Abstract
Background
Rare diseases pose immense challenges for healthcare systems due to their low prevalence, associated disabilities, and attendant treatment costs. Advancements in gene therapy, such as treatments for Spinal Muscular Atrophy (SMA), have introduced novel therapeutic options, but the high costs, exemplified by Zolgensma® at US$2.1 million, present significant financial barriers. This scoping review aimed to compare the funding approaches for rare disease treatments across high-performing health systems in Australia, Singapore, South Korea, the United Kingdom (UK), and the United States (US), aiming to identify best practices and areas for future research.
Methods
In accordance with the PRISMA-ScR guidelines and the methodological framework by Arksey and O’Malley and ensuing recommendations, a comprehensive search of electronic databases (Medline, EMBASE, and Cochrane) and grey literature from health department websites and leading national organizations dedicated to rare diseases in these countries was conducted. Countries selected for comparison were high-income countries with advanced economies and high-performing health systems: Australia, Singapore, South Korea, the UK, and the US. The inclusion criteria focused on studies detailing drug approval processes, reimbursement decisions and funding mechanisms, and published from 2010 to 2024.
Results
Based on a thorough review of 18 published papers and grey literature, various strategies are employed by countries to balance budgetary constraints and access to rare disease treatments. Australia utilizes the Life Saving Drugs Program and risk-sharing agreements. Singapore depends on the Rare Disease Fund, which matches public donations. South Korea’s National Health Insurance Service covers specific orphan drugs through risk-sharing agreements. The UK relies on the National Institute for Health and Care Excellence (NICE) to evaluate treatments for cost-effectiveness, supported by the Innovative Medicines Fund. In the US, a combination of federal and state programs, private insurance and non-profit support is used.
Conclusion
Outcome-based risk-sharing agreements present a practical solution for managing the financial strain of costly treatments. These agreements tie payment to actual treatment efficacy, thereby distributing financial risk and promoting ongoing data collection. Countries should consider adopting and expanding these agreements to balance immediate expenses with long-term benefits, ultimately ensuring equitable access to crucial treatments for patients afflicted by rare diseases.
Similar content being viewed by others
Introduction
A rare disease is characterized by its low prevalence within the population. In the United States (US), a disease is classified as rare if it impacts fewer than 200,000 individuals [1]. In contrast, Japan sets this threshold at 50,000 individuals, while Australia defines a rare disease as one affecting fewer than 2,000 individuals. These criteria generally correspond to prevalences ranging from 1 to 8 per 10,000 people [2]. Singapore’s definition specifies a rare disease as one affecting less than one in 2,000 patients [3]. A significant number of rare diseases lead to fatal outcomes, and the majority have their roots in genetics, stemming from mutations in genes or chromosomes [4].
Previously, many of these rare diseases had only symptom-relieving treatments [5]; today, with the advent of gene therapy, large strides have been made with novel treatments that significantly improve one’s quality of life [6]. Using the example of Spinal Muscular Atrophy (SMA), which if left untreated, progressively weakens muscles and can lead to severe physical disabilities and death [7]. For a long time, Risdiplam stood as the treatment of choice for SMA. For those undergoing this treatment, it necessitates a daily oral regimen that extends throughout their lifetime [8]. In Singapore, the average annual cost of Risdiplam in public healthcare institutions is approximately S$375,000 [8]. There are no further subsidies by the Singaporean government and SMA treatment is not currently covered by the Rare Disease Fund (RDF). Since April 2023, Zolgensma® has been approved by local Health Sciences Authority (HSA) under the Register of Class 2 Cell, Tissue or Gene Therapy Products for use in Singapore [9]. Zolgensma®, however, costs around US$2.1 million per dose [10], and the staggering cost poses an immense financial barrier for the vast majority of patients and their families [11]. In the US and the United Kingdom (UK)/European Union (EU), Spinraza® (nusinersen) was the first approved drug for SMA [12], and its approval set a precedent for subsequent SMA treatments, including Zolgensma®, which was mostly recommended for reimbursement as an alternative.
The rarity and high cost of these treatments pose unique challenges for healthcare policy and funding. Policymakers must balance the ethical imperative to provide access to life-saving treatments with the practical constraints of healthcare budgets. Different countries have adopted various strategies to manage these challenges. For example, Australia utilizes the Life Saving Drugs Program (LSDP) and risk-sharing agreements [13], while Singapore relies on a rare disease fund that matches public donations [2]. South Korea’s National Health Insurance Service (NHIS) covers certain orphan drugs based on cost-effectiveness analyses [14], the UK employs the National Institute for Health and Care Excellence (NICE) to evaluate treatments for cost-effectiveness [15], and the US combines federal and state programs with private insurance and non-profit support [16].
This scoping review thus aimed to compare and contrast the approaches to funding rare disease treatments across high-performing health systems in Australia, Singapore, South Korea, the UK, and the US. By examining the existing policies, approval processes, and reimbursement mechanisms in these countries, this review seeks to identify best practices, learning points and potential areas for improvement in ensuring equitable access to treatment for patients with rare diseases. In addressing rare diseases, it is crucial to establish a suitable financing structure to avoid creating a schism between families who can afford these treatments and those who cannot. This also raises a parallel question on whether the price of rare disease therapies is justified, and how health systems can provide equitable treatment access for all patients, regardless of the rarity of their condition and the cost of treatment.
Methods
Country selection
To ensure a comparable assessment, countries with similar high-income status (based on the World Bank Group country classification) were chosen [17]. The countries selected for comparison were: Australia, Singapore, South Korea, the UK and the US. These are all countries with advanced economies, high-income economy with a high GDP per capita [17], and with high-performing health systems. Low- and middle-income countries (LMICs) were not sampled as formal health technology assessment is typically lacking or limited in these settings [18].
Search strategy
This scoping review protocol adhered to the PRISMA-ScR (Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews) guidelines [19] and the methodological framework outlined by Arksey and O’Malley [20], as well as further recommendations made by Levac et al. [21]. To this end, a comprehensive search, encompassing both electronic databases and internet-based sources, was performed independently by five authors (CO, KEC, TSKO, IJXL and ASPT), with any discrepancies resolved by the senior author (QXN).
