Abstract
Background
Fortification of foodstuffs with iodine, mainly through iodization of salt, which commenced in several African countries after 1995 is the main method for mitigating iodine deficiency in Africa. We assessed the degree of iodine nutrition in pregnancy across Africa before and after the implementation of national iodine fortification programs (CRD42018099434).
Methods
Electronic databases and gray literature were searched for baseline data before implementation of population-based iodine supplementation and for follow-up data up to September 2020. R-metamedian and metamean packages were used to pool country-specific median urinary iodine concentration (UIC) estimates and derived mean UIC from studies with similar features.
Results
Of 54 African countries, 23 had data on iodine nutrition in pregnancy mostly from subnational samples. Data before 1995 showed that severe iodine deficiency was prevalent in pregnancy with a pooled pregnancy median UIC of 28.6 μg/L (95% CI 7.6–49.5). By 2005, five studies revealed a trend towards improvement in iodine nutrition state in pregnancy with a pooled pregnancy median UIC of 174.1 μg/L (95% CI 90.4–257.7). Between 2005 and 2020 increased numbers of national and subnational studies revealed that few African countries had sufficient, while most had mildly inadequate, and some severely inadequate iodine nutrition in pregnancy. The pooled pregnancy median UIC was 145 μg/L (95% CI 126–172).
Conclusion
Improvement in iodine nutrition status in pregnancy following the introduction of fortification of foodstuffs with iodine in Africa is sub-optimal, exposing a large proportion of pregnant women to the risk of iodine deficiency and associated disorders.
Systematic review registration
PROSPERO CRD42018099434
Similar content being viewed by others
Background
Iodine deficiency has a spectrum of consequences that not only affect pregnancy outcomes but also subsequent childhood and maternal health [1,2,3]. Fetal and maternal complications include spontaneous miscarriages, growth restriction, still birth, and maternal postpartum thyroiditis and in cases of severe or persistent iodine deficiency, subclinical and overt hypothyroidism, stunted growth, altered serum lipids, and mental and motor deficits that can affect both mother and child [1,2,3]. The risk of these complications is higher in settings with endemic iodine deficiency like most countries in Africa in the early 1990s before the initiation of iodine fortification. The degree of iodine deficiency deteriorates in pregnancy due to physiological increase in renal iodine filtration and subsequent loss in urine [4, 5]. Even mild to moderate iodine deficiency during pregnancy is associated with psychomotor and cognitive impairment [1].
Before programs encouraging the fortification of salt and other foodstuffs in Africa, it was estimated that only 10% of the population on the African continent had adequate iodine nutrition [6,7,8]. This was attributed to low soil iodine content as well as high thiocyanate levels, one of the major goitrogens on the continent [9]. By 2021, surveys using national or subnational samples of school age children (SAC) yielded median urinary iodine concentration (UIC) consistent with adequate iodine intake in most African countries [10]. Despite this, significant disparity in access to iodized salt still exists in several African countries at community level. This is attributed to insufficient capacity by small-scale salt producers to consistently iodize salt, as well as unfavorable trade policies between countries that preclude the importation of affordable iodized salt from neighboring African countries with large production capacity [11].
Due to variation in dietary habits and iodine metabolism of school age children and pregnant women, the school age children median UIC does not accurately predict the degree of iodine nutrition among pregnant women from the same setting [12, 13]. Of the eleven African countries with data on iodine nutrition in pregnancy, five had insufficient, four adequate, and two more than adequate iodine intake in pregnancy [14].
A daily iodine intake of at least 200 μg, up from the recommended 100–150 μg in non-pregnant women, is necessary to cater for the physiological requirements of pregnancy and compensate for the elevated renal losses [15]. In pregnancy a median UIC of < 150 μg/l reflects insufficient intake while UIC of 150–249 μg/l adequate, 250–499 μg/l more than adequate, and UIC>500 μg/l reflecting excessive iodine intake [16]. In the general population and among women in reproductive age at inception of pregnancy, median IUC of < 20 μg/l, 20–49 μg/l, and 50–99 μg/l reflect severe, moderate, and mild iodine deficiency, respectively [15]. The same values may be used to identify populations with pregnant women at risk of moderate and severe iodine deficiency, and 100–149 μg/l for populations with pregnant women at risk of mild iodine deficiency (Table 1) [17]. It is not certain if the iodine fortification efforts have had a significant and sustainable impact on the iodine nutrition status in pregnancy in Africa [18].
