Abstract
Background
Polycystic ovarian syndrome (PCOS) is a common reproductive endocrine disease that is seen among adolescent women. Currently, there is limited evidence to support treatment options leading to considerable variation in practice among healthcare specialists. The objective of this study is to review and synthesize all the available evidence on treatment options for PCOS among adolescent women.
Methods/design
We will conduct a systematic review of all randomized controlled trials evaluating the use of metformin, oral contraceptive pills as monotherapy, or as combination with pioglitazone, spironolactone, flutamide, and lifestyle interventions in the treatment of PCOS in adolescent women ages 11 to 19 years. The primary outcome measures are menstrual regulation and change hirsutism scores. The secondary outcome measures include acne scores, prevalence of dysglycaemia, BMI, lipid profile, total testosterone level, and adverse events. We will perform literature searches through Ovid Medline, Ovid Embase, and Cochrane Central Register of Controlled Trials (CENTRAL), and gray literature resources. Two reviewers will independently screen titles and abstracts of identified citations, review the full texts of potentially eligible trials, extract information from eligible trials, and assess the risk of bias and quality of the evidence independently. Results of this review will be summarized narratively and quantitatively as appropriate. We will perform a multiple treatment comparison using network meta-analysis to estimate the pooled direct and indirect effects for all PCOS interventions on outcomes if adequate data is available.
Discussion
PCOS treatment poses a clinical challenge to the patients and physicians. This is the first systematic review and network meta-analysis for PCOS treatment in adolescents. We expect that our results will help improve patient care, unify the treatment approaches among specialists, and encourage research for other therapeutic options.
Systematic review registration
PROSPERO CRD42015016148
Similar content being viewed by others
Background
Polycystic ovarian syndrome (PCOS) is a common reproductive endocrine disease encountered among adolescents and young women [1]. Its prevalence varies between 1.8 and 15 % depending on the diagnostic criteria used and ethnicity [1–3]. Patients with PCOS can present with a constellation of symptoms including chronic anovulation (amenorrhea, oligomenorrhea, irregular menstrual cycles), clinical features of hyperandrogenism (acne and hirsutism), biochemical evidence of hyperandrogenism, polycystic ovaries on ultrasound, and features of metabolic syndrome. Oligomenorrhea is the presenting feature in about 75 % of cases [4], while hirsutism and acne are present in 60–70 % of cases and contribute to psychological distress in adolescent patients [4, 5].
Three different diagnostic criteria have been used for the diagnosis of PCOS: the National Institutes of Health (NIH), the Rotterdam, and the Androgen Excess Society Criteria [6–8]. All of them require the presence of menstrual cycle disturbance and presence of clinical and/or biochemical hyperandrogenism, while the last two require the presence of polycystic ovarian morphology on ultrasound [6, 7]. To date, the preferred diagnostic criteria in adolescents are the NIH criteria [9, 10].
The etiology of PCOS is complex and not well understood. Primary intrinsic ovarian pathology in combination with hypothalamic–pituitary–ovarian axis abnormalities may lead to increased ovarian androgen secretion [11, 12]. Insulin resistance with compensatory hyperinsulinemia may also play a role as it can lead to direct stimulation of ovarian and adrenal androgen secretion, which leads to decreased hepatic sex hormone binding globulin synthesis and therefore, to an increased bioavailability of free testosterone level [11–14]. Insulin resistance is involved in the development of cardiometabolic disturbances such as dysglycaemia, hyperlipidemia, and obesity [15–17], and it has been described that between 18 and 24 % of adolescents with PCOS have some degree of abnormal glucose metabolism [18–20]. These patients are at increased risk of type 2 diabetes, hypertension, myocardial infarction, angina, and psychiatric diseases [21, 22] in addition to gynecological and obstetrical complications, such as infertility, higher rate for pregnancy loss, gestational diabetes, premature delivery, as well as gynecological and non-gynecological cancers [22–26]. In addition to the aforementioned co-morbidities, patients with PCOS experience a low perceived health quality over lack of symptom improvement, primarily with weight control, hirsutism, acne, menstrual irregularity, and infertility as inferred from qualitative studies [27–29].
