Abstract
Environmental transmission of Chlamydia abortus as a result of enzootic disease or disease outbreaks and the threats posed by this pathogen has been previously reported, however a state-of-the-science review of these reports and the identification of future research priorities in this area is still lacking. This study provides an overview of the current knowledge of host–pathogen–environment interactions, addressing public health risks and identifying critical questions and research gaps. We performed a systematic PubMed and Web of Science search for publications related to Chlamydia abortus in the past four decades, and we reviewed and combined the evidence critically discussing and commenting the results. A total of 182 studies, 5 chapters of specific books and the “OIE terrestrial manual” were included in this review. There were substantial variations between the studies in topic addressed and experimental design. Overall, the literature largely supports the crucial role played by environmental exposure on the acquisition of zoonotic disease caused by Chlamydia abortus. We also identify the paucity of information related to interspecies transmission and pathogen adaptation in relation to environmental dissemination and zoonotic risk. This analysis further highlights the need for additional research given that environmental transmission represents a serious risk not only to susceptible patients (pregnant women and immunocompromised individuals), but also for other species including wildlife.
Similar content being viewed by others
1 Introduction
Chlamydia abortus (C. abortus) is a non-motile obligate intracellular Gram-negative pathogenic bacterium, belonging to the Chlamydiales family. C. abortus infects mainly ruminants, especially sheep and goats, and less frequently cattle, pigs and horses; however, it can also affect humans, being of particular concern in pregnant women [1, 2]. C. abortus is known as the causative agent of enzootic abortion of ewes (EAE) or ovine enzootic abortion (OEA) which represents one of the most common causes of ovine and caprine infectious abortion worldwide, along with other infectious agents such as Campylobacter sp, Toxoplasma sp, Listeria sp, Salmonella sp, Border disease virus and Cache Valley virus [3, 4]. Abortion occurs in the later stages of pregnancy, as C. abortus is able to progressively colonize the placenta, causing damage and affecting the fetus(es) to varies degrees [5]. The infection can result in foetal loss (abortion), the birth of stillborn or weak lambs or, in some cases of unaffected animals; presence of a weak lamb with a healthy tween is also not uncommon [6]. Breeders can incur great economic losses if numerous cases occur in a farm (abortion storm), usually when the infection first affects a naïve flock [7]. Another important aspect is the spread of this enzootic infection to humans, which can develop as severe disease, especially in pregnant women [2], generally affecting female farmers, abattoir workers and veterinarians. However, environmental contamination with the bacteria released by abortion products or infected animals may also play a crucial role in disease spread, interspecies cross-over and adaptation [8]. Indeed, abortion products, in particular vaginal fluids, placentas, dead/aborted lambs, fleeces and still born/infected lambs are all characterized by a high bacterial load and represent a significant risk, both for naïve animals and for humans [9]. Different types of flock management are also involved in the extent of environmental contamination and the spread of the pathogen: in intensively managed flocks, where the animals are kept in smaller enclosures, there is a higher incidence of C. abortus, as the environmental contamination is concentrated in small spaces; conversely in extensively managed flocks, where animals are kept within larger areas, a lower incidence of the pathogen is observed, linked to the fact that animals are less likely to come into contact with a contaminated area [3]. In addition, C. abortus can survive in the environment even in unfavourable conditions from a few days to a few months, thanks to the presence of a spore-like cell wall, which gives it considerable resilience [7]. This resistance seems to be directly connected to the greater possibility for the bacterium to come into contact and infect many animal species, farmed or wild ones, and consequently to spread more easily to humans [2]. Specific aspects of this will be discussed later.
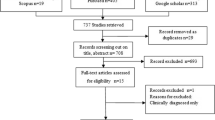
To better understand the role of environmental contamination in the spread of the infection we performed a systematic search of the literature available in PubMed and Web of Science databases to retrieve all available studies on Chlamydia abortus, including the ones focused on the animal-to-human transmission, using the following search terms: “Chlamydia abortus”, “Chlamydophila abortus [title]”, “chlamydial abortion [title]”, “Chlamydia psittaci (previous nomenclature) [title] abortion [title]”, “chlamydial developmental cycle [title]”, “Chlamydia psittaci sheep [title]”, “Enzootic abortion of ewes [title]”, “Chlamydia psittaci [title] interferon-gamma”, “Chlamydia cell biology [title]”, “the ovine placenta [title]”, “OEA” [title], “EAE” [title], “Ovine enzootic abortion” and “Enzootic abortion of ewes”. Our review was open to inclusion of studies written in English published in peer-reviewed journals and government reports, selected according to the relevance for the topics covered in the review. Information on genetics and genomics, host–pathogen interactions, infection and pathogenesis of the disease, both for animals and humans, host immune response and the main available vaccines, methods for diagnosis, epidemiology of the disease and environmental aspects are summarized and critically discussed. Our inclusion criteria did not consider any limit in respect of geographical location. All the retrieved studies relevant to the topics were considered suitable for inclusion in the literature review and were cited. Journal articles were not omitted even if only presenting limited data sets. With the keywords previously named the search on PubMed delivered a total of 562 results. Having removed duplicate results and those not available as full text, 180 articles were selected. In addition to the published articles, the books “Intracellular pathogens 1: Chlamydiales” and “Disease of sheep” and the “OIE Terrestrial Manual” were consulted [1, 3, 10,11,12,13]. Studies included were variable in terms of topic addressed, experimental design, results and conclusions, and we also incorporated work showing contradictory findings. We extracted information from each study and each of the co-authors reviewed the studies independently before discussing and critically evaluating specific points.
2 Genetics and genomics
The zoonotic potential and the possibility of environmental transmission of Chlamydia abortus are strictly correlated to the genome type and the genetic diversity of the microorganism. In particular, rearrangements in a variable region of the genome indicated as the “Plasticity Zone” (PZ) and in the tryptophan biosynthetic operon, seem to have evolved to enable better adaptation to the mammalian host and persistence [14]. The genome of C. abortus consists of a circular 1.14 million bp chromosome with an overall G + C content of 39.97%. Sequence analysis identified 961 coding sequences (CDS), 746 of which have been functionally assigned, using previously compiled databases, motif matches and experimental evidence. For those with no functional assignments, 110 sequences have been recognized as similar to proteins already found in other members of the Chlamydiaceae. Moreover, 29 pseudogenes coding for membrane proteins, Pmp (Polymorphic Membrane Proteins)-family proteins and some hypothetical preserved proteins have also been discovered among the 961 CDS. Some functional CDS in the genome of C. abortus, appear as pseudogenes in other species within the Chlamydiaceae [14]. Complete genomic sequences of several species of Chlamydia have been available for some time, such as C. trachomatis (2013, GCA_000590575.1), C. suis (2018, GCA_900149625.2), C. psittaci (2014, GCA_000687395.1) and C. abortus (2014, GCA_000952935.1). Comparative analyses between members of the Chlamydiaceae family have been published by different groups and highlight the limited correlation between genome conservation and species or tissues tropism. A comparison of the total genome of C. abortus with C. caviae and C. pneumoniae showed a high level of conservation among the three genomes, especially in the region defined as “core”, which was preserved in all three species [14]. This however contrasts with the significant differences shown by these species regarding host range, tissue tropism and disease outcome. Despite the high conservation of the core, several variations were detected, particularly in the “Plasticity Zone” or replication termination region terminus, where the two major clusters of polymorphic genes that encode for TMH (Transmembrane Head)/Inc (Inclusion Membrane Proteins) and Pmp proteins and biotin biosynthetic operon are located [14]. The PZ of C. abortus, being 12 kb and encoding 11 genes, similarly to C. pneumoniae, is very small and with a lower number of CDS compared to C. caviae, which encodes for 22 genes. The small size of the PZ of C. abortus is mainly the result of loss of the tryptophan biosynthetic operon (trp) [14]. Therefore, C. abortus needs to acquire the host’s tryptophan to grow and multiply [15], while this is not required for survival outside the host and for transmission [14]. In the same study, it was suggested that the loss of the trp gene occurred following the niche adaptation of the bacterium [14]. Further adaptation of C. abortus can also be seen when comparing the region encoding toxin genes within the PZ of C. muridarium, C. caviae and C. trachomatis with that of C. abortus. These genes have been lost in C. abortus, whereas biotin biosynthetic genes, absent in other species, such as C. caviae, have instead been identified in its genome [14].
All these differences may reflect the diversity in niche adaptation of the different chlamydial species, thus explaining the variation in host, tissue tropism and pathogenicity that characterizes each species. Once new chlamydial genomes became available, additional comparative analyses might reveal important differences linked to the genomic evolution of these species [8].
3 Host–pathogen interaction
The specific interactions between C. abortus and its respective hosts have been investigated for some but not all its host species; however, some of the general mechanisms can be extrapolated from work carried out on other Chlamydia species [16].
The interaction between Chlamydia spp. and the host (Figure 1) starts with the infectious form of the pathogen, namely the elementary body (EB) [16] coming in contact with the cell surface, particularly the mucosal epithelial cells. This is followed by cellular adhesion and internalization, and the invasion of the host cell process which relies both on host and bacterial factors [10, 11]. The interaction between bacterial adhesins and Pmp proteins (polymorphic membrane proteins) with the host receptor molecules (some yet to be identified) are species-specific, and responsible for host and tissue tropism [11, 17].
Once internalised, Chlamydia spp. promote the creation of a vacuole known as the inclusion, through actin remodelling [10, 16, 17]. Cell entry and persistence are regulated by a limited number of stress response genes, among which are the genes encoding a chlamydial homologue of GTPase, which is however truncated at the C-terminal domain, therefore unclear if capable to function as true GTPase, but involved in other functions such as cell division, stress response and ribosome maturation [18]. This is followed by the injection of pre-packaged effectors throughout a Type 3 Secretion System (T3SS), able to induce cytoskeletal rearrangements, to promote invasion and to activate host signalling [16].
The EB, now enclosed in a newly formed inclusion, starts a primary differentiation process to become a more conventional bacterial form, the reticulate body (RB), which is also the metabolically active form, which communicates with the host cell through the inclusion membrane, in order to scavenge all the nutrients necessary to grow and multiply [12, 16]. Of central importance, is the capability of Chlamydia spp. to promote its own fusion with specific cellular compartments, namely the ones rich in nutrients (i.e., exocytic vesicles), while avoiding the fusion with damaging compartments (i.e., lysosomes). The nutrients needed by Chlamydia are mainly eukaryotic lipids (i.e., sphingomyelin and cholesterol), necessary for replication, homotypic fusion, growth, reactivation from persistence and for the secondary differentiation from RBs to EBs. Other nutrients, such as amino acids, sugars, nucleotides and fatty acids are likely acquired through the participation of bacterial transporters, porins and translocases [19].
Through the acquisition of nutrients, the bacteria rapidly multiply by binary fission, until the inclusion is completed and enlarged. At this point, following unknown signals, the RB starts a secondary differentiation into EB: in this phase late-cycle genes are expressed, and the newly differentiated EB exits the cell by lysis or by extrusion [16, 17].
RBs can also enter a state of quiescence (persistent state) if exposed to critical environmental conditions, for example the depletion of essential growth substances, or the presence of antibiotics. C. abortus, lacking the tryptophan biosynthetic operon (trp), enters into a persistent state if in presence of IFN-γ: this cytokine induces the expression of indoleamine-2,3-dioxygenase (IDO), which in turns degrades the host tryptophan, necessary for bacterial growth. Although C. abortus lacks the tryptophan biosynthetic pathway, it can still grow and multiply into the placenta probably through the rescue of tryptophan from maternal-to-foetal nutrients [14]. IDO is known to have multiple functions related to protective immunity (IFN-γ linked), tolerance (by suppression of T cells) and physiology, therefore the animal physiological, nutritional or immune status could influence induction of persistence [20, 21].