Electronic database search
Using combinations of relevant key words including ‘orphan disease’, ‘rare disease’ and ‘orphan drugs’, we searched Medline, EMBASE, and Cochrane databases for studies published up to 31 May 2024. The full search strategy is displayed in the supplementary (Table S1). The search focused on published original research articles, reviews, policy papers, and government reports related to rare disease funding and policy. Inclusion criteria encompassed studies that detailed drug approval processes, reimbursement decisions and funding mechanisms in the five high-income countries (Australia, Singapore, South Korea, the UK and US), and published in the last decade (published during or after 2010) to ensure it covers recent policy changes. Exclusion criteria included non-English studies and editorial/opinion pieces lacking substantial data.
Internet-based search
In addition to the database search, grey literature was searched via the health department websites of these five countries (Australia, Singapore, South Korea, the UK, and US) to source government reports and monographs related to rare disease policy and funding. Following this, the websites of leading national organizations dedicated to rare diseases in each country were also screened to gather more reports. The main internet sources used for data collection are listed in Table 1. The search terms employed included ‘rare diseases’ or ‘orphan diseases’ along with related phrases (such as ‘specialized care’, ‘health policy’, ‘patient advocacy’, ‘treatment access’, ‘healthcare quality’, and ‘government support’), linked by the conjunction ‘or’. The review encompassed reports published up to 31 January 2024, limited to documents published in English or translatable to English using web Google translate. The translation pertained to documents in Korean, and the Google translation was cross-checked with ChatGPT and also manually verified by a native speaker of the language.
Scope of review
Given the intricacies within the rare disease policy ecosystem, the analysis was confined to the processes of listing and reimbursing orphan drugs, as well as any special funding mechanisms available for such drugs. Hence, government initiatives focusing on advancing research and development (R&D) for new orphan drugs, elevating awareness and diagnostic capabilities for rare diseases, and the influence of rare disease advocacy groups’ social and political capital were not within the scope of this discussion.
Data analysis and synthesis
The narrative synthesis approach was chosen as it allowed for a flexible yet rigorous analysis of the diverse study types and reporting, accommodating the broad range of research and policy documents included in our scoping review. Briefly, the data analysis and synthesis process were rooted in best practices for narrative synthesis, as outlined by Popay et al. [22], as we attempted to integrate findings from individual studies to produce a cohesive interpretation. This process began with a preliminary synthesis, forming an initial understanding of the data. We then explored relationships within and between reports to identify patterns, trends, and differences. This exploration included grouping studies by methodology, outcomes, and specific aspects of rare disease funding policies.
Results
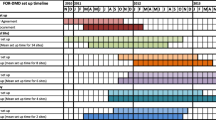
From an initial search of Medline, Embase and Cochrane database, 5762 articles were found. After removal of 616 duplicates, 5146 articles were assessed in the title and abstract sieve. A total of 169 studies were eventually sought for full-text screening, resulting in a final selection of 18 articles for this study [23,24,25,26,27,28,29,30,31,32,33,34,35,36,37,38,39,40]. All studies were published from 2011 to 2023. The search and abstraction process are illustrated in Fig. 1, and the key study findings are summarised in Table 2.
After reviewing the internet-based sources, the salient features and comparison for the countries reviewed are holistically considered and summarised in Table 3.
Australia
A national single-payer funding system, Medicare serves as the publicly funded universal health insurance scheme in Australia, supplemented by the Pharmaceutical Benefits Scheme (PBS), which aids in covering expenses for certain medications and treatments [41]. The Pharmaceutical Benefits Advisory Committee (PBAC), an independent expert body appointed by the government, employs specific criteria, including cost-effectiveness, to assess a medicine’s eligibility for inclusion in the PBS [41]. While the consideration of cost-effectiveness is pivotal for managing budgets, it poses a challenge in evaluating drugs for rare diseases due to their limited evidence base on effectiveness and higher pricing, influenced by extensive research costs and reduced competition in smaller markets [42]. Accordingly, Australia established the LSDP in 1995 as a complementary initiative to the PBS. The LSDP aims to broaden access to high-cost drugs intended for treating rare diseases, acknowledging the unique challenges posed by such medications within the healthcare landscape. As of 2023, 17 medicines are subsidised via the LSDP [13].
Risk-sharing agreements are commonly used by the PBS and LSDP to manage certain risks and uncertainties with new orphan drugs. Sponsors may voluntarily propose risk-sharing agreements with are captured through a legal deed of agreement that is negotiated between the sponsor and the Government. Some financial risk share agreements can be class deeds where sponsors share the risk based on market share. While such mutual agreements remain confidential, the majority of agreements are likely to be financial-based agreements which include price-volume, rebate or discount-based schemes [43]. However, a hybrid of financial and outcome-based agreements is also possible [44].
Specifically, for the LSDP however, the usage of outcome-based risk-sharing agreements are referenced [45]. These agreements allow funding under the condition that ongoing data collection assesses the drug’s impact on the disease. Price adjustments might occur if emerging data suggests the drug’s efficacy differs from initial assumptions. In the past, LSDP mirrored PBS by implementing a policy to progressively reduce medicine prices on specific listing anniversaries [46]. However, as of June 2022, this policy within LSDP has been discontinued [47]. For orphan drugs under the LSDP, periodic reviews 24 months post-listing remain a crucial aspect of assessing medication usage, clinical benefits, and financial impacts [45]. Recommendations post-review may involve modifying eligibility criteria, adjusting risk-sharing arrangements, altering data collection scopes, referring the medication to PBAC for PBS listing consideration, or even removing it from the LSDP listing [45].
In 2022, Zolgensma® was approved for SMA by listing under the PBS, saving approximately 20 patients AUS$ 2.5 million [48]. In the following year, the scheme was expanded to include pre-symptomatic babies as well, thus extending the subsidy to an additional 15 babies [49]. A cost-minimisation approach was taken, where PBS received a substantial unlisted discount from the sponsor [50]. An outcome-based risk sharing agreement was also established, which encompassed an unspecified rebate on the cost over at least 5 years, following circumstances of a patient’s death and the failure to meet certain developmental milestones [51].
