Abstract
Background
Virtual reality (VR) and augmented reality (AR) are rapidly developing technologies that offer a wide range of applications and enable users to experience digitally rendered content in both physical and virtual space. Although the number of studies about the different use of VR and AR increases year by year, a systematic overview of the applications of these innovative technologies in intensive care medicine is lacking. The aim of this systematic review was to provide a detailed summary of how VR and AR are currently being used in various areas of intensive care medicine.
Methods
We systematically searched PubMed until 1st March 2023 to identify the currently existing evidence for different applications of VR and AR for both health care providers in the intensive care unit and children or adults, who were in an intensive care unit because of a critical illness.
Results
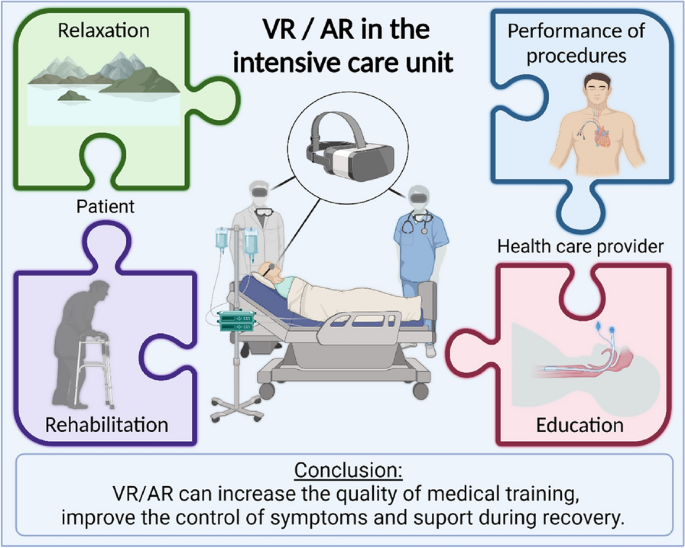
After screening the literature, a total of 59 studies were included. Of note, a substantial number of publications consists of case reports, study plans or are lacking a control group. Furthermore, study designs are seldom comparable. However, there have been a variety of use cases for VR and AR that researchers have explored. They can help intensive care unit (ICU) personnel train, plan, and perform difficult procedures such as cardiopulmonary resuscitation, vascular punctures, endotracheal intubation or percutaneous dilatational tracheostomy. Patients might benefit from VR during invasive interventions and ICU stay by alleviating stress or pain. Furthermore, it enables contact with relatives and can also assist patients in their rehabilitation programs.
Conclusion
Both, VR and AR, offer multiple possibilities to improve current care, both from the perspective of the healthcare professional and the patient. It can be assumed that VR and AR will develop further and their application in health care will increase.
Graphic Abstract
Similar content being viewed by others
Background
Virtual reality (VR) and augmented reality (AR) are emerging technologies that allow various applications, ranging from immersive entertainment or educational experiences to medical care. VR is defined as the user’s complete immersion into a virtual three-dimensional environment, while AR retains the connection to the real world but supplements it with virtual elements to increase information [1]. Both VR and AR necessitate special VR/AR glasses for the user. Medical applications are growing and there are already areas that have been intensively researched, such as cardiovascular care [2] or neurosurgery [3]. The technologies are also increasingly being used in intensive care medicine and might positively influence this area of medicine from the perspectives of both medical staff and patients [4]. In a safe environment, VR can help health care providers in acquiring and practice complex intensive care procedures [5]. Augmented reality can also support the user both before and during procedures by integrating various additional information into reality [6]. From the patient´s point of view, VR can help to reduce stress during the stay in the intensive care unit through different means, such as distraction from pain, for both adults [7] and children [8]. In addition, by combining virtual reality and gaming, it is possible to improve cognitive and motor skills [9]. Thus, VR and AR could potentially be used at different time points by several users and for different purposes.
The present systematic review presents the current status of the application of VR and AR in critical care medicine. Based on a literature review, we summarized the current state-of-the-art.
Methods
Literature search
We systematically searched PubMed databases for publications up until 1st March 2023, applying the following keywords: “VR” and “ICU”, “virtual reality” and “ICU”, "virtual reality" and "critical care", “virtual reality” and “intensive care unit”, "augmented reality" and "ICU, “augmented reality" and "critical care", "augmented reality" and "intensive care", “mixed reality” and “ICU”, "mixed reality" and "critical care", “mixed reality” and “intensive care unit” (Appendix 1) to identify all published studies reporting on the application of virtual or augmented reality in the intensive care unit.
Eligibility and selection criteria
Eligible articles were: randomized controlled trials, nonrandomized trials, observational studies (cases and controls, cohort, and cross-sectional studies), proof-of-concept studies, study protocols, and case reports or series. All studies that met the following criteria were included: (1) type of participants: subjects were either health care providers in the intensive care unit or children or adults, who were in an intensive care unit because of a critical illness. (2) Type of interventions: VR or AR (3) Language: studies published in English or German, both in full text or abstract-only formats.
Data abstraction
Three independent reviewers screened all articles using the above-mentioned inclusion criteria. An independent fourth investigator was involved in the case of discrepancies in the extraction and assessment of the data. The following data were abstracted: author’s name, year of publication, study type, sample size, inclusion criteria, patient characteristics (age, medical background, and treatment), use of AR/VR, frequency of application, and outcomes.
Data synthesis
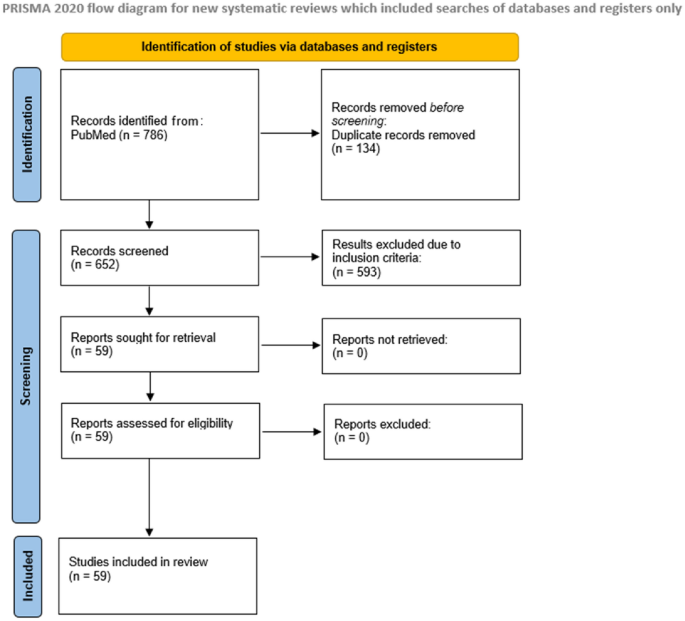
The key characteristics and results of included studies were summarized and synthesized using tables and complemented by a qualitative summary. This study was conducted and reported following the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines for reporting systematic reviews [10].
