Abstract
Background
Postoperative pain after a cesarean section has negative consequences for the mother during the postoperative period. Over the years, various postoperative pain management strategies have been used following cesarean section. Opioid-based analgesics and landmark approaches have negative side effects, while ultrasound-based regional analgesia necessitates resources and experience, but various wound infiltration adjuvants are innovative with few side effects and are simple to use. The efficacy and safety of each adjuvant, however, are unknown and require further investigation.
Objective
This network meta-analysis is intended to provide the most effective wound infiltration drugs for postoperative management after cesarean section.
Method
A comprehensive search will be conducted in PubMed/MEDLINE, Cochrane Library, Science Direct, CINHAL, and LILACS without date and language restrictions. All randomized trials comparing the effectiveness of wound infiltration drugs for postoperative pain management after cesarean section will be included. Data extraction will be conducted independently by two authors. The quality of studies will be evaluated using the Cochrane risk of bias tool, and the overall quality of the evidence will be determined by GRADEpro software.
Discussion
The rate of postoperative acute and chronic pain is very high which has a huge impact on the mother, family, healthcare practitioners, and healthcare delivery. It is a basic human right to give every patient with postoperative pain treatment that is realistic in terms of resources, technique, cost, and adverse event profile.
Systematic review registration
PROSPERO CRD42021268774
Similar content being viewed by others
Introduction
Description of the condition
Cesarean section rates have increased globally over the last three decades, particularly in developed countries [1,2,3,4,5]. According to a World Health Organization report, more than 18 million cesarean sections are performed worldwide each year [4]. However, over 6 million cesarean sections were performed unnecessarily, primarily in the middle- and high-income countries, with China and Brazil accounting for half of all unnecessary cesarean sections, which is higher than the recommended cesarean section rates for a country [1, 3, 4].
The increase in the global trend of the cesarean section presents a significant challenge to postoperative pain management globally [6]. Different postoperative pain management modalities have been employed over the years after cesarean section. However, none of them is with postoperative adverse events to the mother. Systemic opioid and non-opioid medications, regional blocks, and local wound infiltration of various local anesthetics and other drugs are among the most commonly used postoperative pain treatment strategies [7,8,9,10,11,12,13,14,15,16,17,18,19,20].
Evidence revealed that individual pain variability is highly influenced by different factors such as pain sensitivity, gender, age, heredity, preoperative anxiety, preoperative pain, history of depressive symptoms, and history of substance use [6, 21,22,23,24,25,26,27].
Despite advances in the understanding of the pathophysiology of postoperative pain and the introduction of various postoperative analgesic drugs and modalities, the prevalence of postoperative pain after cesarean section remains high, ranging from 25.5 to 80% [6, 21, 22, 25, 26, 28, 29].
Postoperative pain after a cesarean section has an unfavorable impact on ambulation, breastfeeding, and maternal attachment to their newborn [30]. Furthermore, poorly managed acute postoperative pain is linked to a variety of consequences, including postpartum depression, myocardial infarction, pulmonary infection, decreased gastric motility, nausea, vomiting, impaired immune function, and impaired wound healing [21, 26, 27].
Description of the intervention
Postoperative wound infiltration techniques after cesarean have been employed due to their convenience of use and feasibility in terms of cost-effectiveness, administration processes, and adverse effects. The commonly used approach was wound infiltration with local anesthetics alone or coupled with adjuvants [8, 13, 17,18,19, 31,32,33,34,35,36,37,38,39,40,41,42]. However, recent studies comparing local anesthetics with glucocorticoids, opioids [16, 20, 36, 43,44,45,46], ketamine [14, 32, 34, 47,48,49,50], nonsteroidal anti-inflammatory agents [51], alpha 2 agonists [8, 52], and magnesium sulphate [37, 53, 54] are emerging.
How the intervention might work
Enhanced recovery after caesarean section recommends multimodal analgesics with minimum side effects, various sites of action, and opioid sparing analgesia as much as feasible for postoperative pain management after caesarean Sect. [55, 56]. In this regard, a number of techniques and drugs have been employed over the years for postoperative pain management after a cesarean section including epidural analgesia, Transvers abdominis plan block, Illioinguinal and Illiohypogastric nerve block, quadratus lumborum block, and abdominal wound infiltration with different drugs [7, 10, 57, 58]. This network meta-analysis, however, aims to investigate the efficacy and safety of several wound infiltration medications for postoperative pain relief following a cesarean section. Local anesthetics are known to be injected into localized wounds where they block the sodium channel to stop the propagation of action potentials and pain perception [59,60,61]. Despite disagreements regarding their effectiveness, various medications like ketamine, dexamethasone, week opioids, selective alpha 2 agonists, and magnesium sulphate are used alone or as adjuvants to local anesthetics. Although the exact mechanism by which each medication reduces pain is unknown, it is believed to be accomplished through inhibiting neuronal transmission, inflammatory mediators, and N-methyl-d-aspartate (NMDA) receptors [38, 62,63,64,65,66,67,68,69,70].
