Abstract
Background
The rise in antimicrobial resistance is a global threat responsible for about 33,000 deaths in 2015 with a particular concern for extended-spectrum beta-lactamase-producing Enterobacterales (ESBL-E) and has led to a major increase in the use of carbapenems, last-resort antibiotics.
Methods
In this retrospective propensity-weighted multicenter observational study conducted in 11 ICUs, the purpose was to assess the efficacy of non carbapenem regimen (piperacillin–tazobactam (PTZ) + aminoglycosides or 3rd-generation cephalosporin (3GC) + aminoglycosides) as empiric therapy in comparison with carbapenem in extended-spectrum β-lactamase-producing Enterobacterales (ESBL-E) urinary septic shock. The primary outcome was Day-30 mortality.
Results
Among 156 patients included in this study, 69 received a carbapenem and 87 received non carbapenem antibiotics as empiric treatment. Baseline clinical characteristics were similar between the two groups. Patients who received carbapenem had similar Day-30 mortality (10/69 (15%) vs 6/87 (7%), OR = 1.99 [0.55; 5.34] p = 0.16), illness severity, resolution of septic shock, and ESBL-E infection recurrence rates than patients who received an empiric non carbapenem therapy. The rates of secondary infection with C. difficile were comparable.
Conclusions
In ESBL-E urinary septic shock, empiric treatment with a non carbapenem regimen, including systematically aminoglycosides, was not associated with higher mortality, compared to a carbapenem regimen.
Similar content being viewed by others
Background
The rise in antimicrobial resistance is a major threat worldwide [1]. The spread of ESBL-E has led to a major increase in the use of carbapenems resulting in the emergence of carbapenem-resistant Enterobacterales (CRE). It is therefore essential to avoid the use of carbapenems as much as possible [2,3,4,5]. ESBL-E mostly remain susceptible to piperacillin-tazobactam (about 85% of ESBL-producing Escherichia coli isolates and 70% of ESBL-producing Klebsiella pneumoniae) [6] and to certain aminoglycosides, especially amikacin (about 87% of both ESBL-producing E. coli and K. pneumoniae) [7]. Regimen, including those molecules, should be investigated as alternatives to carbapenems [8,9,10].
Regarding severe ESBL-E infections, a retrospective, multicenter study conducted in 2019 [11], including about 100 patients in ICU, found no significant difference between a beta-lactam–beta-lactamase inhibitor (βL–βLI) combination and carbapenem regarding Day-30 mortality but only 6% of these infections were urinary tract ones. The randomized international multicenter MERINO trial [12] did not achieve to demonstrate the non-inferiority of PTZ compared to meropenem regarding the mortality at Day-30 in the treatment of 3GC-resistant E. coli and K. pneumoniae bloodstream infections but UTI was present only in 60% of the patients. Regarding urinary tract infections [13,14,15], the third leading cause of septic shock, aminoglycosides are of particular interest as carbapenem-sparing candidates due to their excellent diffusion in the urinary tract [16]. A recent study confirmed this potential interest but included only 10% of septic shock [17]. Despite those encouraging results, current recommendations strongly recommend the use of carbapenems as empiric treatment in urinary septic shock patients with risk factors for ESBL-E infections [18, 19].
The aim of this study is thus to compare the efficacy of carbapenem vs non carbapenem therapy as empiric antimicrobial therapy in ESBL-E urinary septic shock patients.
Methods
Study design and inclusion criteria
The SCRUTIN study is a retrospective cohort study conducted in 11 French intensive care units (ICU) from 8 teaching hospitals and 3 general hospitals. Every patient admitted to ICU for septic shock of urinary tract origin between January, 2014 and December, 2020 was considered for inclusion. Septic shock was defined according to the SEPSIS III definition. ESBL-E urinary tract infection was diagnosed by isolation of bacteria from urine culture with antimicrobial susceptibility testing performed with Vitek 2 instrument (bioMérieux®, Marcy l’Étoile, France). ESBL production was defined as resistance to one or more oxyimino cephalosporins (e.g., ceftazidime, ceftriaxone, cefotaxime) and confirmed by culture thanks to ESBL Etest (bioMérieux®) [20]. Bacterial species was further identified by MALDI Biotyper®, Bruker, Bremen, Germany. Patients were included if they received a carbapenem or a non carbapenem agent (3GC + amikacin or PTZ + amikacin) as empiric therapy. For patients with multiple episodes of urinary septic shock due to ESBL-E, only the first episode was considered. Non-inclusion criteria were infection with a Carbapenem-resistant Enterobacterales, a suspected associated source of infection, and decisions of withholding or withdrawing intensive therapies.