Results
The initial search strategy identified 786 articles (Fig. 1). After the screening on predefined criteria and removal of duplicates, 59 studies were included.
There were 48 studies about the application of VR: 12 randomized control trials, 2 nonrandomized trials, 26 observational studies, 2 proof-of-concept studies, 4 study protocols and 2 case reports, and 11 studies about the use of AR: 3 randomized control trial, 7 observational studies, and 1 case series.
Table 1 and Table 2 summarize all studies about the use of VR (Table 1) and AR (Table 2) in intensive care medicine that were included in the search strategy. So all relevant studies are described and commented on in a systematic review. Part 1 focuses on VR and Part 2 on AR. For each perspective, we discuss different applications, both in the adult and pediatric intensive care unit.
Part 1: VR
VR as a tool for health care providers to improve clinical practice
Adult intensive care medicine
VR might assist in educating and training healthcare professionals [2] (Fig. 2) as intensive care treatment strategies are often complex and require not only theoretical knowledge but also practical preparation. In a randomized controlled trial of 381 participants, Nas et al. evaluated the value of VR for learning cardiopulmonary resuscitation (CPR). They reported comparable chest compression rates but an inferior compression depth compared with face-to-face training [11]. The research on VR/AR in this field is generally very heterogeneous [12]. Wolff et al. developed a VR training environment to improve the traditional training for extracorporeal membrane oxygenation (ECMO) [5]. Bronchoscopy is another important tool for diagnostic and therapeutic purposes in ICU patients and performing this procedure can be challenging. Colt et al. created a virtual reality bronchoscopy simulation. Through the acquired skills after VR training, five novice physicians were comparable to four experienced physicians regarding dexterity, speed, and accuracy in the model [13]. In a prospective randomized study with 60 healthcare providers, Chiang et al. evaluated 15-min VR-based learning on tracheostomy care. The use of VR materials increased significantly participants' self-efficacy (increased familiarity, more self-confidence, and less anxiety) and the positive impact persisted until 3 to 4 weeks later [14].
Pediatric intensive care unit
Caring for patients in the neonatal and pediatric intensive care units (PICU) can be particularly challenging [15], and aspects such as performance, knowledge, self-efficacy, and learner satisfaction are of great importance. In terms of these endpoints, Yu et al. evaluated the effects of a VR simulation program on nursing students. In three scenarios, the interventional group (n = 25) experienced a 40-min VR simulation and routine practice, and the control group (n = 25) only did routine practice. The use of VR resulted in a significant increase in high-risk neonatal infection control performance, self-efficacy, and learner satisfaction [16]. Yang et al. investigated in a non-randomized controlled study the impact of VR neonatal resuscitation program among others on knowledge, problem-solving, or degree of anxiety [17]. The VR group (n = 29) participated in a neonatal resuscitation gamification program, while the simulation group (n = 28) participated in high-fidelity simulations of neonatal resuscitation and online lectures. The control group (n = 26) had only online lectures on neonatal resuscitation. VR and simulation groups achieved significantly higher levels of neonatal resuscitation knowledge and learning motivation than the control group. Furthermore, VR application was found to be effective in increasing problem-solving ability and self-confidence compared to the others groups. However, anxiety was lowest in the simulation group. Ralston et al. investigated VR-based simulation of two scenarios: ectopic junctional tachycardia and low cardiac output syndrome in the early postoperative period and acute respiratory failure in a patient with suspected coronavirus disease [15]. All six pediatric cardiac critical care physicians successfully navigated the VR environment and met the critical endpoints such as connect the patient to the pacemaker and correctly overdrive pace or intubate the patient and connect to the ventilator. Farra et al. compared the success of VR training versus web-based clinical updates for emergency evacuation in a newborn ICU. Although there was no significant difference in terms of cognitive assessments and self-efficacy, the VR group performed statistically and clinically better in the live exercise [18]. Agasthya et al. evaluated a VR tutorial for endotracheal intubation. Participants of the interventional group completed a 19-min immersive guiding and the control group listed the steps from memory. Both groups demonstrated their skills with traditional manikins and were scored on a 24-point checklist. There was no significant difference between the groups [19].
VR as a tool for healthcare providers to reduce stress
Stress is a common phenomenon in the intensive care unit for both patients and health care providers. In a study with 66 ICU nurses investigated Nijland et al. the effect of VR on perceived stress levels. Sixty-two percent of the ICU nurses, who used VR-Relaxation during their breaktime reported VR to be helpful to reduce stress [20]. Bodet-Contentin et al. also showed in a study of 88 intensive unit caregivers that the use of VR could improve the efficiency of the breaks [21].
Patient experiences with VR during and after ICU-stay
Adult intensive care
From the patients' perspective, intensive care treatment is associated with a number several symptoms such as pain [1]. If one now modulates attention, environmental conditions, and mood with VR, this can reduce the attention devoted to pain [22] (Fig. 3). Mosso-Vázquez et al. used VR to present different immersive environments such as Cliff or Dream Castle to 67 patients after cardiac surgery [23]. The results were evaluated with a Likert scale and almost 90% of the patients reported a decreased level of pain experienced post-therapy with VR. Esumi et al. evaluated VR in a patient whose pain after a fasciotomy for acute compartment syndrome could not be adequately controlled and opioid-related side effects, such as respiratory depression, have occurred. The use of VR led to a 25–75% dose reduction in fentanyl administration and the concomitant alleviation of respiratory depression [24]. In a randomized, prospective study of 200 cardiac surgery patients, Laghlam et al. demonstrated that VR application was equivalent to conventional treatment with oxygen and nitrous oxide in terms of reported pain scores during removal of chest tube [25]. Markus et al. focused on the technical and procedural feasibility of VR in daily routine and showed that the VR application takes almost an hour for setup, instruction, VR therapy, and cleaning. Especially in smaller centers such programs would be difficult to implement due to lack of staff and resources [26]. Hoffman et al. demonstrated in their study with 11 burn-injured patients the positive effects of 3-min VR application during wound care on pain relief and a positive correlation between the immersive strength of VR and its pain-relieving effect [27]. However, Faber et al. showed that the effect would be less after three consecutive days [28].