Why is it important to do this review?
Evidence revealed that the rate of a cesarean section is steadily increasing globally. The magnitude of postoperative pain following cesarean delivery is relatively high, posing a significant challenge to health care providers. Inadequate postoperative care after a cesarean section can lead to deep venous thrombosis, delayed breastfeeding, paralytic ileus, postpartum depression, lung infection, delayed wound healing, longer hospital stays, persistent discomfort, and greater health care expenses. As a result, various postoperative pain management strategies have been used following a cesarean section. Opioid-based analgesics and landmark approaches, on the other hand, have undesirable consequences; regional analgesia with ultrasonography demands resources and experience, whereas wound infiltration treatments are innovative procedures with few side effects and are simple to apply. However, the efficacy and safety of each adjuvant are uncertain and need further investigation with a network meta-analysis.
Methods
Protocol and registration
This network meta-analysis will be conducted based on the Preferred Reporting Items for Systematic and Meta-analysis protocol (PRISMA-P) [71]. The network meta-analysis protocol was registered in PROSPERO CRD42021268774 on August 19, 2021.
Eligibility criteria
Types of studies
All randomized controlled trials assessing the efficacy and safety of wound infiltration with ketamine, opioids, alpha 2 agonist, magnesium, steroids, and local anesthetics for postoperative pain management following a cesarean section will be considered. However, observational studies comparing wound infiltration to placebo and other medications must be excluded since they are done in the heterogeneous groups of patients with diverse confounders, which may buffer the effect size of this network meta-analysis. Besides, a comparison of local anesthesia with regional block will be excluded.
Types of participants
The American Society of Anesthesiologists physical status classifications (ASA) I and II, term pregnancy, age greater than 18 years scheduled for a cesarean section under spinal anesthesia, will be included, while the rest will be excluded. The inclusion and exclusion criteria were defined by each primary included study.
Types of intervention
The treatment group will be parturient allocated to one of the wound infiltration drugs which were as per the included studies, while the parturient allocated to the comparator defined by each included study will be considered as controlled groups.
Outcome measures
The primary outcomes of this network meta-analysis protocol will be postoperative pain severity, first analgesic request, total morphine equivalent analgesic consumption, and patient satisfaction, while secondary outcomes will be postoperative nausea and vomiting, sedation, hallucination, dizziness, bleeding, hypotension, hypertension, bruising, infection, and mortality.
Search strategy
The goal of the search strategy is to find all published and unpublished randomized controlled trials comparing wound infiltration modalities for postoperative pain management after a cesarean section among parturient undergoing a cesarean section under spinal or general anesthesia, regardless of language or date restrictions.
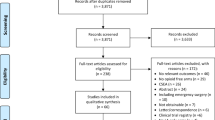
A comprehensive initial search of PubMed/MEDLINE, Cochrane Library, Science Direct, and Latin American and Caribbean Health Sciences Literature (LILACS) will be conducted, followed by an analysis of the text words found in the title/abstract and indexed keywords. A second search will be performed by combining free text words with indexed phrases using Boolean operators. In addition, the third search might be conducted utilizing the reference lists of all papers and publications. Finally, a gray literature search will be conducted using the Google Scholar. EndNote reference manager could be used to remove the duplicates. The remainder will then be considered for inclusion in the systematic review using the PICO technique, which will be carried out in various databases depending on database-specific criteria Mesh terms OR cesarean section OR C-section OR Cesarean delivery AND local anesthetics OR bupivacaine OR Levobupivacaine OR Marcaine OR Lidocaine OR Opioids OR tramadol OR pethidine OR ketamine OR dexamethasone OR steroid OR Glucocorticoid OR Dexmedetomidine OR clonidine OR α2 agonist AND wound infiltration OR subcutaneous infiltration OR abdominal infiltration AND Normal saline OR placebo AND postoperative pain OR analgesia OR toxicity OR adverse effects OR RCT. The detailed search strategies are presented as supplementary material (Supplemental Table 1). The results of the search strategy will be summarized with a Prisma flow chart [72].
Data extraction
Two independent reviewers will retrieve the data using a customized Microsoft Excel 2013 format, and the differences between the two independent reviewers will be settled by the other two reviewers. Names of authors, country, year of publication, sample size, mean age, treatment and control groups, pain intensity, initial analgesic request, overall analgesic consumption, patient satisfaction, nausea and vomiting, sedation, hallucinations, dizziness, infection at the injection site, and other events will be included in the data extraction template. The risk of bias summary for each included study will be calculated after the data have been entered into the review manager. When appropriate, the pairwise meta-analysis, network meta-analysis, meta-regression, and publication bias, as well as sensitivity analysis, shall be carried out using STATA 16 or R software version 4.1.3.