Data collection
Data were retrospectively collected from the electronic medical records and electronic worksheet was completed by two medical intensive care investigators.
Comorbidities were defined as follows: chronic obstructive pulmonary disease and asthma were defined according to lung function testing. Chronic heart failure was defined according to transthoracic echocardiography and chronic coronary disease based on stress test or percutaneous coronary intervention. Other comorbidities included history of chronic kidney disease (glomerular filtration rate < 60 mL/min/1.73 m2), immunosuppression (drugs, hematological disease, blood marrow transplantation, solid organ transplantation, plasma exchanges indicated by autoimmune disorders, human immunodeficiency virus infection), Charlson score, and simplified acute physiology score II (SAPSII). Acute respiratory distress syndrome (ARDS) was defined according to Berlin’s criteria and AKI to KDIGO guidelines.
Nosocomial acquisition was considered when symptoms of infection started over 48 h after hospital admission or within 48 h of hospital discharge, whereas we considered healthcare-associated acquisition if patients had attended hemodialysis or received intravenous chemotherapy in the past 30 days, had been admitted to an acute-care hospital for at least 2 days or had surgery in the past 90 days, or resided in a nursing home or long-term care facility. Other infections were considered community acquired.
In this retrospective study, no recommendation was made to physicians. However, to guide the collection of data, the risk factors for infection with an ESBL-E considered for the choice of carbapenems were, within the 3 previous months, the use of 2GC, 3GC, amoxicillin–clavulanic acid or fluoroquinolones, a trip in an endemic area, hospitalization, history of UTI, or colonization with ESBL-E for community patients, according to current recommendations [21]. In healthcare-associated infections, prolonged hospitalization in a long-stay facility and the presence of an indwelling catheter or gastrostomy are additional factors. The susceptibilities of bacterial isolates were defined according to EUCAST guidelines [20], i.e., susceptibility to PTZ (MIC ≤ 8 mg/L) and to aminoglycosides (MIC ≤ 8 mg/L for amikacin, ≤ 2 mg/L for gentamicin). Recurrence of an ESBL-E infection, occurrence of a CRE infection, or a Clostridioides difficile infection could only be investigated during the current hospitalization.
Outcomes
The primary efficacy outcome was death from any cause at Day 30 after admission to ICU.
Secondary outcomes were in-ICU mortality, Day-90 mortality, ICU and hospital length of stay, illness severity defined by the duration and maximum dose of norepinephrine, use of mechanical ventilation, use of renal replacement therapy, and time to clinical cure which was defined as the first day at which the patient experienced resolution of septic shock (norepinephrine withdrawal) + resolution of sepsis according to clinical (resolution of fever) and biological criteria (decrease by at least twofold of the leukocyte count).
Statistical analyses
No statistical sample size calculation was performed a priori, and sample size was equal to the number of patients admitted to ICU with urinary septic shock due to ESBL-E during the study period. Qualitative variables were described with frequencies and proportions. Quantitative variables were described with frequencies, mean, standard deviation, median, minimum, maximum, 1st, and 3rd quartiles. The quantitative variables were compared by Student t test if the conditions of validity were respected (normal distribution, homogeneous variances) or Student t test for unequal variances in other cases; if the distribution was not normal, the non-parametric Wilcoxon test was used. The qualitative variables were compared with a Chi2 test, or corrected Chi2 test, or with non-parametric Fisher’s exact test, according to the size of the expected values under the hypothesis of independence. All statistical tests were 2-tailed and statistical significance was defined as p < 0.05.