Rationale
We conducted this systematic review and meta-analysis to ascertain the trend in the prevalence of insufficient iodine nutrition status (median UIC <150 μg/L) among pregnant women in Africa following the implementation of national iodization programs and to establish if this has had a positive impact on the iodine nutrition status of pregnant women in Africa.
Methods
The methods of this systematic review and meta-analysis were described in a protocol [19] that was also registered with PROSPERO (CRD42018099434). Observational and intervention studies with data on iodine nutrition status in pregnancy conducted in the various African countries were included in this systematic review. The iodine nutrition status was defined according to the WHO/ICCIDD classification of iodine intake of populations using median urinary iodine concentration [15]. All studies are reported in the English or French, or Portuguese languages and conducted on human subjects were considered. We excluded studies conducted among populations of African origin but residing outside Africa, studies lacking prevalence rates and with the absence of data to compute them, and studies not performed in human participants or published in languages other than English, French, and Portuguese. This systematic review is reported in accordance with the Preferred Reporting Items for Systematic reviews and Meta-Analysis (PRISMA) Guidelines [20].
Search strategy for study identification
Electronic searches
We searched PubMed-MEDLINE, Google Scholar, SCOPUS, ISI Web of Science (Science Citation Index), Africa Wide Information, African Index Medicus (AIM), and AFROLIB databases for published studies on iodine deficiency in pregnancy in Africa up to the 30th of September 2020. This search was conducted using a predefined comprehensive and sensitive search strategy combining relevant terms with names of countries in Africa, to obtain the maximum possible number of studies. This search was guided by the African search filter, which has been reported to have good sensitivity (and improved precision) of 74% (1.3–9.4%) and 73% (5–28%) for MEDLINE and EMBASE, respectively [21]. This search filter included names of each African country and shortened terms to capture studies from regions. Countries with official names in a language other than English were entered in the official form, and for countries that have changed names over time, both names were included in the search. The search strategy can be found in the published protocol for this review [19]. We also searched reference lists of relevant citations for articles of interest.
Grey literature
We also searched for national ministries of health, international organizations such as the WHO, UNICEF, ICCIDD, IGN, other non-government organisations’ reports, conference, and workshop proceedings using Google Scholar search engine, and major relevant websites such as WHO “African Index Medicus and African Journals Online” (AJOL).
Study records
Data management
All identified studies were entered into endnote software for de-duplication of records. Prior to screening of studies, we created standardized questions according to the inclusion criteria which were pre-tested on a sample of eligible studies.
Screening
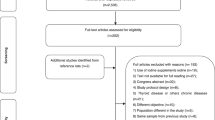
Two investigators (CBB and HM) independently selected studies that meet inclusion criteria. Citations and abstracts were screened for possible inclusion, and duplicate citations were excluded. Titles and abstracts were then screened following the inclusion criteria described above, following which the full texts of potentially eligible articles were obtained. The full texts were then screened using a standardized and pre-tested form to include eligible studies. Disagreements were resolved by consensus, or consultation of a third author (APK). Corresponding authors of potentially eligible studies that did not report the relevant data were contacted. The reasons for exclusion of non-eligible studies were documented. The whole selection process was summarised in a flow chart (Fig. 1).
Data extraction
Two investigators (CBB and HM) independently extracted data from included studies, using a standardized and pre-tested data extraction form. Any inconsistencies or disagreement resolved by consensus or consultation with the third investigator (APK).
Data items
Data including the year, geographic region, and country where the study was conducted, year of publication, study design, setting (rural or urban, health facility or community-based, national or sub-national), sample size, and the criteria used for determination of the iodine intake were extracted. The median (25th–75th percentiles) and or mean (standard deviation) UIC were recorded.
Assessment of methodological quality and risk of bias
Two investigators (CBB and HM) independently scored the quality of included studies. The risk of bias in individual studies was assessed using the Risk of Bias Tool for Prevalence Studies as previously described [19, 22]. Discrepancies were resolved by consensus. The risk of bias and quality scores are presented in Table 2.
Data synthesis, analysis and assessment of heterogeneity
Prevalence data was summarized by country and period of study (Table 2). Median pregnancy IUC were pooled using R meta-median package. Sub-group analysis was carried out according to the time the studies were conducted that is before 1995, between 1995–2004 and 2005–2020 (Fig. 2) In order to check for heterogeneity and publication bias, the mean UIC and standard deviation were derived from the median UIC using the methods described elsewhere [63, 64] (Table 3). The derived means were then pooled using metamean R package and degree of heterogeneity between the included studies and the difference in the mean of subgroups estimated. Publication bias was assessed using a funnel plot and an accompanying linear regression test.