4 Infection and pathogenesis
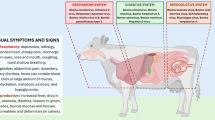
In livestock, infection with C. abortus occurs mainly via oronasal transmission, after ingestion of the placenta or contaminated bedding or via aerosol inhalation of infectious EBs released in the environment by the infected ewes [15, 19, 22, 23]. Indeed, the disease spreads mostly through environmental contamination from abortion products, in particular placentas and coats of dead/aborted lambs which contain a high bacterial load, and vaginal fluids discharge, which can last up to 10 days post-abortion [9]. The EBs released into the environment are characterized by a great resistance to unfavourable conditions, remaining infectious for a few days after pasture contamination during the spring season, when temperatures are mild, and between few weeks and few months at lower temperatures, when temperatures drop below freezing [9]. This prolonged persistence in the environment poses a serious risk both to farmed and wild animals, which circulate in the contaminated areas, and to people who come into contact with contaminated fields. Once the EBs enter the organism, they are thought to colonise the tonsils and/or the nasopharyngeal lymphatic tissues, and from there disseminate to other organs through blood and lymph [19, 23, 24].
The next stage in the pathogenesis varies according to the physiological status of the animal: if a pregnant ewe is infected up to 5–6 weeks before lambing, the most frequent outcome is a sub-clinical infection manifesting only as clinical disease when abortion (last 2–3 weeks of gestation) or dead/weak lambs appear [3]. If the infection occurs when the ewe is not pregnant or nor in the last 5–6 weeks of gestation [3], no clinical disease or abortion ensues, however a latent form of infection is established (possibly within the lymphoid tissue), and infected ewe will appear healthy until the subsequent pregnancy when abortion can occur [23, 25,26,27].
The establishment of latency is thought to be related to unfavourable conditions encountered by the bacterium when initially infecting the host. One of the possible causes of latency, as highlighted during in vitro studies, is the presence of IFN-γ, a cytokine produced by the host in response to the infection. IFN-γ is expressed in order to aid the development of a solid immune response against the pathogen, however at the same time the presence of this cytokine causes the instauration of a latent infection, controlled by a continuous low-level release of IFN-γ, in response to antigen pulsing (LPS of C. abortus). Since in vivo studies must take in consideration the complex biology of the animal and therefore are more complex to perform, additional knowledge is still required to clarify the persistence mechanism [23, 25]. C. abortus then remains in a latent status until the final stages of the sheep pregnancy. At this stage, the bacterium reactivates from latency [25, 28], probably due to pregnancy-related hormonal changes which alter the balance of the immune response: the presence of IFN-γ is harmful for pregnancy, reducing the tolerance to the semi-allogeneic foetus, therefore the immune response shifts from a Th1-type to a Th2-type response. Th2-type cytokines, primarily IL-4 and IL-10, antagonize and downregulate Th1-type cytokines, reducing production of IFN-γ. This reduction in the control mechanism could allow C. abortus to multiply and colonize the placenta, causing abortion [25, 29]. In pregnant women however induction of latency is not common, and foetal colonisation is established soon after infection with stillbirth or abortion generally occurring 3 to 8 days after the symptoms start [9]. This is probably related to the different type of placentation, with the sheep synepitheliochorial placenta offering a more robust barrier to the establishment of the infection.
C. abortus is able to multiply in several organs, including lungs and liver, however here the infection is controlled by the host [30]. On the contrary, the host fails to control and eliminate the infection in its primary target organ, the placenta [27], particularly in late pregnancy [30]. In sheep, it is only at approximately 60 days of gestation, when maternal haematomata appear in the placentome hilus, that C. abortus circulating in the bloodstream or being latent in a yet undefined site is able to begin the actual infection, coming into direct contact with the chorionic epithelium [31, 32]. Work from Álvarez et al. [33] suggests that the bacterium is likely to remain latent on the maternal side of the placenta until the final stages of gestation due to high levels of progesterone, then reactivates in concomitance to the drop of progesterone that occurs at the end of pregnancy, allowing the invasion of trophoblasts and consequently the development of the disease. Although the damages are limited to the hilar zone of some placentomes, the viability and functionality of the surrounding areas are also affected [31]. As well as a placentitis, characterized by chorioallantoic arteritis and thrombosis [34] damage is also found in the foetus, with focal hepatic necrosis and, to a lower extent, small foci of necrosis in lung, spleen, brain and lymph nodes [27]. The underlying cause of abortion is the destruction of the chorionic epithelium and the associated placental damage [9], causing a reduction of the efficiency of the foetal-maternal exchanges [31]. Moreover, the destruction of the chorionic epithelium of the placenta causes an impairment of the hormonal balancing, with a decrease in progesterone levels in the peripheral plasma, with concomitant increase of 17β oestradiol and prostaglandin E2 in the amniotic and allantoid fluids, thus causing premature labour [35,36,37]. Finally, presence of inflammatory cytokines such as TNF-α and IFN-γ (derived from mononuclear cells in infected arteries and arterioles and in the chorionic epithelium of the infected placentas and from resident monocytes and macrophages, respectively) as well as presence of a mixed inflammatory cell infiltrate with vasculitis and thrombosis in the mesenchyme of the intercotyledonary membranes is also thought to contribute to abortion [5].
After abortion, the contact between the ewe and the highly infected placenta induces a massive antigenic stimulation, followed by instauration of solid immunity, preventing reoccurrence of abortion [25, 38]. Indeed, protective immunity only develops after labour or abortion (or after vaccination) and correlates with seroconversion to specific chlamydial antigens contained in the infected placenta [23].
5 Zoonotic infection
C. abortus infections in humans are infrequent: in absence of global data, the UK generally reports 1 or 2 cases each per year in pregnant women. The lack of reported cases may be partially explained with the low specificity of the serological tests used to differentiate C. abortus from other Chlamydia species. Although not frequent, the infection can carry very serious consequences, especially in pregnant women and immunocompromised individuals. The route of infection and the infectious dose for humans are still unclear, but infection is thought to be acquired through contact with infected sheep or goats or secondary contaminated environments and the oronasal mucosa, rather than from incorrect handling of placentas or contact with post-partum secretions by people who work closely with livestock, despite them being generally well aware of the risks [39]. Therefore, the people most at risk of being infected are those who work closely with infected animals, especially during lambing (farmers) and those who work with materials and products derived from infected animals (veterinary surgeons, laboratory technicians, abattoir workers, meet processing plant workers and butchers). Moreover, people who may come into contact with fomites, handling contaminated clothing and boots (hence also the families of the above categories) can also be considered at risk. Finally, those who work with animals recently vaccinated with live attenuated vaccines or who have suffered a vaccine inoculation incident, due to self-injection during vaccine administration are also at increased susceptibility, since the temperature-sensitive attenuated vaccinal strain has shown to be causing disease in some vaccinated animals [40, 41]. C. abortus in pregnant women colonizes and replicates in the trophoblast epithelium, causing pelvic inflammatory disease and triggering placental dysfunction and foetal death [42]. The disease presents with a worsening flu-like febrile episode, with fever up to 41 °C [39], associated to thrombocytopenia, coagulopathy, pneumonia and often liver damage [43]. Often the loss of foetus follows closely the initial febrile episode and seriously compromises the health of the mother: septicemia, shock and multi-organ failure can develop, often requiring hospitalisation and intensive care, including mechanical ventilation and catecholamine administration [44]. In non-pregnant women, only one conclusive case has been reported by Walder et al. in 2003 in a 39-year-old woman suffering from chronic abdominal pain, increased vaginal discharge and abnormal menstruation since adolescence. Patient history revealed that at an early age she had been in contact with sheep and contracted C. abortus infection as confirmed by C. abortus specific PCR and presence of anti-chlamydia antibodies [42]. Borel et al. [45] also investigated a number of patients undergoing intestinal biopsy and found C. abortus via DNA microarray analysis in the colon of an 81-year-old female patient; results however were not confirmed by Immunohistochemistry which makes this an intriguing but still unexplained finding. Ortega and collaborators, on the contrary, reported a case of C. abortus infection in a 47-year-old male working as a veterinary researcher in a laboratory where studies of intranasal infection of C. abortus in sheep were carried out. The patient presented with flu-like symptoms for 7 days and atypical pneumonia, but tested negative for common respiratory pathogens. Serological tests confirmed presence of antibodies specific for C. abortus which was also isolated in cell cultures and confirmed by PCR. Sequence analysis confirmed that the strain (C. abortus AB7) causing pneumonia was the same strain used in the laboratory. This is the first reported case of human respiratory tract infection by C. abortus, and highlights the importance for veterinarians, researchers working in the field and farmers of being vigilant to the possible inhalation of aerosols containing C. abortus [46].
6 Host immune response and vaccines
Numerous studies have been carried out to elucidate the components involved in the ruminant host immune response, in most cases using murine models, because of the expected similarities in the development of the infection between sheep and mice [47]. Murine models enable the investigation of endometrial tissues (the main target in C. abortus infection) since cells that are functionally and morphologically analogue to those present in the endometrial tissues of sheep are also present in mice. In addition, when a pregnant mouse is infected with C. abortus, the infection progression and the immune response closely follow the ones observed in the natural host, allowing infection to be eliminated from all organs except the placenta [48]. Consequently, the infection in mice results in a late-term abortion, similar to what happens in infected sheep [7, 47].
Innate immunity is the first line of defence established when a primary infection with C. abortus occurs; in addition to controlling the infection, innate immunity is also able to initiate and shape a specific immune response thanks to the secretion of cytokines [48]. Innate immune cells, such as Polymorphonuclear Neutrophils (PMN) and Natural Killer cells (NK) also play a pivotal role [49, 50] as demonstrated by the dramatic influence on the recall of macrophages and T cells (especially CD4+ve and CD8+ve) and an increase in mortality following PMN depletion in mouse [49]. Neutrophils-induced recruitment of different cells populations including NK cells, which in turns are able to control the bacterial multiplication, is fundamental in the early control of the infection. Neutrophil depletion is also accompanied by reduction in IFN-γ levels, probably attributable to reduction in NK cell numbers, which correlated with the uncontrolled multiplication of C. abortus [50]. Other cellular populations, specifically CD8+ve lymphocytes, are also key components in limiting C. abortus infection [51]. In spleen, CD8+ve T cells depletion in experimentally infected mice induced an increase in the secretion of IFN-γ, as well as augmented mortality and morbidity, whereas CD4+ve T cells depletion led to a decrease in morbidity. Therefore, CD8+ve T lymphocytes, in addition in playing an important direct role in controlling the infection, show also regulatory function, namely on the activity of CD4+ve T cells, preventing the immune response from being harmful (immunopathology) to the host [52].
Despite the initial immune response, generally the infection progresses towards the establishment of a persistent infection [53] to eventually reactivate when the sheep host becomes pregnant. This leads in most cases to late abortion of the foetus, while in other cases the delivery occurs normally, although clear placental infection accompanied by pathology can be present. Protective immunity develops at this stage and investigating the mechanisms of this have been at the basis of vaccine development. Vaccination programs triggering a protective immune response and consequent reduction of abortion occurrences can greatly contribute to the reduction in environmental contamination and disease spread. On the contrary, a common farming practice, the use of antibiotics, especially long-acting oxytetracycline (20 mg/kg) during the last month of pregnancy [54] to prevent abortion outbreaks, is not advised. Oxytetracycline treatment is not guaranteed to eradicate disease at flock level, cannot reverse heavy infections and their prophylactic use could potentially lead to emergence of acquired tetracycline resistance, such as that observed for Chlamydia suis [55]. However, according to a 1980 study [56], routine administration of oxytetracyclines fortnightly during pregnancy and until lambing seems to reduce or eliminate chlamydial shedding, which is crucial to prevent excretion of C. abortus at birth as well as on-farm spread of the infection.