Prescribing carbapenem or a non carbapenem solution in urinary tract-onset septic shock could be related to a patient severity profile. Thus, physicians might have a propensity to treat more severe patients with carbapenems and less severe patients with a non carbapenem regimen. We therefore constructed a propensity score for receiving carbapenems in the empiric treatment of urinary septic shock. For this purpose, we performed a univariate and then a multivariate logistic regression of the risk of being treated with carbapenems compared to an alternative. The explanatory variables retained were age, sex (male), Charlson index, cardiovascular history, immunosuppression status, presence of risk factors for ESBL-E infection, SOFA score, and obstructive pyelonephritis. The propensity score of each patient was then integrated into the multivariate model analyzing the risk factors of mortality at Day-30 to adjust for the impact of the empiric treatment. The treatment effect was estimated by a weighted logistic regression model. The parameters of the model were estimated by bootstrapping. The balancing property of propensity score was assessed graphically using standardized differences before and after ponderation by weighting.
Ethics
The study obtained the approval of the Institutional Review Board of the Bordeaux University Hospital (CER-BDX-2022-02). This database is registered by the Commission Nationale Informatique et Libertés (CNIL, Registration no 2222361v0.).
Results
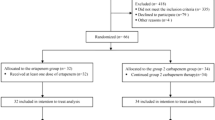
One hundred and fifty-six patients admitted to ICU for ESBL-E urinary septic shock between January 2014 and December 2020 were retrospectively included, 69 (44%) treated with carbapenem, and 87 (56%) with non carbapenem empiric therapy (36 patients treated with 3GC + aminoglycoside, 56 patients treated with PTZ + aminoglycoside) (Fig. 1).
Patients’ baseline characteristics are summarized in Table 1. Baseline characteristics were similar overall between patients receiving carbapenem and those receiving non carbapenem therapy, i.e., the rate of immunocompromised patients in both groups (respectively, 26 (38%) vs 32 (37%), p = 0.91) or the Charlson Index (respectively, 4 [2;6], and 3 [1.5;5], p = 0.37). Nevertheless, patients treated with non carbapenem therapy had more often cardiovascular history (70/87 (80%) vs 42/69 (61%), p = 0.01) but less history of urinary tract infections (41/87 (47%) vs 45/69 (65%), p = 0.02) particularly regarding ESBL-E infections (7/87 (17%) vs 28/69 (62%), p < 0.001) (Table 1).
Patients’ presentation
SAPS2 was significantly higher in the carbapenem group than in the non carbapenem group (respectively, 54 [46;65] vs 63 [55;71], p < 0.001) but not the SOFA score (8 [7;10] vs 8 [6;10], p < 0.56). Regarding organ failure, there was no significant difference in the rate of respiratory failure nor in the rate of cardiac impairment, but more patients in the carbapenem group had acute kidney injury (64/69 (93%) vs 70/87 (80.4%), p = 0.03) (Table 1). In the non carbapenem group, there were significantly more patients with lithiasis on urinary tract imaging (respectively, 11/69 (22%) vs 19/87 (16%), p = 0.05) (Additional file 1).
Source control
Regarding the need for urological surgery, the two groups were comparable (29/69 (39%) vs 39/87 (45%), p = 0.47). All patients with urinary tract dilatation, regardless of the cause (lithiasis or non-lithiasis), underwent urinary diversion by catheterization (Additional file 2).
Antimicrobial therapy
All patients in the non carbapenem group received aminoglycosides (78/87 received amikacin and 9/87 gentamycin). Only 5/69 patients of the carbapenem group did not receive aminoglycosides (61 received amikacin and 3 received gentamycin). 3GC therapy (n = 36) included cefotaxime (n = 25) and ceftriaxone (n = 11). Between H24 and H72, ESBL could be suspected either during the laboratory identification process or following information delivered by the family physician about ESBL carriage: 22 of the 56 patients receiving an empirical TZP treatment were switched to carbapenems, TZP was maintained in 18, and 6 received cotrimoxazole, 6 fluoroquinolones, and 4 cefoxitin. Another 31 patients received 3GC whom 9 were switched to carbapenems, 10 TZP, 5 fluoroquinolones, 4 cotrimoxazole, and 3 to cefoxitin. In the carbapenem group, 5 were switched to TZP, 3 cotrimoxazole, and 2 to fluoroquinolones. Total duration of antimicrobial treatment was 14 days [14;14] for carbapenem group and 14 days [14;15] for non carbapenem group (p = 0.5) (Table 2). Regarding aminoglycosides, 64/69 (93%) of patients receiving meropenem also received aminoglycosides infusion (57 (89%) 1 dose, 6 (9%) 2 doses, and 1 (2%) 3 doses); 56/56 (100%) of patients receiving TZP also received aminoglycosides (49 (88%) 1 dose, 5 (9%) 2 doses, and 2 (3%) 3 doses); and 31/31 (100%) of patients receiving 3CG also received aminoglycosides (25 (81%) 1 dose, 4 (13%) 2 doses, and 2 (6%) 3 doses). β-lactam therapy was never discontinued even in the case of susceptibility to aminoglycosides.