Median urinary iodine concentration (IUC μg/L) of pregnant women for studies conducted before 1995, between 1995–2004 and 2005–2020 (the dashed vertical line shows adequate median UIC during pregnancy; a [b, c] denotes median with IQR, a [±b] denotes mean and standard deviation, and a [b – c] median with the range). NS national survey, ss sub-national survey
Results
Figure 1 shows the PRISMA flow chart of the study selection process. A total of 521 abstracts were identified from the searches. After removing duplicates, the titles and abstracts of 182 articles were screened for eligibility. Of these, 62 full-text articles were accessed and screened out of which 42 studies met the inclusion criteria and were included in the meta-analysis [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62, 65,66,67].
Characteristics of included studies
Out of the 42 studies, two were carried out before 1995, five between 1995 and 2005, and thirty-five between 2006 and 2020. Only eleven of the forty-two studies had data derived from national representative samples. The internal and external validity of the included studies were determined using a 9-point score (Table 2). Most of the studies (37/42) had a low risk of bias with the rest having intermediate risk (Table 2).
The prevalence of insufficient iodine intake (UIC <150 μg/L) among pregnant women on the various African countries before 1995, 1995–2005, and 2006–2020
Before 1995, available data from two studies revealed moderate countrywide iodine deficiency in pregnancy in the Democratic Republic of Congo at the time and severe iodine deficiency in pregnancy in a subnational sample from North-Eastern Algeria [23, 24]. The pooled median UIC across the two studies was 28.6 μg/L (95% CI 7.6–49.5), with considerable heterogeneity (I2 99.73 %, p < 0.001, Fig. 2).
Between 1995 and 2005, four subnational studies from Ivory coast, Nigeria Sudan, and Senegal, and one national survey from Swaziland [25,26,27,28,29] yielded a pooled pregnancy UIC of 174.1 μg/L (95% CI 90.4–257.7, Fig. 2), with considerable heterogeneity (I2 99.96 %, p < 0.001).
Between 2005 and 2020, 35 studies from 18 countries had pregnancy median UIC data. Eleven of the studies were national surveys from 10 countries. These national surveys revealed more than adequate intake in Djibouti and Somalia [34, 65]; adequate iodine intake in Ghana, Sierra Leone, and Tanzania [46, 58, 61]; mild inadequate intake in Egypt, Gambia, and Tanzania [35, 60], and moderate insufficient iodine intake in Burkina Faso, Burundi, and Madagascar [31, 32, 50]. The remaining studies [30, 33, 36,37,38,39,40,41,42,43,44, 47,48,49, 51,52,53,54,55,56,57, 59, 62, 66, 67] were subnational studies. The pooled median pMUIC across the 35 studies conducted between 2005 and 2020 was 145 μg/L (95% CI 126–172), with substantial heterogeneity (I2 99.81%, p < 0.001) (Fig. 2). There was a significant increase in pregnancy median UIC between 1995 and 2020 compared to the period before 1995 (Kendaull’s tau correlation co-efficient 0.270, p = 0.032).
Derived mean UIC by time-period
The pooled derived mean pregnancy UIC (Table 2, Fig. 3) was 27.96 μg/L (95% CI 11.6–67.04, tau 0.630) before 1995; 143.22 μg/L (95% CI 108.65–188.78, tau 0.362) between 1995 and 2005; and 127.99 μg/L (95% CI 108.59–150.85, tau 0.493), with significant difference across time-period (Q = 12.24, d.f. = 2, p = 0.002).
Assessment of publication bias
Publication bias was assessed using funnel plots. The funnel plot for the studies in the period 1995–2004 was not suggestive of potential publication bias (Fig. 4) (R metabias linear regression test t = −0.36005, p value = 0.7335). No additional studies were imputed after checking for funnel asymmetry using the Twedie and Duval’s trim and fill test. The funnel plot for the studies carried out between 2005 and 2020 was asymmetrical (Fig. 5). The trim and fill test imputed sixteen potential missing studies suggesting potential publication bias (Fig. 6). The funnel plot asymmetry was confirmed by the R metabias linear regression test (t = 3.872, p < 0.001).
