Abstract
Background
Sensorineural hearing loss (SNHL) is the most common form of hearing impairment and is characterized by a loss of receptor hair cells and/or spiral ganglion neurons. Regenerative stem cell therapy could potentially restore normal hearing and slow the progression of hearing loss in patients. Preclinical animal studies have demonstrated that mesenchymal stem cells (MSCs) could be a promising new therapy for this condition. These findings have prompted investigators to begin human clinical trials to assess the safety and efficacy of MSCs for the treatment of SNHL. The objective of the proposed systematic review is to examine the efficacy of MSCs as a therapy for SNHL in animal models.
Methods
We will include preclinical animal studies of SNHL in which MSCs are administered, and outcomes are compared against MSC-naïve controls. The primary outcome will include audiologic tests that are routinely used in experimental studies of hearing loss, such as auditory brainstem response (ABR) and distortion product otoacoustic emissions testing (DPOAE). Secondary outcomes will include histology, microscopy, gene protein expression, and behavioral responses of animals. Electronic searches of MEDLINE via PubMed, Scopus, ScienceDirect, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) will be performed. Search results will be screened independently and in duplicate. Data from eligible studies will be extracted, pooled, and analyzed using random effects models. Risk of bias and publication bias will be assessed using the Systematic Review Center for Laboratory Animal Experimentation (SYRCLE) risk of bias tool and Funnel Plots/Egger’s regression tests, respectively.
Discussion
This systematic review will provide a summary of the efficacy of MSC therapy in animal models of SNHL, utilizing functional hearing assessment as a primary outcome. Findings from this review are important because they can elucidate research gaps that should be addressed in future preclinical studies and in turn can be translated into clinical studies.
Systematic review registration
CAMARADES (http://www.dcn.ed.ac.uk/camarades/)
Similar content being viewed by others
Background
Sensorineural hearing loss (SNHL) is the most common form of hearing impairment [1]. SNHL affects up to 4.6 infants per 1000 live births [1] and has a multifactorial etiology, including congenital anomalies, exposure to ototoxic drugs, noise induced, and/or aging [2]. Individuals with any degree of SNHL are at increased risk for language delay, depression, and cognitive decline [3, 4].
Current approaches to treat SNHL focus on the use of hearing aids and cochlear implants. These devices bypass the damaged ear by augmenting sound intensity to a detectable threshold [5]. Although supportive, these interventions are not curative. Future therapies should focus on restoring and/or attenuating progressive hearing loss.
Major advancements in regenerative medicine have stimulated interest in the potential of cell-based therapies for SNHL. Mesenchymal stem/stromal cells (MSCs) have emerged as the cell line with most therapeutic potential due to their ease for isolation, regenerative properties, and easy and non-invasive retrieval [6]. Preclinical studies have now demonstrated that MSCs provide favorable results in orthopedics, myocardial infarctions, liver fibrosis, respiratory distress syndrome, and autoimmune conditions [7,8,9,10]. MSCs are novel and viable options to treat SNHL since they have the potential to differentiate into hair cells and spiral ganglion neurons. As well, preclinical animal studies have revealed an improvement in auditory functioning [2, 11,12,13]. Currently, a phase I/II clinical trial (NCT02038972) is evaluating the safety and efficacy of umbilical cord-derived MSCs for treatment of SNHL. Despite these advancements, there has been no systematic synthesis of preclinical studies evaluating the use of MSCs for SNHL.
The objective of the proposed systematic review is to examine the efficacy of MSCs as a therapy for SNHL in animal models. Results from this work may help guide subsequent preclinical studies, as well as potentially impact key elements in future clinical trials.
Study question
In preclinical studies of SNHL, does administration of MSCs improve hearing outcomes when compared to placebo or untreated controls?
Methods/design
Protocol and registration
The protocol was developed through discussions with our scientific research team. The team was comprised of clinicians (AM) and translational scientists (KC, MW, NM, WH). This protocol will adhere to the Systematic Review Protocol for Animal Intervention Studies guidelines set forth by the Systematic Review Centre for Laboratory Animal Experimentation (SYRCLE) [14]. This protocol has been registered under Collaborative Approach to Meta-Analyses and Review of Animal Data from Experimental Studies (CAMARADES) website, found at http://www.dcn.ed.ac.uk/camarades/research.html#protocols, and is also attached as an additional file [see Additional file 1].
SNHL definition and type of studies
In the current study, SNHL is a type of hearing loss in which the root cause lies in the vestibulocochlear nerve or the inner ear. SNHL is characterized by a loss of receptor hair cells and/or spiral ganglion neurons, which carry afferent signals from the cochlea [12]. There are a variety of causes of SNHL, most commonly genetic dysfunction, ototoxic drugs like aminoglycosides and loop diuretics, noise exposure, and aging [11]. In preclinical studies, SNHL is induced via pharmacological agent, immunological conditioning, hereditary dysfunction, and noise induction [2, 12, 13].