Singapore
In January 2018, the Singapore government began mulling over the possibility of establishing a separate fund to better support children with rare diseases and their families [52]. Policy discussions culminated in the creation of the RDF, launched in July 2019, to fund five medicines used for the treatment of three rare disease conditions [3]. With an initial endowment of S$70 million, the charity fund operates by combining government-matching contributions with community donations: for every S$1 donated by the public, the government contributes S$3 (3-to-1 matching). According to the then Senior Minister of State for Health, Mr Edwin Tong, the donation matching approach was adopted to galvanise the larger community to “jointly support these patients and their families as part of our caring and inclusive society” [53]. The policy’s focus on collective action and shared responsibility mirrors the core principles of the “Many Helping Hands” approach, a community-based framework that encourages collaboration among stakeholders to address social welfare issues [54].
Although the RDF’s initial focus was directed towards five specific treatments, its non-restrictive framework allows for future expansion to include a wider range of conditions and therapies. In November 2019, the RDF was expanded to cover Pompe disease, a rare inherited neuromuscular disorder where patients can incur medical expenses exceeding S$500,000 each year [55]. Two years later, the RDF was extended to support the treatment of Mucopolysaccharidosis Type VI as well [56]. As of 2023, the RDF covers five conditions and seven medications [3], and has helped relieve the medical financial burden of nine Singaporean patients [57]. It is important to note that the scope of the RDF caters to a relatively small percentage of families requiring additional financial assistance for high-cost treatments. Other avenues, such as Medisave, MediShield Life, and MediFund [58], exist to assist the majority of individuals with rare diseases by covering treatments and medical bills. However, the extent of financial support available through these avenues for such individuals remains limited and subjected to annual caps.
As of the conclusion of the fiscal year 2022, the RDF had a reported total of S$143 million [59]. There have been numerous calls to expand the scope of the RDF to cover more illnesses. In 2021, Member of Parliament Cheryl Chan called for the RDF to be extended to cover the treatment of Neuroblastoma and Krabbe disease, which are among the 10 most common rare diseases afflicting young children in the world [60]. She further added that patients with rare diseases outside the list of approved conditions and medication, unfortunately, face nothing but “the strictest of processes and a flat rejection”. While there remains a strong desire and momentum to support life-saving treatments for various rare diseases, the truth is that the healthcare financing system “is not designed to support such high-cost treatments” [60]. The government’s position, as explained in a Parliamentary reply, is that increasing donations, particularly from high-net-worth individuals, foundations, and corporate sponsors, remains the key approach to securing additional funds for patients and their families [61].
South Korea
In South Korea, healthcare revolves around the NHIS, a public insurance program managed by the Ministry of Health and Welfare [62]. South Koreans with adequate income contribute to insure themselves and their dependents in this single-payer system. Introduced in 2000, the Mandatory Designation System necessitates all hospitals and clinics to be designated medical care institutions, obligated to provide services to participants in the NHIS, encompassing nearly the entire population [63]. South Korea made a pivotal shift in its National Health Insurance (NHI) drug reimbursement system in 2007, transitioning from a negative to a positive listing approach [14]. Post 2007, only drugs with confirmed cost-effectiveness became eligible for reimbursement. As a result of this change, obtaining reimbursement for orphan drugs where statistically verifying clinical outcomes is challenging, became more arduous. Between 2007 and 2020, South Korea saw the launch and approval of 168 orphan drugs, with 94 of them making it onto the reimbursement formulary [64].
When considering reimbursement pathways for orphan drugs without alternatives, three potential pathways exist. The pharmacoeconomic evaluation exemption pathway was introduced since May 2015 to improve patient accessibility for anticancer and orphan drugs [29]. For orphan drugs classified as essential drugs (ED) or falling under pharmacoeconomic waiver (PEW) categories, submission of a pharmacoeconomic study is not necessary. Instead, these drugs can be listed by referencing the listed prices of the same drug in the A7 countries (which includes the US, the UK, Italy, Germany, Japan, Switzerland, and France). For ED drugs, the average adjusted price in the A7 country sets the reimbursable price, while for PEW drugs, it is the lowest price among the adjusted A7 country prices [14]. ED classification hinges on meeting four criteria: alternative availability, disease severity, patient count, and clinical efficacy. As for PEW drugs, they must simultaneously demonstrate clinical necessity, and evidence challenges, and be listed in over three A7 countries to qualify. The risk-sharing agreement (RSA) pathway is specifically designated for anticancer drugs and orphan drugs lacking alternatives or therapeutically equivalent options [14]. However, within this subset, only those drugs addressing life-threatening critical diseases are eligible to pursue the RSA route. In each pathway, the price for reimbursement gets decided by a committee at the Health Insurance Review and Assessment Service (HIRA), where price negotiation with the NHIS to agree on its budget impact ensues [65]. At present, no special fund for rare disease medications exists in South Korea, although some conditions and drugs are covered under the NHIS [66].
Specific to Zolgensma®, authorities in South Korea studied the results of the available clinical trials and found convincing long-term therapeutic effect that was maintained more than seven years after once dose administration of Zolgensma® [67]. As such, since August 2022, the drug Zolgensma® is covered under the NHIS and patients who require it only have to pay 5.98 million won (around US$4400) despite the drug’s marketed price of 2 billion won (around US$1.5 million) [68]. Patients who receive the drug must consent to a five-year follow-up for regular evaluations of response as part of the government’s effort to continually re-evaluate the usefulness and cost-effectiveness of insured drugs.
United Kingdom
The National Health Service (NHS) stands as the UK’s publicly funded healthcare system, operating on the core principles of universality and free access to care for all, regardless of nationality or immigration status [69]. As a single-payer system, it covers primary, emergency, and compulsory healthcare at no cost to individuals. Within the NHS framework, the NICE evaluates health technologies based on evidence-based assessments of their effectiveness, safety, and cost-effectiveness. NICE’s role is to ascertain if proposed healthcare expenditures within the NHS offer superior value compared to alternative treatments. Their evaluation involves analysing the cost and benefit of new treatments relative to existing ones, often considering interventions costing less than £20,000 per Quality-Adjusted Life Year (QALY) as cost-effective, allowing some flexibility up to £30,000 per QALY [70]. Notably, once NICE approves a treatment, the NHS is mandated to provide funding for it.