Discussion
This review found that pregnant women in Africa had moderate to severe iodine deficiency before the implementation of iodine supplementation in 1995. Mild to moderate iodine deficiency in pregnancy was still prevalent in several regions of various African countries by 2005, the year designated for elimination of iodine deficiency globally. However, there was significant improvement in the iodine nutrition status in pregnancy in Africa between 2005 and 2020 compared to the period before 1995 although this is still insufficient (median pMUIC < 150 μg/L). Overall, there is paucity of nationwide representative data on iodine nutrition status in pregnancy in Africa. In order to ensure successful elimination of iodine deficiency disorders, the World Health Organization recommends regular monitoring of iodine nutrition status at national level as well as for high-risk populations such as pregnant women, lactating mothers, and children 7–24 months of age [15]. Pregnancy median UIC data was available for about 50% of the African countries with most derived from sub-national samples. This can be overcome by including the assessment of the iodine nutrition status in the national demographic health surveys.
The limited available data before 1995 showed that some African countries had moderate to severe regional or nationwide iodine deficiency in pregnancy [23, 24]. This may reflect the continental iodine nutritional status in pregnancy at that time since only about 10% of the general population in Africa had adequate iodine nutrition before 1995 [6]. Protracted iodine deficiency predisposes to severe thyroid hyper-stimulation, which together with the prevalent dietary thiocyanates and nitrates in several African countries leads to inflammation, infiltration by immune cells, and oxidative damage to thyroid parenchyma and necrosis [68]. This is exacerbated by the increased loss of iodine through urine during pregnancy, which could account for the disproportionately higher rates of thyroid diseases among women [4, 7].
Following the initiation of iodine fortification of foodstuffs in most countries in 1995 and thereafter, the World Health Organization (WHO) earmarked the 2005 as the year for elimination of iodine deficiency globally [15]. Although the current study found a pooled UIC of 174.1μg/L from eligible studies conducted between 1995 and 2005, which is suggestive of sufficient iodine intake during pregnancy, the number of studies was small and therefore not representative of all the pregnant women in Africa during this period. The studies also revealed that in several countries, there were areas with optimum and others with insufficient iodine nutrition status in pregnancy. This demonstrates lack of equity in implementation of iodine deficiency mitigating strategies within individual countries. This could partly have been due to the dependence on median school age UIC (SAC UIC) as a surrogate measure of national iodine nutrition status. Median SAC UIC does not to accurately estimate iodine nutrition state in pregnancy [11, 69]. Hence, in areas with marginally sufficient iodine intake as estimated using median SAC UIC, pregnant women and their unborn babies may still be at high risk of iodine deficiency. However, the level of iodine insufficiency as revealed in studies conducted between 1995 and 2005 was marginal compared to countries with data before 1995 implying a significant positive impact of iodine fortification on the degree of iodine deficiency in pregnancy in Africa.
Between 2005 and 2020, an increased number of national and sub-national surveys were conducted to assess the iodine nutrition status in pregnancy in several African countries. Some regions within individual countries had sufficient while others had various degrees of insufficient iodine intake in pregnancy more than 20 years after implementation of iodine fortification. Some of these subnational surveys revealed a pregnancy median UIC marginally above the sufficient level. This implies that large proportions of pregnant women may still be at risk of iodine deficiency and its attendant adverse effects. This calls for establishment and strengthening of iodine nutritional status monitoring mechanisms through collaborative efforts of national health departments as well as health related local and international non-governmental organizations. Populations still at risk of moderate to severe iodine deficiency would benefit from iodine supplementation such an annual dose of iodized oil until iodine deficiency is eliminated through equitable access to adequately iodized salt and other national food fortification programs [15]. Further research and innovative strategies to overcome barriers to equitable access of iodised salt such as parallel distribution and use of non-iodized salt in the food industry need further consideration.
Strengths and limitations
To our knowledge, this is first systematic review aiming at assessing the level of iodine deficiency among pregnant women in Africa from the time of initiation of iodine supplementation to September 2020. This review was limited by the small number of studies before 1995 and by the subnational nature of the majority of studies conducted after 1995 most of which were from small geographical locations within the African countries hence not representative of national populations.
Conclusion
There is still paucity of data on iodine nutrition status in pregnancy from half of the countries in Africa. The available data shows a significant but inadequate improvement in the iodine nutrition status of pregnant women in several African countries after 1995. A few countries still have moderate to severe iodine deficiency in pregnancy at national or regional more than two decades after implementation of iodine food fortification. The inclusion of iodine nutrition assessment in national demographic surveys will help identify populations and geographical locations that may need iodine supplementation as well as regularly monitor the effectiveness of national iodization programs. Legal frameworks and trade policies that regulate the production and trade in iodized salt within and between countries need to be reviewed so as to foster a sustainable production and supply of adequately iodized salt at community level.