Due to discomforts such as aggressive noises, lights, and a lack of information, the intensive care units are often associated with negative feelings such as anxiety or stress for patients [7]. Merliot‑Gailhoustet et al. investigated in a randomized trial E‑CHOISIR (Electronic‑CHOIce of a System for Intensive care Relaxation) the effects of different electronic relaxation devices on the reduction of overall discomfort, pain, anxiety, dyspnea, thirst, lack of rest feeling and stress in sixty ICU-patients. The patients received four relaxation sessions (standard relaxation with TV or radio, music therapy, and two VR systems with real or synthetic motion pictures). In the group with synthetic motion pictures the overall discomfort, pain, and stress could be significant decrease, while the real motion pictures were associated with a reduction in lack of rest. Both VR-Systems led to a significant decrease in anxiety. Three adverse events might occur: claustrophobia, dyspnea, and agitation. However, in general cybersickness (occurrence of symptoms such as headaches or nausea during VR use) rarely occurred [29].
Haley et al. evaluated in a pilot study 5-min VR sessions in 10 mechanically ventilated patients. VR therapy proved to be a potential means of managing anxiety in this patient group without the occurrence of predefined safety events or cybersickness [30]. The quality of sleep could also be positively influenced by the use of VR. In a study with 100 patients, it was shown that due to the VR application, the sleep quality was significantly better but the total sleep time and light sleep time did not differ between the groups [31].
Hypnosis has been used in the management of acute and chronic pain for a long time [32]. Rousseaux et al. tested a “virtual reality hypnosis” in patients undergoing cardiac surgery comparing VR to control patients, hypnosis without VR, and VR without hypnosis. All four techniques were used one day before and one day after surgery [33, 34]. However, in their randomized-controlled study with 100 patients, there were no significant differences regarding the outcome measures (anxiety, pain, fatigue, relaxation, physiological parameters, and opioid use) between the groups [35].
To evaluate the usefulness of VR for reducing sensory overload and deprivation in the ICU Jawed et al. put VR goggles on 15 ICU patients for 15 min and exposed them to relaxing beach videos with nature sound effects. Most patients tolerated the headsets well and reported the positive effects of VR therapy on anxiety and stress [36]. Naef et al. investigated how long visual and auditory stimuli should be provided to intensive care unit patients. In their study, visual stimuli should not exceed 10 – 15 min, while auditory stimuli should not exceed one hour to prevent negative side effects [37].
Suvajdzic et al. used a combined approach to prevent delirium in ICU patients—The DREAMS system (Digital Rehabilitation Environment-Altering Medical System) [38], which combined an immersive digital reality acquisition system with a measurement system. The VR environment consisted of a commercially available VR headset. The measurement was sophisticated: it includes physiologic sensors 3-axis wearable accelerometers, a video camera, and environmental sensors for light and noise exposures for measurement of movement, physiologic and emotional responses to assess the movement, physiologic and emotional responses. In addition, an electroencephalogram sensor measures the sleep quality and response to therapy [39]. The DREAMS system has so far only been used in a small feasibility study with 59 non-intubated ICU patients and was well-received but there was no significant effect on physiologic measures, pain, or sleep [40].
Family support also plays a big role for the patients in the ICU [41]. Therefore, He et al. used the fifth generation plus virtual reality (5G + VR) equipment to establish visitation channels for patients and their families during the COVID-19 pandemic. They showed in a cohort study with 141 ICU patients that after 5G + VR visitations, the Hospital Anxiety Depression Scale (HADS) decreased significantly, along with a significant reduction in the proportion of delirium [42].
ICU patients often experience not only delirium but also other neurocognitive impairments [43]. In this context, Turon et al. examined in a pilot study the benefits of VR-assisted early neurocognitive stimulation in 20 critically ill adult patients [44]. The simulation includes a virtual avatar that accompanies patients, helped them orient to time, delivered instructions, motivated them to complete exercises, and encouraged them to relax. This application was found to be feasible, safe, and reliable, and stimulated cognitive functions. Navarra-Ventura et al. evaluated also a VR-based neurocognitive intervention during ICU stay in 34 critically ill patients. A 1-month follow-up that these patients had better working memory scores and showed up to 50% less non-specific anxiety and depression compared to the control group [45].
Early mobilization of ICU patients improves patient outcomes and reduced hospital stay length [46]. Gomes et al. used Nintendo Wii™ in 60 adult ICU patients to increase their physical activity [47]. Activity levels were light to moderate on a modified Borg scale and a majority of patients expressed a desire to play the videogame during their upcoming physical therapy sessions. The study from Parke et al. utilized a similar approach: Xbox Kinect Jintronix software targeting arm, leg, and trunk strength, range of motion, and endurance in 20 adult ICU patients [48]. Most patients found the activity enjoyable, and easy to understand, as well as motivating to continue participating.
ICU stay constitutes a considerable psychological burden for patients. In several studies, Valke et al. investigated the effects of ICU-specific virtual reality on mental health [49,50,51,52]. In one of them with 104 patients the group evaluated three and six months after ICU treatment, repetition of 14-min VR modules about ICU treatment improves subjective well-being and quality of life. VR resulted in a reduction of post-traumatic stress disorder, and depression scores, and the effect was still present six months after exposure. Although the mental health was also initially better this effect was no longer observed after six months.
Pediatric intensive care unit
The stay in the pediatric intensive care unit (PICU) can be an emotional and stressful experience for both children and parents [53]. In a pilot study with 32 critically ill children, Badke et al. investigated the feasibility and satisfaction of virtual reality in the PICU. All participants enjoyed using the technology, and 84% expressed interest in using it for a longer period. The positive effects were also observed among the parents, with 100% reporting satisfaction while watching their children use virtual reality. Moreover, parents reported that their children were calmed by VR [54]. In another study by this group with 115 critically ill children, the positive influence of VR on engagement and physiologic effects such as heart rate variability was confirmed [55].