A better preventative approach is instead the use of vaccines. Several vaccines are currently available for the prevention of OEA, depending on the country. Specifically, two live attenuated vaccines are marketed throughout Europe: Enzovax® (MSD Animal Health) and Cevac Chlamydia® (Ceva Animal Health Ltd). In addition, Mydiavac® (Benchmarks Vaccines Ltd. UK) and INMEVA® (Laboratorios Hipra S.A.) [57], both killed vaccines, consisting of inactivated EBs or of their sub-constituents, are also available in the UK and mainland Europe. The live attenuated vaccines are both based on a live attenuated strain, called 1B, which was obtained by chemical mutagenesis of the wild-type strain AB7, making 1B temperature-sensitive and unable to grow at the temperature of 39.5 °C, which is the normal body temperature of sheep [58]. With only ten single-nucleotide polymorphisms (SNPs) differentiating strain 1B from the original wild type strain, it has been suggested that there is no genetic basis for attenuation [41] and vaccine protection has been attributed to the high dose of live microorganisms administered with the vaccine as demonstrated by a recent study where ewes experimentally infected with low (5 × 103 IFU) and medium (5 × 105 IFU) doses of C. abortus, developed disease, whereas animals receiving high doses (5 × 107 IFU) showed a protective immune response which prevented abortion [23].
Despite the vaccines conferring a great protection against C. abortus and reducing the incidence of abortion, they have some drawbacks: production is expensive, operator infection after accidental injection during administration has been reported, conflicting evidences are outlined on reduction of shedding from ewes and, in some animals, presence of an infection indistinguishable from that seen with the wild-type microorganism, causing the development of placental lesions and abortion in the vaccinated flock [41, 59,60,61,62,63,64]. On the other side, inactivated vaccines are able to reduce the incidence of abortions and the shedding of C. abortus at parturition, but they do not prevent shedding completely [57].
Vaccine research is currently focussed on the development of vaccines that are effective, safe for operators, economical in production and that develop a durable and sterile protective immunity without causing disease or excessive inflammation [53]. The research therefore aims at developing the next generation of vaccines, in particular subunit and DNA vaccines. These are based on a number of different targets including the major outer membrane protein (MOMP), a highly immunogenic protein exposed on the surface [65, 66], CPAF (Chlamydia Protease-like Activity Factor), MIP (Macrophage Infectivity Potentiator) [65] and Pmp18.1 [67]. However, none of these vaccines have yet yielded satisfactory results, lacking effectiveness in protection greater or equal to the live attenuated vaccines currently used [68]. Conversely, vaccine preparations based on C. abortus outer membrane complexes (COMC) have shown more promise in several animal models [69,70,71,72] as well as in the natural sheep host [73] probably due to the preservation of the native conformation of the different components.
7 Diagnosis
An initial diagnosis of Ovine Enzootic Abortion can be achieved by investigating flock history (abortion in the last 2–3 weeks of gestation, birth of stillborn lambs) in combination with examination of the placental membranes which will show inflammation and necrosis [2, 9]. However, diagnostic laboratory confirmation is also required, to differentiate infections by Coxiella burnetii, Campylobacter fetus and Toxoplasma gondii [3]. Diagnosis can be achieved by direct identification of the agent or by serological tests.
Direct identification of the agent can be achieved through staining of smears of placental cotyledons, foetal stomach contents or vaginal swabs of ewes that aborted in the previous 24 h [1] using modified Macchiavello, Giemsa, Brucella differential, or modified Ziehl–Neelsen (MZN) procedures. Of these, MZN is the most reliable method according to the OIE Terrestrial Manual [1, 3]. In order to differentiate C. burnetii from C. abortus, it is also possible to perform a Fluorescent antibody test (FAT) using monoclonal antibodies or a specific antiserum [1]. Antigen detection with ELISA is also possible, as well as Immunohistochemistry. Diagnosis can also be reached by isolating the agent, through cell cultures, using mainly McCoy or Baby Hamster Kidney (BHK) cells or chicken embryos, starting from infected tissue samples (infected cotyledons, intercotyledonary membranes, vaginal swabs and foetal tissues), but this method is outdated and therefore used only in specific circumstances, such as when direct organism isolation is required [1, 3].
The most frequently used diagnostic methods are however molecular, via conventional or Real Time PCR or DNA microarray/ArrayTube microarray (Sachse et al. 2005). Highly sensitive and specific protocols, targeting the 16S-23S rRNA region or the pmp genes have been published by Pantchev et al. (2009) and Laroucau et al. (2001) [75,76,77]. The PCR can also be combined with restriction fragment length polymorphism (RFLP) analysis, to distinguish between the different Chlamydia species, namely C. psittaci, C. abortus and C. pecorum [78, 79]. Real time PCR is widely used for diagnosis because of its specificity, standardized protocols and allows quantification of the chlamydial load [80, 81]. According to the OIE Terrestrial Manual [1] when Real Time PCR is used for diagnosis, a hierarchical use of the technique is recommended, initially performing a PCR screening specific for Chlamydiaceae, by amplifying the 23S rRNA region followed by a PCR assay specific to C. abortus, targeting sequences of the outer membrane protein [82] or performing a DNA microarray. Another technique allowing a specific and sensitive diagnosis is the TETR (Touchdown Enzyme Time-Release)-PCR assay, which delivers a rapid diagnosis in comparison to classical methods [83]. However, it should be noted that PCR detects only DNA presence and not infectivity; data correlating these two parameters would be very useful, especially when evaluation environmental contamination and transmission events.
Serological tests have been used as diagnostic methods for long time. Historically, the complement fixation test (CF) has been the standard serological method for the diagnosis of OEA, however alternative tests are now preferred, as CF is characterized by low specificity [84], due to cross-reactivity of the LPS antigen, which is present in all Chlamydiaceae and in some Gram-negative bacteria (Acinetobacter) [1]. Alternatives to the CF are enzyme linked immunosorbent assays (ELISA), which are more sensitive and specific [85, 86]. Many commercial ELISA kits are available, mainly based on three antigens: MOMP, POMP and LPS. Literature comparison between different ELISA assays shows different levels of sensitivity and specificity, for example, an LPS-indirect ELISA proved to be very sensitive, but not specific enough to distinguish between C. abortus and C. pecorum [85]. A MOMP ELISA showed less cross-reactivity when compared to the CF test, although it was shown to be poorly sensitive in most cases [87]. The indirect POMP ELISA on the other hand, showed good sensitivity in many studies and is considered one of the promising alternatives to the CF test [88,89,90].
Despite the current growth of Environmental DNA approaches for accurate and cost effective detection of pathogens in environmental samples [91], to the authors knowledge, no studies have been conducted to assess C. abortus presence and abundance in different environments potentially linked to transmission occurrences. This highlights a research gap which could yield important information for the management and control of the disease and the zoonotic spread.
8 Epidemiology
C. abortus infection is distributed worldwide, and its disease manifestation, EAE, has been reported in several European countries [92,93,94,95,96,97,98,99,100,101] and South and North America [2, 102,103,104,105,106]. There seems however to be a limited number of serological or epidemiological studies carried out in developing countries, such as Asia [6, 107,108,109,110,111,112,113,114,115,116] and Africa [117,118,119,120,121,122,123,124]. Furthermore, in New Zealand and Australia, very few cases of infection with C. abortus have been identified, and EAE doesn’t seem to represent a major problem [125]. According to the Australian Department of Primary Industries, EAE has never occurred in Australia [126]; however few instances of abortion attributed to infection with Chlamydia pecorum in sheep, as well as C. psttaci in horses, have been identified in NSW in association with placentitis [127]. West in 2002 and Harvey in 2019 indicated that New Zealand is free of C. abortus [127, 128]. Nevertheless, the true prevalence and distribution of EAE however is not completely understood, since relevant data are not collected systematically at a global level and often the only information available is from sporadic reports of diagnosed cases or sero-epidemiological surveys. Figure 2 and Additional file 1 show global seroprevalence rates and detection in different hosts and countries respectively, according to the available (often not exhaustive) data [95, 116, 129,130,131,132,133,134,135,136,137,138,139,140,141,142,143,144,145,146]. The represented distribution is likely to be underestimated in comparison with the actual prevalence of C. abortus, both because of the small amount of data available globally and because of the variable specificity of the tests available for the detection of C. abortus.
Representation of the global spread of C. abortus. The reconstruction of the map is based on the collection of data available to date, not exhaustive and probably far from representing the real situation. In addition, the tests used in the seroprevalence study have varying specificity levels, sometimes confusing some Chlamydial species. A The percentage of seroprevalence in the different countries where the studies were conducted (different color). B The percentage of seroprevalence in the different countries (spot size) and the animal species concerned (different color).
9 Environmental contamination
Environment contamination with possibility of transmission of C. abortus is generally thought to occur through pasture/farm contamination by placenta, abortion material including dead lambs, the coats of dead and alive lambs and post-partum vaginal secretions. C. abortus shows a great resistance to inactivation, mainly due to the EBs structural conformation and the presence of a “outer membrane complex”, a spore-like cell wall stabilized by a series of proteins bound together by disulfide bridges responsible for resistance to the extracellular environment by making the pathogen osmotically stable and poorly permeable [7]. This feature represents a critical point in the transmission of C. abortus: following abortion, the EBs-loaded infected placenta is expelled and vaginal discharges are spread in the surrounding environment. These organs and secretions contain the highest bacterial load and represent the main source of infection, both for animals and for humans. In a recent study, aborting ewes were shown to shed higher numbers of C. abortus (up to an average of 2.7 × 107 chlamydial genomes per microgram of total tissue DNA) in vaginal swabs and placental material [82] compared to ewes that produced live lambs, when quantified by qPCR [65]; moreover, vaccinated ewes demonstrated even lower levels of bacterial shedding (average 4 × 104).
The risk of transmission through vaginal fluids is reduced 2–3 weeks after abortion, when the discharges begin to dry and stop, although it is still necessary to maintain biosecurity measures [147]. Other risks, although to a lesser extent, are related to the contact of a healthy subject (animal or human) with an aborting sheep, sheep at risk of abortion and dead lambs. An additional risk is related to the ingestion of grass or pasture contaminated by the abortion products by ruminants or other animals [30, 148]. Moreover, Gupta et al. [149] identified presence of C. abortus in conjunctival swabs from ruminants, indicating that other organs/apparatuses can also be involved in carrying the bacteria and possibly in interspecies transmission. In pigs, one instance of C. abortus identification in conjunctival swab in a potential mixed infection with C. pecorum and C. suis has been associated with ruminant contact [150]. In horses, occurrences of abortion linked to C. abortus infection have been reported [151,152,153] showing that C. abortus is present in equine foetal membranes, therefore these and veterinary or husbandry care around abortion, still birth or foaling should also be considered a potential zoonotic risk.
