Abstract
Background
The worldwide dissemination of extended spectrum beta-lactamase producing Enterobacteriales (ESBL-E) is of major concern. Microbiota may play a role in the host resistance to colonization with ESBL-E, but the underlying mechanisms remain unknown. We aimed to compare the gut microbiota composition between ESBL-producing E. coli or K. pneumoniae carriers and ESBL-E non-carriers according to the bacterial species.
Results
Among 255 patients included, 11 (4,3%) were colonized with ESBL-producing E. coli and 6 (2,4%) with ESBL-producing K. pneumoniae, which were compared with age- and sex-matched ESBL-E non carriers. While no significant differences were found between ESBL-producing E. coli carriers and non-carriers, gut bacteriobiota α-diversity was decreased in ESBL-K. pneumoniae faecal carriers compared both with non-carriers (p = 0.05), and with ESBL-producing E. coli carriers. The presence of Sellimonas intestinalis was associated with the absence of ESBL-producing E. coli fecal carriage. Campylobacter ureolyticus, Campylobacter hominis, bacteria belonging to Clostridium cluster XI and Saccharomyces sp. were associated with the absence of ESBL-producing K. pneumoniae faecal carriage.
Conclusions
The composition of the gut microbiota differs between ESBL-producing E. coli and K. pneumoniae faecal carriers suggesting that microbial species should be taken into account when investigating the role of gut microbiota in resistance to gut colonization with ESBL-E.
Trial registration number: NCT04131569, date of registration: October 18, 2019.
Similar content being viewed by others
Background
Antimicrobial resistance in both community and healthcare-acquired infections is a major public health concern leading to about 35,000 associated deaths per year in Europe [1] and with 10,000,000 deaths per year worldwide expected in 2050 according to the World Health Organization [2]. Extended spectrum beta-lactamase (ESBL) producing Enterobacteriales (ESBL-E) are a major source of both antimicrobial resistance and empirical antimicrobial therapy failure in Europe. Containment measures, including antimicrobial stewardship, have been installed but with limited impact [3]. Consequently, new strategies to contain ESBL-E dissemination are urgently needed.
Gut microbiota is nowadays suggested to be a key player in host resistance to colonization with multi-drug resistant organisms (MDRO), including ESBL-E [4]. This resistance to colonization is mediated both by indirect mechanisms (i.e., the microbiota stimulating host immune defences) but also by direct interactions between microbial species as commensal species can directly suppress intestinal pathogens by competitive exclusion and antimicrobial activities (i.e., type IV secretion systems, production of bacteriocins, …) [4, 5]. A first step into the analysis of gut microbiota composition associated with the resistance to the acquisition of MDRO has identified the presence of Lactobacillus sp. to be protective but this study did not specifically assess the type of antimicrobial resistance nor the bacterial species [6]. A step forward has been performed regarding colonization with vancomycin-resistant Enterococcus faecium (VRE) allowing the identification of a bacterial consortium restoring colonization resistance to VRE [7]. The modulation of gut microbiota has been proposed as a new strategy to contain MDRO dissemination by re-establishing microbiota-mediated colonization resistance which markedly reduced infections with those antibiotic-resistant bacteria [5].
However, the association of gut microbiota composition and the underlying mechanisms involved in the resistance to colonization with ESBL-E in critically ill patients remains unknown. The impact of the bacterial species carrying the ESBL enzyme, Escherichia coli or Klebsiella pneumoniae being the most frequently isolated species on clinical samples, is also unknown. The aim of this study is thus to compare the gut bacterial and fungal microbiota (bacteriobiota and mycobiota) composition between patients colonized with ESBL-producing E. coli and K. pneumoniae and to compare gut microbiota composition between ESBL-E faecal carriers and non-carriers according to the bacterial species carrying the ESBL enzyme.
Methods
Patients inclusion and data collection
Every consecutive patient older than 18 years of age admitted to the medical ICU at Bordeaux university hospital from October 2019 to March 2020 was prospectively screened to participate to Microbe study (NCT04131569). ESBL-E faecal carriage was diagnosed by isolation of bacteria from rectal swabs performed within the first 2 h after admission to ICU prior any antimicrobial therapy in ICU on chromID ESBL® culture media (bioMérieux® reference number: 43481) and confirmed by culture with MAST® AMPC & ESBL DETECTION DISCS D68C. Bacterial or fungal species were further identified using MALDI–TOF mass spectrometer, Bruker Biotyper, Bremen, Germany®.
Data were prospectively recorded by physicians in charge of the patient by questioning the patients, patients’ family and patients’ general practitioners. Electronic worksheets were completed by two medical intensive care residents. Definitions of comorbidities are available in the Additional information.
Samples collection and preparation for microbiota analysis
Rectal swabs (Transport Swab VWR, Copan®) used for faecal ESBL-E carriage screening at admission were collected and frozen at − 80 °C. DNA extraction was performed by QIAamp® PowerFaecal® Pro DNA kit (QIAgen®). A step of mechanical lysis (2 cycles of 30 s at 7,000 rpm on Precellys evolution) was added to the chemical lysis of the kit as previously described [8]. V3–V4 regions of 16SRNA gene and ITS2 loci of rDNA gene were amplified by PCR. Sequencing (2 × 250 bp paired-end) was performed on MiSeq sequencer (Illumina®) at the PGTB platform (INRAe, Pierroton, France).