Abbreviations
- ICCIDD:
-
International Council for Control of Iodine Deficiency Disorders
- IGN:
-
Iodine Global Network
- PRISMA-P:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols
- pMUIC:
-
Pregnancy median urinary iodine concentration
- SAC:
-
School age children
- STROBE:
-
Strengthening the Reporting of Observational Studies in Epidemiology
- UIC:
-
Urine iodine excretion
- WHO:
-
World Health Organization
- UNICEF:
-
United Nations Children’s Education Fund
- UIC:
-
Urinary iodine concentration
- USI:
-
Universal salt iodization
References
Zimmermann MB. The importance of adequate iodine during pregnancy and infancy. World Rev Nutr Diet. 2016;115:118–24.
Zantour B, Alaya W, Marmouch H, et al. Hypothyroidism in pregnancy. In: Potluková E, editor. Current topics in hypothyroidism with focus on development. Rijeka: In Tech; 2013. p. 29–62.
Lazarus HJ. Ch 14: thyroid regulation and dysfunction in the pregnant patient. [Online]. 2016. Available: http://www.thyroidmanager.org/wp-content/uploads/chapters/thyroid-regulation-and-dysfunction-in-the-pregnant-patient.pdf.
Leung AM, Pearce EN, Braverman EL. Iodine nutrition in pregnancy and lactation. Endocrinol Metab Clin North Am. 2011;40(4):765–77.
Cheung KL, Lafayette RA. Renal physiology of pregnancy. Adv Chronic Kidney Dis. 2013;20(3):209–14.
Joy EJM, Ander EL, Young SD, et al. Dietary mineral supplies in Africa. Physiol Plant. 2014;151:208–29.
Tsegaye B, Ergete W. Histopathologic pattern of thyroid disease. East Afr Med. 2003;80(10):525–8.
Kishosha PA, Galukande M, Gakwaya AM. Selenium deficiency a factor in endemic goiter persistence in sub-Saharan Africa. World J Surg. 2011;35(7):1540–5.
Taga I, Oumbe VAS, Johns R, et al. Youth of west-Cameroon are at high risk of developing IDD due to low dietary iodine and high dietary thiocyanate. Afr Health Sci. 2008;8(3):180–5.
Iodine Global Network (IGN). Global scorecard of iodine nutrition in 2020 in the general population based on school-age children (SAC). Ottawa: IGN; 2021.
Yusufali R, Matlhafuna T. Universal salt iodisation in Africa: road to overcoming the last hurdles. 2005. https://www.nutritionintl.org/content/user_files/2017/06/Universal-Salt-Iodization-In-Africa-Road-toovercoming-the-last-hurdles.pdf.
Gowachirapant S, Winichagoon P, Wyss L, et al. Urinary iodine concentrations indicate iodine deficiency in pregnant Thai women but iodine sufficiency in their school-aged children. J Nutr. 2009;139:1169–72.
Ittermann T, Albrecht D, Arohonka P, Bilek R, de Castro JJ, Dahl L, et al. Standardized map of iodine status in Europe. Thyroid. 2020;30(9):1346–54.
Iodine Global Network (IGN). Global scorecard of iodine nutrition in 2017 in the general population and in pregnant women (PW). Zurich: IGN; 2017.
WHO (World Health Organization). Assessment of iodine deficiency disorders and monitoring their elimination. A guide for programme managers. Geneva: World Health Organization; 2007.
WHO (World Health Organization). Proceedings of the WHO Technical Consultation on control of iodine deficiency in pregnant women and young children. Geneva: World Health Organization; 2005.
Skeaff SA. Iodine deficiency in pregnancy: the effect on neurodevelopment in the child. Nutrients. 2011;3:265–73.
Harika R, Faber M, Samuel F, Kimiywe J, Mulugeta A, Eilander A. Micronutrient status and dietary intake of iron, vitamin A, iodine, folate and zinc in women of reproductive age and pregnant women in Ethiopia, Kenya, Nigeria and South Africa: a systematic review of data from 2005 to 2015. Nutrients. 2017;2017. https://doi.org/10.3390/nu9101096.
Businge CB, Longo-Mbenza B, Kengne AP. The prevalence of insufficient iodine intake in pregnancy in Africa: protocol for a systematic review and meta-analysis. Syst Rev. 2019;8(209). https://doi.org/10.1186/s13643-019-1092-7.