Kucher et al. [56] and Hoffmann et al. [8] evaluated VR for better pain management and both were able to show positive effects. Abdulsatar et al. investigated the feasibility and safety of using Nintendo Wii™ in a pilot-trials with 12 critically ill children [57]. The application improved upper limb activity but grip strength did not change significantly from baseline. Lai et al. used VR on two adolescents suffering from Covid-19. The patients could choose from various active games such as boxing and non-active games such as racing. The authors conclude that VR gaming improved participants’ affect and alertness, motivating them to engage more in early mobilization therapy [58].
The hospital-induced separation between the child and the family is difficult for both sides. Therefore, Tallent et al. also established a VR-based virtual visit and the staff surveys showed that the application did not lead to an increased duration of the visit. Endpoints on parental perception are not reported, but VR appeared to be very well accepted by the treatment team in this study [59].
Part 2: AR
AR as a tool to assist ICU procedures
Adult intensive care unit
AR can also help health care providers in the implementation of procedures in the ICU. Huang et al. evaluated the AR application during central venous line placement. The AR intervention consisted of a 5- to 10-min hands-on instructional course to allow familiarity with the AR equipment and—during central line placement in a manikin—a video that repeated essential steps. There was no difference between the groups regarding the meantime for placement or procedure time, but a significantly higher adherence level to the checklist between the two groups favoring the AR group was observed [60]. Fumagalli et al. evaluated the value of AR for venous puncture in 103 ICU patients. The use of AR reduced the incidence of hematomas and anxiety levels but did not reduce the duration of the procedure or the number of attempts [61]. Morillas Perez et al. also confirmed the positive influence of AR on vascular puncture in a study with 6 operators, who performed a total of 76 punctures. AR application resulted in higher accuracy and better quality of the images and eliminated variability between operators and sonographers. Furthermore, it provided more comfort as the hands are free and the view remains focused on the work area [62]. In a controlled trial with 32 ICU trainees, Alismail et al. investigated the use of AR during the endotracheal intubation of a manikin. The use of AR, where the essential steps were repeated, resulted in a longer need of time to intubate and ventilate but demonstrated higher compliance with the checklist [63]. Heo et al. randomized 30 nurses without experience in mechanical ventilation into 2 training groups: with or without AR. Compared to the control group, the AR group requested less assistance and showed higher self-confidence [64]. Gan et al. evaluated in 6 cases the AR for percutaneous dilatational tracheostomy and again it was confirmed that this new technology allowed the procedure to be carried out successfully [65]. A pilot study by Zackoff et al. evaluated AR in two critical situations. AR not only improved the ability to assess many factors such as the mental or respiratory status of the patient, but also had a positive impact on the recognition of critical situations such as shock, apnea, and hypoxemia. However, the detection of cardiac arrest was not significantly better [66]. To improve the training of future perfusionists in the field of extracorporeal circulation (ECC) Yamada et al. developed an AR program for smartphones or tablets [67]. The AR training might be beneficial for future perfusionists, but currently there has not yet been a clinical study examining the use of the app.
Pediatric intensive
Care unit
Dias et al. also evaluated AR to improve performing endotracheal intubation. Forty-five participants were randomly divided into three groups and used for intubation on a manikin either direct laryngoscopy or indirect video laryngoscopy or AR-assisted video laryngoscopy. AR-assisted video laryngoscopy was comparable to indirect video laryngoscopy but resulted in increased safety compared with direct laryngoscopy [68]. The dosage of the drugs used during critical situations in the ICU is often based on weight. Therefore, Scquizzato et al. developed a smartphone app that estimates child weight using the smartphone camera and augmented reality (AR). So far, it has not been evaluated in clinical trials [69].
Limitations
Although the number of studies about the use of VR or AR significantly increases year by year, attempts at systematic synthesis of evidence such as the present study are limited by scarcely comparable methods, devices, and protocols [70]. A limited number of prospective randomized controlled trials are currently available in this field and the data are generally very heterogeneous. Thus, quantitative synthesis by meta-analysis and the use of methods to assess the risk of bias in the included studies is hardly possible. Several sources of bias could affect the validity and reliability of studies investigating the use of VR and AR in the ICU. The sample size of the studies is often small and not representative of the overall population of ICU patients, what increases the selection bias. Moreover, the inclusion of older adults may be limited by the fact that they are less familiar with new technologies such as VR/AR and may be hesitant or resistant to trying these innovation methods. It is important that VR/AR interfaces can accommodate age-related changes, such as visual impairments, hearing impairments, and decreased dexterity, to facilitate use the technologies. The performance bias can be high because most studies are not blinded and this can influence the behavior of participants. Furthermore, the outcomes are in most studies subjective and dependent on observation. Establishment of objective evaluation criteria is necessary to improve these aspects. However, there are some subjects such as post-traumatic disorders that are inherently complex and multifaceted, making it difficult to develop such criteria that capture all relevant factors. In addition, a common challenge is the diversity of applied VR and AR systems. This can affect not only the complexity of the application but also the tolerance of the users. VR/AR tools can provide varying levels of user comfort, performance, and immersion. This can make it difficult to reproduce the data, which can reduce the reliability and comparability of the research results. Furthermore, only a few studies describe exactly how time-intensive the application of the technologies can be. This, combined with differences in cost and accessibility, may impact the widespread application of VR/AR.
The present systematic review found the same difficulties for intensive and critical care medicine. In upcoming studies, the protocols should be harmonized as far as possible to expand significant clinical knowledge. The development of a core outcome set plays an important role for future systematic research about VR and AR. This would allow better comparability of studies, improve the quality and relevance of results, and facilitate evidence synthesis and meta-analyses. By providing this information, it would be even more possible to generalize the results and to understand the benefits and limitations of VR in the clinical setting.