Bioinformatics analysis
DADA2 pipeline on R software (R foundation for Statistical Computing Vienna, Austria) was used for bioinformatics analyses [9]. DADA2 pipeline was preferred as it allows inter-studies comparison (if identical primers are used for amplification) [9] and is more accurate for mycobiota analysis [10]. We defined bacteriobiota as the bacterial kingdom of the microbiota and mycobiota as the fungal kingdom of the microbiota. Gut bacteriobiota and mycobiota α-diversity was expressed by Shannon index, Simpson index and evenness. This reflects the within sample diversity taking into account the number of different species and their relatives abundances in this sample. Between sample beta-diversity differences (measured using Bray Curtis dissimilarity) were tested using a permutational multivariate ANOVA (PERMANOVA) from “vegan” package with 10,000 permutations, while accounting for individual identity as a covariate. This β-diversity reflects between sample diversity and how similar is the composition of the microbiota between the samples included in the analysis. Gut bacteriobiota and mycobiota α and β diversities were compared thanks to “Phyloseq” package on R software. Linear discriminant analysis (LDA) effect size (LefSe) analysis was performed was performed from microbiomeMarker package. In brief, this analysis first uses the non-parametric factorial Kruskal–Wallis (KW) sum-rank test to detect features with significant differential abundance with respect to the class of interest (ESBL-E facal carriage or not); biological significance is subsequently investigated using a set of pairwise tests among subclasses using the (unpaired) Wilcoxon rank-sum test. As a last step, LEfSe uses Linear Discriminant Analysis to estimate the effect size of each differentially abundant feature [11]. We used mock communities (compositions in the Additional information) and negative controls (three from the DNA extraction step with unloaded swabs and three from the PCR amplification step) to ensure the sequencing quality. Comparison of β-diversity between negative control, mock community and samples are available in Additional file 1: Figs. S1 and S2 for bacteriobiota and mycobiota respectively. The final average read counts were 66,434 (standard deviation ± 17,634) for 1285 bacterial amplicon sequence variants (ASVs) and 3,647 (standard deviation ± 1267) for 361 fungal ASVs. The 16S rRNA gene and ITS2 sequences have been submitted to the European Nucleotide Archive (Accession N◦ Accession N◦ ERP134947). Statistical analysis was performed with the R studio program (version 1.3.1056 for Windows™); correction for multiple-testing was performed using the Benjamini–Hochberg false discovery rate (FDR) procedure, a p value or FDR adjusted p value equal to or less than 0.05 was considered statistically significant.
Statistical analysis
No statistical sample size calculation was performed a priori, and sample size was equal to the number of patients admitted to ICU during the study period. As ESBL-E fecal carriers, especially these colonized with ESBL-producing K. pneumoniae, are known to have more comorbidities than ESBL-E non fecal carriers [12, 13], control patients were selected as consecutive patients matched on sex and age ± 5 years but not on comorbidities and severity scores.
Quantitative variables are presented as median and interquartile range (IQR) and compared by use of the Mann–Whitney Wilcoxon rank-sum test. Categorical variables are expressed as number of patients (percentage) and compared by mean of the χ2 or Fisher tests. All statistical tests were two-tailed and statistical significance was defined as p < 0.05. Statistical analyses were assessed by the R 3.6.0 statistical software.
Ethics
According to French law and the French Data Protection Authority, the handling of these data for research purposes was declared to the Data Protection Officer of the Bordeaux university hospital. The study obtained the approval of the Institutional Review Board of the University Hospital of Bordeaux (declaration number CER–BDX-2021-37). Patients (or their relatives, if any) were notified about the anonymized use of their healthcare data via the department's booklet.
Results
Flow-chart
Among the 255 patients admitted to single centre ICU, 23 (9%) had a faecal carriage with an ESBL-E: 11/23 (48%) E. coli, 6/23 (26%) K. pneumoniae and 6/23 (8%) Enterobacter aerogenes, Citrobacter freundii or Serratia marcescens (2 patients for each) (Fig. 1). Because of statistical issues, only ESBL-producing E. coli and K. pneumoniae faecal carriers were further included in the analysis. In this analysed population, every ESBL-E fecal carriage was community-acquired but 2 ESBL-producing E. coli carriage were hospital-acquired prior to admission to ICU.
