Abstract
Background
Data about critically ill metastatic cancer patients functional outcome after unplanned admission to the ICU are scarce. The aim of this study was to assess factors associated with 90-day return home and 1-year survival in this population.
Study design and methods
A multicenter retrospective study included all consecutive metastatic cancer patients admitted to the ICU for unplanned reason between 2017 and 2020.
Results
Among 253 included metastatic cancer patients, mainly with lung cancer, 94 patients (37.2%) could return home on day 90. One-year survival rate was 28.5%. Performance status 0 or 1 (OR, 2.18; 95% CI 1.21–3.93; P = 0.010), no malnutrition (OR, 2.90; 95% CI 1.61–5.24; P < 0.001), female gender (OR, 2.39; 95% CI 1.33–4.29; P = 0.004), recent chemotherapy (OR, 2.62; 95% CI 1.40–4.90; P = 0.003), SOFA score ≤ 5 on admission (OR, 2.62; 95% CI 1.41–4.90; P = 0.002) were significantly predictive for 90-day return home. Malnutrition (HR, 1.66; 95% CI 1.18–2.22; P = 0.003), acute respiratory failure (ARF) as reason for admission (HR, 1.40; 95% CI 1.10–1.95; P = 0.043), SAPS II on admission (HR, 1.03; 95% CI 1.02–1.05; P < 0.001) and decisions to forgo life-sustaining therapies (DFLST) (HR, 2.80; 95% CI 2.04–3.84; P < 0.001) were independently associated with 1-year mortality.
Conclusions
More than one out of three metastatic cancer patients could return home within 3 months after an unplanned admission to the ICU. Previous performance and nutritional status, ongoing specific treatment and low severity of the acute illness were found to be predictive for return home. Such encouraging findings should help change the dismal perception of critically ill metastatic cancer patients.
Similar content being viewed by others
Introduction
Cancer is the second most common cause of death in the world [1]. Continuous improvements in early diagnosis, oncologic treatment and supportive care led to better outcome [2]. New therapeutic approaches targeting actionable oncogenic mutations in tumour cells or their immune microenvironment may provide a prolonged survival with acceptable quality of life to patients formerly considered refractory [3]. These advances result in a rising number of patients with active cancer at risk of developing life-threatening complications [4], and a recent observational study found that 5% of cancer patients experience a critical illness resulting in intensive care unit (ICU) admission within 2 years after cancer diagnosis [5]. In a worldwide survey including 10069 patients admitted to the ICU from 730 centres in 84 countries, 888 (8.8%) had solid non-metastatic cancer and 332 (3.3%) had metastatic cancer [6]. Advanced or metastatic stage of underlying malignancy is often reported as worsening short- or medium-term prognosis in critically ill cancer patients, and oncologists and intensivists are often reluctant to propose or admit these patients to the ICU [7]. Data on outcome of critically ill metastatic cancer patients are scarce and studies in the field often assess survival rate [4, 8,9,10,11,12]. Few studies evaluated the clinical evolution after ICU discharge, in terms of functional status, quality of life and ability to receive further specific treatment [13, 14].
The aim of our study was to determine the factors associated with survival of metastatic cancer patients admitted to the ICU, particularly those associated with 90-day return home, a pragmatic endpoint aligned with patients’ individual goals and needs [15].
Patients and methods
Main objective
The primary objective of this study was to determine the predictive factors for return home after an unplanned ICU stay among metastatic solid cancer patients. The secondary objective was to assess factors associated with 1-year survival in this population.
Study design, settings and participants
We performed a multicentre retrospective study including all consecutive adult patients (age ≥ 18 years) with metastatic solid tumour requiring unplanned admission to three ICUs between January 1, 2017 and December 31, 2020. Non-inclusion criteria were: admission to secure a procedure, planned admission following elective surgery and patients with testicle cancer, as the course and management of this subtype of metastatic cancer is very specific. For patients with multiple ICU admissions, only the first qualifying ICU stay was considered.
The study was conducted at the Paoli-Calmettes Institute, a comprehensive cancer center, Nord Teaching Hospital (Assistance-Publique Hôpitaux de Marseille), an academic center, both in Marseille (France), and at the Sainte Musse Hospital in Toulon (France), a general hospital.