Optimal first line treatment of PCOS in adolescents remains controversial. Current Endocrine Society treatment guidelines first recommend lifestyle changes (dietary and exercise modification) followed by either oral contraceptive pills (OCP) to control symptoms of hyperandrogenism or metformin therapy in patients with impaired glucose tolerance or features of metabolic syndrome [10]. However, there is significant variability in clinical practice, depending on whether the physician and patient’s primary goal of treatment is to treat the symptoms of hyperandrogenism or the features of metabolic syndrome [30, 31]. Additionally, in clinical practice anti-androgenic medications such as spironolactone, flutamide, and insulin sensitizing agents such as pioglitazone are used as add-on therapy when OCP or metformin fail to produce the clinically desired outcomes [4, 31], yet the Endocrine Society guidelines do not comment on their use in the adolescent population.
To date, there is one systematic review and meta-analyses in adolescents (in press) that identified low number of low quality evidence from head-to head trials and identified large number of trials that compared metformin to placebo, OCP to placebo, and other PCOS combination therapy [32]. A traditional meta-analysis can only evaluate the direct treatment efficacy of two treatment approaches at a time while a network meta-analysis can provide effect estimates for all direct and indirect treatment comparisons [33]. Therefore, we aim to conduct a network meta-analysis to address the following objectives: (1) assess the effectiveness and safety of using metformin and OCP as monotherapy in adolescents with PCOS; (2) assess the effectiveness and safety of using metformin and/or OCP in combination with pioglitazone, spironolactone, flutamide, and lifestyle interventions, as evaluated across multiple outcomes such as menstrual cycle regulation, improvement in clinical and or biochemical evidence of hyperandrogenism, and metabolic profile in adolescents with PCOS; (3) evaluate the effectiveness of different formulations of OCPs on hirsutism and acne scores.
Methods/design
This systematic review and network meta-analysis protocol is registered on PROSPERO International prospective register of systematic reviews (CRD42015016148). The report will comply with the Preferred Reporting Items for Systematic Review and Network Meta-Analysis Protocols (PRISMA-P) [34].
Eligibility criteria
The search for studies will be limited to randomized clinical trials (RCT) (including all designs such as crossover, cluster, and patient-randomized clinical trials) assessing the efficacy, effectiveness, or safety of different regimen for the treatment of PCOS that enrolled adolescent girls ages 11–19 years. The definition of adolescent age group is based on the widely accepted World Health Organization definition for adolescent [35]. Studies that include both adolescents and adults participants will be included in the review, and upon contact, we will ask authors to provide separate data for the adolescent participants. If we are unable to obtain this information, we will include the study and we will conduct subgroup analyses in order to assess the difference between studies which included only adolescents and studies which included both adolescents and adults. Sub-studies or secondary analysis of reported eligible studies will be excluded to avoid duplication.
The diagnosis of PCOS will be based on the known PCOS diagnostic criteria: Endocrine Society Guidelines, NIH criteria, Rotterdam criteria, and the Androgen Excess Society criteria [6, 7, 10]. We will exclude studies that included normal control participants or patients with other causes of oligomenorrhea or hyperandrogenism, such as hyperprolactinemia, thyroid dysfunction, androgen secreting tumors, or late-onset congenital adrenal hyperplasia.
We will include studies that evaluated single and/or combined interventions, at any dose, such as metformin, OCP, pioglitazone, spironolactone, flutamide, and lifestyle interventions. In order to be included, the study will have had to report the effectiveness of one of these interventions and the intervention effect on one or more of the outcomes of interest.
Our primary outcomes are menstrual cycle regulation and hirsutism scores. The secondary outcomes include acne scores, prevalence of dysglycaemia, BMI, total testosterone level, lipid profile (triglyceride, total cholesterol, LDL, HDL), and adverse events; Table 1 shows the definitions of outcome measures. We chose not to report on pregnancy outcomes because it necessities changing the scope of the review to involve fertility induction medications. Hence, we will exclude studies that only used fertility induction medications and which primary outcome of interest was pregnancy.
Data sources and search strategy
We performed literature search through Ovid MEDLINE, Ovid EMBASE, and Cochrane Central Register of Controlled Trials (CENTRAL) from the database inception to January 2015 using combination of controlled terms, i.e., Medical Subject Heading (MeSH), Emtree terms, and free-text terms with various synonyms for polycystic ovarian syndrome (PCOS), adolescent, metformin, pioglitazone, oral contraceptive pills, flutamide, and lifestyle interventions (Appendix).