Seroprevalence studies have further highlighted the wider species distribution of the infection, which also extends to wildfowl [154], psittacids [155], chickens [156], llamas [147], fur animals [157], yaks [158,159,160], deer [161] and dolphins [162]. In chickens, a study conducted by Szymańska-Czerwińska et al. (2017) identified a seroprevalence of 15.4% at flock level, and this species is thought to represent an asymptomatic carrier [156] which could be relevant for environmental contamination and risk of zoonosis. Serological survey on roe deer (Capreolus capreolus) in Flanders by Tavernier et al. in 2015, detected a seroprevalence of C. abortus of more than 20% [161] although a similar study in Italian red deer [163] could not find any evidence of exposure. The differences in deer species, the territory covered as well as the probability of coming into contact with livestock might explain this result, or at least evidence the fact that the amount of available information, even based on serosurveys, is still very limited. Farmed fur animals such as foxes, raccoon dogs and mink were also shown, by molecular methods, to harbour Chlamydia spp., with C. abortus being the dominant Chlamydia species identified [157]. Phylogenetic analysis showed high similarity of these Chlamydia species to C. abortus S26/3 and B577, generally found in ruminants, although there is no information regarding potential for transmissibility between these hosts, other animal species and humans. The authors hypothesise that feed contamination (feed containing C. abortus-infected pork), could represent a potential route of transmission, and highlight the potential for a zoonotic transmission through contact with faeces of the infected animals.
Birds, both urban and wild, have also been implicated as possible reservoir species. Urban pigeons were tested for possible transmission of C. abortus to humans in a 2012 study [164]: whereas C. psittaci was the predominant chlamydial agent detected and cultivated from cloacal swabs and faecal samples, C. abortus was also identified in a small number of samples. Testing of community workers in daily contact with the pigeons however did not provide indication of exposure (both PCR and antibody negative). However, in a different study, no C. abortus was detected in a large cohort (431) of pigeons and doves, which were instead carrying other chlamydial species [165]. Similarly, an investigation on the potential for outdoor farmed turkeys to harbour and transmit C. abortus to abattoir workers provided negative results, albeit detecting 0.7% positivity for another chlamydial pathogen, namely C. gallinacea [166]. Oral uptake of C. abortus and faecal excretion with or without host infection, could nevertheless contribute to dissemination, as proven by analogy in ducklings where a C. psittaci challenge was followed by bird-to-bird transmission of the challenge strains [167], supporting previous findings of grassland contamination through faecal shedding [168]. Moreover, a number of published works in wild birds found chlamydial species that could not be classified but represented instead intermediates between C. psittaci and C. abortus [169,170,171,172,173]. Recently, a new group of avian C. abortus strains with worldwide distribution in various wild bird species has been described [174]. Whole genome sequencing (WGS) of three of these strains (15-70d24, 15-49d3 and 15-58d44, representing genotypes G1, G2 and 1V, respectively) indicated that these avian C. abortus strains show features characteristic of both C. abortus and C. psittaci species, although phylogenetic analyses demonstrated a closer relationship with classic C. abortus strains. Currently, species classification established by the ICSP Subcommittee on the taxonomy of Chlamydiae, determines that these avian C. abortus strains 15-70d24, 15-49d3 and 15-58d44 should be classified as C. abortus. However, the authors of this study conclude that the current taxonomic definition of C. abortus is outdated and should be amended to include two subgroups, mammalian and avian, the latter of which would include all isolates so far referred to as atypical C. psittaci or C. psittaci/C. abortus intermediates [174]. The zoonotic potential and the potential for environmental contamination from these species is still unknown, however, considering their close relationship to two of the most widespread zoonotic Chlamydiaceae, it cannot be excluded.
In Argentina, a study conducted by Origlia et al. in 2019, provided the first description of psittacine pet birds infection in symptomatic and asymptomatic animals. Although this evidence needs to be confirmed by additional studies, a new hypothesis has been formulated regarding the possibility that these animals also represent a reservoir of C. abortus [155]. Finally, intermediate C. psittaci/C. abortus strains were also isolated from Polish wildfowl [154], as well as swans and mallards which, living in closer contact with human settlements, might also be a possible source of environmental contamination and population exposure. The majority of Chlamydiae detected in this study were classified as new genotypes, phylogenetically closer to C. abortus, with the authors proposing a reclassification of this species to include isolates of avian origin, as well as mammalian ones.
C. abortus has also been detected by molecular methods in a boa constrictor [175] held in captivity, although the significance of this particular finding is not clear, especially considering that snakes harbour C. pneumoniae, which is the most commonly reported etiological agent in reptilian chlamydiosis, in addition to their own Chlamydia species and several Chlamydia-like organisms. Finally, Chlamydia-like organisms have been detected in several environments including water [176, 177], inside amoebae [178], in flea [179] and ticks [180, 181].
In Africa, several wild animals from the Serengeti National Park were surveyed by Pospischil et al. (2012) with C. abortus identified (by Real Time PCR, microarray and sequencing followed by serological assays) for the first time in African buffalos and a spotted hyena. It is possible that African buffalos may have come into contact with farmed cattle and thus contracted the infection, whereas the positivity of the spotted hyena could be linked to consuming meat of infected animal [182]. In another study carried out in Africa, an increased number of infections in farmed animals was demonstrated in areas where contact with the local wild fauna and people occurs, due to the lack of physical barriers [183]. The same situation seems also to be present in northeastern China in the Xinjiang region, where goitered gazelles (Gazella subgutturosa) were found positive for C. abortus, and thus are considered a carrier in this region [184].
Overall, our literature search revealed lack of data on environmental detection, distribution and quantification of C. abortus. Therefore, further work should address these gaps to evaluate the degree of contamination of pastures and other environmental areas potentially infected by C. abortus in relation with conditions such as temperature and humidity, in order to establish exposure risks. By analogy, C. psittaci elementary bodies can remain infectious in the environment for months with persistence on dry inanimate surfaces reported for up to 15 days [185]. Another challenge is represented by the identification of the geographic distribution of C. abortus among wild and farmed animals.
10 Management of disease
Following an initial abortion a number of approaches are required to limit environmental contamination and infection spread until a definitive diagnosis is reached. Ewes that have aborted must be isolated for a minimum of 7–10 days, or until the post-partum discharges have dried up. Live lambs, if present, must also be isolated with their mother. Bedding, placenta and dead lambs must be disposed safely, using protective equipment (gloves and waterproofs at minimum) and limiting contact with farm staff and other individuals to the minimum possible [2, 3, 186]. Cleaning and disinfection of the affected area needs to be carried out as soon as possible, again wearing PPE and washing hands after contact with the affected animals and possible fomites. PPE and work clothes need to be washed and/or disinfected as soon as possible, considering the possibility of transmission of the infection to other members of the household. C. abortus is resistant to acid and alkali therefore disinfectants such as quaternary ammonium compounds, isopropanol alcohol, household bleach or chlorophenols are recommended for cleaning potentially infected areas. Following the initial abortion episode, it is important to identify additional infected ewes as soon as possible to limit the spread of the infection, not only during the current lambing seasons but also to minimise consequences in the next breeding season. Despite being refractory to another abortion episode, ewes that have aborted might became persistently infected and excrete C. abortus at the next breeding season [2, 3, 186]. Moreover, ewes or lambs that became infected as consequence of the initial abortion can became latently infected and abort at the successive season. Therefore, a close flock, or one where replacement animals are acquired from an accredited breeder, along with vaccination, is the optimal way to reduce the introduction of C. abortus in a flock. Additionally, rams, birds, dogs, feral sheep and wildlife should be considered for potential zoonotic risk [154, 157].
11 Conclusions
This review encompasses the available research findings related to C. abortus and highlights future research needs, which are mainly related to the risk of exposure to this microorganism. Besides farmed animals, wild or non-farmed animals can act as reservoirs, and therefore can contribute to the transmission and environmental spread of C. abortus in different locations, both to other animals and humans, making controlling the spread of the pathogen more difficult. In this regard, all the evidence indicate that future work should concentrate on multiple topics, including the deepening of bacterial evolutionary strategies leading to genetic and genomic changes responsible for host and environment adaptation, the elucidation of host–pathogen interaction mechanisms and some pathogenetic aspects linked to transmission, latency, host immune response and persistence. More complete epidemiological surveys at animal and human levels are also advisable in order to determine distribution and quantification of Chlamydia abortus worldwide, as well as the development of protective and safe new generation vaccines. For example, a number of studies conducted on non-canonical species (eg avian, wildlife, reptiles etc.) has also provided contradictory findings, with contrasting seroprevalence levels in similar species observed and/or presence/absence detected at molecular level. Whereas differences in cohorts, methodologies and population dynamics can explain this observation, this highlights the need for more work in this area to understand which additional animal species can act as carriers and their relative importance to the spread of the disease to livestock and humans.
Finally, there is an almost complete lack of evidence related to environmental diagnosis, along with the need for the improvement of serological tests and the definition of correlations between infectivity and molecular detection. Further knowledge of the impact of available vaccines on environmental contamination as well as the development of candidate vaccines able to control the bacterial shedding also represent an urgent need.
Addressing these research needs will improve the knowledge, assess the extent of the problem, and consequently develop more effective control strategies to reduce C. abortus transmission between animals, wildlife and humans within an “One Health” approach.