Moher D, Liberati A, Tetzlaff J, Altman DG, the PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. Ann Intern Med. 2009;151:264–9.
Pienaar E, Grobler L, Busgeeth K, Eisinga A, Siegfried N. Developing a geographic search filter to identify randomised controlled trials in Africa: finding the optimal balance between sensitivity and precision. Health Inf Libr J. 2011;28:210–5.
Hoy D, Brooks P, Woolf A, Blyth F, March L, Bain C, et al. Assessing risk of bias in prevalence studies: modification of an existing tool and evidence of interrater agreement. J Clin Epidemiol. 2012;65:934–9.
Chaouki ML, Benmiloud M. Prevention of iodine deficiency disorders by oral administration of lipiodol during pregnancy. Eur J Endocrinol. 1994;130(6):547–51.
Ngo DB, Dikassa L, Okitolonda W, Kashala TD, Gervy C, Dumont J, et al. Selenium status in pregnant women of a rural population (Zaire) in relationship to iodine deficiency. Trop Med Int Health. 1997;2(6):572–81. https://doi.org/10.1046/j.1365-3156.1997.d01-326.x.
Hess SY, Zimmermann MB, Staubli-Asobayire F, Tebi A, Hurrell RF. An evaluation of salt intake and iodine nutrition in a rural and urban area of the Cote d'Ivoire. Eur J Clin Nutr. 1999;53(9):680–6. https://doi.org/10.1038/sj.ejcn.1600818.
Ojule AC, Osotimehin BO. Maternal and neonatal thyroid status in Saki, Nigeria. Afr J Med Med Sci. 1998;27(1-2):57–61.
Dillon JC, Milliez J. Reproductive failure in women living in iodine deficient areas of West Africa. BJOG. 2000;107:631–6.
Eltom A, Eltom M, Elnagar B, Elbagir M, Gebre-Medhin M. Changes in iodine metabolism during late pregnancy and lactation: a longitudinal study among Sudanese women. Eur J Clin Nutr. 2000;54:429–33.
Lwenje SM, Mtetwa VSB, Ginindza S. Assessment of iodine deficiency in pregnant women in Swaziland. UNISWA Res J Agric Sci Technol. 2000;4(2):119–23.
Akdader-Oudahmanea S, Hamouli-Saida Z, Zimmermann MB, et al. High prevalence of TPO-Abs and subclinical hypothyroidism in iodine sufficient pregnant women in Northern Algeria. J Trace Elem Med Biol. 2020. https://doi.org/10.1016/j.jtemb.2020.126533.
Garnier D, Kabore S, Kargougou R, et al. Iodine status of women of reproductive age and school-age children in Burkina Faso and its association with adequately iodized household salt – results from a national survey. In: Micronutrient forum global conference, Cancun, Mexico; 2016.
Kavishe FP, Ndombi I, Tom C, Mwai JM, Gorstein J. Sustainable prevention and control of iodine deficiency disorders in Eastern and Southern Africa held at Sarova Whitesands Hotel 5-7 November 2019, Mombasa, Kenya. Seattle: IGN; 2020.
Habimana L, Twite KE, Wallemacq P, et al. Iodine and iron status of pregnant women in Lubumbashi, Democratic Republic of Congo. Public Health Nutr. 2013;16(8):1362–70.
Iodine Global Network (IGN). Iodine-rich groundwater, and not iodized salt, provides children and pregnant women in Djibouti with sufficient iodine: IGN; 2017. www.ign.org › djibouti_1
Ministry of Health and Population (Egypt) (MOHP), UNICEF. Egypt iodine survey 2014 / 2015 summary report. Cairo: MOHP; 2017.
Hamza R, Youssef A, Mouharam W, El Danasoury A. Maternal and neonatal iodine nutrition in Cairo. Internet J Pediatr Neonatol. 2007;8(2):1–6.
Elsayed NA, Abdel-Mohsen S, Mohktar SA, Tayel DI. Almost all pregnant women in Alexandria are iodine sufficient. IDD Newsl. 2016; www.ign.org.
Mohammed H, Marquis GS, Aboud F, Bougma K, Samuel A. Pre-pregnancy iodized salt improved children’s cognitive development in randomized trial in Ethiopia. Matern Child Nutr. 2020:e12943. https://doi.org/10.1111/mcn.12943.