Critical appraisal of included studies
The methodological quality of included studies will be assessed by two independent reviewers using the Cochrane handbook Risk of Bias Tool (ROB 2) for systematic reviews of intervention [73], and disagreements will be handled by the other reviewers. Random sequence generation, allocation concealment, blinding of participants and treatment providers, blinding of result assessment, inadequate outcome data, selective outcome reporting, and other bias risks should be assessed. A critical evaluation tool for systematic reviews that contain randomized or non-randomized trials of healthcare interventions, or both, might be used to assess the methodological quality of this systematic review (AMSTAR 2) [73].
Random sequence generation
Studies assessed a computer random number generator or a random number table to generate random sequences were classified as having a minimal risk of bias. Aside from using the lottery technique to generate random sequences, an independent adjudicator can also use tossing a coin, shuffling cards, or throwing dice. It is considered an unknown risk of bias if the technique of randomization was not mentioned yet the experiment was nonetheless presented as randomized.
If the allocation sequence was not randomized or simply quasi-randomized, there is a substantial chance of bias.
Allocation concealment
The patients are assigned by a central independent unit, an on-site closed computer, or identical-looking numbered sealed envelopes or containers generated by an independent investigator, and allocation concealment is considered low risk. If the study was classed as randomized but the allocation concealment procedure was not specified, there is a low risk of bias, and if the allocation sequence was familiar to the investigators who allocated participants, there is a high risk of bias.
Blinding of participants and treatment providers
If the participants and the treatment providers were blinded to intervention allocation and this was described in the article, it is considered to be low risk of bias and it was uncertain if the procedure of blinding was insufficiently described. If blinding of participants and the treatment providers was not performed at all, it was taken as a high risk of bias.
Blinding of outcome assessment
It is said to have a low risk of bias if the outcome assessors were blinded and this was adequately described, but it is unclear if the outcome assessors in the trial were blinded or the extent of blinding was insufficiently described, and it is said to have a high risk of bias if no blinding or incomplete blinding of outcome assessors was performed.
Incomplete outcome data
There were no drop-outs or withdrawals for all outcomes, the numbers and reasons for all withdrawals and drop-outs for all outcomes were clearly stated and could be described as being similar to both groups, or if drop-outs were less than 5%, there is a low risk of bias. If there was insufficient information to assess whether missing data were likely to induce bias on the results, an uncertain risk of bias is assumed. However, a high risk of bias is considered if the results were likely to be skewed by missing data, either because the pattern of drop-outs in the two intervention groups was different or the trial utilized poor strategies to deal with missing data.
Selective outcome reporting
A low risk of bias is considered if a protocol was published before or at the time the trial began, and the outcomes specified in the protocol were reported, and uncertain risk of bias is rated if no protocol was published. If the outcomes in the protocol were not reported at all, a high risk of bias is introduced.
Other risks of bias
If the study looks to be devoid of additional factors that may lead to bias (such as academic or commercial prejudice), it has a low risk of bias. If the study may or may not be free of additional components that may put it at risk of bias but are not stated, it is referred to as unclear risk of bias.
Other elements in the study that might add bias, such as authors performing studies on the same topic or for profit, could raise the likelihood of bias significantly.
The overall risk of bias
Overall, the study is said to have a low risk of bias only if all of the bias domains described are classified as low risk of bias and high risk of bias if any of the bias risk domains described above are classified as “unclear” or high risk of bias.
Grading the quality of evidence
The overall quality of evidence for the studied outcome will be evaluated using the GRADE system (Grading of Recommendations, Assessment, Development, and Evaluation) [52, 74]. The system incorporates study quality (risk of bias), inconsistency (comparison of effect estimates across studies), indirectness (applicability of the population, intervention, comparator, and outcomes to the clinical decision), and imprecision (certainty of confidence interval) and high probability of publication bias. The overall quality of evidence will be categorized by evaluating and combing the above five parameters for maternal.
Data analysis
The data will be analyzed using Review Manager Version 3.3.1 software, R statistical software version 3.6.1, and STATA 16 where applicable. The pooled incidence of postoperative pain, the weighted mean difference in pain score, the first analgesic request, and adverse effects such as nausea and vomiting, hallucination, dizziness, sedation, bleeding at injection site, local anesthetic toxicity, hypotension, hypertension, and infection with fixed and random effect models using the restricted maximum likelihood (REML) method where appropriate, but the meta-analysis results will be reported with random effect model if there is substantial heterogeneity between the included studies.
The heterogeneity among the included studies will be checked with forest plot, χ2 test, I2 test, and the p values. Subgroup analysis will be conducted by the type of intervention, dose range, and types of pain rating scale as postoperative pain usually assessed either with numeric rating scale (NRS) or visual analog scale (VAS). Meta-regression is planned to be conducted with a year of publication, mean age, and sample size. Furthermore, sensitivity analysis might be done to examine the impact of each study on summary effect size by omitting studies one at a time.
Publication bias could be examined with a funnel plot, and the objective diagnostic test will be conducted with Egger’s correlation, Begg’s regression tests, and the Trim and fill method. Network meta-analysis will be performed with the “netmeta” of R version 4.1.3 software to synthesize direct and indirect evidence for efficacy and safety of postoperative pain modalities after cesarean section.
