat intake, fat quality, and health outcomes: a scoping review of systematic reviews of prospective studies. Ann Nutr Metab. 2021;77(1):4–15.
Guyatt GH, Oxman AD, Kunz R, Atkins D, Brozek J, Vist G, et al. GRADE guidelines: 2. Framing the question and deciding on important outcomes. J Clin Epidemiol. 2011;64(4):395–400.
Johnston BC, Guyatt GH. Causal inference, interpreting and communicating results on red and processed meat. Am J Clin Nutr. 2020;111(5):1107–8.
Forrow L, Taylor WC, Arnold RM. Absolutely relative: how research results are summarized can affect treatment decisions. Am J Med. 1992;92(2):121–4.
Naylor CD, Chen E, Strauss B. Measured enthusiasm: does the method of reporting trial results alter perceptions of therapeutic effectiveness? Ann Intern Med. 1992;117(11):916–21.
Tucker G, Metcalfe A, Pearce C, Need AG, Dick IM, Prince RL, et al. The importance of calculating absolute rather than relative fracture risk. Bone. 2007;41(6):937–41.
Zajac JF, Storman D, Swierz MJ, Koperny M, Weglarz P, Staskiewicz W, et al. Are systematic reviews addressing nutrition for cancer prevention trustworthy? A systematic survey of quality and risk of bias. Nutr Rev. 2022;80(6):1558–67.
Zeraatkar D, Bhasin A, Morassut RE, Churchill I, Gupta A, Lawson DO, et al. Characteristics and quality of systematic reviews and meta-analyses of observational nutritional epidemiology: a cross-sectional study. Am J Clin Nutr. 2021;113(6):1578–92.
Vernooij R, Guyatt GH, Zeraatkar D, Han MA, Valli C, El Dib R, Alonso-Coello P, Bala MM, Johnston BC. Reconciling contrasting guideline recommendations on red and processed meat for health outcomes. J Clin Epidemiol. 2021;138:215–8.
Johnston BC, Zeraatkar D, Mi A, Vernooij RWM, Valli C, El Dib R, et al. Unprocessed red meat and processed meat consumption: dietary guideline recommendations from the nutritional recommendations (NutriRECS) consortium. Ann Intern Med. 2019;171(10):756–745.
Guyatt GH, Oxman AD, Vist GE, Kunz R, Falck-Ytter Y, Alonso-Coello P, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6.
Zeng L, Brignardello-Petersen R, Hultcrantz M, Siemieniuk RAC, Santesso N, Traversy G, et al. GRADE guidelines 32: GRADE offers guidance on choosing targets of GRADE certainty of evidence ratings. J Clin Epidemiol. 2021;137:163–75.
Zeng L, Brignardello-Petersen R, Guyatt G. When applying GRADE, how do we decide the target of certainty of evidence rating? Evid Based Ment Health. 2021;24(3):121–3.
Akl EA, Briel M, You JJ, Sun X, Johnston BC, Busse JW, et al. Potential impact on estimated treatment effects of information lost to follow-up in randomised controlled trials (LOST-IT): systematic review. BMJ (Clinical research ed). 2012;344:e2809.
Guyatt GH, Ebrahim S, Alonso-Coello P, Johnston BC, Mathioudakis AG, Briel M, et al. GRADE guidelines 17: assessing the risk of bias associated with missing participant outcome data in a body of evidence. J Clin Epidemiol. 2017;87:14–22.
Zeraatkar D, Johnston BC, Bartoszko J, Cheung K, Bala MM, Valli C, et al. Effect of lower versus higher red meat intake on cardiometabolic and cancer outcomes: a systematic review of randomized trials. Ann Intern Med. 2019;171(10):721–31.
Johnston BC, Guyatt GH. Best (but oft-forgotten) practices: intention-to-treat, treatment adherence, and missing participant outcome data in the nutrition literature. Am J Clin Nutr. 2016;104(5):1197–201.
Schwab U, Reynolds AN, Sallinen T, Rivellese AA, Risérus U. Dietary fat intakes and cardiovascular disease risk in adults with type 2 diabetes: a systematic review and meta-analysis. Eur J Nutr. 2021;60(6):3355–63.