The inclusion criteria are as follows: full-text original papers, controlled animal intervention studies (randomized and non-randomized) that evaluate the therapeutic efficacy of mesenchymal stem cells (MSCs) for sensorineural hearing loss in animals, regardless of methodological quality.
The exclusion criteria are as follows: review and editorial articles, non-intervention studies, no control group, human studies, exclusive in vitro work, or co-intervention studies.
Types of preclinical animal models
We will include preclinical in vivo models of SNHL that represent the pathophysiological features of human SNHL. Eligible animal models include healthy mammals of all genders and ages. A variety of methods to induce SNHL exist, which include surgical injection of neomycin and oubain mixture into the cochlea, animals with hereditary SNHL, and β-tubulin immunization [2, 12, 13]. These models may require surgery or extensive manipulation that is subject to technical variability. However, these models provide a predictable disease phenotype and share a common feature to human SNHL: histological evidence of cochlear cell loss or elevated auditory brainstem response (ABR) thresholds.
Intervention vs. control group
The intervention group will include animals receiving MSCs after the induction of SNHL. Studies treating animals with cell-free products (microRNA, exosomes, microvesicles, etc.) will be excluded. An MSC will be defined per the International Society for Cellular Therapy [15]. The preclinical comparison group will include animals from studies that have experimentally induced or hereditary SNHL but have not been administered an MSC, including placebo-controlled and sham-operated animals.
Type of interventions
The intervention group will include animals that receive administration(s) of MSCs regardless of dosage, timing, delivery routes, and frequency of intervention. MSC sources can be autologous, xenogeneic, allogenic, and syngeneic. Furthermore, we will add studies that have modified (genetically, pharmacologically) MSCs and incorporate them as single or adjuvant agents (with scaffolds, other cells, or conditioned media).
Primary/secondary endpoints
The current gold standard for the diagnosis and evaluation of sensorineural hearing loss is a functional hearing assessment. There are multiple approaches to assess functional hearing in preclinical studies; therefore, this systematic review will include studies that utilize audiologic tests that are routinely used in experimental studies of hearing loss [16]. Therefore, the primary outcomes will include:
-
1.
Cochlear microphonic receptor potentials
-
2.
Auditory brainstem response (ABR)
-
3.
Electrocochleography
-
4.
Distortion product otoacoustic emissions testing (DPOAE)
-
5.
Summating potentials
-
6.
Tympanometry
-
7.
Compound action potentials
-
8.
Brainstem auditory evoked potentials (BAEPs)
The secondary endpoints will include:
-
1.
Histology
-
2.
Microscopy
-
3.
Gene protein expression
-
4.
Behavioral responses of animals
Results from studies that incorporate the same audiologic testing will be pooled for further analysis. If the data is appropriate for quantitative synthesis, meta-analysis will be conducted using a random effects model to generate forest plots. The estimated effect of MSCs on functional hearing will be analyzed with standard mean difference (SMD) and 95% confidence intervals (CI). Statistical heterogeneity between studies will calculated using I2 metrics, and further subgroup analysis using meta-regression will be performed to assess the impact of all variables on the study effect. The variables examined will include animal type, age, sex, species, and strain; type of SNHL induction; type and tissue source of MSC; and timing, frequency, and route of cell administration.
Timing of outcome measurements
Outcomes that meet primary +- secondary end point (before and after intervention, short- vs. long-term, and repeated studies) will be included.
Search strategies
We will conduct a comprehensive search of MEDLINE via PubMed, Scopus, ScienceDirect, and Cumulative Index to Nursing and Allied Health Literature (CINAHL) databases. Only articles in the English language will be included in the review. There will be no restrictions to publication dates.
Search strategies will use a combination of controlled vocabulary (e.g., mesenchymal stem cells, sensorineural hearing loss, animal) and keywords (e.g., SNHL, ABR, MSC), and parsing will be formatted accordingly to each database. An additional file with the search terms utilized for PubMed is attached [see Additional file 2]. Furthermore, a manual review of references of the selected articles will be performed. A sample combination of search terms and keywords includes:
-
i.
Mesenchymal stem cell, mesenchymal stromal cell, MSC
-
ii.
Sensorineural hearing loss, hearing impairment, SNHL
-
iii.
Animal, preclinical, experimental
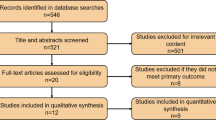
Study selection
Titles and abstracts of the search results will be screened independently by two individuals (KC, MW). Full-text articles will be reviewed based on the inclusion and exclusion criteria. Disagreements between individuals will be resolved by consensus or by a third member of the group (AM). Reasons for study exclusion will be recorded and presented in accordance with the SYRCLE Guidelines.