Abbreviations
- C. abortus :
-
Chlamydia abortus
- EAE:
-
enzootic abortion of ewes
- OEA:
-
ovine enzootic abortion
- CDS:
-
coding sequence
- pmp :
-
Polymorphic membrane proteins
- TMH/Inc:
-
transmembrane head/Inclusion membrane protein
- PZ:
-
plasticity zone
- trp:
-
tryptophan
- EB:
-
elementary body
- T3SS:
-
Type 3 secretion system
- RB:
-
reticulate body
- IFN-γ:
-
interferon-gamma
- IDO:
-
indoleamine-2,3-dioxygenase
- LPS:
-
lipopolysaccharide
- Th1:
-
T helper 1
- Th2:
-
T helper 2
- IL:
-
interleukin
- TNF-α:
-
tumor necrosis factor-alpha
- PCR:
-
polymerase chain reaction
- PMN:
-
polymorhonuclear
- NK:
-
natural killer
- SNP:
-
single-nucleotide polymorphism
- MOMP:
-
major outer membrane protein
- CPAF:
-
Chlamydia protease-like activity factor
- MIP:
-
macrophage infectivity potentiator
- COMC:
-
Chlamydia abortus outer membrane complex
- MZN:
-
modified Ziehl–Neelsen
- FAT:
-
fluorescent antibody test
- BHK:
-
Baby Hamster Kidney
- RFLP:
-
restriction fragment length polymorphism
- TETR:
-
touchdown enzyme time-release
- CF:
-
complement fixation
- ELISA:
-
enzyme linked immunosorbent assay
- POMP:
-
polymorphic outer membrane protein
- NSW:
-
New South Wales
- qPCR:
-
quantitative PCR
- PPE:
-
personal protective equipment
References
OIE Terrestrial Manual. 2018. Office International des Epizooties. Chapter 3.7.5. - Enzootic abortion of ewes (ovine chlamydiosis). In: Manual of diagnostic tests and vaccines for terrestrial animals. World Organisation for Animal Health, pp 1456–1465. https://www.oie.int/fileadmin/Home/eng/Health_standards/tahm/3.07.05_ENZ_ABOR.pdf
Longbottom D, Coulter LJ (2003) Animal chlamydiosis and zoonotic implications. J Comp Pathol 128:217–244
Aitken ID, Longbottom D (2007) Chlamydial abortion. In: Aitken ID (ed) Disease of Sheep, Wiley-Blackwell, Edinburgh, pp 105–112
Tibary A (2021) Abortion in sheep. In: MSD Manual Veterinary Manual. https://www.msdvetmanual.com/reproductive-system/abortion-in-large-animals/abortion-in-sheep. Accessed April 2021
Buxton D, Anderson IE, Longbottom D, Livingstone M, Wattegedera S, Entrican G (2002) Ovine chlamydial abortion: characterization of the inflammatory immune response in placental tissues. J Comp Pathol 127:133–141
Arif ED, Saeed NM, Rachid SK (2020) Isolation and identification of Chlamydia abortus from aborted ewes in Sulaimani Province, Northern Iraq. Pol J Microbiol 69:1–7
Kerr K, Entrican G, McKeever D, Longbottom D (2005) Immunopathology of Chlamydophila abortus infection in sheep and mice. Res Vet Sci 78:1–7
Burnard D, Polkinghorne A (2016) Chlamydial infections in wildlife-conservation threats and/or reservoirs of “spill-over” infections? Vet Microbiol 196:78–84
Essig A, Longbottom D (2015) Chlamydia abortus: new aspects of infectious abortion in sheep and potential risk for pregnant women. Curr Clin Microbiol Rep 2:22–34
Hackstadt T (2012) Initial interactions of Chlamydiae with the host cell. In: Tan M, Bavoil PM (eds) Intracellular Pathogens 1: Chlamydiales. ASM Press, Washington (DC), pp 126–148
Hegemann JH, Moelleken K (2012) Chlamydial adhesion and adhesins. In: Tan M, Bavoil PM (eds) Intracellular Pathogens 1: Chlamydiales. ASM Press, Washington (DC), pp 97–125
Kokes M, Valdivia RH (2012) Cell biology of the chlamydial inclusion. In: Tan M, Bavoil PM (eds) Intracellular Pathogens 1: Chlamydiales. ASM Press, Washington (DC), pp 170–191
Tan M (2012) Temporal gene regulation during the chlamydial developmental cycle. In: Tan M, Bavoil PM (eds) Intracellular Pathogens 1: Chlamydiales. ASM Press, Washington (DC), pp 149–169
Thomson NR, Yeats C, Bell K, Holden MT, Bentley SD, Livingstone M, Cerdeño-Tárraga AM, Harris B, Doggett J, Ormond D, Mungall K, Clarke K, Feltwell T, Hance Z, Sanders M, Quail MA, Price C, Barrell BG, Parkhill J, Longbottom D (2005) The Chlamydophila abortus genome sequence reveals an array of variable proteins that contribute to interspecies variation. Genome Res 15:629–640
Entrican G (2002) Immune regulation during pregnancy and host-pathogen interactions in infectious abortion. J Comp Pathol 126:79–94
Elwell C, Mirrashidi K, Engel J (2016) Chlamydia cell biology and pathogenesis. Nat Rev Microbiol 14:385–400
Abdelrahman YM, Belland RJ (2005) The Chlamydial developmental cycle. FEMS Microbiol Rev 29:949–959
Polkinghorne A, Vaughan L (2011) Chlamydia abortus YhbZ, a truncated Obg family GTPase, associates with the Escherichia coli large ribosomal subunit. Microb Pathog 50:200–206
Jones GE, Anderson IE (1988) Chlamydia psittaci: is tonsillar tissue the portal of entry in ovine enzootic abortion? Res Vet Sci 44:260–261
Brown J, Howie SE, Entrican G (2001) A role for tryptophan in immune control of chlamydial abortion in sheep. Vet Immunol Immunopathol 82:107–119
Entrican G (2004) IDO: a crossroads of immunology and physiology? J Reprod Immunol 61:63–65
Entrican G, Buxton D, Longbottom D (2001) Chlamydial infection in sheep: immune control versus fetal pathology. J R Soc Med 94:273–277
Longbottom D, Livingstone M, Maley S, van der Zon A, Rocchi M, Wilson K, Wheelhouse N, Dagleish M, Aitchison K, Wattegedera S, Nath M, Entrican G, Buxton D (2013) Intranasal infection with Chlamydia abortus induces dose-dependent latency and abortion in sheep. PLoS One 8:e57950
Gutierrez J, William EJ, O’Donovan J, Brady C, Proctor AF, Marques PX, Worrall S, Nally JE, McElroy M, Bassett HF, Sammin DJ, Markey BK (2011) Monitoring clinical outcomes, pathological changes and shedding of Chlamydophila abortus following experimental challenge of periparturient ewes utilizing the natural route of infection. Vet Microbiol 147:119–126
Brown J, Entrican G (1996) Interferon-gamma mediates long-term persistent Chlamydia psittaci infection in vitro. J Comp Pathol 115:373–383
Papp JR, Shewen PE, Gartley CJ (1993) Chlamydia psittaci infection and associated infertility in sheep. Can J Vet Res 57:185–189
Buxton D, Barlow RM, Finlayson J, Anderson IE, Mackellar A (1990) Observations on the pathogenesis of Chlamydia psittaci infection of pregnant sheep. J Comp Pathol 102:221–237
Rocchi MS, Wattegedera S, Meridiani I, Entrican G (2009) Protective adaptive immunity to Chlamydophila abortus infection and control of ovine enzootic abortion (OEA). Vet Microbiol 135:112–121
Wattegedera SR, Livingstone M, Maley S, Rocchi M, Lee S, Pang Y, Wheelhouse NM, Aitchison K, Palarea-Albaladejo J, Buxton D, Longbottom D, Entrican G (2020) Defining immune correlates during latent and active chlamydial infection in sheep. Vet Res 51:75
Navarro JA, García de la Fuente JN, Sánchez J, Martínez CM, Buendía AJ, Gutiérrez-Martín CB, Rodriguez-Ferri EF, Ortega N, Salinas J (2004) Kinetics of infection and effects on the placenta of Chlamydophila abortus in experimentally infected pregnant ewes. Vet Pathol 41:498–505
Sammin D, Markey B, Bassett H, Buxton D (2009) The ovine placenta and placentitis-A review. Vet Microbiol 135:90–97
Maley SW, Livingstone M, Rodger SM, Longbottom D, Buxton D (2009) Identification of Chlamydophila abortus and the development of lesions in placental tissues of experimentally infected sheep. Vet Microbiol 135:122–127
Álvarez D, Caro MR, Buendía AJ, Schnee C, Ortega N, Murcia-Belmonte A, Salinas J (2019) Effect of female sex hormones on the developmental cycle of Chlamydia abortus compared to a penicillin-induced model of persistent infection. BMC Vet Res 15:259
Sammin DJ, Markey BK, Quinn PJ, McElroy MC, Bassett HF (2006) Comparison of fetal and maternal inflammatory responses in the ovine placenta after experimental infection with Chlamydophila abortus. J Comp Pathol 135:83–92
Leaver H, Howie A, Appleyard W, Aitken I, Hay L (1987) Altered steroid hormone and prostaglandin metabolism during chlamydial infection in sheep. Biochem Soc Transactions 15:479–479
Leaver H, Howie A, Aitken I, Appleyard B, Anderson I, Jones G, Hay L, Williams GE, Buxton D (1989) Changes in progesterone, oestradiol 17β, and intrauterine prostaglandin E2 during late gestation in sheep experimentally infected with an ovine abortion strain of Chlamydia psittaci. Microbiology 135:565–573
Howie A, Leaver HA, Aitken ID, Hay LA, Anderson IE, Williams GE, Jones G (1989) The effect of chlamydial infection on the initiation of premature labour: serial measurements of intrauterine prostaglandin E2 in amniotic fluid, allantoic fluid and utero-ovarian vein, using catheterised sheep experimentally infected with an ovine abortion strain of Chlamydia psittaci. Prostaglandins Leukot Essent Fatty Acids 37:203–211
Hagemann JB, Simnacher U, Longbottom D, Livingstone M, Maile J, Soutschek E, Walder G, Boden K, Sachse K, Essig A (2016) Analysis of humoral immune responses to surface and virulence-associated Chlamydia abortus proteins in ovine and human abortions by use of a newly developed line immunoassay. J Clin Microbiol 54:1883–1890
Meijer A, Brandenburg A, de Vries J, Beentjes J, Roholl P, Dercksen D (2004) Chlamydophila abortus infection in a pregnant woman associated with indirect contact with infected goats. Eur J Clin Microbiol Infect Dis 23:487–490
Pichon N, Guindre L, Laroucau K, Cantaloube M, Nallatamby A, Parreau S (2020) Chlamydia abortus in pregnant woman with acute respiratory distress syndrome. Emerging Infect Dis 26:628–629
Longbottom D, Sait M, Livingstone M, Laroucau K, Sachse K, Harris SR, Thomson NR, Seth-Smith H (2018) Genomic evidence that the live Chlamydia abortus vaccine strain 1B is not attenuated and has the potential to cause disease. Vaccine 36:3593–3598
Walder G, Meusburger H, Hotzel H, Oehme A, Neunteufel W, Dierich MP, Würzner R (2003) Chlamydophila abortus pelvic inflammatory disease. Emerg Infect Dis 9:1642–1644
Jorgensen DM (1997) Gestational Psittacosis in a Montana sheep rancher. Emerg Infect Dis 3:191–194
Walder G, Hotzel H, Brezinka C, Gritsch W, Tauber R, Würzner R, Ploner F (2005) An unusual cause of sepsis during pregnancy: recognizing infection with Chlamydophila abortus. Obstet Gynecol 106:1215–1217
Borel N, Marti H, Pospischil A, Pesch T, Prähauser B, Wunderlin S, Seth-Smith HMB, Low N, Flury R (2018) Chlamydiae in human intestinal biopsy samples. Pathog Dis 76:fty081
Ortega N, Caro MR, Gallego MC, Murcia-Belmonte A, Álvarez D, Del Río L, Cuello F, Buendía AJ, Salinas J (2016) Isolation of Chlamydia abortus from a laboratory worker diagnosed with atypical pneumonia. Ir Vet J 69:8