Summary
This review showed that VR and AR offer new possibilities for many aspects of daily intensive care medicine. There are several approaches to supporting traditional clinical training and taking medical education to the next level. They provide a safe environment to practice procedures such as bronchoscopy [13], without risking harm to patients. In the ICU, the health care providers often have to make quick decisions, and by simulating different scenarios using VR such as low cardiac output syndrome [15], the critical decision-making skills can be improved. In addition, the technologies can positively influence aspects such as knowledge or self-efficacy [14, 16], and the stress level of hospital staff [20]. However, the studies also have shown that VR/AR applications do not lead to a significant improvement in the performance of invasive procedures such as central line placement [60]. Furthermore, VR-based CPR training compared with traditional training provided inferior results [71].
Although there is currently limited data on clinically relevant outcomes, combining traditional training with VR/AR applications may be the way to achieve the best results in daily clinical practice.
Several studies confirmed that VR also might be an effective tool for pain management. VR allows us to generate a virtual environment to distract patients from their pain for example after surgery [23] or during wound care [8, 27]. As a result, VR therapy can reduce the need for pain medication and thus prevent the occurrence of undesirable side effects of traditional therapy [24]. Furthermore, the use of VR can lower the stress level and reduce anxiety during the stay in the ICU [36, 72]. This can have a positive impact on sleep quality [31], development of delirium [42], and cognitive impairment [45]. Six studies have also shown that VR can help during rehabilitation [47, 48, 57, 58, 73, 74]. The application led to an increase in activity and was well tolerated by the patient without the occurrence of adverse events such as falls.
It is necessary to pay attention to the duration of the application of these technologies because overstimulation can negatively affect the outcome of patients [37]. Furthermore, cybersickness may occur during the application [29]. Lastly, the implementation of these technologies into clinical practice requires a significant investment of time by ICU staff [26], which also may reduce readiness to use them.
Overall, while VR is not a substitute for established therapy, it can be a useful tool in combination with other treatments to improve the patient's stay in an intensive care unit.
Conclusion
Augmented reality (AR) and virtual reality (VR) are no longer the domains of the science fiction world. We are on the verge of making virtual and augmented reality mainstream in the field of medicine and critical care has the potential to be at the forefront of this evolution. However, we cannot forget that VR and AR are not intended to distract us from the patient. They are provided to complement and optimize, but not replace the relationship between a health care provider and a patient. Furthermore, these are still in the research and development phase. Our involvement in this process is important to ensure that these technological developments are made in the best interest of our patients. This makes it possible to provide the best care and to improve the quality of the hospital stay in the ICU.
Availability of data and materials
The anonymized data can be requested from the authors if required.
Abbreviations
- 3D:
-
Three dimensional
- 5G:
-
Fifth generation
- AR:
-
Augmented reality
- CPR:
-
Cardiopulmonary resuscitation
- ECC:
-
Extracorporeal circulation
- ECMO:
-
Extracorporeal membrane oxygenation
- HADS:
-
Hospital Anxiety Depression Scale
- HMD:
-
Head-mounted display
- ICU:
-
Intensive care unit
- IPD:
-
Interpupillary distance
- PICU:
-
Pediatric intensive care unit
- PICS-F:
-
Post-intensive care syndrome-family
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- TAVR:
-
Transcatheter aortic valve replacement
- VR:
-
Virtual reality
References
Bruno RR, Wolff G, Wernly B, Masyuk M, Piayda K, Leaver S, et al. Virtual and augmented reality in critical care medicine: the patient’s, clinician’s, and researcher’s perspective. Crit Care. 2022;26(1):326.
Jung C, Wolff G, Wernly B, Bruno RR, Franz M, Schulze PC, et al. Virtual and augmented reality in cardiovascular care: state-of-the-art and future perspectives. JACC Cardiovasc Imaging. 2022;15(3):519–32.
Kundu M, Ng JC, Awuah WA, Huang H, Yarlagadda R, Mehta A, et al. NeuroVerse: neurosurgery in the era of Metaverse and other technological breakthroughs. Postgrad Med J. 2023. https://doi.org/10.1093/postmj/qgad002.
Bruno RR, Bruining N, Jung C, Group V-IS. Virtual reality in intensive care. Intensive Care Med. 2022;48(9):1227–9.
Wolff G, Bruno RR, Reiter M, Kantzow B, Kelm M, Jung C. Virtual reality device training for extracorporeal membrane oxygenation. Crit Care. 2020;24(1):390.
Sutherland J, Belec J, Sheikh A, Chepelev L, Althobaity W, Chow BJW, et al. Applying modern virtual and augmented reality technologies to medical images and models. J Digit Imaging. 2019;32(1):38–53.
Puel F, Minville V, Vardon-Bounes F. What place for virtual reality in the intensive care unit during medical procedures? J Intensive Care. 2021;9(1):30.
Hoffman HG, Rodriguez RA, Gonzalez M, Bernardy M, Peña R, Beck W, et al. Immersive virtual reality as an adjunctive non-opioid analgesic for pre-dominantly Latin American children with large severe burn wounds during burn wound cleaning in the intensive care unit: a pilot study. Front Hum Neurosci. 2019;13:262.
Silva JNA, Southworth M, Raptis C, Silva J. Emerging applications of virtual reality in cardiovascular medicine. JACC Basic Transl Sci. 2018;3(3):420–30.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372: n71.
Nas J, Thannhauser J, Vart P, van Geuns RJ, Muijsers HEC, Mol JQ, et al. Effect of face-to-face vs virtual reality training on cardiopulmonary resuscitation quality: a randomized clinical trial. JAMA Cardiol. 2019. https://doi.org/10.1001/jamacardio.2019.4992.
Ricci S, Calandrino A, Borgonovo G, Chirico M, Casadio M. Viewpoint: virtual and augmented reality in basic and advanced life support training. JMIR Serious Games. 2022;10(1): e28595.
Colt HG, Crawford SW, Galbraith O 3rd. Virtual reality bronchoscopy simulation: a revolution in procedural training. Chest. 2001;120(4):1333–9.
Chiang DH, Huang CC, Cheng SC, Cheng JC, Wu CH, Huang SS, et al. Immersive virtual reality (VR) training increases the self-efficacy of in-hospital healthcare providers and patient families regarding tracheostomy-related knowledge and care skills: a prospective pre-post study. Medicine (Baltimore). 2022;101(2): e28570.
