Abstract
Background
The COVID-19 pandemic is a heavy burden in terms of health care resources. Future decision-making policies require consistent data on the management and prognosis of the older patients (> 70 years old) with COVID-19 admitted in the intensive care unit (ICU).
Methods
Characteristics, management, and prognosis of critically ill old patients (> 70 years) were extracted from the international prospective COVID-ICU database. A propensity score weighted-comparison evaluated the impact of intubation upon admission on Day-90 mortality.
Results
The analysis included 1199 (28% of the COVID-ICU cohort) patients (median [interquartile] age 74 [72–78] years). Fifty-three percent, 31%, and 16% were 70–74, 75–79, and over 80 years old, respectively. The most frequent comorbidities were chronic hypertension (62%), diabetes (30%), and chronic respiratory disease (25%). Median Clinical Frailty Scale was 3 (2–3). Upon admission, the PaO2/FiO2 ratio was 154 (105–222). 740 (62%) patients were intubated on Day-1 and eventually 938 (78%) during their ICU stay. Overall Day-90 mortality was 46% and reached 67% among the 193 patients over 80 years old. Mortality was higher in older patients, diabetics, and those with a lower PaO2/FiO2 ratio upon admission, cardiovascular dysfunction, and a shorter time between first symptoms and ICU admission. In propensity analysis, early intubation at ICU admission was associated with a significantly higher Day-90 mortality (42% vs 28%; hazard ratio 1.68; 95% CI 1.24–2.27; p < 0·001).
Conclusion
Patients over 70 years old represented more than a quarter of the COVID-19 population admitted in the participating ICUs during the first wave. Day-90 mortality was 46%, with dismal outcomes reported for patients older than 80 years or those intubated upon ICU admission.
Similar content being viewed by others
Introduction
The severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a risk factor for acute respiratory distress syndrome (ARDS) that is currently a major healthcare challenge worldwide. The prognosis of this disease widely varies between countries, the age of the patients, the characteristics of the population studied, and the severity of the ARDS [1]. Then, the case fatality rates observed in ARDS-related SARS-CoV-2 is close to 30–40% [2,3,4], but can reach 70% in the older patients [5,6,7]. Given the heavy burden of ARDS-related SARS-CoV-2 infection in terms of health care resources and the worrisome prognosis of this disease, the pandemic has raised several ethical questions. One of them is the decision to admit the oldest patients in the ICU [8], which should be guided by robust data on the outcomes of that population. Therefore, there is an urgent need to provide consistent data on the management and prognosis of the elderly patients in the intensive care unit (ICU) [9]. These data may serve policymakers to properly and fairly allocate health care resources to that population and also to provide transparent information to the patient and caregivers. To date, few studies specifically reported the management and prognosis of the elderly patients in the context of SARS-CoV-2 lower respiratory tract infection [10, 11], but none were focused on a population admitted in ICU. In a large German study enrolling 10,021 patients, 923 (9%) patients over 70 years old received ventilatory support which was associated with 63% in-hospital mortality in those 70–79 years [4]. This result concurred with the dismal prognosis reported in previous studies focused on elderly patients with ARDS not related to SARS-CoV-2 infection [12, 13]. As the debate is still active whether the management of COVID-19 should differ from ARDS related to other causes [14], the specific ICU management and outcomes of the old patients with SARS-CoV-2 related ARDS has not been fully described so far. We sought to assess the characteristics, management, and prognosis of the patients over 70 years enrolled in the international COVID-ICU cohort [15].
Methods
Study design, patients
We performed an ancillary analysis of the COVID-ICU study. COVID-ICU was a multi-center, observational, and prospective cohort study conducted in 149 ICUs from 138 centers, across three countries (France, Switzerland, and Belgium) and has been described elsewhere [15]. It received approval from the ethical committee of the French Intensive Care Society (CE-SRLF 20-23) and Swiss and Belgium ethical committees following local regulations. All patients or close relatives were informed that their medical data were anonymously included in the COVID-ICU cohort. Patients and relatives had the possibility not to participate in the study. In case of refusal, the data were not collected accordingly. This manuscript follows the STROBE statement for reporting cohort studies.
For this analysis, we restricted the study population to patients who were 70 and above 70 years of age at the time of the admission to the participating ICU between February 25, 2020, and May 4, 2020, with laboratory-confirmed SARS-CoV-2 infection, and available Day-90 vital status. Laboratory confirmation for SARS-Cov-2 was defined as a positive result of real-time reverse transcriptase-polymerase chain reaction (RT-PCR) assay from either nasal or pharyngeal swabs, or lower respiratory tract aspirates [16].
Data collection
Full description of data collection is provided in the Additional file 1. Baseline information collected at ICU admission were: age, sex, body mass index (BMI), active smoking, Simplified Acute Physiology Score (SAPS) II score [17], worse Sequential Organ Failure Assessment (SOFA) [18] during the first 24 h, comorbidities, immunodeficiency (if present), Clinical Frailty Scale [19], the date of the first symptom, and dates of the hospital and ICU admissions. The Clinical Frailty Scale was collected upon ICU admission by the physician in charge of the patient during the medical examination. If the patient was not able to communicate, the physician obtained the information from the relatives. The Clinical Frailty Scale is an ordinal hierarchical scale of 9 ranks, with a score of 1 being very fit, 2 well, 3 managing well, 4 vulnerable, 5 mildly frail, 6 moderately frail, 7 severely frail, 8 very severely frail, and 9 terminally ill. We also collected modes of ventilation and oxygenation and complications over the ICU stay. Patient outcomes included duration of mechanical ventilation, vital status at ICU and hospital discharge, and 28, 60, and 90 days after ICU admission. Lastly, life-sustaining treatment decisions were also collected.
Statistical analyses
Characteristics of patients were described as frequencies and percentages for categorical variables, whereas continuous variables were reported as mean and standard deviation or median and interquartile range. Categorical variables were compared by Chi-square or Fisher's exact test, and continuous variables were compared by Student's t-test or Wilcoxon's rank-sum test. Kaplan–Meier overall survival curves until Day-90 were computed, and were compared using log-rank tests. Detailed statistical analysis is provided is the Additional file 1.