Data synthesis
Narration
The authors want to discuss the sample size, country, intervention, comparator, methodological quality, mean age of participants, baseline clinical factors, primary and secondary outcomes, conclusion, and recommendation of each included study. In addition, the table will summarize the descriptions of the included studies.
Pairwise meta-analysis
This systematic review will be conducted in compliance with the updated Cochrane Handbook for Systematic Reviews of Interventions [75]. The meta-analysis will be conducted with review manager 5 [76] to estimate the pooled effect sizes and risk of bias summary while, STATA 16 software [77], and R software version 4.2 [78] will be used for meta-regression, sensitivity analysis, and publication bias analysis where appropriate. We will conduct the meta-analysis with a restricted maximum likelihood (REML) estimator with both random and fixed effect models as recommended by different authors [79, 80]. Substantial heterogeneity among the included studies will be investigated with subgroup analysis and meta-regression, and the final decision to report the finding either narratively or doing the meta-analysis with a random effect model depends on the clinical importance of the outcome [81,82,83,84]. Publication bias will be checked with a funnel plot, and the objective diagnostic test will be conducted with Egger’s correlation, Begg’s regression tests, and the trim and fill method.
Network meta-analysis
The network meta-analysis will be performed with the “netmeta” of R version 4.1.3 software to synthesize direct and indirect evidence for assessing the efficacy and safety among different wound infiltrative medications (local anesthetics, opioids, ketamine, nonsteroidal anti-inflammatory agents, alpha two agonists, and magnesium sulfate) regimens for postoperative pain management after cesarean section. The inconsistency between direct and indirect comparisons will be assessed by the node splitting method when a loop connecting three arms existed. P scores will be used to rank the treatment effects of different wound infiltration regimens which are based on the point estimates and standard errors of the network assessment.
The geometry of the network
The function of “forest. Netmeta” of R software version 4.1.3 will be used to draw network plots to describe and present the geometry of different wound infiltration regimens. The nodes and edges will be used to reveal the head-to-head comparisons among interventions.
Patient and public involvement
No patient involved.
Ethics and dissemination
Ethical approval is not required for this study as it is a systematic review and meta-analysis. The final result will be presented to international and national conferences. Besides, the manuscript will be published in a national or international peer-reviewed journal.
Discussion
This network meta-analysis is planned to investigate wound infiltration postoperative pain management modalities after a cesarean section.
A systematic review and meta-analysis, and randomized controlled trials revealed that systemic opioid-based analgesics, neuraxial analgesia, and locoregional blocks provide better postoperative pain relief after a cesarean Sect. [7, 18, 30, 62,63,64, 85,86,87,88,89]. However, systemic opioid-based analgesics are associated with several postoperative adverse events including nausea, vomiting, respiratory depression, opioids addiction, and other gastrointestinal complications [88, 90]; neuraxial and thoracoabdominal field block requires resources, expertise, and are also associated with complications including hypotension, high spinal, bradycardia, nerve damage, organ damage, and local anesthetics toxicity [91, 92].
Local wound infiltration techniques using local anesthetics, ketamine, opioids, dexmedetomidine, glucocorticoids, and nonsteroidal anti-inflammatory agents, on the other hand, are feasible due to technical issues, resources, low complication rates, and patient acceptance, despite effectiveness and superiority differences [93].
Evidence revealed that the incidence of postoperative acute and chronic pain is quite high, having a significant influence on the mother, family, healthcare practitioners, and healthcare delivery [21, 26, 27].
Availability of data and materials
Data and material can be available where appropriate.
References
Betran A, Torloni MR, Zhang J, Gülmezoglu A, Aleem H, et al. WHO statement on caesarean section rates. BJOG. 2016;123(5):667–70.
Betrán AP, Merialdi M, Lauer JA, Bing-Shun W, Thomas J, Van Look P, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiol. 2007;21(2):98–113.
Betran AP, Torloni MR, Zhang J, Ye J, Mikolajczyk R, Deneux-Tharaux C, et al. What is the optimal rate of caesarean section at population level? A systematic review of ecologic studies. Reprod Health. 2015;12(1):1–10.
Gibbons L, Belizán JM, Lauer JA, Betrán AP, Merialdi M, Althabe F. The global numbers and costs of additionally needed and unnecessary caesarean sections performed per year: overuse as a barrier to universal coverage. World health report. 2010;30(1):1–31.
Keag OE, Norman JE, Stock SJ. Long-term risks and benefits associated with cesarean delivery for mother, baby, and subsequent pregnancies: systematic review and meta-analysis. PLoS Med. 2018;15(1):e1002494.
Ismail S, Shahzad K, Shafiq F. Observational study to assess the effectiveness of postoperative pain management of patients undergoing elective cesarean section. J Anaesthesiol Clin Pharmacol. 2012;28(1):36.
Abdallah F, Halpern S, Margarido C. Transversus abdominis plane block for postoperative analgesia after caesarean delivery performed under spinal anaesthesia? A systematic review and meta-analysis. Br J Anaesth. 2012;109(5):679–87.