Specific to rare diseases, gaining approval for expensive orphan drugs often faces hurdles due to insufficient evidence for smooth endorsement by the NICE. In 2021, England’s Rare Disease Framework aimed to address this inequality by refining the technology approval process [71]. The changes within the Highly Specialised Technologies (HST) Programme give more weight to health benefits in severe conditions, offer flexibility when evidence generation is challenging, and offer a higher cost-effectiveness threshold of £300,000 per QALY [72]. However, typically, “no more than 300 people in England are eligible for the technology in its licensed indication and no more than 500 across all its indications”, and there should be no other drug options for patients [73]. NICE also considers ‘severity modifiers’ in its appraisals, whereby if the absolute QALY shortfall or proportional QALY shortfall scores are high enough, a QALY weight is applied, effectively increasing the cost-effectiveness threshold [74].
Additionally, the Innovative Medicines Fund (IMF), modelled on the reformed Cancer Drugs Fund (CDF), supports early access to promising treatments for any condition, including rare diseases [15]. With a £340 million annual grant, the IMF provides interim funding for drugs with uncertain clinical and cost-effectiveness. Data collection via trials and studies aims to fill evidence gaps. Negotiations on pricing occur within a value-based framework to strive for cost-effectiveness [75]. However, drugs not deemed superior or cost-effective compared to existing treatments during this evaluation may not receive additional funding. Manufacturers would then bear the financial responsibility for patient access if NICE does not recommend the drug [76]. The approach, though the timeline of patient funding is uncertain, seeks to incentivise high-risk, potentially breakthrough treatments by attracting innovative manufacturers to invest in substantial therapeutic advancements.
Zolgensma®’s successful listing as a subsidised drug under the NHS in 2021 served as the inspiration for the creation of the IMF [77]. A confidential commercial discount was agreed upon, which potentially lowered the Incremental Cost Effectiveness Ratio (ICER), allowing Zolgensma® to be approved under the HST Programme. An outcome-based risk-sharing agreement was set up, linking payment for the drug to substantial clinical advancements. The payment spans five years, and if the therapy falls short of delivering expected clinical outcomes, a partial refund will be issued [78].
United States
The US’s approach involves a combination of federal and state programs, private insurance, pharmaceutical company initiatives, and non-profit organizations. A signature initiative is the Orphan Drug Act of 1983, which was signed into law and allows the FDA to grant certain drugs or biological products an orphan drug designation [16]. This provides incentives such as tax credits for clinical research, grant funding, assistance in clinical research design, and seven years of market exclusivity upon drug approval for drugs used to treat rare (or orphan because they have been typically neglected) diseases [32], although some have criticized this to be overly lucrative for drug manufacturers [79]. The US National Institutes of Health (NIH), particularly through the National Center for Advancing Translational Sciences (NCATS) and its Office of Rare Diseases Research (ORDR), also plays a significant role in funding and conducting research on rare diseases. The Rare Diseases Clinical Research Network is an initiative that involves collaboration between the NIH, patient advocacy groups, and clinical researchers. Suffice to say, all these efforts ensure constant innovation and a steady pipeline of drug development to change the disease course of rare disease sufferers.
In the US, private health insurance is a major contributor to covering the costs of treatments, including those for rare diseases [80]. However, coverage and out-of-pocket costs can vary significantly and the health systems can be challenging to navigate. An analysis of out-of-pocket spending on orphan drugs from 2013 to 2018 also found an increasing trend (almost doubling from 2013 to 2018) and a higher burden on payers and families despite private insurance coverage [80]. Parents and guardians of children with SMA have also reflected drawn out processing coverage decisions by insurance companies, a lack of transparency in the claims and preauthorization processes and being dependent on employment insurance for coverage [81].
In terms of government-funded health insurance programs (Medicaid and Medicare), they provide coverage for certain individuals, including those with disabilities and the elderly. They may cover some treatments for rare diseases, depending on the state and specific policy details. In particular, the Affordable Care Act (ACA), also known as Obamacare, has provisions that impact rare disease patients, such as prohibiting insurance companies from denying coverage due to pre-existing conditions, which includes many rare diseases [82]. However, entry criteria for Medicaid relies on family income and assets that varies from one state to another [83].
Also worth mention is the numerous non-profit organizations in the US that provide support for rare disease research and advocate for patients [84]. These organizations often fundraise to support research, increase awareness, and assist patients with accessing and affording treatments.
Discussion
Comparing these high-performing countries’ approaches to rare disease funding reveals a fine balancing act between creating patient access and weighing budgetary impacts. While some countries have well-documented policies and reimbursement mechanisms for rare diseases, others lack detailed studies on the effectiveness and sustainability of their funding models. Identifying these gaps would help to direct future research efforts towards areas that require additional investigation. Singapore’s approach resembles South Korea’s practice of exempting certain orphan drugs from cost-effectiveness analysis. There are shared challenges in conducting such analyses for high-cost, rare disease drugs given the infrequency of rare diseases. However, Singapore’s system, unlike South Korea’s, appears slow in adding drugs to its whitelist and lacks a transparent benchmark for selecting orphan drugs within its RDF. Internationally, countries like Australia, the UK, and South Korea also utilize distinct risk-sharing agreements, which Singapore’s framework does not currently emulate. Additionally, the RDF’s reliance on public goodwill and donations admittedly creates funding instability, and the absence of an early access mechanism or a real-world data monitoring system for orphan drugs prolongs approval processes, contrasting with practices elsewhere. This would inadvertently result in inequities, particularly for patients with non-listed rare diseases. Similarly, in the US, the fragmented healthcare system results in varied access and high out-of-pocket costs, despite robust research funding and the Orphan Drug Act providing incentives for drug development.