De Souza RJ, Mente A, Maroleanu A, Cozma AI, Ha V, Kishibe T, et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015;351.
Hooper L, Martin N, Jimoh OF, Kirk C, Foster E, Abdelhamid AS. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2020;5(5):Cd011737.
Zeraatkar D, Kohut A, Bhasin A, Morassut RE, Churchill I, Gupta A, et al. Assessments of risk of bias in systematic reviews of observational nutritional epidemiologic studies are often not appropriate or comprehensive: a methodological study. BMJ Nutr Prev Health. 2021;4(2):487–500.
Hartling L, Ospina M, Liang Y, Dryden DM, Hooton N, Krebs Seida J, Klassen TP. Risk of bias versus quality assessment of randomised controlled trials: cross sectional study. BMJ. 2009;19(339): b4012.
da Costa BR, Beckett B, Diaz A, Resta NM, Johnston BC, Egger M, Jüni P, Armijo-Olivo S. Effect of standardized training on the reliability of the Cochrane risk of bias assessment tool: a prospective study. Syst Rev. 2017;6(1):44.
Akl EA, Sun X, Busse JW, Johnston BC, Briel M, Mulla S, et al. Specific instructions for estimating unclearly reported blinding status in randomized trials were reliable and valid. J Clin Epidemiol. 2012;65(3):262–7.
Sterne JAC, Savovic J, Page MJ, Elbers RG, Blencowe NS, Boutron I, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ. 2019;366: l4898.
Ge L, Sadeghirad B, Ball GDC, da Costa BR, Hitchcock CL, Svendrovski A, et al. Comparison of dietary macronutrient patterns of 14 popular named dietary programmes for weight and cardiovascular risk factor reduction in adults: systematic review and network meta-analysis of randomised trials. BMJ. 2020;369:m696. : https://doi.org/10.1136/bmj.m696.
Akl EA, Johnston BC, Alonso-Coello P, Neumann I, Ebrahim S, Briel M, et al. Addressing dichotomous data for participants excluded from trial analysis: a guide for systematic reviewers. PLoS ONE. 2013;8(2): e57132.
White IR, Horton NJ, Carpenter J, Pocock SJ. Strategy for intention to treat analysis in randomised trials with missing outcome data. BMJ. 2011;342: d40.
Ferlay J, Soerjomataram I, Dikshit R, Eser S, Mathers C, Rebelo M, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 2015;136(5):E359–86.
The Emerging Risk Factors C. Diabetes mellitus, fasting blood glucose concentration, and risk of vascular disease: a collaborative meta-analysis of 102 prospective studies. Lancet. 2010;375(9733):2215–22.
Guyatt GH, Oxman AD, Santesso N, Helfand M, Vist G, Kunz R, et al. GRADE guidelines: 12. Preparing summary of findings tables-binary outcomes. J Clin Epidemiol. 2013;66(2):158–72.
Schünemann HJ, Vist GE, Higgins JPT, Santesso N, Deeks JJ, Glasziou P, Akl EA, Guyatt GH. Chapter 15: Interpreting results and drawing conclusions. In: Higgins JPT, Thomas J, Chandler J, Cumpston M, Li T, Page MJ, Welch VA (editors). Cochrane Handbook for Systematic Reviews of Interventions version 6.1 (updated September 2020). Cochrane, 2020. Available from www.training.cochrane.org/handbook.
Carrasco-Labra A, Devji T, Qasim A, Phillips MR, Wang Y, Johnston BC, et al. Minimal important difference estimates for patient-reported outcomes: a systematic survey. J Clin Epidemiol. 2021;133:61–71.
Johnston BC, Ebrahim S, Carrasco-Labra A, Furukawa TA, Patrick DL, Crawford MW, et al. Minimally important difference estimates and methods: a protocol. BMJ Open. 2015;5(10): e007953.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41(5):582–92.
Hooper L, Martin N, Abdelhamid A, Davey Smith G. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database Syst Rev. 2015(6):Cd011737.