Ralston BH, Willett RC, Namperumal S, Brown NM, Walsh H, Muñoz RA, et al. Use of virtual reality for pediatric cardiac critical care simulation. Cureus. 2021;13(6): e15856.
Yu M, Yang M, Ku B, Mann JS. Effects of virtual reality simulation program regarding high-risk neonatal infection control on nursing students. Asian Nurs Res (Korean Soc Nurs Sci). 2021;15(3):189–96.
Yang SY, Oh YH. The effects of neonatal resuscitation gamification program using immersive virtual reality: a quasi-experimental study. Nurse Educ Today. 2022;117: 105464.
Farra S, Hodgson E, Miller ET, Timm N, Brady W, Gneuhs M, et al. Effects of virtual reality simulation on worker emergency evacuation of neonates. Disaster Med Public Health Prep. 2019;13(2):301–8.
Agasthya N, Penfil S, Slamon N. Virtual reality simulation for pediatric airway intubation readiness education. Cureus. 2020;12(12): e12059.
Nijland J, Veling W, Lestestuiver BP, Van Driel CMG. Virtual reality relaxation for reducing perceived stress of intensive care nurses during the COVID-19 pandemic. Front Psychol. 2021;12: 706527.
Bodet-Contentin L, Letourneur M, Ehrmann S. Virtual reality during work breaks to reduce fatigue of intensive unit caregivers: A crossover, pilot, randomised trial. Aust Crit Care. 2022. https://doi.org/10.1016/j.aucc.2022.01.009.
Eccleston C, Crombez G. Pain demands attention: a cognitive-affective model of the interruptive function of pain. Psychol Bull. 1999;125(3):356–66.
Mosso-Vázquez JL, Gao K, Wiederhold BK, Wiederhold MD. Virtual reality for pain management in cardiac surgery. Cyberpsychol Behav Soc Netw. 2014;17(6):371–8.
Esumi R, Yokochi A, Shimaoka M, Kawamoto E. Virtual reality as a non-pharmacologic analgesic for fasciotomy wound infections in acute compartment syndrome: a case report. J Med Case Rep. 2020;14(1):46.
Laghlam D, Naudin C, Coroyer L, Aidan V, Malvy J, Rahoual G, et al. Virtual reality vs. Kalinox® for management of pain in intensive care unit after cardiac surgery: a randomized study. Ann Intensive Care. 2021;11(1):74.
Markus LA, Willems KE, Maruna CC, Schmitz CL, Pellino TA, Wish JR, et al. Virtual reality: feasibility of implementation in a regional burn center. Burns. 2009;35(7):967–9.
Hoffman HG, Patterson DR, Seibel E, Soltani M, Jewett-Leahy L, Sharar SR. Virtual reality pain control during burn wound debridement in the hydrotank. Clin J Pain. 2008;24(4):299–304.
Faber AW, Patterson DR, Bremer M. Repeated use of immersive virtual reality therapy to control pain during wound dressing changes in pediatric and adult burn patients. J Burn Care Res. 2013;34(5):563–8.
Merliot-Gailhoustet L, Raimbert C, Garnier O, Carr J, De Jong A, Molinari N, et al. Discomfort improvement for critically ill patients using electronic relaxation devices: results of the cross-over randomized controlled trial E-CHOISIR (Electronic-CHOIce of a SYSTEM for Intensive care Relaxation). Crit Care. 2022;26(1):263.
Haley AC, Wacker DA. Cinematic virtual reality for anxiety management in mechanically ventilated patients: a feasibility and pilot study. Acute Crit Care. 2022;37(2):230–6.
Lee SY, Kang J. Effect of virtual reality meditation on sleep quality of intensive care unit patients: a randomised controlled trial. Intensive Crit Care Nurs. 2020;59: 102849.
Squintani G, Brugnoli MP, Pasin E, Segatti A, Concon E, Polati E, et al. Changes in laser-evoked potentials during hypnotic analgesia for chronic pain: a pilot study. Ann Palliat Med. 2018;7(1):7–16.
Rousseaux F, Bicego A, Ledoux D, Massion P, Nyssen AS, Faymonville ME, et al. Hypnosis associated with 3D immersive virtual reality technology in the management of pain: a review of the literature. J Pain Res. 2020;13:1129–38.
Rousseaux F, Faymonville ME, Nyssen AS, Dardenne N, Ledoux D, Massion PB, et al. Can hypnosis and virtual reality reduce anxiety, pain and fatigue among patients who undergo cardiac surgery: a randomised controlled trial. Trials. 2020;21(1):330.
Rousseaux F, Dardenne N, Massion PB, Ledoux D, Bicego A, Donneau AF, et al. Virtual reality and hypnosis for anxiety and pain management in intensive care units: A prospective randomised trial among cardiac surgery patients. Eur J Anaesthesiol. 2021. https://doi.org/10.1097/EJA.0000000000001633.
Jawed YT, Golovyan D, Lopez D, Khan SH, Wang S, Freund C, et al. Feasibility of a virtual reality intervention in the intensive care unit. Heart Lung. 2021;50(6):748–53.
Naef AC, Erne K, Exl MT, Nef T, Jeitziner MM. Visual and auditory stimulation for patients in the intensive care unit: a mixed-method study. Intensive Crit Care Nurs. 2022;73: 103306.
Suvajdzic M, Bihorac A, Rashidi P. D.R.E.A.M.S: (Digital rehabilitation environment-altering medical system). SeGAH IEEE Int Conf Serious Games Appl Health. 2017. https://doi.org/10.1109/SeGAH.2017.7939293.
Suvajdzic M, Bihorac A, Rashidi P, Ong T, Applebaum J. Virtual reality and human consciousness: the use of immersive environments in delirium therapy. Technoetic Arts. 2018;16(1):75–83.
Ong TL, Ruppert MM, Akbar M, Rashidi P, Ozrazgat-Baslanti T, Bihorac A, et al. Improving the intensive care patient experience with virtual reality-a feasibility study. Crit Care Explor. 2020;2(6): e0122.
Arofiati F, Primadani M, Ruhyana R. Role of family in the hospitalization of critical patients in the intensive care unit. Medisains. 2020. https://doi.org/10.30595/medisains.v18i1.6482.
He M, Li X, Zhang T, Jin X, Hu C. The fifth generation mobile communication technology plus virtual reality system for intensive care unit visits during COVID-19 pandemic: keep the delirium away. J Nurs Manag. 2022;30(8):3885–7.