Baseline risk factors of death at Day-90 were assessed using univariate and multivariate Cox regression model stratified on the center variable. Proportional hazard assumption was assessed by inspecting the scaled Schoenfeld residuals and Harrell’s test [20]. To assess invasive mechanical ventilation effect on Day-90 mortality, we used a Cox proportional hazard model weighted on inverse probability of treatment weighting (IPTW) using propensity score (PS) defined as the predictive probability of invasive mechanical ventilation conditional on measured baseline covariates [21]. A multivariate logistic regression model was performed to estimate the PS for each patient in that population. To assess the balance of measured covariates between treatment groups, we used the standardized mean differences before and after PS weighting [22]. Then, a Cox proportional hazard model weighted on IPTW was performed to estimate the average treatment effect in the entire eligible population [21]. Hazard ratio and its 95% confidence interval were then estimated for the Day-90 mortality associated with invasive mechanical ventilation at Day-1. This analysis was performed on the complete cases data set, and a sensitivity analysis was performed using multiple imputations due to missing data.
All analyses were performed at a two-sided α level of 5% and conducted with R version 3.5.1 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Characteristics of patients at ICU admission
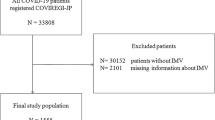
From the 4244 patients enrolled in the COVID-ICU dataset, 1199 (28%) (1115, 41, 43 patients in France, Switzerland, and Belgium, respectively) met the inclusion criteria of the present study (i.e., age over 70 years old) (see the Additional file 1: Figure S1). The main descriptors of the patient’s characteristics are presented in Table 1. The median (IQR) age was 74 (72–78) years. Fifty-three percent of the patients were 70–74 years old, 31% were 75–79 years old and 16% were over 80 years old. The majority of the patients were male (73%). The most frequent comorbidities were chronic hypertension (62%), diabetes (30%), and chronic respiratory disease (25%). Noticeably, the median (IQR) Clinical Frailty Scale was 3 (2–3), with only 160/1085 (15%) vulnerable patients (i.e., Clinical Frailty Scale 4), and 99/1085 (9%) frail patients (i.e., Clinical Frailty Scale 5–9). The time between first symptoms and ICU admission was 8 (6–12) days. SAPS II and SOFA scores at ICU admission were 43 (35–54) and 5 (3–8), respectively.
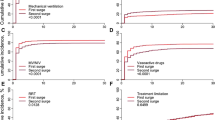
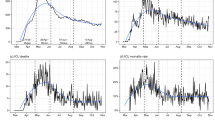
Mortality was 41%, 45%, and 46% at Day-28, Day-60, and Day-90, respectively (Additional file 1: Table S1). Mortality at Day-90 increased with the age and the Clinical Frailty Scale (Fig. 1). Indeed, Day-90 mortality increased from 39% in the patients between 70 and 74 years to 47% and 67% in the groups of patients between 75 and 79 years and those over 80 years old, respectively (p < 0.001) (Fig. 2a). Similarly, mortality at Day-90 was 40%, 61%, and 71% in the patients' groups with Clinical Frailty Scale from 1–3; 4; and ≥ 5, respectively (p < 0.001) (Fig. 2b). The mortality was also higher in patients intubated during their ICU stay ranging from 44 to 74% (Additional file 1: Figure S2). Of note, during the period of the first 14 days following the ICU admission, 253/1,199 (21%) of the patients had a life-sustaining treatment limitation decision, whom 223 (88%) died at day 90 (207 (82%) while in the ICU).
Predictive factors of mortality at Day-90
Results of the multivariable analysis are reported in Table 2. Because of multicollinearity observed between age and Clinical Frailty Scale, invasive mechanical ventilation at Day-1 and PaO2/FiO2 ratio, renal replacement therapy and the renal component of the SOFA, only Clinical Frailty Scale, PaO2/FiO2 ratio, and the renal component of the SOFA were retained in the model. Day-1 patients’ characteristics significantly associated with a higher 90-Day mortality rate identified by the Cox regression model after center stratification were older age, diabetes, higher cardiovascular component of the SOFA score, lower PaO2/FiO2, and a shorter time between first symptoms and ICU admission (Table 2). The same analysis re-run of missing after multiple imputations data (Additional file 1: Table S2) yielded similar conclusions. Interestingly, being admitted to the ICU after March 29 was also associated with a better outcome (Additional file 1: Figure S3). Kaplan–Meier survival estimates according to age categories, Clinical Frailty Scale, and PaO2/FiO2 ratio at Day-1 of ICU admission are provided in Fig. 2.
Propensity score analysis
Six hundred and forty-four patients had a cardiovascular component of the SOFA < 2, comprising 425 patients intubated on Day-1 and 219 initially treated without invasive mechanical ventilation. These two groups differed in several respects (Additional file 1: Table S3). Patients intubated on Day-1 had a higher SOFA cardiovascular component and were more likely admitted to the ICU before March 28. Interestingly, their Clinical Frailty Scale, their BMI, the time between first symptoms and ICU admission, and the PaO2/FiO2 ratio were not different. After weighting on the Inverse Probability Weighting Treatment using propensity score estimated in 269 patients with no missing values, 123 non-intubated patients were compared to 146 patients intubated at Day-1 with a similar medical history and initial severity Additional file 1: Table S3). We found a significantly different Day-90 mortality (28% in the non-intubated group vs. 42% in the intubated group; HR 1.68; 95% CI 1.24–2.27; p < 0.001) (Fig. 3). A similar analysis performed after multiple imputations of missing data (i.e., 644 patients) yielded similar conclusions (HR 1.33; 95% CI 1.11–1.59; p = 0.002).
Discussion
Herein, we report the characteristics, management, and outcomes of a large prospective cohort of old critically ill patients during the first wave of the COVID-19 outbreak. Patients over 70 years represented 28% of the COVID-19 population admitted during that period of 8 weeks in the participating ICUs. Their overall Day-90 mortality was 46%, which increased with the age and the Clinical Frailty Scale and reached 67% for the patients over 80 years. Older age, diabetes, a longer time between first symptoms and ICU admission, a SOFA cardiovascular component ≥ 3, a lower PaO2/FiO2 ratio, and being admitted to the ICU during the first month of the pandemic were independent risk factors of Day-90 mortality. Noticeably, our propensity score analysis suggests that an early invasive mechanical ventilation strategy seemed associated with a worse prognosis in that population.