Estruch R, Ros E, Salas-Salvado J, Covas MI, Corella D, Aros F, et al. Primary prevention of cardiovascular disease with a mediterranean diet supplemented with extra-virgin olive oil or nuts. N Engl J Med. 2018;378(25): e34.
Karmali KN, Lloyd-Jones DM, Berendsen MA, Goff DC Jr, Sanghavi DM, Brown NC, Korenovska L, Huffman MD. Drugs for primary prevention of atherosclerotic cardiovascular disease: an overview of systematic reviews. JAMA Cardiol. 2016;1(3):341–9. https://doi.org/10.1001/jamacardio.2016.0218.
Posadzki P, Pieper D, Bajpai R, Makaruk H, Könsgen N, Neuhaus AL, Semwal M. Exercise/physical activity and health outcomes: an overview of Cochrane systematic reviews. BMC Public Health. 2020;20(1):1724.
Savovic J, Turner RM, Mawdsley D, Jones HE, Beynon R, Higgins JPT, Sterne JAC. Association between risk-of-bias assessments and results of randomized trials in cochrane reviews: the ROBES Meta-Epidemiologic Study. Am J Epidemiol. 2018;187(5):1113–22.
Naghshi S, Aune D, Beyene J, Mobarak S, Asadi M, Sadeghi O. Dietary intake and biomarkers of alpha linolenic acid and risk of all cause, cardiovascular, and cancer mortality: systematic review and dose-response meta-analysis of cohort studies. BMJ. 2021;375: n2213.
Trieu K, Bhat S, Dai Z, Leander K, Gigante B, Qian F, et al. Biomarkers of dairy fat intake, incident cardiovascular disease, and all-cause mortality: a cohort study, systematic review, and meta-analysis. PLoS Med. 2021;18(9): e1003763.
Serra-Majem L, Nissensohn M, Øverby NC, Fekete K. Dietary methods and biomarkers of omega 3 fatty acids: a systematic review. Br J Nutr. 2012;107(Suppl 2):S64-76.
Prentice RL. Dietary assessment and opportunities to enhance nutritional epidemiology evidence. Ann Intern Med. 2020;172(5):354–5.
Balduzzi S, Rücker G, Schwarzer G. How to perform a meta-analysis with R: a practical tutorial. Evid Based Ment Health. 2019;22(4):153–60.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
BCJ, DZ, MMB, GG, PAC, JS, and LH conceptualized the review. BCJ, DZ, DRFdJ, MC, JS, and LH drafted the manuscript. JS, DRFdJ, HZ, MS, MC, MM, BCR, DS, MJS, NG, YC, YZ, LH, and BCJ drafted screening criteria, data extraction, and risk of bias assessment forms. All authors reviewed the manuscript and approved it for publication.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not needed. The research will be done using published data.
Consent for publication
Not applicable.
Competing interests
As part of his start-up funds at Texas A&M University, BCJ received a grant from Texas A&M AgriLife Research (2019–2020) to fund investigator-initiated research related to saturated and polyunsaturated fats. The grant was from Texas A&M AgriLife institutional funds from interest and investment earnings, not a sponsoring organization, industry, or company. These funds were used to support, in part, an overview of systematic reviews addressing saturated fat and health outcomes (under review). Otherwise, these funds were not used to support any work on this project. DRFdJ was on an exchange program to Texas A&M University supported by the requalification of official or contracted university teaching staff grant (RECUALI21/16) from the University of Basque Country and the Spanish Ministry of Universities, funded by the European Union-Next-Generation EU. LH has received funding (to her institution) from WHO to update a Cochrane systematic review on the effects of reducing saturated fat on cardiovascular disease. These recent WHO funds paid for about 60% of LH’s salary. BCJ, MMB, and PAC are GRADE working group members; GG is the Co-Chair of the GRADE working group. Otherwise, authors claim no other relationships or activities that could appear to have influenced the submitted work.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Johnston, B.C., Zeraatkar, D., Steen, J. et al. Saturated fat and human health: a protocol for a methodologically innovative systematic review and meta-analysis to inform public health nutrition guidelines. Syst Rev 12, 39 (2023). https://doi.org/10.1186/s13643-023-02209-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-023-02209-1