We used the randomized controlled trial filter created from McMaster University for Ovid Embase platform and the Cochrane library filter for Ovid Medline platform [36, 37]. These filters provide a good balance between sensitivity and specificity. Our search strategy was developed in liaison with an experienced librarian. No language, publication status, or date limit was used. Additionally, we performed a gray literature search through (1) manual hand search of bibliographies of identified randomized controlled trials and guidelines; (2) trials registries (Clinicaltrials.gov, World Health Organization WHO International Clinical Trials Registry Platform Search Portal, controlled-trials.com and the National Institutes of Health database of funded studies for ongoing or unpublished trials); and (3) conferences preceding and abstracts of the North American and European Endocrine Society and The Society of Adolescent Medicine and Health. Search alerts are set up for monthly notification, and the search will be repeated before the final manuscript submission to identify any new literature. We will contact the authors of unpublished work to establish eligibility and methodological quality of the study.
Study selection
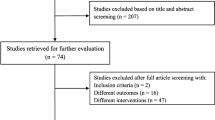
Two reviewers (RA and IF) will independently and in duplicate screen the title and abstract available of identifiable articles to assess its eligibility. In case of disagreement, the full text will be retrieved and reviewed independently by one of the authors (EB), to resolve discrepancy. We will refer to inclusion and exclusion criteria during the screening process. Records of ineligible articles along with the reason for ineligibility will be saved for future reference. Eligible articles citations will be saved in EndnoteX6 library. We will include the PRISMA flow diagram demonstrating the search and screening process (Fig. 1). We will contact authors of primary studies during data extraction to provide any missing information.
Data extraction
The study data will be collected in standardized online data extraction forms (Google forms) according to pre-specified instructions. The data extraction form will include information pertaining to study background, language of publication, country, funding sources, confirm study eligibility, participant ages, PCOS diagnostic criteria, the study design, number of intervention groups, intervention details, number of participants allocated to each intervention group, randomization, concealment of allocation, blinding, length of follow up, analysis type, outcome definition, unit of measurement, ascertainment of the outcome, estimate of intervention effect with confidence interval, and missing follow up data. When studies measure outcomes at more than one time point, we will collect results for the last measurement point in the study. The data extraction form will be pilot tested by all reviewers independently before its use. Four reviewers will perform data extraction (RA, IF, EB, BD), working in pairs independently and in duplicate. In case of disagreement in assessing the methodological quality of the study, we will try to resolve it by consensus. If consensus cannot be reached, a third designated reviewer from the team will be involved.
Assessment of risk of bias in included studies
Two independent reviewers will assess each included study for risk of bias using the modified Cochrane handbook for systematic reviews of interventions tool [37], which assesses six elements: (1) sequence generation, (2) allocation concealment, (3) blinding of participants, personnel and outcome assessors, (4) completeness of follow up, (5) selective outcome reporting, and 6) presence of other biases. Each domain will be assigned a score of “low risk,” “high risk,” or “unclear risk.” We will further categorize the “unclear risk” to “probably low risk” or “probably high risk” in order to give a better understanding of the unclear risk of bias score. We will rate the overall risk of bias score for each study as “high risk” if the study meets more than two criteria for high risk of bias, “moderate risk of bias” if the study meets one to two criteria for high risk of bias, and “low risk of bias” if the study does not meet any high risk of bias criteria [38].
Standard direct comparisons
We will perform a pairwise meta-analysis using R software. Effect estimates and their 95th confidence interval (CI) will be calculated using risk ratio (RR) for binary outcomes and mean difference for continuous outcomes if they are reported using the same metrics; otherwise, estimates reported using different metrics will be converted into standardized mean difference (SMD). We will pool all direct evidence using random-effect meta-analysis with the maximal likelihood (ML) estimator [39]. We will assess for heterogeneity by estimating the variance between studies using the chi-square test and quantify it using the I2 test statistic. We will interpret the I2 using the thresholds set forth by the Cochrane Collaboration [37].
The network meta-analysis
Given that many of the treatment combinations available to treat PCOS were not compared in head-to-head studies, a network meta-analysis (NMA) will be necessary to provide effect estimates for all indirect comparisons [33]. We will perform a multiple treatment comparison to estimate the pooled direct, indirect, and the network estimates (mixed evidence from direct and indirect estimates) for all PCOS interventions on outcomes if the assumptions of homogeneity and similarity are judged to be reasonable. Effect estimates will be presented along with their corresponding 95 % credibility intervals (CrIs); these are the Bayesian analog of 95 % CIs. However, mixed evidence will only be used if the consistency assumption is met.