Caro MR, Buendía AJ, Del Rio L, Ortega N, Gallego MC, Cuello F, Navarro JA, Sanchez J, Salinas J (2009) Chlamydophila abortus infection in the mouse: a useful model of the ovine disease. Vet Microbiol 135:103–111
Buendía AJ, Sánchez J, Martínez MC, Cámara P, Navarro JA, Rodolakis A, Salinas J (1998) Kinetics of infection and effects on placental cell populations in a murine model of Chlamydia psittaci-induced abortion. Infect Immun 66:2128–2134
de Oca RM, Buendía AJ, Del Río L, Sánchez J, Salinas J, Navarro JA (2000) Polymorphonuclear neutrophils are necessary for the recruitment of CD8(+) T cells in the liver in a pregnant mouse model of Chlamydophila abortus (Chlamydia psittaci serotype 1) infection. Infect Immun 68:1746–1751
Buendía AJ, Martínez CM, Ortega N, Del Río L, Caro MR, Gallego MC, Sánchez J, Navarro JA, Cuello F, Salinas J (2004) Natural killer (NK) cells play a critical role in the early innate immune response to Chlamydophila abortus infection in mice. J Comp Pathol 130:48–57
Del Río L, Buendía AJ, Sánchez J, Garcés B, Caro MR, Gallego MC, Bernabé A, Cuello F, Salinas J (2000) Chlamydophila abortus (Chlamydia psittaci serotype 1) clearance is associated with the early recruitment of neutrophils and CD8(+)T cells in a mouse model. J Comp Pathol 123:171–181
Martínez CM, Buendía AJ, Sánchez J, Ortega N, Caro MR, Gallego MC, Navarro JA, Cuello F, Salinas J (2006) Relative importance of CD4+ and CD8+ T cells in the resolution of Chlamydophila abortus primary infection in mice. J Comp Pathol 134:297–307
Entrican G, Wheelhouse N, Wattegedera SR, Longbottom D (2012) New challenges for vaccination to prevent chlamydial abortion in sheep. Comp Immunol Microbiol Infect Dis 35:271–276
Bommana S, Polkinghorne A (2019) Mini review: antimicrobial control of chlamydial infections in animals: current practices and issues. Front Microbiol 10:113
Marti H, Kim H, Joseph SJ, Dojiri S, Read TD, Dean D (2017) Tet(C) gene transfer between Chlamydia suis strains occurs by homologous recombination after co-infection: implications for spread of tetracycline-resistance among Chlamydiaceae. Front Microbiol 8:156
Rodolakis A, Souriau A, Raynaud JP, Brunault G (1980) Efficacy of a long-acting oxytetracycline against chlamydial ovine abortion. Ann Rech Vet 11:437–344
Montbrau C, Fontseca M, March R, Sitja M, Benavides J, Ortega N, Caro MR, Salinas J (2020) Evaluation of the efficacy of a new commercially available inactivated vaccine against ovine enzootic abortion. Front Vet Sci 7:593
Rodolakis A, Bernard F (1984) Vaccination with temperature-sensitive mutant of Chlamydia psittaci against enzootic abortion of ewes. Vet Rec 114:193–194
Sargison ND, Truyers IG, Howie FE, Thomson JR, Cox AL, Livingstone M, Longbottom D (2015) Identification of the 1B vaccine strain of Chlamydia abortus in aborted placentas during the investigation of toxaemic and systemic disease in sheep. N Z Vet J 63:284–287
Wheelhouse N, Aitchison K, Laroucau K, Thomson J, Longbottom D (2010) Evidence of Chlamydophila abortus vaccine strain 1B as a possible cause of ovine enzootic abortion. Vaccine 28:5657–5663
Laroucau K, Aaziz R, Vorimore F, Menard MF, Longbottom D, Denis G (2018) Abortion storm induced by the live C. abortus vaccine 1B strain in a vaccinated sheep flock, mimicking a natural wild-type Infection. Vet Microbiol 225:31–33
Caspe SG, Livingstone M, Frew D, Aitchison K, Wattegedera SR, Entrican G, Palarea-Albaladejo J, McNeilly TN, Milne E, Sargison ND, Chianini F, Longbottom D (2020) The 1B vaccine strain of Chlamydia abortus produces placental pathology indistinguishable from a wild type infection. PLoS One 15:e0242526
Caspe SG, Palarea-Albaladejo J, Underwood C, Livingstone M, Wattegedera SR, Milne E, Sargison ND, Chianini F, Longbottom D (2021) Distribution and severity of placental lesions caused by the Chlamydia abortus 1B vaccine strain in vaccinated ewes. Pathogens 10:543
Livingstone M, Caspe SG, Longbottom D (2021) Complete genome sequence of Chlamydia abortus MRI-10/19, isolated from a sheep vaccinated with the commercial LiveC. abortus1B vaccine strain. Microbiol Resour Announc 10:e00203-e221
O’Neill LM, Keane OM, Ross PJ, Nally JE, Seshu J, Markey B (2019) Evaluation of protective and immune responses following vaccination with recombinant MIP and CPAF from Chlamydia abortus as novel vaccines for enzootic abortion of ewes. Vaccine 37:5428–5438
Ling Y, Liu W, Clark JR, March JB, Yang J, He C (2011) Protection of mice against Chlamydophila abortus infection with a bacteriophage-mediated DNA vaccine expressing the major outer membrane protein. Vet Immunol Immunopathol 144:389–395
Pan Q, Zhang Q, Chu J, Pais R, Liu S, He C, Eko FO (2017) Chlamydia abortus Pmp181 induces IL-1β secretion by TLR4 activation through the MyD88, NF-κB, and caspase-1 signaling pathways. Front Cell Infect Microbiol 7:514
Longbottom D, Livingstone M (2006) Vaccination against chlamydial infections of man and animals. Vet J 171:263–275
Batteiger BE, Rank RG, Bavoil PM, Soderberg LS (1993) Partial protection against genital reinfection by immunization of guinea-pigs with isolated outer-membrane proteins of the chlamydial agent of guinea-pig inclusion conjunctivitis. J Gen Microbiol 139:2965–2972
de Sa C, Souriau A, Bernard F, Salinas J, Rodolakis A (1995) An oligomer of the major outer membrane protein of Chlamydia psittaci is recognized by monoclonal antibodies which protect mice from abortion. Infect Immun 63:4912–4916
Pal S, Theodor I, Peterson EM, de la Maza LM (1997) Immunization with an acellular vaccine consisting of the outer membrane complex of Chlamydia trachomatis induces protection against a genital challenge. Infect Immun 65:3361–3369
Livingstone M, Wattegedera SR, Palarea-Albaladejo J, Aitchison K, Corbett C, Sait M, Wilson K, Chianini F, Rocchi MS, Wheelhouse N, Entrican G, Longbottom D (2021) Efficacy of two Chlamydia abortus subcellular vaccines in a pregnant ewe challenge model for ovine enzootic abortion. Vaccines 9:898
Tan TW, Herring AJ, Anderson IE, Jones GE (1990) Protection of sheep against Chlamydia psittaci infection with a subcellular vaccine containing the major outer membrane protein. Infect Immun 58:3101–3108
Sachse K, Hotzel H, Slickers P, Ellinger T, Ehricht R (2005) DNA microarray-based detection and identification of Chlamydia and Chlamydophila spp. Mol Cell Probes 19:41–50
Pantchev A, Sting R, Bauerfeind R, Tyczka J, Sachse K (2009) New real-time PCR tests for species-specific detection of Chlamydophila psittaci and Chlamydophila abortus from tissue samples. Vet J 181:145–150
Laroucau K, Souriau A, Rodolakis A (2001) Improved sensitivity of PCR for Chlamydophila using pmp genes. Vet Microbiol 82:155–164
Laroucau K, Vorimore F, Sachse K, Vretou E, Siarkou VI, Willems H, Magnino S, Rodolakis A, Bavoil PM (2010) Differential identification of Chlamydophila abortus live vaccine strain 1B and C. abortus field isolates by PCR-RFLP. Vaccine 28:5653–5656
Everett KD, Hornung LJ, Andersen AA (1999) Rapid detection of the Chlamydiaceae and other families in the order Chlamydiales: three PCR tests. J Clin Microbiol 37:575–580
Vorimore F, Cavanna N, Vicari N, Magnino S, Willems H, Rodolakis A, Siarkou VI, Laroucau K (2012) High-resolution melt PCR analysis for rapid identification of Chlamydia abortus live vaccine strain 1B among C. abortus strains and field isolates. J Microbiol Methods 90:241–244
Sachse K, Vretou E, Livingstone M, Borel N, Pospischil A, Longbottom D (2009) Recent developments in the laboratory diagnosis of chlamydial infections. Vet Microbiol 135:2–21
Opota O, Brouillet R, Greub G, Jaton K (2017) Methods for Real-Time PCR-based diagnosis of Chlamydia pneumoniae, Chlamydia psittaci, and Chlamydia abortus infections in an opened molecular diagnostic platform. Methods Mol Biol 1616:171–181
Livingstone M, Wheelhouse N, Maley SW, Longbottom D (2009) Molecular detection of Chlamydophila abortus in post-abortion sheep at oestrus and subsequent lambing. Vet Microbiol 135:134–141
Amin AS (2003) Application of touchdown enzyme time release (TETR)-PCR for diagnosis of Chlamydophila abortus infection. Res Vet Sci 74:213–217
Wilson K, Livingstone M, Longbottom D (2009) Comparative evaluation of eight serological assays for diagnosing Chlamydophila abortus infection in sheep. Vet Microbiol 135:38–45
O’Neill LM, O’Driscoll Á, Markey B (2018) Comparison of three commercial serological tests for the detection of Chlamydia abortus infection in ewes. Ir Vet J 71:13
Markey BK, McNulty MS, Todd D (1993) Comparison of serological tests for the diagnosis of Chlamydia psittaci infection of sheep. Vet Mcrobiol 36:233–252
Livingstone M, Entrican G, Wattegedera S, Buxton D, McKendrick IJ, Longbottom D (2005) Antibody responses to recombinant protein fragments of the major outer membrane protein and polymorphic outer membrane protein POMP90 in Chlamydophila abortus-infected pregnant sheep. Clin Diagn Lab Immunol 12:770–777
Buendía AJ, Cuello F, Del Rio L, Gallego MC, Caro MR, Salinas J (2001) Field evaluation of a new commercially available ELISA based on a recombinant antigen for diagnosing Chlamydophila abortus (Chlamydia psittaci serotype 1) infection. Vet Microbiol 78:229–239
Longbottom D, Psarrou E, Livingstone M, Vretou E (2001) Diagnosis of ovine enzootic abortion using an indirect ELISA (rOMP91B iELISA) based on a recombinant protein fragment of the polymorphic outer membrane protein POMP91B of Chlamydophila abortus. FEMS Microbiol Lett 195:157–161
McCauley LM, Lancaster MJ, Young P, Butler KL, Ainsworth CG (2007) Comparison of ELISA and CFT assays for Chlamydophila abortus antibodies in ovine sera. Aust Vet J 85:325–328
Peters L, Spatharis S, Dario MA, Dwyer T, Roca IJT, Kintner A, Kanstad-Hanssen Ø, Llewellyn MS, Praebel K (2018) Environmental DNA: a new low-cost monitoring tool for pathogens in salmonid aquaculture. Front Microbiol 9:3009
Greco G, Totaro M, Madio A, Tarsitano E, Fasanella A, Lucifora G, Buonavoglia D (2005) Detection of Chlamydophila abortus in sheep and goat flocks in southern Italy by PCR using four different primer sets. Vet Res Comm 29:107–115
Masala G, Porcu R, Sanna G, Tanda A, Tola S (2005) Role of Chlamydophila abortus in ovine and caprine abortion in Sardinia, Italy. Vet Res Commun 29:117–123