Fereja M, Gebremedhin S, Gebreegziabher T, Girma M, Stoecker BJ. Prevalence of iodine deficiency and associated factors among pregnant women in Ada district, Oromia region, Ethiopia: a cross-sectional study. BMC Pregnancy Childbirth. 2018;18. https://doi.org/10.1186/s12884-018-1905-z.
Kedir H, Berhane Y, Worku A. Subclinical iodine deficiency among pregnant women in Haramaya District, Eastern Ethiopia: a community-based study. J Nutr Metab. 2014:878926. https://doi.org/10.1155/2014/878926.
Ersino G, Tadele H, Bogale A, Abuye C, Stoecker BJ. Clinical assessment of goitre and low urinary iodine concentration depict presence of severe iodine deficiency in pregnant Ethiopian women: a cross-sectional study in rural Sidama, Southern Ethiopia. Ethiop Med J. 2013;51(2):133–41.
Takele WW, Alemayehu M, Derso T, Tariku A. Two-thirds of pregnant women attending antenatal care clinic at the University of Gondar Hospital are found with subclinical iodine deficiency. BMC Res Notes. 2017;11:738. https://doi.org/10.1186/s13104-018-3829-0.
Keno T, Ahrens C, Lauvai J, Kurabachewc H, Biesalski HK, Scherbauma V. Iodine status in pregnant women and school children of the Aira district in Ethiopia. NFS J. 2017;7(2017):1–7.
Negeri Z, Gobena T, Rajesh PN, Kassim M. Determining the magnitude of iodine deficiency and its associated risk factors among pregnant women visiting Jimma University Specialized Hospital for Antenatal Care. World J Med Med Sci. 2014;2(4):1–16.
National Nutrition Agency (NaNA)-Gambia, UNICEF, Gambia Bureau of Statistics (GBOS), GroundWork. Gambia national micronutrient survey 2018. Banjul: NaNA-Gambia; 2019.
Ghana Health Service (GHS). National iodine survey report, Ghana 2015. Accra: GHS; 2017.
Gyamfi D, Wiafe YA, Danquah KO, Adankwah E, Amissah GA, Odame A. Urinary iodine concentration and thyroid volume of pregnant women attending antenatal care in two selected hospitals in Ashanti Region, Ghana: a comparative cross-sectional study. BMC Pregnancy Childbirth. 2018;18. https://doi.org/10.1186/s12884-018-1820-3.
Adu-Afarwuah S, Young RT, Lartey A, Okronipa H, et al. Supplementation during pregnancy with small-quantity lipid-based nutrient supplements or multiple micronutrients, compared with iron and folic acid, increases women's urinary iodine concentration in semi urban Ghana: a randomized controlled trial. Matern Child Nutr. 2018;14(2). https://doi.org/10.1111/mcn.12570.
Farebrother J, Zimmermann MB, Abdallah F, et al. Effect of excess iodine intake from iodized salt and/or groundwater iodine on thyroid function in non-pregnant and pregnant women, infants, and children: a multicenter study in East Africa. Thyroid. 2018;28(9):1198–210.
Randremanana RV, Bastaraud A, Rabarijaona LP, et al. First national iodine survey in Madagascar demonstrates iodine deficiency. Matern Child Nutr. 2019;15:e12717. https://doi.org/10.1111/mcn.12717.
Stinca S, Andersson M, Herter-Aeberli I, et al. Moderate-to-severe iodine deficiency in the “first 1000 days” causes more thyroid hypofunction in infants than in pregnant or lactating women. J Nutr. 2017;147(4):589–95.
Stinca S, Andersson M, Weibel S, et al. Dried blood spot thyroglobulin as a biomarker of iodine status in pregnant women. J Clin Endocrinol Metab. 2017;102(1):23–32.
Sadou H, Seyfoulaye A, Alma MM, Daouda H. Inadequate status of iodine nutrition among pregnant women residing in three districts of Niamey, the Niger Republic’s capital. Matern Child Nutr. 2013;10(4):650–6.
Hess SY, Ouedraogo CT, Young RR, Bamba IF, Stinca S, Zimmermann MB, et al. Urinary iodine concentration identifies pregnant women as iodine deficient yet school-aged children as iodine sufficient in rural Niger. Public Health Nutr. 2017;20(7):1154–61.
Jibril ME, Abbiyesuku FM, Aliyu SI, et al. Nutritional iodine status of pregnant women in Zaria, North-Western Nigeria. Sub-Saharan Afr J Med. 2016;3:41–4.