To address the high costs (and current uncertain long-term efficacy) of treatments for rare diseases like SMA, countries can benefit from implementing risk-sharing agreements with pharmaceutical companies. An important driver for uncertainty is the sustainability of remission, as it could range from 1 year to life-long effects. A risk-sharing agreement approach involves the government or healthcare providers negotiating with drug manufacturers to agree on terms that link the payment for the drugs to their performance in the real world or to specific outcomes. Given the paucity of long-term effectiveness data for treatments for rare diseases, making future payments conditional on the actual health outcomes and cost savings achieved would be a financially prudent approach for governments. Moreover, a recent study conducted found that pharmaceutical manufacturers and public payers had high interest in outcomes-based agreements and understood their role in facilitating timely market access for patients in need, provided that they are carefully designed to ensure value [85].
The core advantage of this model lies in its potential to make expensive therapies more accessible while managing financial risks. These agreements can be structured in various ways, such as paying for a drug only if it meets certain efficacy benchmarks or spreading the cost over time based on continued patient benefit. This strategy aligns the interests of public healthcare systems, patients, and pharmaceutical companies, ensuring that payment is contingent on the actual value provided by the treatment. Moreover, a payment-by-instalment method, which has been contemplated elsewhere, helps to spread the cost of these high-priced therapies over a period of time, thereby easing the immediate impact on healthcare budgets [86].
Such arrangements are not new, and outcome-based rates, tied to short- and long-term outcomes of patients post-treatment, have been successfully established for other high-cost gene therapies in the US and elsewhere [87]. In fact, risk-sharing agreements to mitigate investment risk for high-cost drugs are growing at an annual rate of 24% since 2012 [88]. Such agreements also benefit from the involvement of various stakeholders such as patients, healthcare providers, payers, policymakers, and manufacturers. In the case of Zolgensma®, a risk-sharing agreement could involve initial partial payment, with subsequent payments contingent upon the drug demonstrating a certain level of effectiveness in patients. Similar to the South Korean approach [28], such agreements also encourage pharmaceutical companies to invest in long-term studies and data collection to validate the effectiveness of their products.
Nonetheless, outcome-based pricing shifts some financial risks to drug manufacturers, who may only receive full payment upon proven effectiveness of the treatment. This risk might lead to higher initial pricing or reluctance from manufacturers to engage in further research and development of therapeutics for other rare diseases. Likewise, outcome-based pricing models require certain alterations in traditional healthcare insurance practices, which may be resistant to change due to established protocols and risk aversion. Defining reasonable outcomes that accurately reflect the effectiveness of the treatment can also be a challenge, especially when it comes to gene therapies where studies are still ongoing and long-term effects are not yet fully understood. The added administrative burden for healthcare providers and insurers to keenly track and monitor patient outcomes could also potentially impede the overall efficiency of the healthcare system [89].
Despite these challenges, the potential benefits of risk-sharing agreements in managing the financial burden of expensive rare disease treatments make them a compelling option for most high-performing health systems. They offer a pragmatic approach to balancing cost, access and innovation in healthcare. For the future, countries should also share best practices and data across borders as this can enhance global understanding of rare disease management and funding. Collaborative efforts can better drive innovation and harmonize approval and reimbursement processes, benefiting patients worldwide.
Limitations
Despite performing a comprehensive literature search across multiple databases and grey literature sources, there are some shortcomings to the present scoping review and policy analysis. First, in spite of best attempts at ensuring that the search strategy and literature consulted were wide-ranging, certain policy documents and commercial agreements may be confidential and not privy to the public. As such, the scoping review may not cover all relevant policy measures, considerations and outcomes, which could result in an incomplete picture of the strategies and their effectiveness in managing access and the cost of rare disease treatments. Second, the specific focus on high-income countries with advanced healthcare systems limits the generalizability of our findings to LMICs. In particular, LMICs face various challenges and have different healthcare infrastructure and funding mechanisms, which are not addressed in our review. Third, the overt lack of standardized outcome measures (e.g. cost-effectiveness ratios) across the reviewed studies impeded close comparisons of the relative effectiveness and impact of different funding strategies. Future research should prioritize the development and use of uniform metrics to enhance the comparability and synthesis of findings.
Conclusion
Through this scoping review and policy analysis, we recognize that while no country has effectively addressed the challenge of financing rare diseases, the majority have clearly acknowledged that fairness of access is a moral obligation of public health systems. Developed countries and high-performing health systems should further explore and implement outcome-based risk-sharing agreements to balance immediate costs with long-term benefits for patients afflicted by rare diseases. These agreements can ensure that payments are contingent on real-world efficacy, spreading financial risk and encouraging ongoing data collection. Given the rarity and substantial expense of treatments for rare diseases, the most feasible solution seems to lie in improving national healthcare insurance schemes. Equitable rare disease funding should be an area of continued interest and research.
Data availability
The authors confirm that the data supporting the findings of this study are available within the article and its supplementary material.
References
Richter T, Nestler-Parr S, Babela R, Khan ZM, Tesoro T, Molsen E, Hughes DA, International Society for Pharmacoeconomics and Outcomes Research Rare Disease Special Interest Group. Rare disease terminology and Definitions-A systematic global review: report of the ISPOR Rare Disease Special Interest Group. Value Health. 2015;18(6):906–14. https://doi.org/10.1016/j.jval.2015.05.008.
KK Women’s and Children’s Hospital. Rare Disease Fund. KK Women’s and Children’s Hospital. 2023. https://www.kkh.com.sg/giving/Documents/Rare-Disease-Fund/index.html. Accessed January 30, 2024.
Haendel M, Vasilevsky N, Unni D, Bologa C, Harris N, Rehm H, Hamosh A, Baynam G, Groza T, McMurry J, Dawkins H, Rath A, Thaxton C, Bocci G, Joachimiak MP, Köhler S, Robinson PN, Mungall C, Oprea TI. How many rare diseases are there? Nat Rev Drug Discov. 2020;19(2):77–8. https://doi.org/10.1038/d41573-019-00180-y.