We will fit a Bayesian random-effect hierarchical model with non-informative priors using vague normal distribution (mean 0, variance 10,000) and adjusting for correlation between effects in multi-arm trials. We will generate posterior samples using Markov Chain Monte-Carlo (MCMC) simulation technique running the analysis in four parallel chains. We will use a series of 100,000 burn-in simulations to allow convergence and then a further 20,000 simulations (succeeding 50,000 simulations saved at an interval of 10 in each chain) to produce the outputs. We will assess model convergence using Gelman and Rubin diagnostic test [40]. The Bayesian model provides flexibility for moderate levels of treatment heterogeneity, sampling variability, and incoherence [41]. This model introduces a random effect representing any changes in the observed treatment effect that may be due to the comparison being made [42]. We will interpret variability in this random effect as incoherence [41]. We will use the node-splitting method to detect incoherence between direct and indirect evidence within a closed loop as well as identify loops with large inconsistency [42, 43]. We will measure the goodness-of-fit of the model using the deviance information criterion (DIC) [42].
To ensure interpretability of the NMA results, we will present the network geometry, the results with probabilistic statements, and also the estimates of interventions effects and corresponding 95 % CrIs, as well as forest plots. We will first rank the intervention and report each interventions’ probability of ranking first (being the best treatment) as well as the surface under the cumulative ranking curve (SUCRA) values [44]. High SUCRA values are expected for the best treatments, and low SUCRA values are expected for the worst treatments.
The above analysis assumes that the interventions are competing (suitable when most components forming an intervention are pharmaceutical and hence cannot go together), so that each combination is considered to be a separate treatment. For example, a combination of components of metformin, flutamide, and exercise forming an intervention and another combination of metformin and exercise forming another intervention are treated as competing interventions and assesses whether one combination is better than another. However, it is possible to perform the network meta-analysis treating these combinations as complex intervention [45]. Such an analysis fits a similar hierarchical regression model but considers multiple components of an intervention as dummy variables in the same model. Hence, the analysis allows the estimation of the effects and ranking of a combination of all possible and appropriate components. Thus, it is possible to explore such a combination that could have been the best for the treatment of PCOS but has never been tested before in any trial. Further, such an analysis allows the assessment of additive or multiplicative (interaction) effects between two or more components if sufficient data are available. We will re-analyze the data under complex intervention approach as well [45] to assess if there exists a potentially better combination of components which have been ever or never assessed.
We will perform the Bayesian network meta-analysis in JAGS (version 3.4.0) or WinBUGS software (version 1.4.3, MRC Biostatistics Unit, Cambridge, UK) interfacing through R software.
Meta-regression
In case there is significant heterogeneity and inconsistency, we will use meta-regression to explain the heterogeneity, provided we have enough data to do so; otherwise, we will perform subgroup analyses. We will perform meta-regression using study level covariates: methodological quality (high risk of bias versus low risk of bias), participant’s average age, BMI status (obese and/or overweight BMI ≥25 kg/m2 versus normal <25 kg/m2), homeostatic model assessment (HOMA-IR) (high and moderate ≥3 versus low <3), medication dose, length of treatment (≥3 months versus <3 months), use of ultrasound to document polycystic ovaries (used versus not used), and studies that included young adults versus adolescents only to examine the improvement or change in model fit after covariates are included into the model. We will also perform a subgroup analysis to evaluate the effectiveness of different oral formulations of contraceptive pill on changes of hirsutism and acne scores.
Rating the confidence in estimates of the effect in NMA
The confidence in the estimates (quality of evidence) for each reported outcome will be assessed independently by two reviewers (RA, IF) using the Grading of Recommendations Assessment, Development, and Evaluation Working Group (GRADE Working Group) approach; see Fig. 2 for the flow of quality assessment [46]. The quality of evidence is categorized by GRADE into four levels: high quality, moderate quality, low quality, and very low quality. For the direct comparisons, we will assess and rate each outcome based on the five GRADE categories: risk of bias, imprecision, inconsistency, indirectness, and publication bias [47].