Data collection
Data will be extracted independently by two individuals (KC, MW) using a standardized form approved by all investigators. If any data is missing or further information is required, the authors of the manuscripts will be emailed. In case of no response after a reminder email at 1 month, studies will be excluded from the analysis. Specific data elements collected for this review are listed in Table 1.
Assessment of risk of bias
The risk of bias will be assessed independently by two individuals using the SYRCLE risk of bias tool [17]. The SYRCLE tool contains ten assessment domains related to selection bias, performance bias, detection bias, attrition bias, and reporting bias. For each included study, each domain will be scored as low, high, or unclear risk of bias.
Assessment of external validity and construct validity
This systematic review will record characteristics that will assess external validity or the degree to which the results can be generalized to different experimental settings. This will assess the ability to replicate the study. This will be evaluated via subgroup analysis of the primary outcome based on species/strain of animal, control group, tissue source, route of administration, timing and dose of MSCs, and modifications to the MSCs. This data will assess the effects of factors such as animal characteristics and preparation/source of MSCs on the primary and secondary outcome. Furthermore, this will establish the ideal conditions for future preclinical and clinical trials.
Construct validity in preclinical research refers to the extent to which the animal study correlates to a clinical scenario [18]. Construct validity will be assessed according to how well the experimental design models SNHL in humans. The domains assessed will be animal subjects (small vs large animal), outcome measures of hearing assessment (whether they are the same ones used in humans), modeling of disease (noise induction vs medication induced), administration of intervention (clinically relevant such as intravenous, subcutaneous vs. non-clinically relevant, i.e., intraperitoneal). This will help determine whether the included studies enable generalization to a potential clinical study of stem cells for SNHL.
Data analysis
Categorical variables will be presented as frequencies and percentages, and continuous variables will be pooled using the ratio of weighted means method with inverse variance random effects modeling [19]. When appropriate, dichotomous variables will be pooled and described as odds ratios and 95% CIs. Statistical heterogeneity of included studies will be measured with I2 tests with 95% uncertainty intervals [20]. If there is an adequate amount of studies, an assessment for the existence of publication bias will be conducted with funnel plot techniques and Egger’s regression test [21].
Discussion
The knowledge gained from these studies is now impacting subsequent experiments that seek to assess the functional benefits of stem cell therapy as a treatment for SNHL. Current research has begun on early phases of clinical trials on the subject [11, 22]. The progression of research on SNHL in human subjects warrants further examination of the efficacy of mesenchymal stem cell (MSC) therapy in animal models. Improving methodology and standardizing the procedure in animal models could optimize results seen in human trials. While there are other studies that have examined the use of cell-free products (microvesicles, conditioned media, and miRNA) as a viable treatment, this systematic review focuses on the use of cell-based therapies, specifically MSCs.
This review will also focus on identifying various gaps or inconsistencies in preclinical experiments. By analyzing and comparing the current data on MSC treatment in animal models of SNHL, we intend to promote a more consistent method and directional approach.
There are several limitations to this study that are common across systematic reviews. The studies included will only be those published and will not include studies that are unpublished or not in English. Furthermore, it will be difficult to ascertain the clinical translatability of our findings, given that this study will only include preclinical animal models.
Abbreviations
- ABR:
-
Auditory brainstem response
- BAEPs:
-
Brainstem auditory evoked potentials
- CINAHL:
-
Cumulative Index to Nursing and Allied Health Literature
- DPOAE:
-
Distortion product otoacoustic emissions testing
- MSC:
-
Mesenchymal stem/stromal cell
- SNHL:
-
Sensorineural hearing loss
- SYRCLE:
-
Systematic Review Centre for Laboratory Animal Experimentation
References
Summary of 2009 National CDC EHDI Data Source: 2009 CDC EHDI Hearing Screening & Follow-up Survey (HSFS) Number of Respondents: 50 (47 states and 3 territories) 2009 Documented EHDI Data Items Summary of 2009 National CDC EHDI Data. 2012;50(January):50–3.
Ma Y, Guo W, Yi H, Ren L, Zhao L, Zhang Y, et al. Transplantation of human umbilical cord mesenchymal stem cells in cochlea to repair sensorineural hearing. Am J Transl Res. 2016;8(12):5235–45.
Yoshinaga-Itano C, Sedey A, Coulter D, Mehl A. Language of early-and later-identified children with hearing loss. Pediatrics. 1998;102(5):1161–71.
Allen TE. Patterns of academic achievement among hearing impaired students: 1974 and 1983. In: Schildroth AN, Karchmer MA, eds. Deaf children in America. Boston, MA: College-Hill press; 1986:161–206.
Youm I, Li W. Cochlear hair cell regeneration: an emerging opportunity to cure noise- induced sensorineural hearing loss. Drug Discov Today [Internet] Elsevier Ltd; 2018;00(00):1–6.