All management decisions were independently made by the attending physicians according to standard practices. According to French regulations, this study was approved by our local Institutional Review Board (n°2020–067), which waived the need for signed consent.
Data collection
The following variables were collected on admission: age, gender, medical background, comorbidities, type of solid tumour, primary tumour site, metastases type and number of sites, main admission reason, previous anticancer treatments (surgery, radiotherapy, cytostatic chemotherapy, targeted therapy, immunotherapy) and number of lines (i.e., number of lines of specific cancer therapy before ICU admission, including or not chemotherapy). Two study investigators reviewed main diagnoses.
The severity of the illness was evaluated using the Sequential Organ Failure Assessment (SOFA) score and the Simplified Acute Physiology Score II (SAPS II) at admission. Comorbidities were determined with the Charlson Comorbidity Index (CCI). Eastern cooperative oncology group performance status (ECOG-PS) 1 month before ICU admission was recorded. Malnutrition was defined as body mass index (BMI) < 18.5 kg/m2, weight loss ≥ 5% in 1 month or ≥ 10% in 6 months before ICU admission, or albumin < 30 g/L on ICU admission. Clinical and laboratory data at ICU admission were collected, including neutropenia and its duration (absolute neutrophil count of < 0.5 × 109/L), as well as organ failures during ICU stay. The Oncoscore was calculated [14]. All microbiological documentations were recorded.
The ICU and hospital length of stay and the time between hospital and ICU admission were calculated. The ICU interventions were defined by the use of mechanical ventilation (MV), including non-invasive ventilation (NIV) and invasive mechanical ventilation (IMV), the use of vasopressors, renal replacement therapy (RRT) and oncologic treatments.
During the ICU stay, life-supporting interventions, anti-infectious agents, prophylactic treatments, and diagnostic procedures were administered at the discretion of the attending intensivist, following best clinical practice and guidelines. Chemotherapy, corticosteroids, hematopoietic growth factors, immunosuppressive drugs and other cancer-related treatments were prescribed by the oncologist in charge in accordance with institutional guidelines. Decisions on ICU discharge were left at the discretion of the attending intensivist, and patients were discharged from ICU without any non-hematological organ failure.
Decisions to forgo life-sustaining therapies (DFLST) before admission and during ICU stay were recorded. Progression free survival and anti-neoplastic therapy after ICU discharge were reported.
Study outcomes
The number of patients returned home on day 90, as well as the ICU, hospital, and 1-year mortality rates were recorded.
Statistical analysis
All data are presented as rates (percentages) for qualitative variables and as medians (25–75th percentiles) for the categorical variables. Patients’ features during the first 90 days after ICU admission were compared across two groups of patients: patients returned home on day 90 versus patients not returned home on day 90. Since we knew the immediate location of all patients discharged alive from the hospital, we classified the 14 patients lost to follow-up 90 days after admission to the ICU in the "no 90-day return home" group. Comparisons between the two groups for continuous variables were made using the Mann–Whitney test. Comparisons between the two groups for categorical variables were made using the Pearson Chi-square test or Fisher exact test. All P values < 0.05 were considered to be statistically significant. We performed logistic regression analyses to identify the independent variables associated with 90-day return home, measured by odds ratio (OR) with a 95% confidence interval (95% CI). Variables yielding a P lower than 0.10 in the bivariate analyses were entered a backward stepwise logistic regression model. One-year survival was calculated from the day of ICU admission until death from any cause (event) or from the last follow-up before death (censored), the follow-up period was censored at 1 year. Correlations between patient characteristics and 1-year mortality were assessed using univariate and multivariate Cox regression models, measured by the estimated hazard ratio (HR) with a 95% confidence interval (95% CI). All statistical tests were two-sided. The required significance level was set at a P value less than 0.05. The Cox proportional hazard model used in the multivariate approach included variables for which a P value less than 0.10 was observed in the univariate analysis as well as clinically relevant variables. A backward stepwise selection procedure (threshold of 0.05) was used to retain the final model. The Cox proportional hazards assumptions were tested using goodness-of-fit tests based on the cumulative sums of the martingale residuals [16]. The variable of interest was 1-year mortality, and results were expressed as HR and 95% CIs.
Statistical tests were conducted using the R software (R Core Team, 2020).