ESBL-producing K. pneumoniae faecal carriers exhibit a lower α-diversity of gut bacteriobiota, but not mycobiota, than ESBL-producing E. coli faecal carriers
To fully decipher the impact of bacterial and fungal microbiota on ESBL-E faecal carriage, we first compared clinical characteristics between ESBL-producing K. pneumoniae and E. coli faecal carriers (Table 1). In brief, ESBL-producing K. pneumoniae faecal carriers had higher SAPS2 score (80, IQR: 68–96 vs 55, IQR: 31–68, p = 0.007) and a higher rate of acute kidney injury (AKI) (6/6 (100%) vs 2/11 (18%), p = 0.002) but similar age, sex-ratio, haemodynamic or respiratory failure rates at admission to ICU compared with ESBL-producing E. coli faecal carriers. The proportion of patients hospitalized or who received prior antimicrobial therapy within the 3 previous months was not different between ESBL-producing K. pneumoniae and E. coli faecal carriers nor between each group compared with matched controls (Table 1). Furthermore, the compositions of the gut bacteriobiota and mycobiota were not different between patients who received antimicrobial therapy within the 3 months prior to admission to ICU (Additional file 1: Fig. S3). Gut bacteriobiota α-diversity was lower for ESBL-producing K. pneumoniae faecal carriers compared to ESBL-producing E. coli faecal carriers regarding Shannon and Simpson indexes, and evenness (p = 0.02, p = 0.007 and p = 0.007, respectively) (Fig. 2A–C), but β-diversity was not different (p = 0.44) (Fig. 1D). We did not find any difference in gut mycobiota α- or β-diversity between patients colonized with ESBL-producing K. pneumoniae and ESBL-producing E. coli (Additional file 1: Fig. S4A–D).
Comparison of gut bacteriobiota between critically ill ESBL-producing Escherichia coli and Klebsiella pneumoniae faecal carriers. A. Boxplot of estimated α-diversity by Shannon index. B. Boxplot of estimated α-diversity by Simpson index. C. Boxplot of estimated α-diversity by evenness. D. Metric Bray–curtis analysis of β-diversity. red: E. coli, green: K. pneumoniae. Threshold for statistical significance: p = 0.05
As it seems of crucial importance to consider not only the phenotype of antimicrobial resistance but also the bacterial species carrying the antimicrobial resistance determinant(s), we further compare independently the microbiota composition of ESBL-producing K. pneumoniae and E. coli faecal carriers to sex- and age-matched non ESBL-E faecal carriers in 1:2 proportion.
Gut bacteriobiota and mycobiota diversities are not different between ESBL-producing E. coli faecal carriers and non-carriers but microbial community enrichment was associated with the absence of ESBL-E faecal carriage
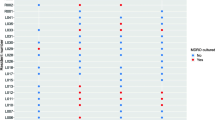
ESBL-producing E. coli faecal carriers’ characteristics were similar to non ESBL-E faecal carriers excepting a lower rate of AKI (p = 0.03) (Table 1). Both α and β diversities of gut bacteriobiota and mycobiota were not dissimilar between ESBL-producing E. coli faecal carriers and non ESBL-E faecal carriers (Additional file 1: Figs. S5, S6A–D). However, using LDA method to compare gut microbiota composition between ESBL-producing E. coli faecal carriers and non ESBL-E faecal carriers, the presence of Sellimonas intestinalis was associated with the absence of ESBL-producing E. coli faecal carriage (LDA score > 3) (Fig. 3A). To the contrary, the presence of Candida albicans appeared to be associated with ESBL-producing E. coli faecal carriage (Fig. 3B).
Comparison of bacterial and fungal species abundances between critically ill ESBL-E fecal carriers and matched non ESBL-E faecal carriers. A. Bacterial species abundances between ESBL-producing E. coli fecal carriers and matched non ESBL-E faecal carriers. B. Fungal species abundances between ESBL-producing E. coli fecal carriers and matched non ESBL-E faecal carriers. C. Bacterial species abundances between ESBL-producing K. pneumoniae fecal carriers and matched non ESBL-E faecal carriers. D. Fungal species abundances between ESBL-producing K. pneumoniae fecal carriers and matched non ESBL-E faecal carriers LefSe analysis with linear discriminant analysis (LDA). Threshold for statistical significance: LDA > 3log. ASV: amplicon sequence variant
ESBL-producing K. pneumoniae faecal carriers exhibit a lower α-diversity of gut bacteriobiota but not mycobiota than non-carriers
ESBL-producing K. pneumoniae faecal carriers had higher SAPSII scores and AKI rates compared to non ESBL-E faecal carriers despite those differences being non-significant (p = 0.08 and p = 0.11, respectively) (Table 1).
Gut bacteriobiota α-diversity was lower in ESBL-producing K. pneumoniae faecal carriers compared to non ESBL-E faecal carriers (respectively for Shannon and Simpson indexes and evenness p = 0.12, p = 0.05 and p = 0.03, respectively) (Fig. 4A–C), but β-diversity was not different (p = 0.8) (Fig. 4D). We did not find any difference in gut mycobiota α- or β-diversity (Additional file 1: Fig. S7A–D).
Comparison of gut bacteriobiota between critically ill ESBL-producing Klebsiella pneumoniae faecal carriers (in red) and matched non ESBL-E faecal carriers (in blue). A. Boxplot of estimated α-diversity by Shannon index. B. Boxplot of estimated α-diversity by Simpson index. C. Boxplot of estimated α-diversity by evenness. D. Metric Bray–curtis analysis of β-diversity. Threshold for statistical significance: p = 0.05
Identification of probiotic candidates for ESBL-producing K. pneumoniae tailored decontamination
Using LDA analysis to detect significant microbial community enrichment, we identified a consortium of bacteria associated with the absence of ESBL-producing K. pneumoniae faecal carriage (LDA score > 3) including Campylobacter hominis, Campylobacter ureolyticus, Porphyromonas sp., Clostridiales fam XI (Peptoniphilus and Anaerococcus) (Fig. 3C).