Microbiological considerations
Escherichia coli and K. pneumoniae were the two most frequently isolated bacteria (52% and 30%, respectively). Most patients had associated bloodstream infections (52/69 (75%) in the carbapenem group vs 57/87 (65%) in the non carbapenem group, p = 0.07). Thirty-three out of 69 (48%) of the isolates were susceptible to PTZ (CMI ≤ 8 mg/L) in the carbapenem group vs 65/89 (65%) in the non carbapenem group (p = 0.06) and 62/69 (90%) and 80/87 (92%) were susceptible to aminoglycosides, respectively. Adequate empirical antimicrobial therapy was not different between non carbapenem (95%) and carbapenem groups (respectively, 95% vs 94%, p = 1.0) (Table 2). In the non carbapenem group, survivors and non-survivors had no difference regarding the proportion of susceptible isolated bacteria: (53/81 (65%) vs 4/6 (66%), p = 1.00) were TZP susceptible and (75/81 (93%) vs 5/6 (83%), p = 0.40) were susceptible to aminoglycosides. All the isolated bacteria were susceptible to the combination of TZP and aminoglycosides.
Primary outcome and propensity score
After adjustment to the weighted propensity score (Additional file 3), there was no significant difference in mortality at Day 30 between the patients receiving carbapenem (10/69, (14%)) or non carbapenem therapy (6/87, (7%)) as empiric antimicrobial therapy (OR = 0.50 95% CI [0.19–1.80], p = 0.16).
Secondary outcomes
There was no significant difference regarding in-ICU mortality rate, Day-90 mortality, ICU length of stay, and hospital length of stay (Table 3). The use of renal replacement therapy was comparable in both groups, as was the need for invasive mechanical ventilation or vasopressive support with dobutamine. Maximal dose and duration of vasopressive support with norepinephrine were similar between the two groups. Time to clinical cure assessed by the Kaplan–Meier curve showed no difference between the two groups (3.8 days in the carbapenem group vs 3.3 days in the non carbapenem group, log rank test, p = 0.38) (Fig. 2). No difference in superinfection rates was observed between carbapenem and non carbapenem groups (n = 7; 10% vs n = 15; 17%; p = 0.56), respectively. No interaction in D30 mortality Odds ratios was observed between the subgroup of patients infected with PTZ R (OR 0.74; 95% CI 0.07–8.56) or S (OR 1.11; 95% CI 0.28–4.37) strains (p = 0.18). Only 1/36 patients treated with 3GC + aminoglycoside died.
Kaplan–Meier curves of reflecting the probability of clinical cure according to the empirical antimicrobial therapy group (carbapenem vs non carbapenem regimen). Kaplan–Meier curves was weighted with the propensity score. For patients with treatment failure, data were censored for length of hospitalization. P-value results from the Log Rank Test
Discussion
In this original study of ESBL-E urinary septic shock patients, no difference in Day-30 mortality and time to clinical cure was observed in patients treated with a non carbapenem empiric therapy compared with those treated with carbapenems. This is the first study showing the potential efficacy of non carbapenem therapy as empiric treatment in ESBL-E urinary tract septic shock. Treatment of infections with ESBL-E remains a challenge extensively discussed in the literature, but very few data regarding urinary septic shock patients were reported to date.