Bhardwaj S, Devgan S, Sood D, Katyal S. Comparison of local wound infiltration with ropivacaine alone or ropivacaine plus dexmedetomidine for postoperative pain relief after lower segment cesarean section. Anesth Essays Res. 2017;11(4):940.
Mishriky BM, George RB, Habib AS. Transversus abdominis plane block for analgesia after cesarean delivery: a systematic review and meta-analysis. Can J Anesth. 2012;59(8):766–78.
Pan PH. Post cesarean delivery pain management: multimodal approach. Int J Obstet Anesth. 2006;15(3):185–8.
Pirbudak L, Balat Ö, Karadaşli H, Ugur MG, Öner Ü. Single perioperative wound infiltration with combination of bupivacaine, tramadol, and tenoxicam for pain relief after cesarean delivery with spinal anesthesia. Pain Clinic. 2004;16(3):287–91.
Demiraran Y, Albayrak M, Yorulmaz IS, Ozdemir I. Tramadol and levobupivacaine wound infiltration at cesarean delivery for postoperative analgesia. J Anesth. 2013;27(2):175–9.
Rackelboom T, Le Strat S, Silvera S, Schmitz T, Bassot A, Goffinet F, et al. Improving continuous wound infusion effectiveness for postoperative analgesia after cesarean delivery: a randomized controlled trial. Obstet Gynecol. 2010;116(4):893–900.
Rahmanian M, Leysi M, Hemmati AA, Mirmohammadkhani M. The effect of low-dose intravenous ketamine on postoperative pain following cesarean section with spinal anesthesia: a randomized clinical trial. Oman Med J. 2015;30(1):11.
Recker DC, Perry PM. Postsurgical pain syndromes: chronic pain after hysterectomy and cesarean section. Tech Reg Anesth Pain Manag. 2011;15(3):133–9.
Sahmeddini MA, Azemati S, Motlagh EM. Local infiltration of tramadol versus bupivacaine for post cesarean section pain control: a double-blind randomized study. Iranian J Med Sci. 2017;42(3):235.
Sarwar A. Effectiveness of local bupivacaine wound infiltration in post-operative pain relief after caesarean section. J Soc Obstet Gynaecol Pak. 2016;6(3):125–8.
Ventham N, Hughes M, O’neill S, Johns N, Brady R, Wigmore S. Systematic review and meta-analysis of continuous local anaesthetic wound infiltration versus epidural analgesia for postoperative pain following abdominal surgery. J Br Surg. 2013;100(10):1280–9.
Wang J, Zhao G, Song G, Liu J. The efficacy and safety of local anesthetic techniques for postoperative analgesia after cesarean section: a Bayesian network meta-analysis of randomized controlled trials. J Pain Res. 2021;14:1559.
Zhu J, Xu C, Wang X, Shi W. Comparison of the analgesic effects of dezocine, tramadol and butorphanol after cesarean section. Pak J Pharm Sci. 2018;31(5(Special)):2191–5.
Gan TJ. Poorly controlled postoperative pain: prevalence, consequences, and prevention. J Pain Res. 2017;10:2287.
Ip HYV, Abrishami A, Peng PW, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. J Am Soc Anesthesiol. 2009;111(3):657–77.
Ip Hui YV, Abrishami A, Peng Philip WH, Wong J, Chung F. Predictors of postoperative pain and analgesic consumption: a qualitative systematic review. Anesthesiology. 2009;111(3):657–77.
Jin J, Peng L, Chen Q, Zhang D, Ren L, Qin P, et al. Prevalence and risk factors for chronic pain following cesarean section: a prospective study. BMC Anesthesiol. 2016;16(1):1–11.
Werner MU, Mjöbo HN, Nielsen PR, Rudin Å, Warner DS. Prediction of postoperative pain: a systematic review of predictive experimental pain studies. J Am Soc Anesthesiol. 2010;112(6):1494–502.
Yang MM, Hartley RL, Leung AA, Ronksley PE, Jetté N, Casha S, et al. Preoperative predictors of poor acute postoperative pain control: a systematic review and meta-analysis. BMJ Open. 2019;9(4):e025091.
Yimer H, Woldie H. Incidence and associated factors of chronic pain after caesarean section: a systematic review. J Obstet Gynaecol Can. 2019;41(6):840–54.
Borges NC, de Deus JM, Guimarães RA, Conde DM, Bachion MM, de Moura LA, et al. The incidence of chronic pain following cesarean section and associated risk factors: a cohort of women followed up for three months. PLoS ONE. 2020;15(9):e0238634.
Getaneh T, Negesse A, Dessie G, Desta M, Temesgen H, Getu T, et al. Impact of cesarean section on timely initiation of breastfeeding in Ethiopia: a systematic review and meta-analysis. Int Breastfeed J. 2021;16(1):1–10.
Xu M, Tang Y, Wang J, Yang J. Quadratus lumborum block for postoperative analgesia after cesarean delivery: a systematic review and meta-analysis. Int J Obstet Anesth. 2020;42:87–98.