Kayode OO, Odeniyi IA, Olopade OB, Iwuala SO, Odukoya OO, Fasanmade OA. Iodine status in pregnant Nigerian women; does gestational age matters? J Clin Sci. 2019;16:20–5.
Ujowundu CO, Ukoha AI, Agha CN, Nwachukwu N, Igwe KO. Assessment of current iodine status of pregnant women in a suburban area of Imo State Nigeria, twelve years after universal salt iodization. Afr J Biochem Res. 2010;4(1):06–012.
Rohner F, Wirth JP, Woodruff BA, et al. Iodine status of women of reproductive age in Sierra Leone and its association with household coverage with adequately iodized salt. Nutrients. 2016;8(2). https://doi.org/10.3390/nu8020074.
Mabasa E, Mabapa NS, Jooste PL, Mbhenyane XG. Iodine status of pregnant women and children age 6 to 12 years feeding from the same food basket in Mopani district, Limpopo province, South Africa. South Afr J Clin Nutr. 2019;32(3):76–82.
Mtumwa AH, Ntwenya JE, Paul E, Huang M, Vuai S. Socio-economic and spatial correlates of subclinical iodine deficiency among pregnant women age 15–49 years in Tanzania. BMC Nutr. 2017;3:47. https://doi.org/10.1186/s40795-017-0163-1.
Ba DM, Ssentongo P, Na M, Kjerulff KH, et al. Factors associated with urinary iodine concentration among women of reproductive age, 20–49 years old, in tanzania: a population-based cross-sectional study. Nutr Epidemiol Public Health. 2020; https://academic.oup.com/cdn/article/4/5/nzaa079/5826812.
Chinyanga EA, Cuidede O, Machisvo A, Choga T, Maeaba L, Sibanda N. Urinary iodine excretion in pregnant women as an index of the impact of a national iodization programme. Cent Afr J Med. 2006;52(7/8):78–83.
Luo D, Wan X, Liu J, Tong T. Optimally estimating the sample mean from the sample size, median, mid-range and/or mid-quartile range. Stat Methods Med Res. 2018;27:1785–805.
Shi J, Luo D, Weng H, Zeng X, Lin L, Chu H, et al. Optimally estimating the sample standard deviation from the five-number summary. Res Synth Methods. 2020;11:641–54.
Ministry of Health FGS, FMS, Somaliland, UNICEF, Brandpro, GroundWork. Somalia micronutrient survey 2019. Mogadishu: MOH-FGS; 2020.
Kassim IAR, Moloney G, Busili A, et al. Iodine intake in Somalia is excessive and associated with the source of household drinking water. J Nutr. 2014;144(3):375–81.
Olife IC, Okaka AN, Dioka CE, Meludu SC, Orisakwe OE. Iodine status and the effect of soil erosion on trace elements in Nanka and Oba towns of Anambra State, Nigeria. Ann Chim. 2007;97(9):895–903.
Contempre B, Morreale de Escobar G, Denef JF, Dumont JE, Many MC. Thiocyanate induces cell necrosis and fibrosis in selenium- and iodine-deficient rat thyroids: a potential experimental model for myxoedematous endemic cretinism in central Africa. Endocrinol. 2004;145:99–102.
Andersson M, Karumbunathan V, Zimmermann MB. Global iodine status in 2011 and trends over the past decade. J Nutr. 2012;142(4):744–50.
Acknowledgements
Not applicable.
Funding
This study is part of a research project supported by the Discovery Foundation Rural Fellowship Grant number 038372. APK is employed by the South African Medical Research Council. The sponsors have no role in designing and conducting of this study.
Author information
Authors and Affiliations
Contributions
CBB and APK conceived and designed the study. CBB searched for the studies to be included in the systematic review. CBB and HM screened the abstracts, extracted the data, and assessed the quality of the included studies. CBB carried out the data analysis and wrote the first manuscript. APK, HM, and LMB took part in critical review of the manuscript. CBB is the guarantor of this review. The authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The current study is based on published data and hence does not require ethical approval. This review is part of a thesis that will be submitted to the Faculty of Health Sciences, University of Cape Town, for the award of a PhD in Medicine whose protocol was granted ethics approval by the University of Cape Town Human Research Ethics committee—IRB0001938 (UCT HREC REF:135/2018).
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Businge, C.B., Musarurwa, H.T., Longo-Mbenza, B. et al. The prevalence of insufficient iodine intake in pregnancy in Africa: a systematic review and meta-analysis. Syst Rev 11, 231 (2022). https://doi.org/10.1186/s13643-022-02072-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-022-02072-6