Cisláková L, Halánová M, Kovácová D, Stefancíková A (2007) Occurrence of antibodies against Chlamydophila abortus in sheep and goats in the Slovak Republic. Ann Agric Environ Med 14:243–245
Czopowicz M, Kaba J, Szaluś-Jordanow O, Nowicki M, Witkowski L, Nowicka D, Frymus T (2010) Prevalence of antibodies against Chlamydophila abortus and Coxiella burnetii in goat herds in Poland. Pol J Vet Sci 13:175–179
Runge M, Binder A, Schotte U, Ganter M (2012) Investigations concerning the prevalence of Coxiella burnetii and Chlamydia abortus in sheep in correlation with management systems and abortion rate in Lower Saxony in 2004. Berl Munch Tierarztl Wochenschr 125:138–143
Chisu V, Porcu R, Tanda A, Masala G (2013) First isolation and characterization of Chlamydophila abortus from abortion tissues of sheep in Sardinia, Italy. Vet Ital 49:331–334
Softic A, Asmare K, Granquist EG, Godfroid J, Fejzic N, Skjerve E (2018) The serostatus of Brucella spp, Chlamydia abortus, Coxiella burnetii and Neospora caninum in cattle in three cantons in Bosnia and Herzegovina. BMC Vet Res 14:40
Tejedor-Junco MT, González-Martín M, Corbera JA, Santana Á, Hernández CN, Gutiérrez C (2019) Preliminary evidence of the seroprevalence and risk factors associated with Chlamydia abortus infection in goats on the Canary Islands, Spain. Trop Anim Health Prod 51:257–260
Chisu V, Loi F, Mura L, Tanda A, Chessa G, Masala G (2021) Molecular detection of Theileria sergentii/orientalis/buffeli and Ehrlichia canis from aborted ovine and caprine products in Sardinia, Italy. Vet Med Sci 7:1762–1768
Zaręba-Marchewka K, Szymańska-Czerwińska M, Niemczuk K (2021) Draft genome sequences of avian Chlamydia abortus genotype G2 strain 15–49d3, isolated from Mallard, and genotype 1V strain 15–58d44, isolated from Magpie in Poland. Microbiol Resour Announc 10:e01203-e1220
Campos-Hernández E, Vázquez-Chagoyán JC, Salem AZ, Saltijeral-Oaxaca JA, Escalante-Ochoa C, López-Heydeck SM, de Oca-Jiménez RM (2014) Prevalence and molecular identification of Chlamydia abortus in commercial dairy goat farms in a hot region in Mexico. Trop Anim Health Prod 46:919–924
Borde G, Lowhar G, Adesiyun AA (2006) Toxoplasma gondii and Chlamydophila abortus in caprine abortions in Tobago: a sero-epidemiological study. J Vet Med B Infect Dis Vet Public Health 53:188–193
Pinheiro Junior JW, Mota RA, Piatti RM, Oliveira AA, da Silva AM, de Oliveira Abreu SR, Anderlini GA, Valença RM (2010) Seroprevalence of antibodies to Chlamydophila abortus in ovine in the State of Alagoas, Brazil. Braz J Microbiol 41:358–364
Villagra-Blanco R, Dolz G, Montero-Caballero D, Romero-Zúñiga JJ (2015) Detection of antibodies against Chlamydophila abortus in Costa Rican sheep flocks. Open Vet J 5:122–126
Di Paolo LA, Alvarado Pinedo MF, Origlia J, Fernández G, Uzal FA, Travería GE (2019) First report of caprine abortions due to Chlamydia abortus in Argentina. Vet Med Sci 5:162–167
Wang FI, Shieh H, Liao YK (2001) Prevalence of Chlamydophila abortus infection in domesticated ruminants in Taiwan. J Vet Med Sci 63:1215–1220
Bandyopadhyay S, Sasmal D, Biswas TK, Samanta I, Ghosh MK (2009) Serological evidence of antibodies against Chlamydophila abortus in free-ranging yak (Poephagus grunniens) in Arunachal Pradesh, India. Rev Sci Tech 28:1051–1055
Talafha AQ, Ababneh MM, Ababneh MM, Al-Majali AM (2012) Prevalence and risk factors associated with Chlamydophila abortus infection in dairy herds in Jordan. Trop Anim Health Prod 44:1841–1846
Chen Q, Gong X, Zheng F, Cao X, Li Z, Zhou J (2014) Seroprevalence of Chlamydophila abortus infection in yaks (Bos grunniens) in Qinghai, China. Trop Anim Health Prod 46:503–507
Qin SY, Yin MY, Cong W, Zhou DH, Zhang XX, Zhao Q, Zhu XQ, Zhou JZ, Qian AD (2014) Seroprevalence and risk factors of Chlamydia abortus infection in Tibetan sheep in Gansu province, northwest China. ScientificWorldJournal 2014:193464
Sun WW, Meng QF, Cong W, Shan XF, Wang CF, Qian AD (2015) Herd-level prevalence and associated risk factors for Toxoplasma gondii, Neospora caninum, Chlamydia abortus and bovine viral diarrhoea virus in commercial dairy and beef cattle in eastern, northern and northeastern China. Parasitol Res 114:4211–4218
Heidari S, Derakhshandeh A, Firouzi R, Ansari-Lari M, Masoudian M, Eraghi V (2018) Molecular detection of Chlamydophila abortus, Coxiella burnetii, and Mycoplasma agalactiae in small ruminants’ aborted fetuses in southern Iran. Trop Anim Health Prod 50:779–785
Hu SF, Li F, Zheng WB, Liu GH (2018) Seroprevalence and risk factors of Chlamydia abortus infection in goats in Hunan Province, Subtropical China. Vector Borne Zoonotic Dis 18:500–503
Iraninezhad Z, Azizzadeh M, Taghavi Razavizadeh A, Mehrzad J, Rashtibaf M (2020) Seroepidemiological feature of Chlamydia abortus in sheep and goat population located in northeastern Iran. Vet Res Forum Fall 11:423–426
Fayez M, Elmoslemany A, Alorabi M, Alkafafy M, Qasim I, Al-Marri T, Elsohaby I (2021) Seroprevalence and risk factors associated with Chlamydia abortus infection in sheep and goats in Eastern Saudi Arabia. Pathogens 10:489
Samkange A, Katsande TC, Tjipura-Zaire G, Crafford JE (2010) Seroprevalence survey of Chlamydophila abortus infection in breeding goats on commercial farms in the Otavi Veterinary District, northern Namibia. Onderstepoort J Vet Res 77:E1–E5
Hireche S, Ababneh MM, Bouaziz O, Boussena S (2016) Seroprevalence and molecular characterization of Chlamydia abortus in frozen fetal and placental tissues of aborting ewes in northeastern Algeria. Trop Anim Health Prod 48:255–262
Djellata N, Yahimi A, Hanzen C, Saegerman C, Kaidi R (2019) Prevalence and factors associated with a higher or lower risk of exposure to Coxiella burnetii, Chlamydia abortus and Toxoplasma gondii in dairy cows that have aborted in Algeria. Rev Sci Tech 38:761–786
Mamlouk A, Guesmi K, Ouertani I, Kalthoum S, Selmi R, Ben Aicha E, Bel Haj Mohamed B, Gharbi R, Lachtar M, Dhaouadi A, Seghaier C, Messadi L (2020) Seroprevalence and associated risk factors of Chlamydia abortus infection in ewes in Tunisia. Comp Immunol Microbiol Infect Dis 71:101500
Tesfaye A, Sahele M, Sori T, Guyassa C, Garoma A (2020) Seroprevalence and associated risk factors for chlamydiosis, coxiellosis and brucellosis in sheep and goats in Borana pastoral area, southern Ethiopia. BMC Vet Res 16:145
Alemayehu G, Mamo G, Alemu B, Desta H, Tadesse B, Benti T, Bahiru A, Yimana M, Wieland B (2021) Causes and flock level risk factors of sheep and goat abortion in three agroecology zones in Ethiopia. Front Vet Sci 8:615310
Selim A, Manaa EA, Waheed RM, Alanazi AD (2021) Seroprevalence, associated risk factors analysis and first molecular characterization of Chlamydia abortus among Egyptian sheep. Comp Immunol Microbiol Infect Dis 74:101600
Benaissa MH, Mimoune N, Youngs CR, Kaidi R, Faye B (2020) First report of Chlamydophila abortus infection in the dromedary camel (Camelus dromedarius) population in Eastern Algeria. Comp Immunol Microbiol Infect Dis 73:101557
Rodolakis A, Laroucau K (2015) Chlamydiaceae and chlamydial infections in sheep or goats. Vet Microbiol 181:107–118
Australian Department of Primary Industries. https://dpi.nsw.gov.au/about-us/services/laboratory-services/veterinary/chlamydiosis
West DM (2002) Ovine abortion in New Zealand. N Z Vet J 50:93–95
Harvey C (2019) Causes of bovine and ovine abortions diagnosed using PCR at Gribbles Veterinary laboratories 2016–2018. VetScript 5:48–50
Merdja S, Khaled H, Dahmani A, Bouyoucef A (2015) Chlamydial abortion in Algerian small ruminants. Bull Univ Agric Sci Vet Med Cluj-Napoca 72:23–26
Blumer S, Moestl K, Krametter-Froetscher R, Hässig M, Pospischil A, Borel N (2012) Influence of commune alpine pasturing on the seroconversion of Chlamydia abortus in the region of Vorarlberg. SAT, Schweizer Archiv für Tierheilkunde 154:13–17
Yin L, Schautteet K, Kalmar I, Bertels G, Van Driessche E, Czaplicki G, Borel N, Longbottom D, Frétin D, Dispas M, Vanrompay D (2014) Prevalence of Chlamydia abortus in Belgian ruminants. Vlaams Diergeneeskundig Tijdschrift 83:164–170
Lima AMC, Alves FSF, Pinheiro RR, Alves SM, de Farias DA, Andrioli A, Eloy AMX, dos Santos MD, Cardoso JFS, Paula NRO (2021) Risk factors associated with seroprevalence of Chlamydia abortus in sheep farms in Ceará. Brazil Acta Sci Vet 49:1784
Araújo JF, Pinheiro RR, Andrioli A, Alves FSF, Faccioli PY, Eloy AMX, dos Santos VWS, Peixoto RM, Cesar Lima AM (2018) Seroprevalence and risk factors of Chlamydophila abortus infection in goats of the state of Rio Grande do Norte. Brazil Acta Sci Vet 46:1592
Huang SY, Wu SM, Xu MJ, Zhou DH, Danba C, Gong G, Zhu XQ (2013) First record of Chlamydia abortus seroprevalence in Tibetan sheep in Tibet, China. Small Rumin Res 112:243–245
Spičic S, Račić I, Andrijanić M, Duvnjak S, Zdelar-Tuk M, Stepanić M, Cvetnić Z (2015) Emerging cases of chlamydial abortion in sheep and goats in Croatia and Bosnia and Herzegovina. Berl Munch Tierarztl Wochenschr 128:183–187
Selim A, Elhaig M, Moawed S (2018) A Serological survey of four abortifacient infectious agents among small ruminant in Egypt. Asian J Anim Vet Adv 13:114–121
Abnaroodheleh F, Emadi A, Dadar M (2021) Seroprevalence of brucellosis and chlamydiosis in sheep and hoats with history of abortion in Iran. Small Rumin Res 202:106459
Al-Qudah KM, Sharif LA, Raouf RY, Hailat NQ, Al-Domy FM (2004) Seroprevalence of antibodies to Chlamydophila abortus shown in Awassi sheep and local goats in Jordan. Vet Med 49:460–466
Elzlitne R, Elhafi G (2016) Seroprevalence of Chlamydia abortus in camel in the western region of Libya. J Adv Vet Anim Res 3:178–183
Benkirane A, Essamkaoui S, El Idrissi A, Lucchese L, Natale A (2015) A sero-survey of major infectious causes of abortion in small ruminants in Morocco. Vet Ital 51:25–30
Hussein MF, AlShaikh MA, El-Rab GMO, Aljumaah RS, Gar El Nabi AR, Abdel Bagi AM (2008) Serological prevalence of Q fever and Chlamydiosis in camels in Saudi Arabia. J Anim Vet Adv 7:685–688
Shabana II, Krimly RA (2020) Seroprevalence of some viral and bacterial zoonoses in domestic ruminants in Medina. J Adv Vet Anim Res 7:42–50
Adesiyun AA, Knobel DL, Thompson PN, Wentzel J, Kolo FB, Kolo AO, Conan A, Simpson GJG (2020) Sero-epidemiological study of selected zoonotic and abortifacient pathogens in cattle at a wildlife-livestock interface in South Africa. Vector Borne Zoonotic Dis 20:258–267