Analyzing fungal species, amplicon sequence variants (ASV) related to Issatchenkia orientalis (Candida krusei), Dipodascus geotrichum (Geotrichum candidum) and to Candida tropicalis were significantly associated with ESBL-producing K. pneumoniae faecal carriage; while ASV related to Saccharomyces species were associated either with the colonization or the absence of colonization with ESBL-producing K. pneumoniae (Fig. 3D).
Discussion
To the best of our knowledge, this study is the first to compare the gut microbiota compositions between ESBL-producing K. pneumoniae and E. coli carriers and to include the analysis of gut mycobiota. Notably, we identified a decreased α-diversity of gut bacteriobiota in ESBL-producing K. pneumoniae compared to ESBL-producing E. coli faecal carriers. Gut microbiota diversities were not different between ESBL-E producing E. coli faecal carriers and non ESBL-E faecal carriers, but ESBL-producing K. pneumoniae faecal carriers exhibited a lower gut bacteriobiota α-diversity, compared to non ESBL-E faecal carriers.
Two previous study investigated the link between gut bacteriobiota composition and gut colonization with MDRO in ICU, one finding no difference in gut bacteriobiota α- and β-diversities between 13 MDRO carriers and 18 non-carriers [14] and the other that Family XI and Prevotellaceae families are more abundant in non-carriers than in MDRO carriers [15]. Nevertheless, these studies included ESBL, carbapenemase and/or high-level AmpC producing Enterobacterales, ceftazidime-resistant Pseudomonas aeruginosa and Stenotrophomonas maltophilia. The mixing of different bacterial species with different pathogenicity abilities, virulence factors and diverse interactions with other microbial species may provide heterogeneity in the analysis.
In our study, gut microbiota α-diversity was found to be different between ESBL K. pneumoniae fecal carriers and other groups, but not β diversity. This apparent discrepancy is not unusual in microbiota studies as α-diversity reflects the within sample diversity taking into account the number of different species and their relatives abundances in this sample whereas the β-diversity reflects between sample diversity and how similar is the composition of the microbiota between the samples included in the analysis.
The decreased α-diversity of gut bacteriobiota in patients colonized with ESBL-producing K. pneumoniae compared with ESBL-producing E. coli faecal carriers and non-carriers of ESBL-producing Enterobacterales, could be, at least partially, explained by the fact that these patients are frailer with more comorbidities as previously described [13] and that increased host frailty is associated with altered gut bacteriobiota composition [16]. This enhances the importance to take the bacterial specie and not only the antimicrobial resistance mechanism into account when assessing the impact of gut microbiota on the fecal carriage of MDRO. Moreover, the correlation between the decrease in α-diversity of the gut microbiota and the inoculum size of the colonizing ESBL-E will soon be feasible thanks to the recently improved sequencing accuracy of the long-read sequencing technologies.
Regarding the community and long-term facility residents, a first study did not find any association between gut microbiota dynamics and colonization with extended-spectrum cephalosporin-resistant Enterobacteriaceae in healthy Swiss travellers to India [17]. Another study did not find either any difference in gut microbiota α-diversity between ESBL-E carriers compared with non-carriers in Thaïland community but find a significant dissimilarity (β-diversity) between the 2 groups, probably reflecting the fact that ESBL-E faecal carriage was significantly lower in farmers than in people with other professions. The presence of Bacteroides uniformis was statistically more abundant in ESBL-E non-carriers than in carriers [18]. The same comparison in the Amerindian Wayampi community showed that ESBL-E faecal carriers had a lower gut bacteriobiota α-diversity than non-carriers while taxa belonging to the genera Desulfovibrio and Oscillospira (Ruminococcaceae) were associated with the absence of ESBL-E faecal carriage and Prevotella was associated with ESBL-E faecal carriage [19]. Comparison of gut bacteriobiota between ESBL-E faecal carriers and non-carriers, not in the community but in nursing home residents, found a decreased α-diversity in ESBL-E faecal carriers with a depletion in butyrate-producing bacterial species and an enrichment in succinate-producing bacterial species [20]. While the impact of microbiota on MDRO is mediated by indirect mechanisms including local and systemic immune activation and by direct mechanisms including competition for nutrients between species composing the microbiota and direct toxicity, none of these studies took ESBL-E bacterial species into account. Only one study specifically assessed the impact of ESBL-E bacterial species in a mice model of ESBL-producing K. pneumoniae gut colonization and concluded that the microbial composition plays a primary role in MDR-colonization rate, whereas the antibiotic susceptibility of individual MDR strains affects this process in a lesser extent [21] enhancing the relevance of taking into account the bacterial specie carrying the resistance mechanism.