Fiani B, Figueras RA, Samones P, Lee C, Castillo A, Sangalang B, et al. Long-Term Intensive Care Unit (ICU) Stays Can Lead to Long-Term Cognitive Impairment (LTCI): Neurosurgery Nursing Strategies to Minimize Risk. Cureus. 2022;14(9): e28967.
Turon M, Fernandez-Gonzalo S, Jodar M, Gomà G, Montanya J, Hernando D, et al. Feasibility and safety of virtual-reality-based early neurocognitive stimulation in critically ill patients. Ann Intensive Care. 2017;7(1):81.
Navarra-Ventura G, Gomà G, de Haro C, Jodar M, Sarlabous L, Hernando D, et al. Virtual reality-based early neurocognitive stimulation in critically Ill Patients: a pilot randomized clinical trial. J Pers Med. 2021;11(12):1260.
Marcarian T, Obreja V, Murray K, Meltzer JS, Miller PS. Success in supporting early mobility and exercise in a cardiothoracic intensive care unit. J Nurs Adm. 2023;53(3):161–7.
Gomes TT, Schujmann DS, Fu C. Rehabilitation through virtual reality: physical activity of patients admitted to the intensive care unit. Rev Bras Ter Intensiva. 2019;31(4):456–63.
Parke S, Hough CL, Aaron EB. The feasibility and acceptability of virtual therapy environments for early ICU mobilization. Pm r. 2020;12(12):1214–21.
Vlake JH, Van Bommel J, Wils EJ, Korevaar TIM, Hellemons ME, Schut AFC, et al. Effect of intensive care unit-specific virtual reality (ICU-VR) to improve psychological well-being and quality of life in COVID-19 ICU survivors: a study protocol for a multicentre, randomized controlled trial. Trials. 2021;22(1):328.
Vlake JH, Van Bommel J, Wils EJ, Korevaar TIM, Bienvenu OJ, Klijn E, et al. Virtual reality to improve sequelae of the postintensive care syndrome: a multicenter, randomized controlled feasibility study. Crit Care Explor. 2021;3(9): e0538.
Vlake JH, van Bommel J, Wils EJ, Bienvenu J, Hellemons ME, Korevaar TI, et al. Intensive care unit-specific virtual reality for critically Ill patients With COVID-19: multicenter randomized controlled trial. J Med Internet Res. 2022;24(1): e32368.
Vlake JH, van Bommel J, Hellemons ME, Wils EJ, Gommers D, van Genderen ME. Intensive care unit-specific virtual reality for psychological recovery after ICU treatment for COVID-19; a brief case report. Front Med (Lausanne). 2020;7: 629086.
Debelić I, Mikolčić A, Tihomirović J, Barić I, Lendić Đ, Nikšić Ž, et al. Stressful experiences of parents in the paediatric intensive care unit: searching for the most intensive PICU stressors. Int J Environ Res Public Health. 2022;19(18):11450.
Badke CM, Essner BS, O’Connell M, Malakooti MR. An innovative virtual reality experience in the PICU: a pilot study. Pediatr Crit Care Med. 2019;20(6):e283–6.
Badke CM, Krogh-Jespersen S, Flynn RM, Shukla A, Essner BS, Malakooti MR. Virtual reality in the pediatric intensive care unit: patient emotional and physiologic responses. Front Digit Health. 2022;4: 867961.
Kucher N, Larson JM, Fischer G, Mertaugh M, Peterson L, Gershan LA. 3-Dimensional nature-based therapeutics in pediatric patients with total pancreatectomy and islet auto-transplant. Complement Ther Med. 2020;48: 102249.
Abdulsatar F, Walker RG, Timmons BW, Choong K. “Wii-Hab” in critically ill children: a pilot trial. J Pediatr Rehabil Med. 2013;6(4):193–204.
Lai B, Powell M, Clement AG, Davis D, Swanson-Kimani E, Hayes L. Examining the feasibility of early mobilization with virtual reality gaming using head-mounted display and adaptive software with adolescents in the pediatric intensive care unit: case report. JMIR Rehabil Assist Technol. 2021;8(2): e28210.
Tallent S, Turi JL, Thompson J, Allareddy V, Hueckel R. Extending the radius of family-centered care in the pediatric cardiac intensive care unit through virtual rounding. J Am Assoc Nurse Pract. 2021;205–212. https://doi.org/10.1097/JXX.0000000000000610.
Huang CY, Thomas JB, Alismail A, Cohen A, Almutairi W, Daher NS, et al. The use of augmented reality glasses in central line simulation: “see one, simulate many, do one competently, and teach everyone.” Adv Med Educ Pract. 2018;9:357–63.
Fumagalli S, Torricelli G, Massi M, Calvani S, Boni S, Roberts AT, et al. Effects of a new device to guide venous puncture in elderly critically ill patients: results of a pilot randomized study. Aging Clin Exp Res. 2017;29(2):335–9.
Morillas Perez J, Mecho Meca S, Caballero Galindo G, Miguel P-LJ. Validation of the effectiveness of augmented reality-assisted vascular puncture: an experimental model. J Vasc Access. 2023. https://doi.org/10.1177/11297298231156006.
Alismail A, Thomas J, Daher NS, Cohen A, Almutairi W, Terry MH, et al. Augmented reality glasses improve adherence to evidence-based intubation practice. Adv Med Educ Pract. 2019;10:279–86.
Heo S, Moon S, Kim M, Park M, Cha WC, Son MH. An augmented reality-based guide for mechanical ventilator setup: prospective randomized pilot trial. jMIR Serious Games. 2022;10(3): e38433.
Gan A, Cohen A, Tan L. Augmented reality-assisted percutaneous dilatational tracheostomy in critically Ill patients with chronic respiratory disease. J Intensive Care Med. 2019;34(2):153–5.
Zackoff MW, Cruse B, Sahay RD, Fei L, Saupe J, Schwartz J, et al. Development and implementation of augmented reality enhanced high-fidelity simulation for recognition of patient decompensation. Simul Healthc. 2021;16(3):221–30.