Amin S, Tahir S. Impact of bupivacaine infiltration of postoperative wound on parenteral narcotic analgesic requirement for pain. J Surg Pak. 2010;15(4):177–81.
Bharati K, Kumar B, Singh HD. A randomized clinical comparison of levobupivacaine versus levobupivacaine with ketamine for postoperative pain control in LSCS. Eur J Mol Clin Med. 2021;7(11):8051–8.
Chompubai P, Nontawasi K, Jaturasrivilai P, Saetae S. Analgesic efficacy of pfannenstiel wound infiltration following cesarean section: comparison between 0.25% bupivacaine and mixture of 0.25% bupivacaine with lidocaine. Lampang Med J. 2016;37(2):46–56.
Choudhary D. Comparative assessment of the subcutaneous infiltration of levobupivacaine alone versus levobupivacaine with ketamine in lower segment cesarean section. Eur J Mol Clin Med. 2021;7(8):5744–50.
Deshwal R, Kumar N, Sharma JP, Kumar R. Efficacy of dexmedetomidine added to ropivacaine infilteration on postoperative pain following spine surgeries: a randomized controlled study. Anesth Essays Res. 2018;12(3):700.
Edomwonyi N, Osazuwa M, Iribhogbe O, Esangbedo S. Postoperative analgesia using bupivacaine wound infiltration with intravenous tramadol or dexamethasone following obstetric spinal anaesthesia. Niger J Clin Pract. 2017;20(12):1584–9.
Eldaba AA, Amr YM, Sobhy RA. Effect of wound infiltration with bupivacaine or lower dose bupivacaine/magnesium versus placebo for postoperative analgesia after cesarean section. Anesth Essays Res. 2013;7(3):336.
Haliloglu M, Bilgen S, Menda F, Ozcan P, Ozbay L, Tatar S, et al. Analgesic efficacy of wound infiltration with tramadol after cesarean delivery under general anesthesia: randomized trial. J Obstet Gynaecol Res. 2016;42(7):816–21.
Kaler P, Verma I, Grewal A, Taneja A, Sood D. Comparison of levobupivacaine alone versus levobupivacaine with ketamine in subcutaneous infiltration for postoperative analgesia in lower segment cesarean section. J Obstet Anaesth Crit Care. 2019;9(2):60.
Li X, Zhou M, Shi X, Yang H, Li Y, Li J, et al. Local anaesthetic wound infiltration used for caesarean section pain relief: a meta-analysis. Int J Clin Exp Med. 2015;8(6):10213.
Nasir F, Sohail I, Sadiq H, Habib M. Local wound infiltration with ropivacaine for postoperative pain control in caesarean section. Cureus. 2019;11(9):e5572.
Paladini G, Di Carlo S, Musella G, Petrucci E, Scimia P, Ambrosoli A, et al. Continuous wound infiltration of local anesthetics in postoperative pain management: safety, efficacy and current perspectives. J Pain Res. 2020;13:285.
Behdad S, Sekhavat L, Ayatollahi V, Meshkat F, Mortazavi A. Comparison of postoperative analgesic effect of tramadol and bupivacaine subcutaneous infiltration in patients undergoing cesarean section. Acta Clin Croat. 2013;52(1.):93–7.
Ekmekçi P, Çağlar GS, Yilmaz H, Kazbek BK, Gursoy AY, Kiseli M, et al. Effects of different doses of tramadol added to levobupivacaine in continuous wound infusion for postoperative pain treatment following cesarean section. J Matern Fetal Neonatal Med. 2017;30(3):343–6.
Haliloglu M, Bilgen S, Menda F, Ozbay L, Ozer UD, Koner O. A randomised trial of the analgesic efficacy of wound infiltration with tramadol after caesarean section under general anesthesia: 11AP5–7. Eur J Anaesthesiol EJA. 2014;31:191.
Jabalameli M, Safavi M, Honarmand A, Saryazdi H, Moradi D, Kashefi P. The comparison of intraincisional injection tramadol, pethidine and bupivacaine on postcesarean section pain relief under spinal anesthesia. Adv Biomed Res. 2012;1:53.
Atashkhoyi S, Sadagiani MM, Azarfarin R. Efficacy of pre-incisional subcutaneous infiltration of low-dose ketamine on postoperative pain after cesarean section. 2011.
Kazemnejad K, Hosseini SM, Haydari A, Ghourchaei A. Comparison of the effect of subcutaneous injection of ketamine and lidocaine in reducing postoperative pain in patients undergoing elective inguinal hernia surgery under general anesthesia. J Gorgan Univ Med Sci. 2020;22(1):1–6.
Khajavi MR, Navardi M, Moharari RS, Pourfakhr P, Khalili N, Etezadi F, et al. Combined ketamine-tramadol subcutaneous wound infiltration for multimodal postoperative analgesia: a double-blinded, randomized controlled trial after renal surgery. Anesth Pain Med. 2016;6(5):e37778.