Results
During the study period, 253 patients, aged of 65 years [56–72] with a 1:1 sex ratio , were included (Fig. 1). Their features are presented in Table 1. The CCI was 10 [8–11]. The most frequent primary tumour sites were lung for 95 (37.5%) patients, breast (16.2%) and colorectal (9.1%). The median number of metastatic sites was 2 [1–3], mainly lung/pleura (49%), bone (40.7%) and liver (38.3%). One hundred and one (39.9%) patients had an ECOG-PS of 0 or 1 one month before ICU admission. Before ICU admission, the median number of administered treatment lines was 2 [0–2], whereas 68 (23.9%) patients did not receive any treatment. Malnutrition was identified in 137 (53.5%) patients.
The ICU stay characteristics are presented in Table 2. Reasons for ICU admission were mainly acute respiratory failure in 149 (58.9%) patients and septic shock in 53 (20.9%). Infection represented 46.2% of final etiological diagnoses. Tumour-related reason for ICU admission was present in 92 (36.4) patients, and anti-neoplastic drug side effect was reported in 22 (8.7%) patients.
Vasopressors and mechanical ventilation were required in 105 (41.5%) and 60 (23.7%) patients, respectively. The SAPS II, the SOFA score on day 1 were 45 [38–53] and 5 [3–8], respectively, while Oncoscore was 4 [3–6]. DFLST during the ICU stay were reported for 90 (35.6%) patients.
Outcome
90-Day return home
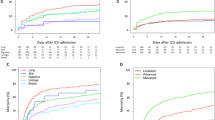
On day 90, 94 (37.2%) patients returned home. The ICU, hospital, 90-day and 1-year mortality rates were 15.8%, 36.8%, 52.6% and 71.5%, respectively. Thirty-two (12.6%) patients, who were discharged alive from hospital, were lost to follow-up at 1 year.
Among the 159 (62.8%) patients who did not return home on day 90, 93 (36.8%) died in the hospital, 40 (15.8%) died within 3 months, after hospital discharge, 14 (5.5%) were lost to follow-up and 12 (4.7%) were admitted to post-acute care facilities.
Univariate analysis
Factors associated with 90-day return home and 1-year mortality are presented in Tables 1, 2 and 3.
Young age, female gender, low CCI, ECOG-PS at 0 or 1, good nutritional status and breast primitive tumour were associated with 90-day return home. Moreover, on-going chemotherapy for the underlying malignancy before ICU stay favoured 90-day return home. Conversely, increased ICU severity scores (i.e., SOFA score and SAPS II) were predictive for reduced rates of 90-day return home.
Multivariate analysis
In multivariate analysis, five factors were independently associated with 90-day return home (Table 4). ECOG-PS 0 or 1 (OR, 2.18; 95% CI 1.21–3.93; P = 0.010), lack of malnutrition (OR, 2.90; 95% CI 1.61–5.24; P < 0.001), female gender (OR, 2.39; 95% CI 1.33–4.29; P = 0.004), recent chemotherapy (i.e., within the previous 3 months) (OR, 2.62; 95% CI 1.40–4.90; P = 0.003), SOFA score ≤ 5 on ICU admission (OR, 2.62; 95% CI 1.41–4.90; P = 0.002) were significantly predictive of 90-day return home.
1-year mortality
The results of the univariate analysis for 1-year mortality are shown in Table 3. In multivariate analysis, malnutrition (HR, 1.66; 95% CI 1.18–2.22; P = 0.003), acute respiratory failure (ARF) as reason for admission (HR, 1.40; 95% CI 1.10–1.95; P = 0.043), SAPS II on admission (HR, 1.03; 95% CI 1.02–1.05; P < 0.001) and DFLST (HR, 2.80; 95% CI 2.04–3.84; P < 0.001) were independently associated with 1-year mortality. In contrast, recent chemotherapy (HR, 0.71; 95% CI 0.52–0.96; P = 0.029) and hormone therapy (HR, 0.57; 95% CI 0.35–0.93; P = 0.024) were associated with 1-year survival (Table 5).