For the assessment of confidence in the estimates obtained in the NMA, we will use the recent approach recommended by the GRADE working group [48]. We will assess and rate the confidence in all the indirect comparisons, if available, obtained from first order loops following the five GRADE categories used for assessing the direct comparisons in addition to the intransitivity assessment. Then, we will rate the confidence in each NMA effect estimate using the higher quality rating when both direct and indirect evidence are present. However, the estimate can be rated down for incoherence [48].
Discussion
PCOS treatment in adolescents poses clinical challenges to patients and physicians. To our best knowledge, our study will be the first NMA in adolescents to investigate the effectiveness and safety of using metformin and OCP as monotherapy as well as in combination with pioglitazone, spironolactone, flutamide, or lifestyle interventions.
Our planned approach for this review has many strengths. We will implement a wide search strategy that included published and unpublished work. As adolescent women share some similar physiology with adult women and in an effort to overcome publication bias, we also plan to include studies that included adolescents and young adults. Additionally, we aim to report on many patient important outcomes as inferred from previous qualitative research. Similar to previous systematic reviews in adults with PCOS, we anticipate that we will identify studies which use different definitions of PCOS, various definitions for outcome measures of interest, and small sample sizes [49]. These factors may pose potential limitations to our study.
We hope that this review will provide hierarchical evidence to improve patient care, help unify the treatment approaches among specialists, and encourage research for new therapeutic options.
Abbreviations
- BMI:
-
body mass index
- DIC:
-
deviance information criterion
- GRADE:
-
Grading of Recommendations Assessment, Development and Evaluation
- NIH:
-
National Institutes of Health
- NMA:
-
network meta-analysis
- OCP:
-
oral contraceptive pill
- PCOS:
-
polycystic ovarian syndrome
- RCT:
-
randomized controlled trials
- T2DM:
-
type two diabetes mellitus
References
Li R, Zhang Q, Yang D, Li S, Lu S, Wu X, et al. Prevalence of polycystic ovary syndrome in women in China: a large community-based study. Hum Reprod. 2013;28(9):2562–9.
Christensen SB, Black MH, Smith N, Martinez MM, Jacobsen SJ, Porter AH, et al. Prevalence of polycystic ovary syndrome in adolescents. Fertil Steril. 2013;100(2):470–7.
Yildiz BO, Bozdag G, Yapici Z, Esinler I, Yarali H. Prevalence, phenotype and cardiometabolic risk of polycystic ovary syndrome under different diagnostic criteria. Hum Reprod. 2012;27(10):3067–73.
Roe AH, Dokras A. The diagnosis of polycystic ovary syndrome in adolescents. Rev Obstet Gynecol. 2011;4(2):45–51.
Kumarapeli V, Seneviratne Rde A, Wijeyaratne C. Health-related quality of life and psychological distress in polycystic ovary syndrome: a hidden facet in South Asian women. BJOG. 2011;118(3):319–28.
Rotterdam ESHRE/ASRM-Sponsored PCOS Consensus Workshop Group. Revised 2003 consensus on diagnostic criteria and long-term health risks related to polycystic ovary syndrome. Fertil Steril. 2004;81(1):19–25.
Azziz R, Carmina E, Dewailly D, et al. The Androgen Excess and PCOS Society criteria for the polycystic ovary syndrome: the complete task force report. Fertil Steril. 2009;91(2):456–88.
Zawadski J, Dunaif A. Diagnostic criteria for polycystic ovary syndrome: towards a rational approach. In: Dunaif A, Givens J, Haseltine F, Merriam G, editors. Polycystic Ovary Syndrome. 1st ed. Boston: Blackwell Scientific Publications; 1992. p. 377–84.
Hardy TS, Norman RJ. Diagnosis of adolescent polycystic ovary syndrome. Steroids. 2013;78(8):751–4.
Legro RS, Arslanian SA, Ehrmann DA, Hoeger KM, Murad MH, Pasquali R, et al. Diagnosis and treatment of polycystic ovary syndrome: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2013;98(12):4565–92.
Ehrmann DA. Polycystic ovary syndrome. N Engl J Med. 2005;352(12):1223–36.
Goodarzi MO, Dumesic DA, Chazenbalk G, Azziz R. Polycystic ovary syndrome: etiology, pathogenesis and diagnosis. Nat Rev Endocrinol. 2011;7(4):219–31.
Pauli JM, Raja-Khan N, Wu X, Legro RS. Current perspectives of insulin resistance and polycystic ovary syndrome. Diabet Med. 2011;28(12):1445–54.