The mortality of elderly patients admitted in the ICU for SARS-Cov-2-related ARDS varied from 77 to 84% [1]. These mortality rates appear very high compared to those reported in ARDS outside COVID-19 [12, 23]. For instance, the Large Observational Study to Understand the Global Impact of Severe Acute Respiratory Failure (LUNG SAFE) reported Day-90 mortality rates of 47%, 51%, and 50% for the 70–74 years, 75–79, and > 80 years old patients, respectively (unpublished data, personal communication from the authors) [24]. Our Day-90 mortality (46%) contrasts with early reports (1–3) and the large German cohort of 10,021 patients (923 patients over 70 years) [4] despite a large proportion of patients intubated during their ICU stay in our study (78%). It was, however much higher than the 25% Day-90 mortality observed in the rest of the population of the COVID-ICU cohort (i.e., patients < 70 years old) [15]. Besides, the mortality of our patients over 80 years old seems higher when compared with same-age patients with non-COVID-19-related ARDS, planned [25], or unplanned ICU admission [26]. Several factors such as triage policy before ICU admission, ICU resources at the time of the pandemic, ICU case volume [27] and patients’ comorbidities may explain these discrepancies.
Before the context of COVID-19, frailty as measured with the Clinical Frailty Scale in elderly critically ill patients was strongly associated with Day-30 mortality [26]. This tool was even a better predictor of mortality than SOFA score [25] or classical geriatric scales [26]. Recently, in a large observational study performed in the United Kingdom that enrolled 1564 COVID-19 patients with a median age of 74 years, and more than 50% of the population with a Clinical Frailty Scale > 4, the crude hazard ratio (95% confidence interval) for mortality were 3.12 (2.05–4.76) and 4.41 (2.90–6.71) for those with a Clinical Frailty Scale of 5–6 and 7 to 9, respectively [11]. However, the overall low Clinical Frailty Scale reported in our study and our low proportion of vulnerable or frail patients suggest that a significant triage was performed before ICU admission [28]. No national ICU admission criteria policy was provided at the time of the study, and the ICU admission decision was left to the discretion of the physicians in charge of the patient. Whether this triage resulted from intensivist’s evaluation, non-intensivists practitioner’s judgment, ICU beds occupancy, or the patients themselves should be further investigated.
Old patients admitted to the ICU with COVID-19 are at increased risk of death [3, 29] and the decision of ICU admission can be challenging [8]. The use of the Clinical Frailty Scale has proven to be helpful in this context [9]. Besides, the respect of the patient’s wishes and values, expressed directly by the patient via advance directives or reported by the healthcare surrogate should have to be taken into consideration [30]. In old patients with an uncertain prognosis, it can be particularly difficult to decide whether or not to admit to the ICU and provide invasive treatments such as mechanical ventilation. In such circumstances, an “ICU-trial of limited-time” has been proposed [31]. However, in the context of COVID-19, this strategy could be challenging as a long invasive mechanical duration is often required to see any clinical improvement. In other words, an ICU trial with a too-short limited-time could lead to misinterpretation and ethical misconduct. This important point is reinforced by the extremely long durations of invasive mechanical ventilation, and ICU length of stay observed in our surviving patients.
Beyond the admission of elderly patients in the ICU, the decision of the timing of intubation remains crucial. The majority of our patients (62%) were intubated on ICU Day-1. Interestingly, apart from obvious reasons such as hemodynamic instability, relevant clinical differences were scarce between patients who were intubated upon admission and those who were not. For instance, their Clinical Frailty Scale, time between first symptoms and ICU admission, and PaO2/FiO2 ratio were not significantly different, suggesting that the decision of intubation on admission was mainly driven by the experience of the physicians and the limited knowledge of this new disease at that time. As reported by others [32], the proportion of patients being intubated upon ICU admission during the first period of the study decreased from 67 to 56% during the last month (after March 29th, 2020), with being admitted in that latter period independently associated with a lower Day-90 mortality. An early intubation strategy was even associated with a poorer outcome in our matching analysis while further studies are warranted to confirm this finding. Less reluctance of the caregivers to provide non-invasive oxygen strategies along the first COVID-19 wave has been reported [15], but the benefit in terms of survival is still uncertain [33]. These strategies seem promising in that at-risk population where patients receiving invasive mechanical ventilation are more likely to experience long-term physical, neuropsychiatric, and quality of life impairments [34, 35].
Our study is a large international cohort of old critically ill patients with detailed characteristics and Day-90 outcome. However, despite a large number of participating ICUs, our population sample may be prone to selection biases that may limit generalizability. Since the study was mainly conducted in France (1115, 41 and 43 patients in France, Switzerland, and Belgium, respectively) during a period with high pressure on the health system and before the publication of several core randomized trials [36, 37], our findings may differ during subsequent COVID-19 outbreaks, and in countries with different public health care organizations, ICU admission policy, or ICU resources [4]. Comparison with further studies from other countries will help to better allocate health care resources and determine the indications and contra-indications of non-invasive ventilatory strategies in this specific population. Besides, we only provided data on patients who were admitted to the ICU, and no information was available on treatments before ICU admission nor on patients for whom an ICU admission was denied in the participating ICUs. Besides, important detailed information is also lacking regarding therapy limitations. This information would have allowed a thorough investigation of ICU-admission criteria used during this surge of ICU resources.
Conclusions
During the first COVID-19 pandemic wave, patients over 70 years old represented more than a quarter of the COVID-19 population in the participating ICUs of that study. Their overall Day-90 mortality was 46% with a dismal prognosis in patients older than 80 years old. Given the very long duration of mechanical ventilation as well as a prolonged ICU and hospital stay in the survivors, further studies are urgently warranted to evaluate the long-term psychological, neurocognitive, and functional outcomes of this high-risk and vulnerable population.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
References
Lim ZJ, Subramaniam A, Ponnapa Reddy M, et al. Case fatality rates for patients with COVID-19 requiring invasive mechanical ventilation. A meta-analysis. Am J Respir Crit Care Med. 2021;203:54–66.
Wang Y, Lu X, Li Y, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med. 2020;201:1430–4.
Grasselli G, Zangrillo A, Zanella A, et al. Baseline characteristics and outcomes of 1591 patients infected with SARS-CoV-2 admitted to ICUs of the Lombardy Region, Italy. JAMA. 2020;323:1574–81.
Karagiannidis C, Mostert C, Hentschker C, et al. Case characteristics, resource use, and outcomes of 10,021 patients with COVID-19 admitted to 920 German hospitals: an observational study. Lancet Respir Med. 2020;8:853–62.