Discussion
Patients with metastatic solid malignancies are often denied access to the ICU because of predicted poor outcome. Indeed, previous studies reported high mortality rates in similar patients. Recent advances in oncological treatment, mainly targeted therapies and immunotherapy, and specific supportive care led to improved survival in critically ill patients with metastatic solid malignancies. Yet, only few studies assessed the functional status or the quality of life of these patients in the era of new therapeutic strategies [17]. We report here the results of our multicentre retrospective study in this specific population, using a pragmatic outcome endpoint, i.e., 90-day return home.
In our study, 94 out of 253 critically ill metastatic cancer patients returned home within 90 days after an unplanned ICU stay. One-year mortality was 71.5%. ICU-mortality and hospital mortality were 16% and 37%, respectively. Considering that we included only metastatic patients with unplanned ICU admission, one could expect higher mortality rates. Yet, our results are consistent with most recent studies, as survival in this population constantly improved during the two past decades [10, 18]. Indeed, in a similar setting, Ha et al. reported in 2017 an ICU-mortality and hospital mortality of 16% and 37%, respectively [8], while Vigneron et al. mentioned a 1-year mortality of 78.5% among critically ill patients with mainly advanced or metastatic cancer. In this study, ICU-mortality and hospital mortality were 24.8% and 44.3%, respectively [4].
In our study, ECOG-PS from 0 to 1 and the lack of malnutrition favoured 90-day return home (Table 4), while malnutrition was independently associated with 1-year mortality (HR 1.61, 95% CI [1.18–2.22], P = 0.003) (Table 5). Our findings are consistent with recent studies, highlighting the dominance of previous physiological condition, such as ECOG-PS, on underlying malignancy’s characteristics for short- and long-term survival [9, 19, 20]. Hospital mortality seems more associated with acute organ failure during the ICU stay than with cancer features [8, 12, 13, 21]. Interaction and communication between oncologists and intensivists are needed to find the balance point, avoiding both futile treatments and loss of chance.
As return home after ICU stay has been poorly investigated in this specific subgroup of patients, we cannot compare our results to previous findings. However, 37.2% of critically ill metastatic cancer patients returning home after an ICU stay should prompt us to revise misconceptions about actual outcome and consider broader admission criteria or time limited trials in this specific population. The ICU and hospital mortality are solid endpoints, but view from patients and their relatives, short-term return home, reflecting an acceptable quality of life may be a critical achievement. Indeed, often aware of the incurable nature of the disease, the patients rarely request survival at any cost.
Considering this innovative endpoint, we found questioning results on factors associated with return home in this very specific population. Indeed, unlike determinants of ICU-, hospital and 1-year survival, the primary site of cancer did not seem to influence return home. Our cohort included 82 (33%) patients with non-small cell lung cancer, known as high-risk malignancy [14, 22]. Nevertheless, this type of cancer did not result in higher mortality rates than others. In addition, it did not jeopardized return home. Yet, as female gender is associated with return home, one could hypothesize that breast cancer may influence this result in larger studies.
Moreover, cancer-related complications per se as main diagnosis did not influence the rate of return home in our cohort. However, previous studies underlined cancer-related complications as predictive of short- and long-term mortality [23, 24]. We hypothesized that, due to a better knowledge of prognostic factors and new fast-acting targeted therapies available, the patients with metastatic solid malignancy admitted to our ICUs were carefully selected. Another uncommon result of our study was that recent chemotherapy significantly favours return home in multivariable analysis (OR 2.62, 95% CI [1.40–4.90], P = 0.003). Such result was previously reported in only one study [13]. Actually, it probably reflects good general functional status of patients able to receive active treatment and might be a sign of previous triage decisions.
Previous triage decisions, in the oncology ward or emergency department, are critical for this population, although they could not be assessed in our study. We think that the potential reversibility of acute life-threatening cancer-related complications may have guided the admission decision-making process, leading to better outcome.
As expected, DFLST were an independent risk factor for 1-year mortality, in accordance with previous recent studies [4, 22]. As DFLST process is complex with many intricate variables influencing the decision, it is likely that determining factors may have not been recorded nor included in the analysis. Of note, DFLST during ICU stay did not systematically lead to death of the patient, since 16% of those returning home had DFLST during their ICU stay. This highlights the difficulty of triage decisions in this setting.