Díaz JM, Fernández G, Prieto A, Valverde S, Lago N, Díaz P, Panadero R, López C, Morrondo P, Díez-Baños P (2014) Epidemiology of reproductive pathogens in semi-intensive lamb-producing flocks in North-West Spain: a comparative serological study. Vet J 200:335–338
Borel N, Doherr MG, Vretou E, Psarrou E, Thoma R, Pospischil A (2004) Seroprevalences for ovine enzootic abortion in Switzerland. Prev Vet Med 65:205–216
Gokce HI, Kaçar C, Genç O, Sozmen M (2007) Seroprevalence of Chlamydophila abortus in aborting ewes and dairy cattle in north-east part of Turkey. Bull Vet Inst Pulawy 51:9–13
Nietfeld JC (2001) Chlamydial infections in small ruminants. Vet Clin North Am Food Anim Pract 17:301–314
Rodolakis A, Yousef Mohamad K (2010) Zoonotic potential of Chlamydophila. Vet Microbiol 140:382–391
Gupta S, Chahota R, Bhardwaj B, Priyanka P, Verma S, Sharma M (2014) Identification of chlamydiae and mycoplasma species in ruminants with ocular infections. Lett Appl Microbiol 60:135–139
Hoffmann K, Schott F, Donati M, Di Francesco A, Hässig M, Wanninger S, Sidler X, Borel N (2015) Prevalence of Chlamydial infections in fattening pigs and their influencing factors. PLoS One 10:e0143576
Jiménez D, Romero-Zuñiga JJ, Dolz G (2014) Serosurveillance of infectious agents in equines of the Central Valley of Costa Rica. Open Vet J 4:107–112
Baumann S, Gurtner C, Marti H, Borel N (2020) Detection of Chlamydia species in 2 cases of equine abortion in Switzerland: a retrospective study from 2000 to 2018. J Vet Diagn Invest 32:542–548
Pantchev A, Sting R, Bauerfeind R, Tyczka J, Sachse K (2010) Detection of all Chlamydophila and Chlamydia spp. of veterinary interest using species-specific real-time PCR assays. Comp Immunol Microbiol Infec Dis 33:473–484
Szymańska-Czerwińska M, Mitura A, Niemczuk K, Zaręba K, Jodełko A, Pluta A, Scharf S, Vitek B, Aaziz R, Vorimore F, Laroucau K, Schnee C (2017) Dissemination and genetic diversity of chlamydial agents in Polish wildfowl: isolation and molecular characterisation of avian Chlamydia abortus strains. PLoS One 12:e0174599
Origlia JA, Cadario ME, Frutos MC, Lopez NF, Corva S, Unzaga MF, Piscopo MV, Cuffini C, Petruccelli MA (2019) Detection and molecular characterization of Chlamydia psittaci and Chlamydia abortus in psittacine pet birds in Buenos Aires Province, Argentina. Rev Argent Microbiol 51:130–135
Szymańska-Czerwińska M, Mitura A, Zaręba K, Schnee C, Koncicki A, Niemczuk K (2017) Poultry in Poland as Chlamydiaceae carrier. J Vet Res 61:411–419
Li Z, Liu P, Cao X, Lou Z, Zaręba-Marchewka K, Szymańska-Czerwińska M, Niemczuk K, Hu B, Bai X, Zhou J (2018) First report of Chlamydia abortus in farmed fur animals. Biomed Res Int 2018:4289648
Li Z, Cao X, Fu B, Chao Y, Cai J, Zhou J (2015) Identification and characterization of Chlamydia abortus isolates from Yaks in Qinghai. China. Biomed Res Int 2015:658519
Qin SY, Huang SY, Yin MY, Tan QD, Liu GX, Zhou DH, Zhu XQ, Zhou JZ, Qian AD (2015) Seroprevalence and risk factors of Chlamydia abortus infection in free-ranging White Yaks in China. BMC Vet Res 11:8
Liang L, Wen Y, Li Z, Liu P, Liu X, Tan S, Liu D, Zhou J, Tong D (2021) Seroprevalence of Chlamydia abortus infection in yak (Bos grunniens) in Tibet. China Ir Vet J 74:19
Tavernier P, Sys SU, De Clercq K, De Leeuw I, Caij AB, De Baere M, De Regge N, Fretin D, Roupie V, Govaerts M, Heyman P, Vanrompay D, Yin L, Kalmar I, Suin V, Brochier B, Dobly A, De Craeye S, Roelandt S, Goossens E, Roels S (2015) Serologic screening for 13 infectious agents in roe deer (Capreolus capreolus) in Flanders. Infect Ecol Epidemiol 5:29862
Santoro M, Iaccarino D, Di Nocera F, Degli Uberti B, Lucibelli MG, Borriello G, De Luca G, D’Amore M, Cerrone A, Galiero G (2019) Molecular detection of Chlamydia abortus in a stranded mediterranean striped dolphin Stenella coeruleoalba. Dis Aquat Organ 132:203–208
Di Francesco A, Donati M, Nicoloso S, Orlandi L, Baldelli R, Salvatore D, Sarli G, Cevenini R, Morandi F (2012) Chlamydiosis: seroepidemiologic survey in Red Deer (Cervus elaphus) population in Italy. J Wildl Dis 48:488–491
Sachse K, Kuehlewind S, Ruettger A, Schubert E, Rohde G (2012) More than classical Chlamydia psittaci in urban pigeons. Vet Microbiol 157:476–480
Mattmann P, Marti H, Borel N, Jelocnik M, Albini S, Vogler BR (2019) Chlamydiaceae in wild, feral and domestic pigeons in Switzerland and insight into population dynamics by Chlamydia psittaci multilocus sequence typing. PLoS One 14:e0226088
Vogler BR, Trinkler M, Marti H, Borel N, Pesch T, Prähauser B, Hoop R, Mattmann P, Albini S (2019) Survey on Chlamydiaceae in cloacal swabs from Swiss turkeys demonstrates absence of Chlamydia psittaci and low occurrence of Chlamydia gallinacean. PLoS One 14:e0226091
Thierry S, Vorimore F, Rossignol C, Scharf S, Sachse K, Berthon P, Durand B, Virlogeux-Payant I, Borel N, Laroucau K (2016) Oral uptake of Chlamydia psittaci by Ducklings results in systemic dissemination. PLoS One 11:e0154860
Vorimore F, Thébault A, Poisson S, Cléva D, Robineau J, de Barbeyrac B, Durand B, Laroucau K (2015) Chlamydia psittaci in ducks: a hidden health risk for poultry workers. Pathog Dis 73:1–9
Stalder S, Marti H, Borel N, Sachse K, Albini S, Vogler BR (2020) Occurrence of Chlamydiaceae in raptors and crows in Switzerland. Pathogens 9:724
van Loock M, Vanrompay D, Herrmann B, Vander Stappen J, Volckaert G, Goddeeris BM, Everett KDE (2003) Missing links in the divergence of Chlamydophila abortus from Chlamydophila psittaci. Int J Syst Evol Microbiol 53:761–770
Madani SA, Peighambari SM (2013) PCR-based diagnosis, molecular characterization and detection of atypical strains of avian Chlamydia psittaci in companion and wild birds. Avian Pathol 42:38–44
Aaziz R, Gourlay P, Vorimore F, Sachse K, Siarkou VI, Laroucau K (2015) Chlamydiaceae in North Atlantic seabirds admitted to a wildlife rescue center in Western France. Appl Environ Microbiol 81:4581–4590
Luján-Vega C, Hawkins MG, Johnson CK, Briggs C, Vennum C, Bloom PH, Hull JM, Cray C, Pesti D, Johnson L, Ciembor P, Ritchie BR (2018) Atypical Chlamydiaceae in wild populations of hawks (Buteo spp.) in California. J Zoo Wildl Med 49:108–115
Zaręba-Marchewka K, Szymańska-Czerwińska M, Livingstone M, Longbottom D, Niemczuk K (2021) Genome sequencing and comparative genome analyses of Chlamydia abortus strains of avian origin suggests that Chlamydia abortus species should be expanded to include avian and mammalian subgroups. Pathogens 10:1405
Staub E, Marti H, Biondi R, Levi A, Donati M, Leonard CA, Ley SD, Pillonel T, Greub G, Seth-Smith HMB, Borel N (2018) Novel Chlamydia species isolated from snakes are temperature-sensitive and exhibit decreased susceptibility to azithromycin. Sci Rep 8:5660
Wheelhouse N, Sait M, Gidlow J, Deuchande R, Borel N, Baily J, Caldow G, Longbottom D (2011) Molecular detection of Chlamydia-like organisms in cattle drinking water. Vet Microbiol 152:196–199
Codony F, Fittipaldi M, López E, Morató J, Agustí G (2012) Well water as a possible source of Waddlia chondrophila infections. Microbes Environ 27:529–532
Corsaro D, Müller KD, Wingender J, Michel R (2013) “Candidatus Mesochlamydia elodeae” (Chlamydiae: Parachlamydiaceae), a novel chlamydia parasite of free-living amoebae. Parasitol Res 112:829–838
Croxatto A, Rieille N, Kernif T, Bitam I, Aeby S, Péter O, Greub G (2014) Presence of Chlamydiales DNA in ticks and fleas suggests that ticks are carriers of Chlamydiae. Ticks Tick Borne Dis 5:359–365
Hokynar K, Sormunen JJ, Vesterinen EJ, Partio EK, Lilley T, Timonen V, Panelius J, Ranki A, Puolakkainen M (2016) Chlamydia-like organisms (CLOs) in finnish Ixodes ricinus ticks and human skin. Microorganisms 4:28
Pilloux L, Aeby S, Gaümann R, Burri C, Beuret C, Greub G (2015) The high prevalence and diversity of Chlamydiales DNA within Ixodes ricinus ticks suggest a role for ticks as reservoirs and vectors of Chlamydia-related bacteria. Appl Environ Microbiol 81:8177–8182
Pospischil A, Kaiser C, Hofmann-Lehmann R, Lutz H, Hilbe M, Vaughan L, Borel N (2012) Evidence for Chlamydia in wild mammals of the Serengeti. J Wildl Dis 48:1074–1078
Bhandi S, Pfukenyi DM, Matope G, Murondoti A, Tivapasi M, Ndengu M, Scacchia M, Bonfini B, De Garine-Wichatitsky M (2019) Brucellosis and Chlamydiosis seroprevalence in goats at livestock-wildlife interface areas of Zimbabwe. Onderstepoort J Vet Res 86:e1–e9
Wu JY, Li JJ, Wang DF, Wei YR, Meng XX, Tuerxun G, Bolati H, Liu KK, Muhan M, Shahan A, Dilixiati D, Yang XY (2020) Seroprevalence of five zoonotic pathogens in wild ruminants in Xinjiang, Northwest China. Vector Borne Zoonotic Dis 20:882–887
Kramer A, Schwebke I, Kampf G (2006) How long do nosocomial pathogens persist on inanimate surfaces? A systematic review BMC Infect Dis 6:130
Seaman JT (1985) Chlamydia isolated from abortion in sheep. Aust Vet J 62:436
Acknowledgements
LT and SS are financed by the University of Milan (Italy), MR is supported by the Scottish Government’s Rural and Environmental Science and Analytical Services Division (RESAS), and NW is funded by Edinburgh Napier University through Scottish Funding Council. The content is entirely under responsibility of the authors and does not necessarily represents the official views of the Institutions/founders.
Author information
Authors and Affiliations
Contributions
LT, SS, NW and MSR wrote, edited and reviewed the manuscript. Each of the co-authors examined the published studies independently before discussing and critically evaluating specific points. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Epidemiological studies reporting animal species and prevalence rate of global spread of Chlamydia abortus according to the currently available data. The represented distribution is likely to be underestimated in comparison with the actual prevalence of C. abortus, both because of the small amount of data available globally and because of the variable specificity of the tests available for the detection of C. abortus.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Turin, L., Surini, S., Wheelhouse, N. et al. Recent advances and public health implications for environmental exposure to Chlamydia abortus: from enzootic to zoonotic disease. Vet Res 53, 37 (2022). https://doi.org/10.1186/s13567-022-01052-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13567-022-01052-x