Yamada Y, Nakamura T, Yamada M, Maruyama J, Maruyama K, Azuma E. Use of augmented reality to assist teaching for future perfusionists in extracorporeal technology. J Extra Corpor Technol. 2019;51(4):244–7.
Dias PL, Greenberg RG, Goldberg RN, Fisher K, Tanaka DT. Augmented reality-assisted video laryngoscopy and simulated neonatal intubations: a pilot study. Pediatrics. 2021. https://doi.org/10.1542/peds.2020-005009.
Scquizzato T, Landoni G, Carenzo L, Forti A, Zangrillo A. A smartphone application with augmented reality for estimating weight in critically ill paediatric patients. Resuscitation. 2020;146:3–4.
Yeung AWK, Tosevska A, Klager E, Eibensteiner F, Laxar D, Stoyanov J, et al. Virtual and augmented reality applications in medicine: analysis of the scientific literature. J Med Internet Res. 2021;23(2): e25499.
Nas J, Thannhauser J, Vart P, van Geuns RJ, Muijsers HEC, Mol JQ, et al. Effect of face-to-face vs virtual reality training on cardiopulmonary resuscitation quality: a randomized clinical trial. JAMA Cardiol. 2020;5(3):328–35.
Gerber SM, Jeitziner MM, Wyss P, Chesham A, Urwyler P, Müri RM, et al. Visuo-acoustic stimulation that helps you to relax: a virtual reality setup for patients in the intensive care unit. Sci Rep. 2017;7(1):13228.
Hemphill S, Nguyen A, Kwong J, Rodriguez ST, Wang E, Caruso TJ. Virtual reality facilitates engagement in physical therapy in the pediatric CVICU. Pediatr Phys Ther. 2021;33(1):E7-e9.
Chillura A, Bramanti A, Tartamella F, Pisano MF, Clemente E, Lo Scrudato M, et al. Advances in the rehabilitation of intensive care unit acquired weakness: a case report on the promising use of robotics and virtual reality coupled to physiotherapy. Medicine (Baltimore). 2020;99(28): e20939.
OCEBM Levels of Evidence Working Group JH, Iain Chalmers (James Lind Library), Paul Glasziou, Trish Greenhalgh, Carl Heneghan, Alessandro Liberati, Ivan Moschetti, Bob Phillips, Hazel Thornton, Olive Goddard and Mary Hodgkinson. The Oxford Levels of Evidence 2. 2011.
Vlake JH, Wils EJ, van Bommel J, Korevaar TIM, Gommers D, van Genderen ME. Virtual reality tailored to the needs of post-ICU Patients: a safety and immersiveness study in healthy volunteers. Crit Care Explor. 2021;3(5): e0388.
Gerber SM, Jeitziner MM, Knobel SEJ, Mosimann UP, Müri RM, Jakob SM, et al. Perception and performance on a virtual reality cognitive stimulation for use in the intensive care unit: a non-randomized trial in critically Ill patients. Front Med (Lausanne). 2019;6:287.
Gerber SM, Jeitziner MM, Sanger SD, Knobel SEJ, Marchal-Crespo L, Muri RM, et al. Comparing the relaxing effects of different virtual reality environments in the intensive care unit: observational study. JMIR Perioper Med. 2019;2(2): e15579.
Vlake JH, van Genderen ME, Schut A, Verkade M, Wils EJ, Gommers D, et al. Patients suffering from psychological impairments following critical illness are in need of information. J Intensive Care. 2020;8:6.
Blair GJ, Kapil S, Cole SP, Rodriguez S. Virtual reality use in adult ICU to mitigate anxiety for a patient on V-V ECMO. J Clin Anesth. 2019;55:26–7.
Small C, Stone R, Pilsbury J, Bowden M, Bion J. Virtual restorative environment therapy as an adjunct to pain control during burn dressing changes: study protocol for a randomised controlled trial. Trials. 2015;16:329.
Naef AC, Jeitziner MM, Gerber SM, Jenni-Moser B, Muri RM, Jakob SM, et al. Virtual reality stimulation to reduce the incidence of delirium in critically ill patients: study protocol for a randomized clinical trial. Trials. 2021;22(1):174.
Umoren R, Bucher S, Hippe DS, Ezenwa BN, Fajolu IB, Okwako FM, et al. eHBB: a randomised controlled trial of virtual reality or video for neonatal resuscitation refresher training in healthcare workers in resource-scarce settings. BMJ Open. 2021;11(8): e048506.
Scapin SQ, Echevarría-Guanilo ME, Fuculo PRBJ, Martins JC, Barbosa MDV, Pereima MJL. Use of virtual reality for treating burned children: case reports. Rev Bras Enferm. 2017;70(6):1291–5.
Bloom D, Colombo JN, Miller N, Southworth MK, Andrews C, Henry A, et al. Early preclinical experience of a mixed reality ultrasound system with active GUIDance for NEedle-based interventions: the GUIDE study. Cardiovasc Digit Health J. 2022;3(5):232–40.
Acknowledgements
Not applicable.
Funding
Open Access funding enabled and organized by Projekt DEAL. This work was supported by the Forschungskommission of the Medical Faculty of the Heinrich-Heine-University Düsseldorf No. 2020-21 to RRB for a Clinician Scientist Track. Furthermore, institutional support has been received by the German Research Council (SFB 1116, B06) as well as the State of North Rhine Westphalia (Giga for Health: 5GMedizincampus. NRW, Project number 005-2008-0055 and PROFILNRW-2020-107-A, TP4). No (industry) sponsorship has been received.
Author information
Authors and Affiliations
Contributions
DK and RRB performed a literature search, interpreted the patient data, and wrote the manuscript. GW, MK, and CJ reviewed the manuscript. All authors approved the final manuscript and assumed responsibility for the integrity of the data and the accuracy of the data analysis.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Ethics approval was not applicable for the literature search in this study.
Consent for publication
The manuscript does not contain any individual person’s data in any form. People on images gave the written approval for the picture and its publication. VR glasses were not active on the images as shown and can be understand as examples. Local approval depending on relevant regulations needs to be obtained for the active use of such devices.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Appendices
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Kanschik, D., Bruno, R.R., Wolff, G. et al. Virtual and augmented reality in intensive care medicine: a systematic review. Ann. Intensive Care 13, 81 (2023). https://doi.org/10.1186/s13613-023-01176-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01176-z