Regarding the identification of potential probiotics for tailored ESBL-producing E. coli faecal carriage decontamination, S. intestinalis could be an interesting candidate as it belongs to Clostridiales cluster XIVa which includes several butyrate-producing or bacteriocin-producing bacterial species. S. intestinalis has only been discovered in 2016 and requires further investigation [22,23,24]. The fact that C. albicans presence is associated with ESBL-producing E. coli faecal carriage is of major interest as C. albicans wall components provide a higher level of E. coli resistance to ofloxacin within a polymicrobial biofilm [25]. Furthermore, mannose and mannans composing C. albicans wall seem to inhibit E. coli phagocytosis by macrophages [26].
Regarding the identification of potential probiotics for tailored ESBL-producing K. pneumoniae faecal carriage decontamination, few data exist about the interactions between identified bacterial and fungal species and K. pneumoniae. Several studies suggest that bacterial species belonging to Campylobacter genus are associated with a decreased inoculum of K. pneumoniae. In fact, broilers fed with Campylobacter jejuni have lower amount of K. pneumoniae isolated at both ileal and caecal areas [27]. This antagonism seems to be two-sided as K. pneumoniae is also able to products metabolites that decrease C. jejuni growth [28, 29]. In this study, we identified Saccharomyces sp. to be associated both with ESBL-producing K. pneumoniae carriage and non-carriage. Explaining this apparent discrepancy, species belonging to Saccharomyces genus have been reported to have contrary interactions with K. pneumoniae. One one hand, Saccharomyces boulardii supernatant inhibits K. pneumoniae metabolism and growth [30]. On the other hand, Saccharomyces cerevisiae seems to stimulate K. pneumoniae growth via the production of 3-hydroxypropionic acid and quinone pyrroloquinolin [31, 32]. Regarding Candida tropicalis and Issatchenkia orientalis (also known as Candida krusei), only one study assessed their potential interaction with K. pneumoniae and did not find any effect of K. pneumoniae lipopolysaccharides on in vitro biofilm formation of these Candida species [33] and no data are available for Dipodascus geotrichum.
The potential role of gut mycobiota should not be underestimated in the resistance to colonization with ESBL-E as demonstrated by the identification of fungal species associated with the presence or absence of colonizing ESBL-E. Besides the direct inter-kingdoms interactions occurring in the microbiota [34], commensal fungi also modulate local and systemic immunity [35].
The main limitation is the monocentric character of our study and the relative small number of patients. Age- and sex-matching was performed to limit microbiota composition variability as these 2 factors are key determinants of microbiota composition [36,37,38]. Patients were not matched on comorbidities and severity as ESBL-producing K. pneumoniae fecal carriers have more cardiovascular and neurological comorbidities and are more immunosuppressed than ESBL-producing E. coli fecal carriers and ESBL-E non carriers [12, 13]. The absence of matching on these parameters would have been a bias if we were looking for an independent association between the gut microbiota composition and the ESBL-E colonization or if we wanted to explain the causes of these alterations. To the contrary, we aimed to compare these gut microbiota alterations between ESBL-E fecal carriers and non-carriers, whether or not these alterations are due to the comorbidities of the patients or the severity of the disease. Besides, the use of DADA2 pipeline will allow comparison of the results from different teams if the same primers are used for gene amplification, thus allowing reproducibility assessment [9, 39]. Interestingly, we did not find significant difference in the proportion of patients hospitalized within the 3 previous months which could be consistent with the global dissemination of E-ESBL in the community. Nevertheless, as discussed above, ESBL-producing K. pneumoniae fecal carriers had higher SAPS2 score and a higher rate of AKI compared to ESBL-producing E. coli fecal carriers and a trend compared to non fecal-carriers which could partly explain our results. In fact, it is highly plausible that critical illness [40] and frailty [16] could reduce gut microbial diversity thus impairing host colonization resistance to pathogens [4]. This has been suggested long before the onset of metagenomics tools to investigate gut microbiota composition as aged, frail patients have been demonstrated to have high proportion of oropharyngeal colonization with Gram-negative bacilli even in the absence of previous antimicrobial therapy [41]. If so, persistence of the underlying condition responsible for this frailty or persistence of the critical illness could impair the long-term efficacy of exogenic gut microbiota diversity restoration for providing colonization resistance and could lead to treatment failure or need for repeated probiotics administration [5]. Another limitation is the lack of causality demonstration. To get beyond the association links provided in this study, animal models are needed to assess the real ability of identified probiotic candidates to eradicate ESBL-E faecal carriage.
Moreover, concerns exist about the translocation of probiotics given to patients with increased gut permeability [42] as occurring in ICU patients. In vitro studies are thus needed to identify the underlying mechanisms of micro-organisms inhibition (i.e., bacteriocin production, environment pH modulation via butyrate production, metabolic antagonism, …) as tailored decontamination could also be mediated via microbial metabolites and/or products.
Conclusions
The composition of the gut microbiota differs between ESBL-producing E. coli and ESBL-producing K. pneumoniae faecal carriers: ESBL-producing K. pneumoniae faecal carriers exhibiting lower gut bacteriobiota α-diversity compared to ESBL-producing E. coli faecal carriers and ESBL-E non carriers. These data suggest that bacterial species, in addition to the mechanism of antimicrobial resistance, should be taken into account when investigating the role of gut microbiota in the resistance to gut colonization with ESBL-E. This approach could lead to identification of probiotic candidates for tailored gut decontamination in ESBL-E faecal carriers admitted to ICU.