Fu MP, Merrill SM, Sharma M, Gibson WT, Turvey SE, Kobor MS. Rare diseases of epigenetic origin: challenges and opportunities. Front Genet. 2023;14:1113086. https://doi.org/10.3389/fgene.2023.1113086.
Ng QX, Ong C, Yaow CYL, Chan HW, Thumboo J, Wang Y, Koh GCH. Cost-of-illness studies of inherited retinal diseases: a systematic review. Orphanet J Rare Dis. 2024;19(1):93. https://doi.org/10.1186/s13023-024-03099-9.
Jensen TL, Gøtzsche CR, Woldbye DPD. Current and future prospects for Gene Therapy for Rare Genetic diseases affecting the brain and spinal cord. Front Mol Neurosci. 2021;14:695937. https://doi.org/10.3389/fnmol.2021.695937.
Wurster C, Petri S. Progress in spinal muscular atrophy research. Curr Opin Neurol. 2022;35(5):693–8. https://doi.org/10.1097/WCO.0000000000001102.
Ministry of Health. Singaporeans diagnosed with spinal muscular atrophy and cost of treatment. Ministry of Health. March 22. 2023. https://www.moh.gov.sg/news-highlights/details/singaporeans-diagnosed-with-spinal-muscular-atrophy-and-cost-of-treatment. Accessed January 15, 2024.
Health Sciences Authority. Register of Class 2 Cell, Tissue or Gene Therapy Products. Health Sciences Authority. December 15. 2023. https://www.hsa.gov.sg/ctgtp/ctgtp-register.html. Accessed January 16, 2023.
Nujiten M. Pricing zolgensma – the World’s most expensive drug. J Mark Access Health Policy. 2022;10(1).
Lee L, Baby. in NUH ICU with severe disease, parents hope to raise S$3 million for ‘world’s most expensive drug’. Today. August 23, 2022. https://www.todayonline.com/singapore/baby-icu-nuh-spinal-muscular-atrophy-severe-disease-fundraiser-expensive-drug-1975686. Accessed January 15, 2023.
Hoy SM, Nusinersen. First Global approval. Drugs. 2017;77(4):473–9. https://doi.org/10.1007/s40265-017-0711-7.
Department of Health and Aged Care. About the Life Saving Drugs Programme. 2023 Apr 1. https://www.health.gov.au/our-work/life-saving-drugs-program/about-the-lsdp. Accessed January 16, 2024.
Yoo SL, Kim DJ, Lee SM, Kang WG, Kim SY, Lee JH, Suh DC. Improving Patient Access to New drugs in South Korea: evaluation of the National Drug Formulary System. Int J Environ Res Public Health. 2019;16(2):288. https://doi.org/10.3390/ijerph16020288.
National Institute for Health and Care Excellence. The Innovative Medicines Fund Principles. 2022 Jun 6. https://www.england.nhs.uk/wp-content/uploads/2022/06/B1686-the-innovate-medicines-fund-principles-june-2022.pdf. Accessed January 16, 2024.
Thomas S, Caplan A. The orphan drug act revisited. JAMA. 2019;321(9):833–4.
World Bank. World Bank Country and Lendind Groups. https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups. Accessed January 16, 2024.
Babigumira JB, Jenny AM, Bartlein R, Stergachis A, Garrison LP. Health technology assessment in low-and middle-income countries: a landscape assessment. J Pharm Health Serv Res. 2016;7(1):37–42.
Tricco AC, Lillie E, Zarin W, O’Brien KK, Colquhoun H, Levac D, Moher D, Peters MDJ, Horsley T, Weeks L, Hempel S, Akl EA, Chang C, McGowan J, Stewart L, Hartling L, Aldcroft A, Wilson MG, Garritty C, Lewin S, Godfrey CM, Macdonald MT, Langlois EV, Soares-Weiser K, Moriarty J, Clifford T, Tunçalp Ö, Straus SE. PRISMA Extension for scoping reviews (PRISMA-ScR): Checklist and Explanation. Ann Intern Med. 2018;169(7):467–73. https://doi.org/10.7326/M18-0850.
Arksey H, O’malley L. Scoping studies: towards a methodological framework. Int J Soc Res Methodol. 2005;8(1):19–32.
Levac D, Colquhoun H, O’Brien KK. Scoping studies: advancing the methodology. Implement Sci. 2010;5:69. https://doi.org/10.1186/1748-5908-5-69.
Popay J, Roberts H, Sowden A, Petticrew M, Arai L, Rodgers M, Britten N, Roen K, Duffy S. Guidance on the conduct of narrative synthesis in systematic reviews. A product from the ESRC. Methods Programme Version. 2006;1(1):b92.
Blankart CR, Stargardt T, Schreyögg J. Availability of and access to orphan drugs: an international comparison of pharmaceutical treatments for pulmonary arterial hypertension, fabry disease, hereditary angioedema and chronic myeloid leukaemia. PharmacoEconomics. 2011;29:63–82. https://doi.org/10.2165/11539190-000000000-00000.
Chan AYL, Chan VKY, Olsson S, Fan M, Jit M, Gong M, Zhang S, Ge M, Pathadka S, Chung CCY, et al. Access and Unmet needs of Orphan drugs in 194 countries and 6 areas: A Global Policy Review with Content Analysis. Value Health. 2020;23:1580–91. https://doi.org/10.1016/j.jval.2020.06.020.
Degtiar I. A review of international coverage and pricing strategies for personalized medicine and orphan drugs. Health Policy. 2017;121:1240–8. https://doi.org/10.1016/j.healthpol.2017.09.005.
Gammie T, Lu CY, Ud-Din Babar Z. Access to orphan drugs: a comprehensive review of legislations, regulations and policies in 35 countries. PLoS ONE. 2015;10. https://doi.org/10.1371/journal.pone.0140002.
Huang YJ, Chao WY, Wang CC, Chang LC. Orphan drug development: the impact of regulatory and reimbursement frameworks. Drug Discovery Today. 2022;27:1724–32. https://doi.org/10.1016/j.drudis.2022.03.002.