Jiménez E, Fontán-Vela M, Valencia J, et al. Characteristics, complications and outcomes among 1549 patients hospitalised with COVID-19 in a secondary hospital in Madrid, Spain: a retrospective case series study. BMJ Open. 2020;10:e042398.
Nijman G, Wientjes M, Ramjith J, et al. Risk factors for in-hospital mortality in laboratory-confirmed COVID-19 patients in the Netherlands: a competing risk survival analysis. PLoS ONE. 2021;16:e0249231.
Grasselli G, Greco M, Zanella A, et al. Risk factors associated with mortality among patients with COVID-19 in intensive care units in Lombardy, Italy. JAMA Intern Med. 2020;180:1345–55.
Haas LEM, de Lange DW, van Dijk D, et al. Should we deny ICU admission to the elderly? Ethical considerations in times of COVID-19. Crit Care. 2020. https://doi.org/10.1186/s13054-020-03050-x.
Vallet H, Schwarz GL, Flaatten H, et al. Mortality of older patients admitted to an ICU: a systematic review. Crit Care Med. 2021;49:324–34.
Ma Y, Hou L, Yang X, et al. The association between frailty and severe disease among COVID-19 patients aged over 60 years in China: a prospective cohort study. BMC Med. 2020;18:274.
Hewitt J, Carter B, Vilches-Moraga A, et al. The effect of frailty on survival in patients with COVID-19 (COPE): a multicentre, European, observational cohort study. Lancet Public Health. 2020;5:e444–51.
Eachempati SR, Hydo LJ, Shou J, et al. Outcomes of acute respiratory distress syndrome (ARDS) in elderly patients. J Trauma. 2007;63:344–50.
Milberg JA, Davis DR, Steinberg KP, et al. Improved survival of patients with acute respiratory distress syndrome (ARDS): 1983–1993. JAMA. 1995;273:306–9.
Ferguson ND, Pham T, Gong MN. How severe COVID-19 infection is changing ARDS management. Intensive Care Med. 2020;46:2184–6.
COVID-ICU Group on behalf of the REVA Network and the COVID-ICU Investigators. Clinical characteristics and day-90 outcomes of 4244 critically ill adults with COVID-19: a prospective cohort study. Intensive Care Med. 2021;47:60–73.
Clinical management of severe acute respiratory infection when COVID-19 is suspected. https://www.who.int/publications-detail/clinical-management-of-severe-acute-respiratory-infection-when-novel-coronavirus-(ncov)-infection-is-suspected. Accessed 27 Apr 2020.
Le Gall JR, Lemeshow S, Saulnier F. A new Simplified Acute Physiology Score (SAPS II) based on a European/North American multicenter study. JAMA. 1993;270:2957–63.
Vincent JL, Moreno R, Takala J, et al. The SOFA (Sepsis-related Organ Failure Assessment) score to describe organ dysfunction/failure. On behalf of the Working Group on Sepsis-Related Problems of the European Society of Intensive Care Medicine. Intensive Care Med. 1996;22:707–10.
Juma S, Taabazuing M-M, Montero-Odasso M. Clinical frailty scale in an acute medicine unit: a simple tool that predicts length of stay. Can Geriatr J. 2016;19:34–9.
Grambsch P, Therneau T. Proportional hazards tests and diagnostics based on weighted residuals. Biometrika. 1994;81:515–26.
Austin PC. An introduction to propensity score methods for reducing the effects of confounding in observational studies. Multivar Behav Res. 2011;46:399–424.
Austin PC. Balance diagnostics for comparing the distribution of baseline covariates between treatment groups in propensity-score matched samples. Stat Med. 2009;28:3083–107.
Kao K-C, Hsieh M-J, Lin S-W, et al. Survival predictors in elderly patients with acute respiratory distress syndrome: a prospective observational cohort study. Sci Rep. 2018;8:13459.
Bellani G, Laffey JG, Pham T, et al. Epidemiology, patterns of care, and mortality for patients with acute respiratory distress syndrome in intensive care units in 50 countries. JAMA. 2016;315:788–800.
Flaatten H, De Lange DW, Morandi A, et al. The impact of frailty on ICU and 30-day mortality and the level of care in very elderly patients (≥ 80 years). Intensive Care Med. 2017;43:1820–8.
Guidet B, de Lange DW, Boumendil A, et al. The contribution of frailty, cognition, activity of daily life and comorbidities on outcome in acutely admitted patients over 80 years in European ICUs: the VIP2 study. Intensive Care Med. 2020;46:57–69.
Dres M, Austin PC, Pham T, et al. Acute respiratory distress syndrome cases volume and ICU mortality in medical patients. Crit Care Med. 2018;46:e33–40.
Rockwood K, Song X, MacKnight C, et al. A global clinical measure of fitness and frailty in elderly people. CMAJ. 2005;173:489–95.
Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA. 2020;323:2052–9.
Azoulay É, Beloucif S, Guidet B, et al. Admission decisions to intensive care units in the context of the major COVID-19 outbreak: local guidance from the COVID-19 Paris-region area. Crit Care. 2020;24:293.
Shrime MG, Ferket BS, Scott DJ, et al. Time-limited trials of intensive care for critically ill patients with cancer: how long is long enough? JAMA Oncol. 2016;2:76–83.
Dennis JM, McGovern AP, Vollmer SJ, et al. Improving survival of critical care patients with coronavirus disease 2019 in England: a national cohort study, March to June 2020. Crit Care Med. 2021;49:209–14.
Demoule A, Vieillard Baron A, Darmon M, et al. High-flow nasal cannula in critically III patients with severe COVID-19. Am J Respir Crit Care Med. 2020;202:1039–42.
Barnato AE, Albert SM, Angus DC, et al. Disability among elderly survivors of mechanical ventilation. Am J Respir Crit Care Med. 2011;183:1037–42.
Unroe M, Kahn JM, Carson SS, et al. One-year trajectories of care and resource utilization for recipients of prolonged mechanical ventilation: a cohort study. Ann Intern Med. 2010;153:167–75.
Horby P, Lim WS, Emberson J, et al. Dexamethasone in hospitalized patients with Covid-19. N ENgl J Med. 2021;384:693–704.
Kalil AC, Patterson TF, Mehta AK, et al. Baricitinib plus remdesivir for hospitalized adults with COVID-19. N Engl J Med. 2020;383:1813–26.