Availability of data and materials
The 16S rRNA gene and ITS2 sequences have been submitted to the European Nucleotide Archive (Accession N◦ ERP134947). The scripts used for bioinformatics analysis during the current study are available from the corresponding author on reasonable request.
Abbreviations
- AKI:
-
Acute kidney injury
- ASV:
-
Amplicon sequence variant
- ESBL-E:
-
Extended spectrum beta-lactamase producing Enterobacteriales
- ICU:
-
Intensive care unit
- IQR:
-
Interquartile range
- LDA:
-
Linear discriminant analysis
- LefSe:
-
LDA effect size
- MDRO:
-
Multi-drug resistant organism
- PERMANOVA:
-
Permutational multivariate ANOVA
- SAPSII:
-
Simplified acute physiology score II
- VRE:
-
Vancomycin-resistant Enterococcus faecium
References
Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. the lancet infectious diseases. 2019;19(1):56–66.
Hoffman SJ, Outterson K, Røttingen J-A, Cars O, Clift C, Rizvi Z, et al. An international legal framework to address antimicrobial resistance. Bull World Health Organ. 2015;93:66–66.
Delannoy M, Agrinier N, Charmillon A, Degand N, Dellamonica J, Leone M, et al. Implementation of antibiotic stewardship programmes in French ICUs in 2018: a nationwide cross-sectional survey. J Antimicrob Chemother. 2019;74:2106–14.
Buffie CG, Pamer EG. Microbiota-mediated colonization resistance against intestinal pathogens. Nat Rev Immunol. 2013;13:790–801.
Pamer EG. Resurrecting the intestinal microbiota to combat antibiotic-resistant pathogens. Science. 2016;352:535–8.
Araos R, Tai AK, Snyder GM, Blaser MJ, D’Agata EMC. Predominance of Lactobacillus spp. among patients who do not acquire multidrug-resistant organisms. Clin Infect Dis. 2016;63:937–43.
Caballero S, Kim S, Carter RA, Leiner IM, Sušac B, Miller L, et al. Cooperating commensals restore colonization resistance to Vancomycin-resistant Enterococcus faecium. Cell Host Microbe. 2017;21:592-602.e4.
Vandenborght L-E, Enaud R, Urien C, Coron N, Girodet P-O, Ferreira S, et al. Type 2-high asthma is associated with a specific indoor mycobiome and microbiome. J Allergy Clin Immunol. 2021;147:1296-1305.e6.
Callahan BJ, McMurdie PJ, Rosen MJ, Han AW, Johnson AJA, Holmes SP. DADA2: High resolution sample inference from Illumina amplicon data. Nat Methods. 2016;13:581–3.
Pauvert C, Buée M, Laval V, Edel-Hermann V, Fauchery L, Gautier A, et al. Bioinformatics matters: the accuracy of plant and soil fungal community data is highly dependent on the metabarcoding pipeline. Fungal Ecol. 2019;41:23–33.
Segata N, Izard J, Waldron L, Gevers D, Miropolsky L, Garrett WS, et al. Metagenomic biomarker discovery and explanation. Genome Biol. 2011;12:R60.
Livermore DM, Hope R, Brick G, Lillie M, Reynolds R. BSAC working parties on resistance surveillance non-susceptibility trends among enterobacteriaceae from bacteraemias in the UK and Ireland. J Antimicrob Chemother. 2008;62(2):41–54.
Scheuerman O, Schechner V, Carmeli Y, Gutiérrez-Gutiérrez B, Calbo E, Almirante B, et al. Comparison of predictors and mortality between bloodstream infections caused by ESBL-producing Escherichia coli and ESBL-producing Klebsiella pneumoniae. Infect Control Hosp Epidemiol. 2018;39:660–7.
Fontaine C, Armand-Lefèvre L, Magnan M, Nazimoudine A, Timsit J-F, Ruppé E. Relationship between the composition of the intestinal microbiota and the tracheal and intestinal colonization by opportunistic pathogens in intensive care patients. PLoS ONE. 2020;15: e0237260.
Rubio E, Vergara A, Aziz F, Narváez S, Cuesta G, Hernández M, et al. Changes in the gut microbiota and risk of colonization by multidrug-resistant bacteria, infection and death in critical care patients. Clin Microbiol Infect. 2022;1:1223.
Claesson MJ, Jeffery IB, Conde S, Power SE, O’Connor EM, Cusack S, et al. Gut microbiota composition correlates with diet and health in the elderly. Nature. 2012;488:178–84.
Pires J, Kraemer JG, Kuenzli E, Kasraian S, Tinguely R, Hatz C, et al. Gut microbiota dynamics in travelers returning from India colonized with extended-spectrum cephalosporin-resistant Enterobacteriaceae: a longitudinal study. Travel Med Infect Dis. 2019;27:72–80.
Piewngam P, Quiñones M, Thirakittiwatthana W, Yungyuen T, Otto M, Kiratisin P. Composition of the intestinal microbiota in extended-spectrum β-lactamase-producing Enterobacteriaceae carriers and non-carriers in Thailand. Int J Antimicrob Agents. 2019;53:435–41.