Yet, we cannot exclude that self-fulfilling prophecies played a role in the association between DFLST and mortality. In fact, in this very vulnerable population with a presumed poor outcomes, physicians might be prompt to withdraw or withhold life-sustaining therapies, leading to high-mortality rates and thus confirming the presumed poor outcomes [25]. This circular reasoning has been reported in several studies, mainly concerning patients with intracerebral haemorrhage, traumatic brain injury or cardiac arrest survivors [26, 27]. One could hypothesize that self-fulfilling prophecy might occur in critically ill metastatic cancer patients, as ICU admission and full-code resuscitation is often considered as futile by intensivists [7, 28].
Our results argue for a paradigm shift considering ICU admission for critically ill patients with metastatic cancer. This change should be in line with new admission criteria, based on the stage of the underlying neoplasia and the ICU stay expectations, sharing this perspective with the patients and/or her/his relatives. We believe that return home is perhaps a more meaningful endpoint than the 28-day or 1-year mortality rates. The patient and relatives may also decide if the process of end-of-life at home is a preferred option [29,30,31]. With this in mind, future studies evaluating outcome factors and ICU admission criteria of critically ill patients with advanced-stage/metastatic cancer should investigate new endpoints, taking into account quality of life, functional status and patients’ wishes and preferences, not only crude mortality rates, as developed in a study based on a large database, assessing the number of day at home as future endpoint [32].
The strength of our study relies on its multicentre design, including a large number of critically ill metastatic patients with solid cancer, included on a short period, considering therapeutic innovations, such as targeted therapies and immunotherapy. Indeed, 89 (35%) patients had received targeted therapy or immunotherapy before ICU admission. Moreover, we chose an unusual but pragmatic outcome endpoint (i.e., 90-day return home) and our results suggested that ICU admission for selected patients was not futile in this specific population. In addition, we considered only non-scheduled admissions, excluding scheduled surgical patients known to have lower hospital mortality rates [33].
We acknowledge several limitations. First, although multicentre, this is a retrospective study, intrinsically susceptible to have selection bias. Only critically ill metastatic cancer patients admitted to the ICU were included, so we do not have any information on in-ward or in emergency department triage decisions, by oncologists themselves or after multidisciplinary discussion including an intensivist. Moreover, unidentified confounding factors may have been overlooked in the multivariable analysis. Yet, biological and medical variables were collected prospectively with the information system. Second, we did not record any functional information from patients returned home, such as ECOG-PS or need for home care, for example. We supposed attending physicians would not discharge home bedridden or moribund patients. Third, in line with the previous limitation, we could not collect any data about the subsequent specific treatment and its feasibility. The ability to receive planned cancer treatment after ICU discharge is another relevant and meaningful endpoint in this population [34]. A prospective study would be needed to assess cancer treatment combined to quality-of-life indicators after ICU discharge.
Conclusion
Despite underlying metastatic solid malignancies, more than one out of three (37.2%) patients returned home within 90 days after an unplanned admission to the ICU. Previous performance and nutritional status, ongoing specific treatment and low severity of the acute illness were found to be predictive for return home and survival at 1 year. These results should be utilised to inform meaningful conversations with clinicians, patients and family members to ensure appropriate decision making.
Availability of data and materials
The data sets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Abbreviations
- ARF:
-
Acute respiratory failure
- BMI:
-
Body mass index
- CCI:
-
Charlson comorbidity index
- CI:
-
Confidence interval
- DFLST:
-
Decisions to forgo life-sustaining therapies
- ECOG-PS:
-
Eastern cooperative oncology group performance status
- HR:
-
Hazard ratio
- ICU:
-
Intensive care unit
- IMV:
-
Invasive mechanical ventilation
- IQR:
-
Interquartile range
- LDH:
-
Lactate dehydrogenase
- LOS:
-
Length of stay
- MV:
-
Mechanical ventilation
- NIV:
-
Non-invasive ventilation
- OR:
-
Odds ratio
- RRT:
-
Renal replacement therapy
- SAPS II:
-
Simplified acute physiology score II
- SOFA:
-
Sequential organ failure assessment
References
GBD 2016 Causes of Death Collaborators. Global, regional, and national age-sex specific mortality for 264 causes of death, 1980–2016: a systematic analysis for the global burden of disease study 2016. Lancet. 2017;390:1151–210.