Acknowledgements
The authors are particularly grateful to all caregivers, COVID-ICU investigators and patients who have been involved in the study. Participating sites and COVID-ICU investigators: CHU Angers, Angers, France (Alain Mercat, Pierre Asfar, François Beloncle, Julien Demiselle), APHP—Hôpital Bicêtre, Le Kremlin-Bicêtre, France (Tài Pham, Arthur Pavot, Xavier Monnet, Christian Richard), APHP—Hôpital Pitié Salpêtrière, Paris, France (Alexandre Demoule, Martin Dres, Julien Mayaux, Alexandra Beurton), CHU Caen Normandie—Hôpital Côte de Nacre, Caen, France, (Cédric Daubin, Richard Descamps, Aurélie Joret, Damien Du Cheyron), APHP—Hôpital Cochin, Paris, France (Frédéric Pene, Jean-Daniel Chiche, Mathieu Jozwiak, Paul Jaubert), APHP—Hôpital Tenon, Paris (France, Guillaume Voiriot, Muriel Fartoukh, Marion Teulier, Clarisse Blayau), CHRU de Brest—La Cavale Blanche, Brest, France (Erwen L'Her, Cécile Aubron, Laetitia Bodenes, Nicolas Ferriere), Centre Hospitalier de Cholet, Cholet, France (Johann Auchabie, Anthony Le Meur, Sylvain Pignal, Thierry Mazzoni), CHU Dijon Bourgogne, Dijon, France (Jean-Pierre Quenot, Pascal Andreu, Jean-Baptiste Roudau, Marie Labruyère), CHU Lille—Hôpital Roger Salengero, Lille, France (Saad Nseir, Sébastien Preau, Julien Poissy, Daniel Mathieu), Groupe Hospitalier Nord Essonne, Longjumeau, France (Sarah Benhamida, Rémi Paulet, Nicolas Roucaud, Martial Thyrault), APHM—Hopital Nord, Marseille, France (Florence Daviet, Sami Hraiech, Gabriel Parzy, Aude Sylvestre), Hôpital de Melun-Sénart, Melun, France (Sébastien Jochmans, Anne-Laure Bouilland, Mehran Monchi), Élément Militaire de Réanimation du SSA, Mulhouse, France (Marc Danguy des Déserts, Quentin Mathais, Gwendoline Rager, Pierre Pasquier), CHU Nantes—Hôpital Hotel Dieu, Nantes, France (Reignier Jean, Seguin Amélie, Garret Charlotte, Canet Emmanuel), CHU Nice—Hôpital Archet, Nice, France (Jean Dellamonica, Clément Saccheri, Romain Lombardi, Yanis Kouchit), Centre Hospitalier d'Orléans, Orléans, France (Sophie Jacquier, Armelle Mathonnet, Mai-AhnNay, Isabelle Runge), Centre Hospitalier Universitaire de la Guadeloupe, Pointe-à-Pitre, France (Frédéric Martino, Laure Flurin, Amélie Rolle, Michel Carles), Hôpital de la Milétrie, Poitiers, France (Rémi Coudroy, Arnaud W Thille, Jean-Pierre Frat, Maeva Rodriguez), Centre Hospitalier Roanne, Roanne, France (Pascal Beuret, Audrey Tientcheu, Arthur Vincent, Florian Michelin), CHU Rouen—Hôpital Charles Nicolle, Rouen, France (Marie Anne Melone, Maxime Gauzi, Arnaud Guilbert, Geoffrey Kouadri), CHRU Tours—Hôpital Bretonneau, Tours, France (Valérie Gissot, Stéphan Ehrmann, Charlotte Salmon Gandonniere, Djlali Elaroussi), Centre Hospitalier Bretagne Atlantique, Vannes, France (Agathe Delbove, Yannick Fedun, Julien Huntzinger, Eddy Lebas), CHU Liège, Liège, Belgique (Grâce Kisoka, Céline Grégoire, Stella Marchetta, Bernard Lambermont), Hospices Civils de Lyon—Hôpital Edouard Herriot, Lyon, France (Laurent Argaud, Thomas Baudry, Pierre-Jean Bertrand, Auguste Dargent), Centre Hospitalier Du Mans, Le Mans, France (Christophe Guitton, Nicolas Chudeau, Mickaël Landais, Cédric Darreau), Centre Hospitalier de Versailles, Le Chesnay, France (Alexis Ferre, Antoine Gros, Guillaume Lacave, Fabrice Bruneel), Hôpital Foch, Suresnes, France (Mathilde Neuville, JérômeDevaquet, Guillaume Tachon, Richard Gallot), Hôpital Claude Galien, Quincy sous Senart, France (Riad Chelha, Arnaud Galbois, Anne Jallot, Ludivine Chalumeau Lemoine), GHR Mulhouse Sud-Alsace, Mulhouse, France (Khaldoun Kuteifan, Valentin Pointurier, Louise-Marie Jandeaux, Joy Mootien), APHP—Hôpital Antoine Béclère, Clamart, France (Charles Damoisel, Benjamin Sztrymf), APHP—Hôpital Pitié-Salpêtrière, Paris, France (Matthieu Schmidt, Alain Combes, Juliette Chommeloux, Charles Edouard Luyt), Hôpital Intercommunal de Créteil, Créteil, France (Frédérique Schortgen, Leon Rusel, Camille JUNG), Hospices Civils de Lyon—Hôpital Neurologique, Lyon, France (Florent Gobert), APHP—Hôpital Necker, Paris, France (Damien Vimpere, Lionel Lamhaut), Centre Hospitalier Public du Cotentin—Hôpital Pasteur, Cherbourg-en-cotentin, France (Bertrand Sauneuf, Liliane Charrrier, Julien Calus, Isabelle Desmeules), CHU Rennes—Hôpital du Pontchaillou, Rennes, France (Benoît Painvin, Jean-Marc Tadie), CHU Strasbourg—Hôpital Hautepierre, Strasbourg, France (Vincent Castelain, Baptiste Michard, Jean-Etienne Herbrecht, Mathieu Baldacini), APHP—Hôpital Pitié Salpêtrière, Paris, France (Nicolas Weiss, Sophie Demeret, Clémence Marois, Benjamin Rohaut), Centre Hospitalier Territorial Gaston-Bourret, Nouméa, France (Pierre-Henri Moury, Anne-Charlotte Savida, Emmanuel Couadau, Mathieu Série), Centre Hospitalier Compiègne-Noyon, Compiègne, France (Nica Alexandru), Groupe Hospitalier Saint-Joseph, Paris, France (Cédric Bruel, Candice Fontaine, Sonia Garrigou, Juliette Courtiade Mahler), Centre hospitalier mémorial de Saint-Lô, Saint-Lô, France (Maxime Leclerc, Michel