Gosalbes MJ, Vázquez-Castellanos JF, Angebault C, Woerther P-L, Ruppé E, Ferrús ML, et al. Carriage of Enterobacteria producing extended-spectrum β-Lactamases and composition of the gut microbiota in an Amerindian community. Antimicrob Agents Chemother. 2016;60:507–14.
Le Bastard Q, Chapelet G, Birgand G, Hillmann BM, Javaudin F, Hayatgheib N, et al. Gut microbiome signatures of nursing home residents carrying Enterobacteria producing extended-spectrum β-lactamases. Antimicrob Resist Infect Control. 2020;9:107.
Juhász J, Ligeti B, Gajdács M, Makra N, Ostorházi E, Farkas FB, et al. Colonization dynamics of multidrug-resistant Klebsiella pneumoniae are dictated by microbiota-cluster group behavior over individual antibiotic susceptibility: a metataxonomic analysis. Antibiotics. 2021;10:268.
Seo B, Yoo JE, Lee YM, Ko G. Sellimonas intestinalis gen nov., sp. nov., isolated from human faeces. Int J Syst Evol Microbiol. 2016;66:951–6.
Versluis D, de Bello González J, Zoetendal T, Passel EG, van Mark WJ, Smidt H. High throughput cultivation-based screening on porous aluminum oxide chips allows targeted isolation of antibiotic resistant human gut bacteria. PLoS ONE. 2019;14:210970.
Van den Abbeele P, Belzer C, Goossens M, Kleerebezem M, De Vos WM, Thas O, et al. Butyrate-producing Clostridium cluster XIVa species specifically colonize mucins in an in vitro gut model. ISME J. 2013;7:949–61.
De Brucker K, Tan Y, Vints K, De Cremer K, Braem A, Verstraeten N, et al. Fungal β-1,3-glucan increases ofloxacin tolerance of Escherichia coli in a polymicrobial E. coli/Candida albicans biofilm. Antimicrob Agents Chemother. 2015;59:3052–8.
Felipe I, Bochio EE, Martins NB, Pacheco C. Inhibition of macrophage phagocytosis of Escherichia coli by mannose and mannan. Braz J Med Biol Res. 1991;24:919–24.
Johansen CH, Bjerrum L, Finster K, Pedersen K. Effects of a campylobacter jejuni infection on the development of the intestinal microflora of broiler chickens. Poult Sci. 2006;85:579–87.
Schoeni JL, Doyle MP. Reduction of campylobacter jejuni colonization of chicks by cecum-colonizing bacteria producing anti-C jejuni metabolites. Appl Environ Microbiol. 1992;58:664–70.
Schoeni JL, Wong AC. Inhibition of campylobacter jejuni colonization in chicks by defined competitive exclusion bacteria. Appl Environ Microbiol. 1994;60:1191–7.
Kirillov DA, Perunova NB, Chelpachenko OE, Elagina NN, Valyshev AV, Bukharin OV. Modifying action of Saccharomyces boulardii on the biological properties of enterobacteria. Mikrobiol Epidemiol Immunobiol. 2002;1:57–9.
Wang K, Wang X, Ge X, Tian P. Heterologous expression of aldehyde dehydrogenase from Saccharomyces cerevisiae in Klebsiella pneumoniae for 3-hydroxypropionic acid production from glycerol. Indian J Microbiol. 2012;52:478–83.
Ohsugi M, Noda H, Muro K, Ishiba A, Kondo Y, Nakao S. Effects of the yeast extract components pyrroloquinoline quinone and aspartic acid on vitamin B12 production in Klebsiella pneumoniae IFO 13541. J Nutr Sci Vitaminol. 1989;35:661–5.
Bandara HMHN, Lam OLT, Watt RM, Jin LJ, Samaranayake LP. Bacterial lipopolysaccharides variably modulate in vitro biofilm formation of Candida species. J Med Microbiol. 2010;59:1225–34.
Enaud R, Prevel R, Ciarlo E, Beaufils F, Wieërs G, Guery B, et al. The gut-lung axis in health and respiratory diseases: a place for inter-organ and inter-kingdom crosstalks. Front Cell Infect Microbiol. 2020;10:9.
Jiang TT, Shao T-Y, Ang WXG, Kinder JM, Turner LH, Pham G, et al. Commensal fungi recapitulate the protective benefits of intestinal bacteria. Cell Host Microbe. 2017. https://doi.org/10.1016/j.chom.2017.10.013.
Goodrich JK, Waters JL, Poole AC, Sutter JL, Koren O, Blekhman R, et al. Human genetics shape the gut microbiome. Cell. 2014;159:789–99.
Lynch SV, Pedersen O. The human intestinal microbiome in health and disease. N Engl J Med. 2016;375:2369–79.
The Human Microbiome Project Consortium. Structure, function and diversity of the healthy human microbiome. Nature. 2012;486:207–14.
Callahan BJ, McMurdie PJ, Holmes SP. Exact sequence variants should replace operational taxonomic units in marker-gene data analysis. ISME J. 2017;11:2639–43.