Ullah I, Subbarao RB, Rho GJ. Human mesenchymal stem cells - current trends and future prospective. Biosci Rep [Internet] 2015;35(2):1–18.
Cárdenes N, Cáceres E, Romagnoli M, Rojas M. Mesenchymal stem cells: a promising therapy for the acute respiratory distress syndrome. Respiration. 2013;85(4):267–78.
Karantalis V, Hare JM. Use of mesenchymal stem cells for therapy of cardiac disease. Circ Res. 2015;116(8):1413–30.
Figueroa FE, Carrión F, Villanueva S, Khoury M. Mesenchymal stem cell treatment for autoimmune diseases: a critical review. Biol Res. 2012;45(3):269–77.
Eom YW, Shim KY, Baik SK. Mesenchymal stem cell therapy for liver fibrosis. Korean J Intern Med [Internet] 2015;30(5):580–589.
Lee HS, Kim WJ, Gong JS, Park KH. Clinical safety and efficacy of autologous bone marrow-derived mesenchymal stem cell transplantation in sensorineural hearing loss patients. J Audiol Otol. 2018;22(2):105–9.
Bas E, Van De WTR, Goss G, Hare JM, Goldstein BJ. Adult human nasal mesenchymal-like stem cells. Stem Cells Dev. 2014;23(5):502–14.
Choi BY, Song J, Chang SO, Kim SU, Oh SH. Intravenous administration of human mesenchymal stem cells after noise- or drug- induced hearing loss in rats. Acta Otolaryngol. 2012;132(Suppl 1):S94–102. https://doi.org/10.3109/00016489.2012.660731.
Hooijmans C, Rovers M, de Vries R, Leenaars M, Ritskes-Hoitinga M, Langendam M. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014;14(1):43.
Dominici M, Le Blanc K, Mueller I, Slaper-Cortenbach I, Marini F, Krause D, Deans R, Keating A, Prockop DJ, Horwitz E. Minimal criteria for defining multipotent mesenchymal stromal cells. The international society for cellular therapy position statement. Cytotherapy. 2006;8:315–7.
Reis A. Animal models for hearing evaluations : a literature review Modelos animais Para avaliação auditiva: revisão de literatura. Rev. CEFAC. 2017;19(3):417–27.
Hooijmans CR, Rovers MM, De Vries RBM, Leenaars M, Ritskes-hoitinga M, Langendam MW. SYRCLE’s risk of bias tool for animal studies. BMC Med Res Methodol. 2014:1–9.
Henderson VC, Kimmelman J, Fergusson D, Grimshaw JM, Hackam DG. Threats to validity in the design and conduct of preclinical efficacy studies: a systematic review of guidelines for in vivo animal experiments. PLoS Med. 2013;10(7):e1001489.
Friedrich JO, Adhikari NKJ, Beyene J. The ratio of means method as an alternative to mean differences for analyzing continuous outcome variables in meta-analysis: a simulation study. BMC Med Res Methodol. 2008;15:32.
Higgins JPT, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;1558:1539–58.
Hayashino Y, Noguchi Y, Fukui T. Systematic evaluation and comparison of statistical tests for publication bias. J Epidemiol. 2005;15:235–43.
Liu H, Qu Z, Sun S, Xiao D, Yang T, Chen L, Wang Y. Intravenous injection of human umbilical cord derived mesenchymal stem cells for the treatment of sudden sensorineural hearing loss: a case report. Paper presented at the WIT Transactions on Biomedicine and Health. 2014;19:485–92.
Acknowledgements
N/a
Funding
The project described was supported by the National Center for Advancing Translational Sciences, National Institutes of Health, through Grant KL2 TR001118 to Alvaro Moreira. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIH. This study was also supported by The University of Texas Health San Antonio School of Medicine Clinical Investigator Kickstart Pilot Grant.
Availability of data and materials
All relevant data are within the paper and its Supporting Information files.
Author information
Authors and Affiliations
Contributions
KC, WH, and AM conceived the study design. KC, MW, NM, and AM were responsible for the initial drafting of the manuscript. KC and MW were responsible for the data collection. KC, MW, NM, WH, and AM provided critical revisions for important intellectual content. All authors have reviewed and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
N/a
Consent for publication
N/a
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Systematic Review Center for Laboratory animal Experimentation Protocol for. (PDF 459 kb)
Additional file 2:
Search terms used in MEDLINE's PubMed. (DOCX 11 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Chorath, K.T., Willis, M.J., Morton-Gonzaba, N. et al. Mesenchymal stem cells for sensorineural hearing loss: protocol for a systematic review of preclinical studies. Syst Rev 8, 126 (2019). https://doi.org/10.1186/s13643-019-1015-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-019-1015-7