The current French guidelines [21] recommend the use of carbapenems whenever there is a risk factor for infection with an ESBL-E. Nevertheless, those risk factors were determined in studies conducted in countries with high ESBL-E prevalence and mostly in retrospective studies [22]. The INCREMENT cohort compared empiric treatment with non carbapenem agents (86 patients mainly aminoglycosides (n = 42) and fluoroquinolones) vs carbapenems (245 patients). No significant difference in 30-day mortality between those two groups was observed [23]. Another retrospective study compared empiric therapy with aminoglycosides vs carbapenems or PTZ for the treatment of ESBL-E UTIs, demonstrating the non-inferiority of aminoglycosides in terms of 30-day mortality. However, these studies involved only a low rate of septic shock [17]. In our study, the role of systematically administrated aminoglycosides along with carbapenem or non carbapenem therapy is probably important as they are known to have a good penetration of urinary tract and as shown by the low mortality rate of patients treated with 3 GC + aminoglycoside.
PTZ is another interesting candidate as a carbapenem-sparing agent. Yoon et al. compared the clinical efficacy of PTZ vs ertapenem and showed no significant difference regarding microbiological eradication failure (respectively, 4.4% vs 4.9%, p = 1.00) and in-hospital mortality (respectively, 4.4% vs 13.4%, p = 0.06) [24]. Another multicenter retrospective propensity-matched control study included 186 patients with ESBL-E urinary tract infections, 27% of whom admitted in ICU and found no difference in the resolution of clinical symptoms by Day 7 or in 30-day mortality [25]. Several retrospective cohort studies compared the efficacy of PTZ to carbapenems as empiric antimicrobial therapy in ESBL-E bloodstream infections with neither difference regarding mortality nor clinical response [23]. Another French retrospective multicenter study, including about 100 severe ESBL infections, did not find any significant difference between a combination of beta-lactamase inhibitors and carbapenems on mortality at D30, but only 6% of these infections were urinary tract infections [11]. Finally, in a meta-analysis including 35 publications, no significant differences in overall mortality between a carbapenem vs a non carbapenem regimen was showed [26].
The only randomized trial investigating the non-inferiority of PTZ vs meropenem on Day-30 mortality in the treatment of 3GC-resistant E. coli and K. pneumoniae bloodstream infection (UTI in 60% of the patients) did not prove non-inferiority of a carbapenem-sparing strategy, including PTZ, compared with meropenem (Day-30 mortality, respectively, 12.3% and 3.7% (CI 97.5% [− ∞; + 14.5] p = 0.9)) [12], but some critics have cautioned the authors’ conclusions that PTZ was inferior and carbapenems therefore recommended [10].
In our study, Day-30 mortality is estimated at 10%, which is clearly below the rates reported by the various descriptive epidemiological studies in France and Europe [13]. This could be explained by the fact that mortality is lower in patients with septic shock from urinary tract compared to other sources. The optimization of the management of septic shock since the Sepsis Survey Campaign can also have played a role. Finally, it is suggested that virulence and resistance could possibly be antagonistic in Gram-negative bacteria especially Escherichia coli [27].
The major limitation of this study is its retrospective design limiting the ability to draw definitive conclusions. Nevertheless, we used a weighted propensity-matched analysis to decrease the impact of potential confounding factors. Our study focuses only on ESBL-E, which differs from the Merino cohort, which also included C3G-resistant strains through production of AmpC cephalosporinase, which has a direct impact on PTZ susceptibility. In addition, MICs for TZP were within the EUCAST guidelines of 8 mg/L or less, and strains classified as intermediate were considered resistant in this study. Regarding the percentages of Escherichia coli and Klebsiella pneumoniae isolates susceptible to PTZ and aminoglycosides, our results were in agreement with epidemiological studies [7]. Moreover, in both groups, mortality at Day30 was not related to urinary septic shock treatment failure but rather to complications of ICU stay. Besides, the absence of difference in D30 mortality in the non carbapenem group could be explained by the substantial number of patients in the non carbapenem group who were switched to carbapenem as soon as ESBL was suspected. Finally, this study had not sufficient power to detect small differences, such as the rate of superinfections, which was slightly higher in the non carbapenem group (17 vs 10%) without statistical significant difference.