Bang JS, Lee JH. The national drug formulary listing process for orphan drugs in South Korea: narrative review focused on pricing and reimbursement pathways. Expert Opin Orphan Drugs. 2021;9:105–12. https://doi.org/10.1080/21678707.2021.1913121.
Lee SH, Yoo SL, Bang JS, Lee JH. Patient accessibility and budget impact of orphan drugs in South Korea: long-term and real-world data analysis (2007–2019). Int J Environ Res Public Health. 2020;17. https://doi.org/10.3390/ijerph17092991.
Lee JH. Pricing and reimbursement pathways of New Orphan drugs in South Korea: a longitudinal comparison. Healthc (Basel Switzerland). 2021;9. https://doi.org/10.3390/healthcare9030296.
Song P, Gao J, Inagaki Y, Kokudo N, Tang W. Rare diseases, orphan drugs, and their regulation in asia: current status and future perspectives. Intractable Rare Dis Res. 2012;1:3–9. https://doi.org/10.5582/irdr.2012.v1.1.3.
Abbas A, Vella Szijj J, Azzopardi LM, Serracino Inglott A. Orphan drug policies in different countries. J Pharm Health Serv Res. 2019;10:295–302. https://doi.org/10.1111/jphs.12305.
Mikami K, Sturdy S. Patient organization involvement and the challenge of securing access to treatments for rare diseases: report of a policy engagement workshop. Res Involv Engagem. 2017;3:14. https://doi.org/10.1186/s40900-017-0065-z.
Picavet E, Morel T, Cassiman D, Simoens S. Shining a light in the black box of orphan drug pricing. Orphanet J Rare Dis. 2014;9. https://doi.org/10.1186/1750-1172-9-62.
Stawowczyk E, Malinowski KP, Kawalec P, Bobinski R, Siwiec J, Panteli D, Eckhardt H, Simoens S, Agusti A, Dooms M, et al. Reimbursement status and recommendations related to Orphan drugs in European Countries. Front Pharmacol. 2019;10:1279. https://doi.org/10.3389/fphar.2019.01279.
Annemans L, Ayme S, Le Cam Y, Facey K, Gunther P, Nicod E, Reni M, Roux J-L, Schlander M, Taylor D et al. Recommendations from the European Working Group for Value Assessment and funding processes in Rare diseases (ORPH-VAL). Orphanet J rare Dis 2017, 12, 50, https://doi.org/10.1186/s13023-017-0601-9.
Doshi JA, Li P, Pettit AR, Dougherty JS, Flint A, Ladage VP. Reducing out-of-pocket cost barriers to specialty drug use under Medicare Part D: addressing the problem of too much too soon. Am J Manag Care. 2017;23:S39–45.
Garland K, Condon S, Xiong DD, Crowe D, Knackstedt TJ. Mohs surgery for SEER registry-captured melanoma in situ and rare cutaneous tumors: comparing national utilization patterns before and after implementation of the affordable care act (2010) and appropriate use criteria (2012). Dermatol Surg. 2020;46:1021–9. https://doi.org/10.1097/DSS.0000000000002316.
Lima HA, Moazzam Z, Endo Y, Alaimo L, Diaz A, Woldesenbet S, Shaikh C, Munir MM, Azap LE, Yang J, et al. Impact of the Affordable Care Act on Presentation, Treatment, and outcomes of Intrahepatic Cholangiocarcinoma. J Gastrointest Surgery: Official J Soc Surg Aliment Tract. 2023;27:262–72. https://doi.org/10.1007/s11605-022-05496-6.
Margaretos NM, Bawa K, Engmann NJ, Chambers JD. Patients’ access to rare neuromuscular disease therapies varies across US private insurers. Orphanet J rare Dis 2022, 17, 36, https://doi.org/10.1186/s13023-022-02182-3.
Pharmaceutical Benefits Scheme. AMWG Interim Report to Government - Attachment A. 2008 Jul. https://www.pbs.gov.au/info/general/working-groups/amwg/amwg-interim-report-attachment-a. Accessed January 16, 2024.
Canada’s Drug and Health Technology Agency. Drugs for rare diseases: A review of national and international health technology assessment agencies and public payers’ decision-making processes. Canada’s Drug and Health Technology Agency. January 25. 2023. https://www.cadth.ca/drugs-rare-diseases-review-national-and-international-health-technology-assessment-agencies-and. Accessed January 16, 2024.
Tuffaha HW, Scuffham PA. The Australian Managed Entry Scheme: are we getting it right? PharmacoEconomics. 2018;36(5):555–65. https://doi.org/10.1007/s40273-018-0633-6.
Lu CY, Lupton C, Rakowsky S, Babar ZU, Ross-Degnan D, Wagner AK. Patient access schemes in Asia-pacific markets: current experience and future potential. J Pharm Policy Pract 20156;8(1):6. https://doi.org/10.1186/s40545-014-0019-x.
Department of Health and Aged Care. Procedure guidance for medicines funded through the Life Saving Drugs Program (LSDP). 2018 Jul. https://www.health.gov.au/sites/default/files/documents/2021/11/procedure-guidance-for-medicines-funded-through-the-life-saving-drugs-program-lsdp.pdf. Accessed January 16, 2024.
Chim L, Salkeld G, Kelly P, Lipworth W, Hughes DA, Stockler MR. Societal perspective on access to publicly subsidised medicines: a cross sectional survey of 3080 adults in Australia. PLoS ONE. 2017;12(3):e0172971. https://doi.org/10.1371/journal.pone.0172971.
Department of Health and Aged Care. Ensuring the future sustainability of the Life Saving Drugs Programme (LSDP). 2020 https://www.health.gov.au/sites/default/files/documents/2020/10/ensuring-the-future-sustainability-of-the-life-saving-drugs-program.pdf. Accessed January 16, 2024.
Department of Health and Aged Care. Improving access to medicines – New medicines added to the Pharmaceutical Benefits Scheme. 2022 May. https://www.health.gov.au/sites/default/files/documents/2022/03/budget-2022-23-new-medicines-added-to-the-pharmaceutical-benefits-scheme.pdf. Accessed January 16, 2024.