Siegel RL, Miller KD, Jemal A. Cancer statistics, 2020. CA Cancer J Clin. 2020;70:7–30.
Colonna M, Boussari O, Cowppli-Bony A, Delafosse P, Romain G, Grosclaude P, et al. Time trends and short term projections of cancer prevalence in France. Cancer Epidemiol. 2018;56:97–105.
Vigneron C, Charpentier J, Valade S, Alexandre J, Chelabi S, Palmieri L-J, et al. Patterns of ICU admissions and outcomes in patients with solid malignancies over the revolution of cancer treatment. Ann Intensive Care. 2021;11:182.
Puxty K, McLoone P, Quasim T, Sloan B, Kinsella J, Morrison DS. Risk of critical illness among patients with solid cancers: a population-based observational study. JAMA Oncol. 2015;1:1078–85.
Vincent J-L, Marshall JC, Namendys-Silva SA, François B, Martin-Loeches I, Lipman J, et al. Assessment of the worldwide burden of critical illness: the intensive care over nations (ICON) audit. Lancet Respir Med. 2014;2:380–6.
Nassar AP, Dettino ALA, Amendola CP, dos Santos RA, Forte DN, Caruso P. Oncologists’ and intensivists’ attitudes toward the care of critically Ill patients with cancer. J Intensive Care Med. 2019;34:811–7.
Ha FJ, Weickhardt AJ, Parakh S, Vincent AD, Glassford NJ, Warrillow S, et al. Survival and functional outcomes of patients with metastatic solid organ cancer admitted to the intensive care unit of a tertiary centre. Crit Care Resusc. 2017;19:159–66.
Hautecloque-Rayz S, Albert-Thananayagam M, Martignene N, Le Deley M-C, Carbonnelle G, Penel N, et al. Long-term outcomes and prognostic factors of patients with metastatic solid tumors admitted to the intensive care unit. Oncology. 2022;100:173–81.
Loh KP, Kansagra A, Shieh M-S, Pekow P, Lindenauer P, Stefan M, et al. Predictors of in-hospital mortality in patients with metastatic cancer receiving specific critical care therapies. J Natl Compr Canc Netw. 2016;14:979–87.
Oud L. Critical illness in patients with metastatic cancer: a population-based cohort study of epidemiology and outcomes. J Investig Med. 2021;70:820.
Yuan ZN, Wang HJ, Gao Y, Qu SN, Huang CL, Wang H, et al. Short- and medium-term survival of critically ill patients with solid cancer admitted to the intensive care unit. Ann Palliat Med. 2022 May;11(5):1649–1659. https://doi.org/10.21037/apm-21-2352. Epub 2021 Dec 27. PMID: 35016517.
Gheerbrant H, Timsit J-F, Terzi N, Ruckly S, Laramas M, Levra MG, et al. Factors associated with survival of patients with solid cancer alive after intensive care unit discharge between 2005 and 2013. BMC Cancer. 2021;21:9.
Vincent F, Soares M, Mokart D, Lemiale V, Bruneel F, Boubaya M, et al. In-hospital and day-120 survival of critically ill solid cancer patients after discharge of the intensive care units: results of a retrospective multicenter study-A Groupe de recherche respiratoire en réanimation en Onco-Hématologie (Grrr-OH) study. Ann Intensive Care. 2018;8:40.
Kerckhoffs MC, Kosasi FFL, Soliman IW, van Delden JJM, Cremer OL, de Lange DW, et al. Determinants of self-reported unacceptable outcome of intensive care treatment 1 year after discharge. Intensive Care Med. 2019;45:806–14.
Sfumato P, Filleron T, Giorgi R, Cook RJ, Boher JM. Goftte: A R package for assessing goodness-of-fit in proportional (sub) distributions hazards regression models. Comput Methods Programs Biomed. 2019;177:269–75.
Toffart A-C, M’Sallaoui W, Jerusalem S, Godon A, Bettega F, Roth G, et al. Quality of life of patients with solid malignancies at 3 months after unplanned admission in the intensive care unit: a prospective case-control study. PLoS ONE. 2023;18:e0280027.
Heo SJ, Kim G, Lee C-K, Chung KS, Choi HJ, Sohn J, et al. Prediction of short- and long-term survival for advanced cancer patients after ICU admission. Support Care Cancer. 2015;23:1647–55.