Conclusions
In ESBL-E urinary septic shock, when the empirical treatment include an aminoglycoside and is thus adequate, the 30-day mortality of patients was not different whatever the β-lactam used (carbapenem or non carbapenem).Therefore, our results strongly encourage for future large multicenter prospective non-inferiority randomized study aiming at confirming that a strategy, including non carbapenem β-lactam and aminoglycoside, is safe alternatives to carbapenems as empirical antimicrobial therapy in ESBL-E urinary septic shock.
Availability of data and materials
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- 2GC:
-
2nd-generation cephalosporin
- 3GC:
-
3rd-generation cephalosporin
- AKI:
-
Acute kidney injury
- ARDS:
-
Acute respiratory distress syndrome
- βL-βLIs:
-
β-lactam–β-lactamase inhibitors
- CNIL:
-
Commission Nationale de l'Informatique et des Libertés
- CRE:
-
Carbapenem-resistant Enterobacterales
- ESBL:
-
Extended-spectrum β-lactamase
- ESBL-E:
-
Extended-spectrum β-lactamase—Enterobacterales
- EUCAST:
-
European Committee on Antimicrobial Susceptibility Testing
- HAS:
-
Haute Autorité de Santé
- ICU:
-
Intensive care unit
- IQR:
-
Inter quartile range
- KDIGO:
-
Kidney Disease Improving Global Outcomes
- MDR:
-
Multi-drug Résistant
- MIC:
-
Minimum Inhibitory Concentration
- ONERBA:
-
Observatoire National de l’Epidémiologie de la Résistance aux Antibiotiques
- PMSI:
-
Programme de Médicalisation des Systèmes d’Information
- PTZ:
-
Piperacillin/Tazobactam
- SAPS:
-
Simplified acute physiology score
- SOFA:
-
Sequential Organ Failure Assessment
- SRLF:
-
Société de Réanimation de Langue Française
- UTI:
-
Urinary tract infection
- WHO:
-
World Health Organization
References
Cassini A, Högberg LD, Plachouras D, Quattrocchi A, Hoxha A, Simonsen GS, et al. Attributable deaths and disability-adjusted life-years caused by infections with antibiotic-resistant bacteria in the EU and the European Economic Area in 2015: a population-level modelling analysis. Lancet Infect Dis. 2019;19(1):56–66.
Armand-Lefèvre L, Angebault C, Barbier F, Hamelet E, Defrance G, Ruppé E, et al. Emergence of imipenem-resistant gram-negative bacilli in intestinal flora of intensive care patients. Antimicrob Agents Chemother. 2013;57(3):1488–95.
Tansarli GS, Karageorgopoulos DE, Kapaskelis A, Falagas ME. Impact of antimicrobial multidrug resistance on inpatient care cost: an evaluation of the evidence. Expert Rev Anti Infect Ther. 2013;11(3):321–31.
McLaughlin M, Advincula MR, Malczynski M, Qi C, Bolon M, Scheetz MH. Correlations of antibiotic use and carbapenem resistance in enterobacteriaceae. Antimicrob Agents Chemother. 2013;57(10):5131–3.
Le Terrier C, Vinetti M, Bonjean P, Richard R, Jarrige B, Pons B, et al. Impact of a restrictive antibiotic policy on the acquisition of extended-spectrum beta-lactamase-producing Enterobacteriaceae in an endemic region: a before-and-after, propensity-matched cohort study in a Caribbean intensive care unit. Crit Care. 2021;25:261.
Schuetz AN, Reyes S, Tamma PD. Point-counterpoint: piperacillin-tazobactam should be used to treat infections with extended-spectrum-beta-lactamase-positive organisms. J Clin Microbiol. 2018;56(3):e01917-17.
Rapports ONERBA—Onerba. http://onerba.org/publications/rapports-onerba/. Accessed 7 Aug 2021.
Pierrotti LC, Pérez-Nadales E, Fernández-Ruiz M, Gutiérrez-Gutiérrez B, Tan BH, Carratalà J, et al. Efficacy of β-lactam/β-lactamase inhibitors to treat extended-spectrum beta-lactamase-producing Enterobacterales bacteremia secondary to urinary tract infection in kidney transplant recipients (INCREMENT-SOT Project). Transpl Infect Dis. 2021;23(3):e13520.