Ramakers), Grand Hôpital de l'Est Francilien, Jossigny, France (Pierre Garçon, Nicole Massou, Ly Van Vong, Juliane Sen), Gustave Roussy, Villejuif, France (Nolwenn Lucas, Franck Chemouni, Annabelle Stoclin), Centre Hospitalier Intercommunal Robert Ballanger, Aulnay-sous-Bois, France (Alexandre Avenel, Henri Faure, Angélie Gentilhomme, Sylvie Ricome), Hospices Civiles de Lyon—Hôpital Edouard Herriot, Lyon, France (Paul Abraham, Céline Monard, Julien Textoris, Thomas Rimmele), Centre Hospitalier d'Avignon, Avignon, France (Florent Montini), Groupe Hospitalier Diaconesses—Croix Saint Simon, Paris, France (Gabriel Lejour, Thierry Lazard, Isabelle Etienney, Younes Kerroumi), CHU Clermont-Ferrand—Hôpital Gabriel Montpied, Clermont Ferrand, France (Claire Dupuis, Marine Bereiziat, Elisabeth Coupez, François Thouy), Hôpital d'Instruction des Armées Percy, Clamart, France (Clémet Hoffmann, Nicolas Donat, Violaine Muller, Thibault Martinez), CHU Nancy—Hôpital Brabois, Vandoeuvre-les-Nancy, France (Antoine Kimmoun, Audrey Jacquot, Matthieu Mattei, Bruno Levy), Centre Hospitalier de Vichy, Vichy, France (Ramin Ravan, Loïc Dopeux, Jean-Mathias Liteaudon, Delphine Roux), Hopital Pierre Bérégovoy, Nevers, France (Brice Rey, Radu Anghel, Deborah Schenesse, Vincent Gevrey), Centre Hospitalier de Tarbes, Tarbes, France (Jermy Castanera, Philippe Petua, Benjamin Madeux), Hôpitaux Civils de Colmar—Hôpital Louis pasteur, Colmar, France (Otto Hartman), CHU Charleroi—Hôpital Marie Curie, Bruxelles, Belgique (Michael Piagnerelli, Anne Joosten,Cinderella Noel, Patrick Biston), Centre hospitalier de Verdun Saint Mihiel, Saint Mihiel, France (Thibaut Noel), CH Eure-Seine—Hôpital d'Evreux-Vernon, Evreux, France (Gurvan LE Bouar, Messabi Boukhanza, Elsa Demarest, Marie-France Bajolet), Hôpital René Dubos, Pontoise, France (Nathanaël Charrier, Audrey Quenet, Cécile Zylberfajn, Nicolas Dufour), APHP—Hôpital Lariboisière, Paris, France (Buno Mégarbane, SqébastianVoicu, Nicolas Deye, Isabelle Malissin), Centre Hospitalier de Saint-Brieuc, Saint-Brieuc, France (François Legay, Matthieu Debarre, Nicolas Barbarot, Pierre Fillatre), Polyclinique Bordeaux Nord Aquitaine, Bordeaux, France (Bertrand Delord, Thomas Laterrade, Tahar Saghi, Wilfried Pujol), HIA Sainte Anne, Toulon, France (Pierre Julien Cungi, Pierre Esnault, Mickael Cardinale), Grand Hôpital de l'Est Francilien, Meaux, France (Vivien Hong Tuan Ha, Grégory Fleury, Marie-Ange Brou, Daniel Zafimahazo), HIA Robert Picqué, Villenave d'Ornon, France (David Tran-Van, Patrick Avargues, Lisa Carenco), Centre Hospitalier Fontainebleau, Fontainebleau, France (Nicolas Robin, Alexandre Ouali, Lucie Houdou), Hôpital Universitaire de Genève, Genève, Suisse (Christophe Le Terrier, Noémie Suh, Steve Primmaz, JéromePugin), APHP—Hôpital Beaujon, Clichy, France (Emmanuel Weiss, Tobias Gauss, Jean-Denis Moyer, Catherine PaugamBurtz), Groupe Hospitalier Bretage Sud, Lorient, France (Béatrice La Combe, Rolland Smonig, Jade Violleau, Pauline Cailliez), Centre Hospitalier Intercommunal Toulon, La Seyne sur Mer, France (Jonathan Chelly), Centre Hospitalier de Dieppe, Dieppe, France (Antoine Marchalot, Cécile Saladin, Christelle Bigot), CHU de Martinique, Fort-de-France, France (Pierre-Marie Fayolle, Jules Fatséas, Amr Ibrahim, Dabor Resiere), Hôpital Fondation Adolphe de Rothchild, Paris, France (Rabih Hage, Clémentine Cholet, Marie Cantier, Pierre Trouiler), APHP—Bichat Claude Bernard, Paris, France (Philippe Montravers, Brice Lortat-Jacob, Sebastien Tanaka, AlexyTran Dinh), APHP—Hôpital Universitaire Paris Sud, Bicêtre, France (Jacques Duranteau, Anatole Harrois, Guillaume Dubreuil, Marie Werner), APHP—Hôpital Européen Georges Pompidou, Paris, France (Anne Godier, Sophie Hamada, Diane Zlotnik, Hélène Nougue), APHP, GHU Henri Mondor, Créteil, France (Armand Mekontso-Dessap, Guillaume Carteaux, Keyvan Razazi, Nicolas De Prost), APHP—Hôpitaux Universitaires Henri Mondor, Créteil, France (Nicolas Mongardon, Olivier Langeron, Eric Levesque, Arié Attias), APHP—Hôpital Lariboisière, Paris, France (Charles de Roquetaillade, Benjamin G. Chousterman, Alexandre Mebazaa, Etienne Gayat), APHP—Hôpital Saint-Antoine, Paris, France (Marc Garnier, Emmanuel Pardo, LeaSatre-Buisson, Christophe Gutton), APHP Hôpital Saint-Louis, Paris, France (Elise Yvin, Clémence Marcault, Elie Azoulay, Michael Darmon), APHP—Hôpital Saint-Antoine, Paris, France (Hafid Ait Oufella, Geoffroy Hariri, Tomas Urbina, Sandie Mazerand), APHP—Hôpital Raymond Pointcarré, Garches, France (Nicholas Heming, Francesca Santi, Pierre Moine, Djillali Annane), APHP—Hôpital Pitié Salpêtrière, Paris, France (Adrien Bouglé, Edris Omar, Aymeric Lancelot, Emmanuelle Begot), Centre Hospitalier Victor Dupouy, Argenteuil, France (Gaétan Plantefeve, Damien Contou, Hervé Mentec, Olivier Pajot), CHU Toulouse—Hôpital Rangueil, Toulouse, France (Stanislas Faguer, Olivier Cointault, Laurence Lavayssiere, Marie-Béatrice Nogier), Centre Hospitalier de Poissy, Poissy, France (Matthieu Jamme, Claire Pichereau, Jan Hayon, Hervé Outin), APHP—Hôpital Saint-Louis, Paris, France (François Dépret, Maxime Coutrot, Maité Chaussard, Lucie Guillemet), Clinique du MontLégia, CHC Groupe-Santé, Liège, Belgique (Pierre Goffin, Romain Thouny, Julien Guntz, Laurent Jadot), CHU Saint-Denis, La Réunion, France (Romain Persichini), Centre Hospitalier de Tourcoing, Tourcoing, France (Vanessa Jean-Michel, Hugues Georges, Thomas Caulier), Centre Hospitalier Henri Mondor d'Aurillac, Aurillac, France (Gaël Pradel, Marie-Hélène Hausermann, ThiMy Hue Nguyen-Valat, Michel Boudinaud), Centre Hospitalier Saint Joseph Saint Luc, Lyon, France (Emmanuel Vivier, SylvèneRosseli, Gaël Bourdin, Christian Pommier) Centre Hospitalier de Polynésie Française, Polynésie, France (Marc Vinclair, Simon Poignant, Sandrine Mons), Ramsay Générale de Santé, Hôpital Privé Jacques Cartier, Massy, France (Wulfran Bougouin), Centre Hospitalier Alpes Léman, Contamine sur Arve, France (Franklin Bruna, Quentin Maestraggi, Christian Roth), Hospices Civils de Lyon—Hôpital de la Croix Rousse, Lyon, France (Laurent Bitker, François Dhelft, Justine Bonnet-Chateau, Mathilde Filippelli), Centre Cardiologique du Nord, Saint-Denis, France (Tristan Morichau-Beauchant, Stéphane Thierry, Charlotte Le Roy, Mélanie Saint Jouan), GHU—Hôpital Saint-Anne, Paris, France (Bruno Goncalves, Aurélien Mazeraud, Matthieu Daniel, Tarek Sharshar) CHR Metz—Hôpital Mercy, Metz, France (Cyril Cadoz, RostaneGaci, Sébastien Gette, Guillaune Louis), APHP—Hôpital Paul Brousse, Villejuif, France (Sophe-Caroline Sacleux, Marie-Amélie Ordan), CHRU Nancy—Hôpital Central, Nancy, France (Aurélie Cravoisy, Marie Conrad, Guilhem Courte, Sébastien Gibot), Centre Hospitalier d’Ajaccio, Ajaccio, France (Younès Benzidi, Claudia Casella, Laurent Serpin, Jean-Lou Setti), Centre Hospitalier de Bourges, Bourges, France (Marie-Catherine Besse, Anna Bourreau), Centre hospitalier de la Côte Basque, Bayonne, France (Jérôme Pillot, Caroline Rivera, Camille Vinclair, Marie-Aline Robaux), Hospices Civils de Lyon—Hôpital de la Croix Rousse, Lyon, France (Chloé Achino, Marie-Charlotte Delignette, Tessa Mazard, Frédéric Aubrun), CH Saint-Malo, Saint-Malo, France (Bruno Bouchet, Aurélien Frérou, Laura Muller, Charlotte Quentin), Centre Hospitalier de Mulhouse, Mulhouse, France (Samuel Degoul), Centre Hospitalier de Briançon, Briançon, France (Xavier Stihle, Claude Sumian, Nicoletta Bergero, Bernard Lanaspre), CHU Nice, Hôpital Pasteur 2, Nice, France (Hervé Quintard, Eve Marie Maiziere), Centre Hospitalier des Pays de Morlaix, Morlaix, France (Pierre-Yves Egreteau, Guillaume Leloup, Florin Berteau, Marjolaine Cottrel), Centre Hospitalier Valence, Valence, France (Marie Bouteloup, Matthieu Jeannot, Quentin Blanc, Julien Saison), Centre Hospitalier Niort, Niort, France (Isabelle Geneau, Romaric Grenot, Abdel Ouchike, Pascal Hazera), APHP—Hôpital Pitié Salpêtrière, Paris, France (Anne-Lyse Masse, Suela Demiri, Corinne Vezinet, Elodie Baron, Deborah Benchetrit, Antoine Monsel), Clinique du Val d'Or, Saint Cloud, France (Grégoire Trebbia, Emmanuelle Schaack, Raphaël Lepecq, Mathieu Bobet), Centre Hospitalier de Béthune, Béthune, France (Christophe Vinsonneau, Thibault Dekeyser, Quentin Delforge, Imen Rahmani), Groupe Hospitalier Intercommunal de la Haute-Saône, Vesoul, France (Bérengère Vivet, Jonathan Paillot, Lucie Hierle, Claire Chaignat, Sarah Valette), Clinique Saint-Martin, Caen, France (BenoïtHer, Jennifier Brunet), Ramsay Générale de Santé, Clinique Convert, Bourg en Bresse, France (Mathieu Page, Fabienne Boiste, Anthony Collin), Hôpital Victor Jousselin, Dreux, France(Florent Bavozet, Aude Garin,Mohamed Dlala, KaisMhamdi), Centre Hospitalier de Troye, Troye, France, (Bassem Beilouny, Alexandra Lavalard, Severine Perez), CHU de ROUEN-Hôpital Charles Nicolle, Rouen, France (Benoit Veber, Pierre-Gildas Guitard, Philippe Gouin, Anna Lamacz), Centre Hospitalier Agen-Nérac, Agen, France (Fabienne Plouvier, Bertrand P delaborde, AïssaKherchache, Amina Chaalal), APHP—Hôpital Louis Mourier, Colombes, France (Jean-Damien Ricard, Marc Amouretti, Santiago Freita-Ramos, Damien Roux), APHP—Hôpital Pitié-Salpêtrière, Paris, France (Jean-Michel Constantin, Mona Assefi, Marine Lecore, Agathe Selves), Institut Mutualiste Montsouris, Paris, France (Florian Prevost, Christian Lamer, Ruiying Shi, Lyes Knani), CHU Besançon—Hôpital Jean Minjoz, Besançon, France, (Sébastien PiliFloury, Lucie Vettoretti), APHP—Hôpital Universitaire Robert-Debré, Paris, France (Michael Levy, Lucile Marsac, Stéphane Dauger, Sophie Guilmin-Crépon), CHU Besançon—Hôpital Jean Minjoz, Besançon, France, (Hadrien Winiszewski, Gael Piton, Thibaud Soumagne, Gilles Capellier); Médipôle Lyon-Villeurbanne, Vileurbanne, France, (Jean-Baptiste Putegnat, Frédérique Bayle, Maya Perrou, Ghyslaine Thao), APHP—Ambroise Paré, Boulogne-Billancourt, France (Guillaume Géri, Cyril Charron, Xavier Repessé, Antoine Vieillard-Baron), CHU