Dunaif A. Insulin resistance and the polycystic ovary syndrome: mechanism and implications for pathogenesis. Endocr Rev. 1997;18(6):774–800.
Rehme MF, Pontes AG, Goldberg TB, Corrente JE, Pontes A. Clinical manifestations, biochemical, ultrasonographic and metabolic of polycystic ovary syndrome in adolescents. Rev Bras Ginecol Obstet. 2013;35(6):249–54.
Li L, Chen X, He Z, Zhao X, Huang L, Yang D. Clinical and metabolic features of polycystic ovary syndrome among Chinese adolescents. J Pediatr Adolesc Gynecol. 2012;25(6):390–5.
Bekx MT, Connor EC, Allen DB. Characteristics of adolescents presenting to a multidisciplinary clinic for polycystic ovarian syndrome. J Pediatr Adolesc Gynecol. 2010;23(1):7–10.
Gooding HC, Milliren C, St Paul M, Mansfield MJ, DiVasta A. Diagnosing dysglycemia in adolescents with polycystic ovary syndrome. J Adolesc Health. 2014;55(1):79–84.
Flannery CA, Rackow B, Cong X, Duran E, Selen DJ, Burgert TS. Polycystic ovary syndrome in adolescence: impaired glucose tolerance occurs across the spectrum of BMI. Pediatr Diabetes. 2013;14(1):42–9.
Palmert MR, Gordon CM, Kartashov AI, Legro RS, Emans SJ, Dunaif A. Screening for abnormal glucose tolerance in adolescents with polycystic ovary syndrome. J Clin Endocrinol Metab. 2002;87(3):1017–23.
Mani H, Levy MJ, Davies MJ, Morris DH, Gray LJ, Bankart J, et al. Diabetes and cardiovascular events in women with polycystic ovary syndrome: a 20-year retrospective cohort study. Clin Endocrinol. 2013;78(6):926–34.
Hart R, Doherty DA. The potential implications of a PCOS diagnosis on a woman's long-term health using data linkage. J Clin Endocrinol Metab. 2015;100(3):911–9. jc20143886.
Boomsma CM, Eijkemans MJ, Hughes EG, Visser GH, Fauser BC, Macklon NS. A meta-analysis of pregnancy outcomes in women with polycystic ovary syndrome. Hum Reprod Update. 2006;12(6):673–83.
Barry JA, Azizia MM, Hardiman PJ. Risk of endometrial, ovarian and breast cancer in women with polycystic ovary syndrome: a systematic review and meta-analysis. Hum Reprod Update. 2014;20(5):748–58.
Shen CC, Yang AC, Hung JH, Hu LY, Tsai SJ. A nationwide population-based retrospective cohort study of the risk of uterine, ovarian and breast cancer in women with polycystic ovary syndrome. Oncologist. 2015;20(1):45–9.
Gottschau M, Kjaer SK, Jensen A, Munk C, Mellemkjaer L. Risk of cancer among women with polycystic ovary syndrome: a Danish cohort study. Gynecol Oncol. 2015;136(1):99–103.
Jones GL, Hall JM, Lashen HL, Balen AH, Ledger WL. Health-related quality of life among adolescents with polycystic ovary syndrome. J Obstet Gynecol Neonatal Nurs. 2011;40(5):577–88.
Crete J, Adamshick P. Managing polycystic ovary syndrome: what our patients are telling us. J Holist Nurs. 2011;29(4):256–66.
Nasiri Amiri F, Ramezani Tehrani F, Simbar M, Montazeri A, Mohammadpour Thamtan RA. The experience of women affected by polycystic ovary syndrome: a qualitative study from Iran. Int J Endocrinol Metab. 2014;12(2):e13612.
Conway G, Dewailly D, Diamanti-Kandarakis E, et al. European survey of diagnosis and management of the polycystic ovary syndrome: results of the ESE PCOS Special Interest Group's Questionnaire. Eur J Endocrinol. 2014;171(4):489–98.
Auble B, Elder D, Gross A, Hillman JB. Differences in the management of adolescents with polycystic ovary syndrome across pediatric specialties. J Pediatr Adolesc Gynecol. 2013;26(4):234–8. Date of Publication: August 2013.; 2013.