Puxty K, McLoone P, Quasim T, Kinsella J, Morrison D. Survival in solid cancer patients following intensive care unit admission. Intensive Care Med. 2014;40:1409–28.
Soares M, Toffart A-C, Timsit J-F, Burghi G, Irrazábal C, Pattison N, et al. Intensive care in patients with lung cancer: a multinational study. Ann Oncol. 2014;25:1829–35.
Caruso P, Ferreira AC, Laurienzo CE, Titton LN, Terabe DSM, Carnieli DS, et al. Short- and long-term survival of patients with metastatic solid cancer admitted to the intensive care unit: prognostic factors. Eur J Cancer Care (Engl). 2010;19:260–6.
Vigneron C, Charpentier J, Wislez M, Mira J-P, Lefebvre A, Fournel L, et al. Short-term and long-term outcomes of patients with lung cancer and life-threatening complications. Chest. 2021;S0012–3692(21):00864–73.
Torres VBL, Vassalo J, Silva UVA, Caruso P, Torelly AP, Silva E, et al. Outcomes in critically Ill patients with cancer-related complications. PLoS ONE. 2016;11:e0164537.
Zerbib Y, Rabbat A, Fartoukh M, Bigé N, Andréjak C, Mayaux J, et al. Urgent chemotherapy for life-threatening complications related to solid neoplasms. Crit Care Med. 2017;45:e640–8.
van der Zee EN, Epker JL, Bakker J, Benoit DD, Kompanje EJO. Treatment limitation decisions in critically Ill patients with a malignancy on the intensive care unit. J Intensive Care Med. 2021;36:42–50.
Beekman R, Maciel CB, Ormseth CH, Zhou SE, Galluzzo D, Miyares LC, et al. Early head CT in post-cardiac arrest patients: a helpful tool or contributor to self-fulfilling prophecy? Resuscitation. 2021;165:68–76.
Zahuranec DB, Fagerlin A, Sánchez BN, Roney ME, Thompson BB, Fuhrel-Forbis A, et al. Variability in physician prognosis and recommendations after intracerebral hemorrhage. Neurology. 2016;86:1864–71.
Clément-Duchêne C, Carnin C, Guillemin F, Martinet Y. How accurate are physicians in the prediction of patient survival in advanced lung cancer? Oncologist. 2010;15:782–9.
Khan SA, Gomes B, Higginson IJ. End-of-life care–what do cancer patients want? Nat Rev Clin Oncol. 2014;11:100–8.
Wachterman MW, Luth EA, Semco RS, Weissman JS. Where americans die—is there really “No Place Like Home”? N Engl J Med. 2022;386:1008–10.
Wheatley VJ, Baker JI. “Please, I want to go home”: ethical issues raised when considering choice of place of care in palliative care. Postgrad Med J. 2007;83:643–8.
Martin GL, Atramont A, Mazars M, Tajahmady A, Agamaliyev E, Singer M, et al. Days spent at home and mortality after critical illness: a cluster analysis using nationwide data. Chest. 2022;S0012–3692(22):03997–4006.
Soares M, Caruso P, Silva E, Teles JMM, Lobo SMA, Friedman G, et al. Characteristics and outcomes of patients with cancer requiring admission to intensive care units: a prospective multicenter study. Crit Care Med. 2010;38:9–15.
Borcoman E, Dupont A, Mariotte E, Doucet L, Joseph A, Chermak A, et al. One-year survival in patients with solid tumours discharged alive from the intensive care unit after unplanned admission: a retrospective study. J Crit Care. 2020;57:36–41.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
Study concept and design FG, RS and DM. Data analysis, figures and statistics FG, RS and DM. Drafting of the manuscript FG, RS and DM. Critical revision of the manuscript, all the authors. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
According to French regulations, this study was approved by our local Institutional Review Board (n°2020–067), which waived the need for signed consent.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Gonzalez, F., Starka, R., Ducros, L. et al. Critically ill metastatic cancer patients returning home after unplanned ICU stay: an observational, multicentre retrospective study. Ann. Intensive Care 13, 73 (2023). https://doi.org/10.1186/s13613-023-01170-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01170-5