Amiens Picardie, Amiens, France (Mathieu Guilbart, Pierre-Alexandre Roger, Sébastien Hinard, Pierre-Yves Macq), Hôpital Nord-Ouest, Villefranche-sur-Saône, France (Kevin Chaulier, Sylvie Goutte), CH de Châlons en Champagne, Châlons en Champagne, France (Patrick Chillet, Anaïs Pitta, Barbara Darjent, Amandine Bruneau), CHU Angers, Angers, France (Sigismond Lasocki, Maxime Leger, Soizic Gergaud, Pierre Lemarie), CHU Grenoble Alpes, Grenoble, France (Nicolas Terzi, Carole Schwebel, Anaïs Dartevel, Louis-Marie Galerneau), APHP—Hôpital Européen Georges Pompidou, Paris, France (Jean-Luc Diehl, Caroline Hauw-Berlemont, Nicolas Péron, Emmanuel Guérot), Hôpital Privé d'Antony, Antony, France (AbolfazlMohebbiAmoli, Michel Benhamou, Jean-Pierre Deyme, Olivier Andremont), Institut Arnault Tzanck,Saint Laurent du Var, France (Diane Lena, Julien Cady, Arnaud Causeret, Arnaud De La Chapelle); Centre Hospitalier d’ Angoulême, Angoulême, France (Christophe Cracco, Stéphane Rouleau, David Schnell); Centre Hospitalier de Cahors, Cahors, France (Camille Foucault), Centre hospitalier de Carcassonne, Carcassonne, France (Cécile Lory); CHU Nice—Hôpital L’Archet 2, Nice, France (Thibault Chapelle, Vincent Bruckert, Julie Garcia, Abdlazize Sahraoui); Hôpital Privé du Vert Galant, Tremblay-en-France, France (Nathalie Abbosh, Caroline Bornstain, Pierre Pernet); Centre Hospitalier de Rambouillet, Rambouillet, France (Florent Poirson, Ahmed Pasem, Philippe Karoubi); Hopitaux du Léman, Thonon les Bains, France (Virginie Poupinel, Caroline Gauthier, François Bouniol, Philippe Feuchere), Centre Hospitalier Victor Jousselin, Dreux, France (Florent Bavozet, Anne Heron), Hôpital Sainte Camille, Brie sur Marne, France (Serge Carreira, Malo Emery, Anne Sophie Le Floch, Luana Giovannangeli), Hôpital d’instruction des armées Clermont-Tonnerre, Brest, France (Nicolas Herzog, Christophe Giacardi, Thibaut Baudic, Chloé Thill), APHP—Hôpital Pitié Salpêtrière, Paris, France (Said Lebbah, Jessica Palmyre, Florence Tubach, David Hajage); APHP—Hôpital Avicenne, Bobigny, France (Nicolas Bonnet, Nathan Ebstein, Stéphane Gaudry, Yves Cohen); Groupement Hospitalier la Rochelle Ré Amis, La Rochelle, France (Julie Noublanche, Olivier Lesieur); Centre Hospitalier Intercommunal de Mont de Marsan et du Pays des Sources, Mont de Marsan, France (Arnaud Sément, Isabel Roca-Cerezo, Michel Pascal, Nesrine Sma); Centre Hospitalier Départemental de Vendée, La-Roche-Sur-Yon, France (Gwenhaël Colin, Jean-Claude Lacherade, Gauthier Bionz, Natacha Maquigneau); Pôle Anesthésie-Réanimation, CHU Grenoble (Pierre Bouzat, Michel Durand, Marie-Christine Hérault, Jean-Francois Payen).
Funding
This study was funded by the Foundation AP-HP and the Direction de la Recherche Clinique et du Development and the French Ministry of Health. The REVA network received a 75,000 € research grant form Air Liquide Healthcare. The funder had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Author information
Authors and Affiliations
Consortia
Contributions
MD and MS designed the study. MD, MS, AD, AM, AC, SL, AK, TP, GB and DH coordinated the study. MD, AD, CS, EM and TS analyzed the data. MD, MS, DH wrote the manuscript. All authors had full access to all study data, contributed to drafting the manuscript or critical revision of it for important intellectual content, approved the final version of the manuscript, and take responsibility for the integrity of the data and the accuracy of the data analysis. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Human research ethics committee approval for the study was the ethical committee of the French Intensive Care Society (CE-SRLF 20-23) following our local regulations.
Consent for publication
All patients or close relatives were informed that their data were included in the COVID-ICU cohort.
Competing interests
Dr Schmidt reported personal fees from Getinge, Drager, and Xenios, outside the submitted work. Dr Demoule reports personal fees from Medtronic, grants, personal fees and non-financial support from Philips, personal fees from Baxter, personal fees from Hamilton, personal fees and non-financial support from Fisher & Paykel, grants from French Ministry of Health, personal fees from Getinge, grants and personal fees from Respinor, grants and non-financial support from Lungpacer, outside the submitted work. Dr Dres reported personal fees from Lungpacer. No other disclosures were reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Detailed description of the data collection and statistal analysis and complementary tables and figures
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Dres, M., Hajage, D., Lebbah, S. et al. Characteristics, management, and prognosis of elderly patients with COVID-19 admitted in the ICU during the first wave: insights from the COVID-ICU study. Ann. Intensive Care 11, 77 (2021). https://doi.org/10.1186/s13613-021-00861-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13613-021-00861-1