Pilmis B, Jullien V, Tabah A, Zahar JR, Brun-Buisson C. Piperacillin-tazobactam as alternative to carbapenems for ICU patients. Ann Intensive Care. 2017;7(1):113.
Rodríguez-Baño J, Gutiérrez-Gutiérrez B, Kahlmeter G. Antibiotics for ceftriaxone-resistant gram-negative bacterial bloodstream infections. JAMA. 2019;321(6):612–3.
Luyt CE, Faure M, Bonnet I, Besset S, Huang F, Junot H, et al. Use of non-carbapenem antibiotics to treat severe extended-spectrum β-lactamase-producing Enterobacteriaceae infections in intensive care unit patients. Int J Antimicrob Agents. 2019;53(5):547–52.
Harris PNA, Tambyah PA, Lye DC, Mo Y, Lee TH, Yilmaz M, et al. Effect of Piperacillin-Tazobactam vs Meropenem on 30-day mortality for patients with E. coli or Klebsiella pneumoniae bloodstream infection and ceftriaxone resistance: a randomized clinical trial. JAMA. 2018;320(10):984–94.
Quenot JP, Binquet C, Kara F, Martinet O, Ganster F, Navellou JC, et al. The epidemiology of septic shock in French intensive care units: the prospective multicenter cohort EPISS study. Crit Care Lond Engl. 2013;17(2):R65.
Annane D, Bellissant E, Cavaillon JM. Septic shock. Lancet Lond Engl. 2005;365(9453):63–78.
Rhodes A, Evans LE, Alhazzani W, Levy MM, Antonelli M, Ferrer R, et al. Surviving Sepsis Campaign: International Guidelines for Management of Sepsis and Septic Shock: 2016. Intensive Care Med. 2017;43(3):304–77.
Karaiskos I, Giamarellou H. Carbapenem-sparing strategies for ESBL producers: when and how. Antibiot Basel Switz. 2020;9(2):E61.
Zohar I, Schwartz O, Yossepowitch O, David SSB, Maor Y. Aminoglycoside versus carbapenem or piperacillin/tazobactam treatment for bloodstream infections of urinary source caused by Gram-negative ESBL-producing Enterobacteriaceae. J Antimicrob Chemother. 2020;75(2):458–65.
Paul M, Carrara E, Retamar P, Tängdén T, Bitterman R, Bonomo RA, et al. European Society of Clinical Microbiology and Infectious Diseases (ESCMID) guidelines for the treatment of infections caused by multidrug-resistant Gram-negative bacilli (endorsed by European society of intensive care medicine). Clin Microbiol Infect. 2022;28(4):521–47.
Tamma PD, Aitken SL, Bonomo RA, Mathers AJ, van Duin D, Clancy CJ. Infectious Diseases Society of America Guidance on the treatment of extended-spectrum β-lactamase producing enterobacterales (ESBL-E), carbapenem-resistant enterobacterales (CRE), and Pseudomonas aeruginosa with difficult-to-treat resistance (DTR-P. aeruginosa). Clin Infect Dis Off Publ Infect Dis Soc Am. 2021;72(7):1109–16.
European Committee on Antimicrobial Susceptibility Testing. EUCAST warnings concerning antimicrobial susceptibility testing products or procedures. http://www.eucast.org/ast_of_bacteria/warnings/. Accessed 2 Nov 2018.
Antimicrobial therapy for Enterobacterales and Pseudomonas aeruginosa infections in adults: the role of carbapenems and their alternatives. Recommendations for good practice. HAS. 2019. https://has-sante.fr/jcms/c_2968915/fr/antibiotherapie-des-infections-a-enterobacteries-et-a-pseudomonas-aeruginosa-chez-l-adulte-place-des-carbapenemes-et-de-leurs-alternatives. Accessed 2 Dec 2022.
Tinelli M, Cataldo MA, Mantengoli E, Cadeddu C, Cunietti E, Luzzaro F, et al. Epidemiology and genetic characteristics of extended-spectrum β-lactamase-producing Gram-negative bacteria causing urinary tract infections in long-term care facilities. J Antimicrob Chemother. 2012;67(12):2982–7.