AlKhalifah R, Florez ID, Thabane L, Dennis B, Bassilious E. Metformin versus oral contraceptive pills for the management of polycystic ovarian syndrome in adolescents: systematic review and meta-analysis. PROSPERO International prospective register of systematic reviews2015.
Mills EJ, Thorlund K, Ioannidis JP. Demystifying trial networks and network meta-analysis. BMJ (Clinical research ed). 2013;346:f2914.
Shamseer L, Moher D, Clarke M, Ghersi D, Liberati A, Petticrew M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. Bmj. 2015;349:g7647.
Sacks D; Canadian Paediatric Society. Age limits and adolescents. Paediatrics & Child Health. Nov 2003;8(9):577.
Search Filters for MEDLINE in Ovid Syntax and the PubMed translation. http://hiru.mcmaster.ca/hiru/HIRU_Hedges_MEDLINE_Strategies.aspx, 2015.
Collaboration TC. The Cochrane handbook for systematic reviews of interventions version 5.1.0. 2011.
Guyatt G, Busse J. Commentary on tool to assess risk o f bias in cohort studies. http://www.evidencepartners.com/resources/
Cornell JE, Mulrow CD, Localio R, et al. Random-effects meta-analysis of inconsistent effects: a time for change. Ann Intern Med. 2014;160(4):267–70.
Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Stat Sci. 1992;7:457–72.
Lumley T. Network meta-analysis for indirect treatment comparisons. Stat Med. 2002;21(16):2313–24.
Higgins J. Identifying and addressing inconsistency in network meta-analysis. Paper presented at: Cochrane comparing multiple interventions methods group Oxford training event 2013.
Dias S, Welton NJ, Caldwell DM, Ades AE. Checking consistency in mixed treatment comparison meta-analysis. Stat Med. 2010;29(7–8):932–44.
Salanti G, Ades AE, Ioannidis JP. Graphical methods and numerical summaries for presenting results from multiple-treatment meta-analysis: an overview and tutorial. J Clin Epidemiol. 2011;64(2):163–71.
Welton NJ, Caldwell DM, Adamopoulos E, Vedhara K. Mixed treatment comparison meta-analysis of complex interventions: psychological interventions in coronary heart disease. Am J Epidemiol. 2009;169(9):1158–65.
Guyatt G, Oxman AD, Akl EA, Kunz R, Vist G, Brozek J, et al. GRADE guidelines: 1. Introduction-GRADE evidence profiles and summary of findings tables. J Clin Epidemiol. 2011;64(4):383–94.
Guyatt GH, Oxman AD, Kunz R, Woodcock J, Brozek J, Helfand M, et al. GRADE guidelines: 8. Rating the quality of evidence—indirectness. J Clin Epidemiol. 2011;64(12):1303–10.
Puhan MA, Schunemann HJ, Murad MH, et al. A GRADE working Group approach for rating the quality of treatment effect estimates from network meta-analysis. BMJ. 2014;349:g5630.
Costello M, Shrestha B, Eden J, Sjoblom P, Johnson N. Insulin-sensitising drugs versus the combined oral contraceptive pill for hirsutism, acne and risk of diabetes, cardiovascular disease, and endometrial cancer in polycystic ovary syndrome. Cochrane Database Syst Rev 2007;1:CD005552.
Acknowledgements
We would like to thank Mrs. Neera Bhatnagar, McMaster Health Sciences Librarian for her invaluable assistance in refining the search strategy.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
RA conceptualized and designed the study, drafted and critically reviewed the manuscript, and approved the final manuscript as submitted. IF conceptualized and designed the study, critically reviewed the manuscript, and approved the final manuscript as submitted. BD designed the study, drafted and critically reviewed the manuscript, and approved the final manuscript as submitted. EB conceptualized the study, designed the study, critically reviewed the manuscript, and approved the final manuscript as submitted. LT designed the study, critically reviewed the manuscript, and approved the final manuscript as submitted. BN drafted and critically reviewed the manuscript and approved the final manuscript as submitted. All authors read and approved the final manuscript.
Appendix
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Al Khalifah, R.A., Flórez, I.D., Dennis, B. et al. The effectiveness and safety of treatments used for polycystic ovarian syndrome management in adolescents: a systematic review and network meta-analysis protocol. Syst Rev 4, 125 (2015). https://doi.org/10.1186/s13643-015-0105-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13643-015-0105-4