Kumar B, Singh HD, Bharati K. A randomized clinical comparison of levobupivacaine versus levobupivacaine with ketamine for postoperative pain Control in LSCS. Eur J Mol Clin Med (EJMCM). 7(11):2020.
Lavand’homme PM, Roelants F, Waterloos H, De Kock MF. Postoperative analgesic effects of continuous wound infiltration with diclofenac after elective cesarean delivery. J Am Soc Anesthesiol. 2007;106(6):1220–5.
Abd El-Hamid AM, Alrabiey MI, Abd El-Fattah MH. A comparison of the postoperative analgesic effects of intravenous dexmedetomidine with a combination of dexmedetomidine and bupivacaine wound infiltration for lower segment cesarean section: a prospective, randomized study. Ain-Shams J Anaesthesiol. 2016;9(2):235.
Kundra S, Singh RM, Singh G, Singh T, Jarewal V, Katyal S. Efficacy of magnesium sulphate as an adjunct to ropivacaine in local infiltration for postoperative pain following lower segment caesarean section. J Clin Diagnos Res. 2016;10(4):UC18.
Mohamed MS, Abd El-Razik AN, Abd El-Ghani NA. A comparative study of low dose ketamine versus magnesium sulfate for local wound infiltration after cesarean section.
Bollag L, Lim G, Sultan P, Habib AS, Landau R, Zakowski M, et al. Society for obstetric anesthesia and perinatology: consensus statement and recommendations for enhanced recovery after cesarean. Anesth Analg. 2021;132(5):1362–77.
Sultan P, Sharawi N, Blake L, Habib AS, Brookfield KF, Carvalho B. Impact of enhanced recovery after cesarean delivery on maternal outcomes: a systematic review and meta-analysis. Anaesth Crit Care Pain Med. 2021;40(5):100935.
Roofthooft E, Joshi G, Rawal N, Van de Velde M, AnaesthesiaPWGotESoR, Therapy P, et al. PROSPECT guideline for elective caesarean section: updated systematic review and procedure-specific postoperative pain management recommendations. Anaesthesia. 2021;76(5):665–80.
Adesope O, Ituk U, Habib AS. Local anaesthetic wound infiltration for postcaesarean section analgesia: a systematic review and meta-analysis. Eur J Anaesthesiol EJA. 2016;33(10):731–42.
Tikhonov DB, Zhorov BS. Mechanism of sodium channel block by local anesthetics, antiarrhythmics, and anticonvulsants. J Gen Physiol. 2017;149(4):465–81.
Fozzard H, Lee P, Lipkind G. Mechanism of local anesthetic drug action on voltage-gated sodium channels. Curr Pharm Des. 2005;11(21):2671–86.
Arcisio-Miranda M, Muroi Y, Chowdhury S, Chanda B. Molecular mechanism of allosteric modification of voltage-dependent sodium channels by local anesthetics. J Gen Physiol. 2010;136(5):541–54.
Turan A, Sessler DI. Steroids to ameliorate postoperative pain. J Am Soc Anesthesiol. 2011;115(3):457–9.
Zhao W-L, Ou X-F, Liu J, Zhang W-S. Perineural versus intravenous dexamethasone as an adjuvant in regional anesthesia: a systematic review and meta-analysis. J Pain Res. 2017;10:1529.
Waldron N, Jones C, Gan T, Allen T, Habib A. Impact of perioperative dexamethasone on postoperative analgesia and side-effects: systematic review and meta-analysis. Br J Anaesth. 2013;110(2):191–200.
Almarakbi WA, Kaki AM. Addition of dexmedetomidine to bupivacaine in transversus abdominis plane block potentiates post-operative pain relief among abdominal hysterectomy patients: a prospective randomized controlled trial. Saudi J Anaesth. 2014;8(2):161.
Chetty S. Dexmedetomidine for acute postoperative pain: refresher course. South African J Anaesth Analg. 2011;17(1):139–40.
Halaszynski TM. Dexmedetomidine: a look at a promising new avenue of use. Saudi J Anaesth. 2012;6(2):104.
Radvansky BM, Shah K, Parikh A, Sifonios AN, Le V, Eloy JD. Role of ketamine in acute postoperative pain management: a narrative review. BioMed Res Int 2015;2015.
Tawfic QA. A review of the use of ketamine in pain management. J Opioid Manag. 2013;9(5):379–88.
Zhao Y, He J, Yu N, Jia C, Wang S. Mechanisms of dexmedetomidine in neuropathic pain. Front Neurosci. 2020;14:330.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ. 2015;349:i4086.
Liao C-Y, Ganz J, Vannest K, Wattanawongwan S, Pierson L, Yllades V, et al. PRISMA Flow Diagram of the Search Process. 2019.
Shea BJ, Reeves BC, Wells G, Thuku M, Hamel C, Moran J, et al. AMSTAR 2: a critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ. 2017;358:j4008.