Palacios-Baena ZR, Gutiérrez-Gutiérrez B, Calbo E, Almirante B, Viale P, Oliver A, et al. Empiric therapy with carbapenem-sparing regimens for bloodstream infections due to extended-spectrum β-lactamase–producing enterobacteriaceae: results from the INCREMENT Cohort. Clin Infect Dis Off Publ Infect Dis Soc Am. 2017;65(10):1615–23.
Yoon YK, Kim JH, Sohn JW, Yang KS, Kim MJ. Role of piperacillin/tazobactam as a carbapenem-sparing antibiotic for treatment of acute pyelonephritis due to extended-spectrum β-lactamase-producing Escherichia coli. Int J Antimicrob Agents. 2017;49(4):410–5. https://doi.org/10.1016/j.ijantimicag.2016.12.017. Epub 2017 Mar 1. PMID: 28263710.
Sharara SL, Amoah J, Pana ZD, Simner PJ, Cosgrove SE, Tamma PD. Is piperacillin–tazobactam effective for the treatment of pyelonephritis caused by extended-spectrum β-lactamase-producing organisms? Clin Infect Dis. 2020;71(8):e331–7.
Son SK, Lee NR, Ko JH, Choi JK, Moon SY, Joo EJ, et al. Clinical effectiveness of carbapenems versus alternative antibiotics for treating ESBL-producing Enterobacteriaceae bacteraemia: a systematic review and meta-analysis. J Antimicrob Chemother. 2018;73(10):2631–42.
Johnson JR, Urban C, Weissman SJ, Jorgensen JH, Lewis JS, Hansen G, et al. Molecular epidemiological analysis of Escherichia coli sequence type ST131 (O25:H4) and bla CTX-M-15 among Extended-Spectrum-β-lactamase-producing E. coli from the United States, 2000 to 2009. Antimicrob Agents Chemother. 2012;56(5):2364–70.
Acknowledgements
The authors gratefully acknowledge each manager of the different centers who allowed us to include patients.
Funding
This research received no external funding.
Author information
Authors and Affiliations
Contributions
RP and AB contributed equally as co-last authors. EC, AO, RP, AD, DG, and AB contributed to the conception and design of the study. EC, SS, SF, TS, EC, SN, BS, JP, OG, TS, WP, and KK contributed to the acquisition of data. RG performed statistical analysis. Each author drafted or provided critical revision of the article. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study was approved by the Research Ethics Committee of Bordeaux University Hospital (CER-BDX-2022-02) and performed according to The Code of Ethics of the World Medical Association (Declaration of Helsinki) (CER-BDX-2022-02). This database is registered by the Commission Nationale Informatique et Libertés (CNIL, Registration no 2222361v0).
Consent for publication
Not applicable.
Competing interests
SF declared consulting fees from Novartis, Abionyx Pharma; personal fees from Vifor, Sanofi, Baxter; and support for attending meetings from Sanofi, Alexion. SN declared payment or honoraria for lectures from MSD, Pfizer, Gilead, Biomerieux, Biorad, Fisher & Paykel. EC declared payment or honoraria for lectures from Gilead, Shionozi, Sanofi, and support for attending meetings from Gilead, Shionozi, Sanofi. All the other authors have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Patients’ imaging presentation.
Additional file 2.
Interventions, source control and antimicrobial therapy.
Additional file 3.
Distribution of the propensity to receive carbapenem before vs after adjustment to the propensity score. Patients’ microbiological presentation, bacterial species and antibiotic susceptibility test.
Additional file 4.
Standardized differences before/after adjustment by weighting (95% CI).
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Cariou, E., Griffier, R., Orieux, A. et al. Efficacy of carbapenem vs non carbapenem β-lactam therapy as empiric antimicrobial therapy in patients with extended-spectrum β-lactamase-producing Enterobacterales urinary septic shock: a propensity-weighted multicenter cohort study. Ann. Intensive Care 13, 22 (2023). https://doi.org/10.1186/s13613-023-01106-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-023-01106-z