Lankelma JM, van Vught LA, Belzer C, Schultz MJ, van der Poll T, de Vos WM, et al. Critically ill patients demonstrate large interpersonal variation in intestinal microbiota dysregulation: a pilot study. Intensive Care Med. 2017;43:59–68.
Valenti WM, Trudell RG, Bentley DW. Factors predisposing to oropharyngeal colonization with gram-negative bacilli in the aged. N Engl J Med. 1978;298:1108–11.
Yelin I, Flett KB, Merakou C, Mehrotra P, Stam J, Snesrud E, et al. Genomic and epidemiological evidence of bacterial transmission from probiotic capsule to blood in ICU patients. Nat Med. 2019;25:1728–32.
Acknowledgements
We would like to thank Fabien Beaufils for his participation in the “Bordeaux Micro-Mycobiota Study Group”.
We would like to thank Erwan Guichoux and Marie Massot for technical assistance.
Funding
Funded by a grant from “Fédération Girondine de Lutte contre les Maladies Respiratoires. RP received a personal salary grant from CHU de Bordeaux (MD/PhD program).
Author information
Authors and Affiliations
Contributions
RP, PB, LD, AB and DG contributed to the conception and design of the study. AO, PS, FMZ and VD contributed to the acquisition of data. RP and AC performed DNA extraction. RP and RE performed bioinformatics and statistical analysis. Each author drafted or provided critical revision of the article and provided final approval of the version submitted for publication. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Research Ethics Committee of Bordeaux university hospital (CER BDX-2021-37) and performed according to The Code of Ethics of the World Medical Association (Declaration of Helsinki).
An informed consent was obtained from all patients or from their legal representatives.
Consent for publication
Not applicable
Competing interests
On behalf of all authors, the corresponding author states that there is no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Non metric Bray-curtis analysis of β-diversity of the V3-V4 sequencing run. XXA, B, and C samples: gut bacteriobiota samples. GXX: lung bacteriobiota samples. BlancV3-V4: negative control. Mock: mock community. Figure S2. Non metric Bray-curtis analysis of β-diversity of ITS2 sequencing run. XXA, B, and C samples: gut mycobiota samples. GXX: lung mycobiota samples. Blanc1 and blanc2: negative controls. Mock: mock community. Figure S3. Comparison of gut bacteriobiota and mycobiota between critically ill ESBL-producing Enterobacteriales fecal carriers and non-carriers. A. Boxplot of estimated α-diversity for gut bacteriobiota by Shannon index. B. Boxplot of estimated α-diversity for gut bacteriobiota by Simpson index. C. Metric Bray-curtis analysis of β-diversity for gut bacteriobiota. Threshold for statistical significance: p=0.05. D. Boxplot of estimated α-diversity for gut mycobiota by Shannon index. E. Boxplot of estimated α-diversity for gut mycobiota by Simpson index. F. Metric Bray-curtis analysis of β-diversity for gut mycobiota. Threshold for statistical significance: p=0.05. ATB: prior antimicrobial therapy within the 3 previous months. no-ATB: no prior antimicrobial therapy within the 3 previous months. Figure S4. Comparison of gut mycobiota between critically ill ESBL-producing Escherichia coli and Klebsiella pneumoniae faecal carriers. A. Boxplot of estimated α-diversity by Shannon index. B. Boxplot of estimated α-diversity by Simpson index. C. Boxplot of estimated α-diversity by evenness. D. Metric Bray-curtis analysis of β-diversity. red: E. coli, green: K. pneumoniae. Threshold for statistical significance: p=0.05. Figure S5. Comparison of gut bacteriobiota between critically ill ESBL-producing Escherichia coli (in red) and matched non ESBL-E (in blue) faecal carriers. A. Boxplot of estimated α-diversity by Shannon index. B. Boxplot of estimated α-diversity by Simpson index. C. Boxplot of estimated α-diversity by evenness. D. Metric Bray-curtis analysis of β-diversity. Threshold for statistical significance: p=0.05. Figure S6. Comparison of gut mycobiota between critically ill ESBL-producing Escherichia coli faecal carriers (in red) and matched non ESBL-E faecal carriers (in blue). A. Boxplot of estimated α-diversity by Shannon index. B. Boxplot of estimated α-diversity by Simpson index. C. Boxplot of estimated α-diversity by evenness. D. Metric Bray-curtis analysis of β-diversity. Threshold for statistical significance: p=0.05. Figure S7. Comparison of gut mycobiota between critically ill ESBL-producing Klebsiella pneumoniae faecal carriers (in red) and matched non ESBL-E faecal carriers (in blue). A. Boxplot of estimated α-diversity by Shannon index. B. Boxplot of estimated α-diversity by Simpson index. C. Boxplot of estimated α-diversity by evenness. D. Metric Bray-curtis analysis of β-diversity. Threshold for statistical significance: p=0.05.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Prevel, R., Enaud, R., Orieux, A. et al. Bridging gut microbiota composition with extended-spectrum beta-lactamase Enterobacteriales faecal carriage in critically ill patients (microbe cohort study). Ann. Intensive Care 13, 25 (2023). https://doi.org/10.1186/s13613-023-01121-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01121-0