Guyatt GH, Oxman AD, Kunz R, Brozek J, Alonso-Coello P, Rind D, et al. GRADE guidelines 6 Rating the quality of evidence—imprecision. J Clin Epidemiol. 2011;64(12):1283–93.
Cumpston M, Li T, Page MJ, Chandler J, Welch VA, Higgins JP, et al. Updated guidance for trusted systematic reviews: a new edition of the Cochrane Handbook for Systematic Reviews of Interventions. Cochrane Database Syst Rev. 2019;10:142.
Copenhagen: The Nordic Cochrane Centre TCC. Review Manager (RevMan)[Computer program]. Version 5.3. 2014.
StataCorp L. Stata Statistical Software. Release 16.[software]. College Station, TX. Stata Press. Available at: https://www.stata.com/. Accessed Sept 2019.
Team RC. R: A language and environment for statistical computing. Vienna: R Foundation for Statistical Computing; 2012. (ISBN 3-900051-07-0).
Kontopantelis E, Reeves D. Performance of statistical methods for meta-analysis when true study effects are non-normally distributed: a simulation study. Stat Methods Med Res. 2012;21(4):409–26.
Veroniki AA, Jackson D, Viechtbauer W, Bender R, Bowden J, Knapp G, et al. Methods to estimate the between-study variance and its uncertainty in meta-analysis. Res Synth Methods. 2016;7(1):55–79.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60.
Bowden J, Tierney JF, Copas AJ, Burdett S. Quantifying, displaying and accounting for heterogeneity in the meta-analysis of RCTs using standard and generalised Q statistics. BMC Med Res Methodol. 2011;11(1):1–12.
Melsen W, Bootsma M, Rovers M, Bonten M. The effects of clinical and statistical heterogeneity on the predictive values of results from meta-analyses. Clin Microbiol Infect. 2014;20(2):123–9.
Schroll JB, Moustgaard R, Gøtzsche PC. Dealing with substantial heterogeneity in Cochrane reviews. Cross-sectional study. BMC Med Res Methodol. 2011;11(1):1–8.
Tan HS, Taylor C, Weikel D, Barton K, Habib AS. Quadratus lumborum block for postoperative analgesia after cesarean delivery: a systematic review with meta-analysis and trial-sequential analysis. J Clin Anesth. 2020;67:110003.
Wang P, Chen X, Chang Y, Wang Y, Cui H. Analgesic efficacy of ultrasound-guided transversus abdominis plane block after cesarean delivery: a systematic review and meta-analysis. J Obstet Gynaecol Res. 2021;47(9):2954–68.
Fusco P, Scimia P, Paladini G, Fiorenzi M, Petrucci E, Pozone T, et al. Transversus abdominis plane block for analgesia after cesarean delivery. A systematic review. Minerva Anestesiol. 2014;81(2):195–204.
Bonnet M-P, Mignon A, Mazoit J-X, Ozier Y, Marret E. Analgesic efficacy and adverse effects of epidural morphine compared to parenteral opioids after elective caesarean section: a systematic review. Eur J Pain. 2010;14(9):894. e1-. 9.
Møiniche S, Kehlet H, Dahl JB. A qualitative and quantitative systematic review of preemptive analgesia for postoperative pain relief: the role of timing of analgesia. J Am Soc Anesthesiol. 2002;96(3):725–41.
Jaafarpour M, Taghizadeh Z, Shafiei E, Vasigh A, Sayehmiri K. The effect of intrathecal meperidine on maternal and newborn outcomes after cesarean section: a systematic review and meta-analysis study. Anesthesiol Pain Med. 2020;10(2):e100375.
Fischer B. Benefits, risks, and best practice in regional anesthesia: do we have the evidence we need? Reg Anesth Pain Med. 2010;35(6):545–8 (8).
Brull R, McCartney CJ, Chan VW, El-Beheiry H. Neurological complications after regional anesthesia: contemporary estimates of risk. Anesth Analg. 2007;104(4):965–74.
Riemma G, Schiattarella A, Cianci S, La Verde M, Morlando M, Sisti G, et al. Transversus abdominis plane block versus wound infiltration for post-cesarean section analgesia: A systematic review and meta-analysis of randomized controlled trials. Int J Gynecol Obstet. 2021;153(3):383–92.
Acknowledgements
The authors would like to acknowledge Dilla University for technical support and encouragement to carry out the project.
Funding
No funding was obtained from any organization.
Author information
Authors and Affiliations
Contributions
SA and GM conceived the idea design of the project. SA, GM, BB, SN, and MT were involved in the searching strategy, data extraction, quality assessment, analysis, and manuscript preparation. The authors read and approved the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication.
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1:
Supplemental Table 1. Comprehensive search strategies of different databases as per PICOs criteria.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Abate, S.M., Mergia, G., Nega, S. et al. Efficacy and safety of wound infiltration modalities for postoperative pain management after cesarean section: a systematic review and network meta-analysis protocol. Syst Rev 11, 194 (2022). https://doi.org/10.1186/s13643-022-02068-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-022-02068-2