Butler M, Department of Health and Aged Care. Life changing gene therapy for babies with spinal muscular atrophy. 2023 Oct 23. https://www.health.gov.au/ministers/the-hon-mark-butler-mp/media/life-changing-gene-therapy-for-babies-with-spinal-muscular-atrophy. Accessed January 16, 2024.
Pharmaceutical Benefit Scheme. Public Summary Document – November 2020 PBAC Meeting with May 2021 Addendum. 2021 May. https://www.pbs.gov.au/industry/listing/elements/pbac-meetings/psd/2021-05/files/onasemnogene-abeparvovec-psd-may-2021.docx. Accessed January 16, 2024.
Pharmaceutical Benefit Scheme. Public Summary Document – November 2020 PBAC Meeting with May 2021 Addendum and September 2021 Addendum. 2021 Sep. https://www.pbs.gov.au/industry/listing/elements/pbac-meetings/psd/2021-09/files/onasemnogene-abeparvovec-psd-september-2021.docx. Accessed January 16, 2024.
Today. Govt looking at more help for children with rare diseases. Today. January 9, 2021. https://www.todayonline.com/singapore/govt-looking-more-help-children-rare-diseases. Accessed January 15, 2024.
Ministry of Health. Rare disease fund to provide financial support to Singaporeans with rare diseases. Ministry of Health. July 2. 2019. https://www.moh.gov.sg/news-highlights/details/rare-disease-fund-to-provide-financial-support-to-singaporeans-with-rare-diseases. Accessed January 15, 2024.
National Archives of Singapore Library. Statement by Mr Abdullah Tarmugi. National Archives of Singapore Library. March 10. 1993. https://www.nas.gov.sg/archivesonline/data/pdfdoc/at19950310s.pdf. Accessed January 15, 2024.
Sin Y. Rare disease fund now covers Pompe disease, a rare inherited neuromuscular disorder. The Straits Times. November 3, 2019. https://www.straitstimes.com/singapore/health/rare-disease-fund-now-covers-pompe-disease-a-rare-inherited-neuromuscular-disorder. Accessed January 15, 2024.
KK Women’s and Children’s Hospital. Rare Disease Fund extends support to another rare disease with $6.7 million gift. KK Women’s and Children’s Hospital. August 19. 2021. https://www.kkh.com.sg/news/giving-philanthropy/rare-disease-fund-extends-support-to-another-rare-disease-with-67-million-gift. Accessed January 15, 2024.
Iau J. 9 Singaporean patients helped by Rare Disease Fund since 2019. The Straits Times. April 11, 2023. https://www.straitstimes.com/singapore/9-patients-or-04-per-cent-of-those-who-suffer-from-rare-diseases-helped-by-fund-since-2019. Accessed January 15, 2024.
Medisave MS. Life, and MediFund. Ministry of Health Singapore. https://www.moh.gov.sg/cost-financing/healthcare-schemes-subsidies/medishield-life. Accessed January 15, 2024.
Ministry of Health Singapore. Size annual income and expenditure of rare disease fund. Ministry of Health Singapore. October 4. 2023. https://www.moh.gov.sg/news-highlights/details/size-annual-income-and-expenditure-of-rare-disease-fund. Accessed January 15, 2024.
Ong J. Rare Disease Fund should cover more illnesses, benefit more people: MP Cheryl Chan. Today. August 3, 2021. https://www.todayonline.com/singapore/rare-disease-fund-should-cover-more-illnesses-benefit-more-people-cheryl-chan.html. A Accessed January 15, 2024.
Goh YH. More ill children can get help with more donations to Rare Disease Fund says Koh Poh Koon. The Straits Times. August 2, 2021. https://www.straitstimes.com/singapore/politics/parliament-more-ill-children-can-get-help-with-more-donations-to-rare-diseases. Accessed January 15, 2024.
Jeon B, Kwon S. Effect of private health insurance on health care utilization in a universal public insurance system: a case of South Korea. Health Policy. 2013;113(1):69–76.
Song YJ. The South Korean Healthcare System. Jpn Med Assoc J. 2009;52(3):206–9.
Health insurance review and assessment service: national drug formulary. Wonju. 2020 https://www.hira.or.kr/bbsDummy.do?pgmid=HIRAA030014050000. Accessed January 15, 2024.
Kim S, Cho H, Kim J, Lee K, Lee JH. The current state of patient access to new drugs in South Korea under the positive list system: evaluation of the changes since the new review pathways. Expert Rev Pharmacoecon Outcomes Res. 2021;21(1):119–26. https://doi.org/10.1080/14737167.2020.1758559.
Lim SS, Lee W, Kim YK, Kim J, Park JH, Park BR, Yoon JH. The cumulative incidence and trends of rare diseases in South Korea: a nationwide study of the administrative data from the National Health Insurance Service database from 2011–2015. Orphanet J Rare Dis. 2019;14(1):49. https://doi.org/10.1186/s13023-019-1032-6.
Kim YN. Ultra-expensive SMA drug Zolgensma to get insurance benefits from August. Korea Biomed Rev. July 21, 2022. https://www.koreabiomed.com/news/articleView.html?idxno=14205. Accessed January 15, 2024.
Chang M. Korea’s 1st gene treatment for SMA Zolgensma gets insurance benefits. Korea Biomed Rev. August 1, 2022. https://wwwkoreabiomed.com/news/articleView.html?idxno=14296. Accessed January 16, 2024.
Grosios K, Gahan PB, Burbidge J. Overview of healthcare in the UK. EPMA J. 2010;1(4):529–34. https://doi.org/10.1007/s13167-010-0050-1.
McCabe C, Claxton K, Culyer AJ. The NICE cost-effectiveness threshold: what it is and what that means. PharmacoEconomics. 2008;26(9):733–44.
Department of Health and Social Care. England Rare Diseases Action Plan. 2022. 2022 Feb. https://assets.publishing.service.gov.uk/media/62191cf0d3bf7f4f0ec9b6bf/England-Rare-Diseases-Action-Plan-2022.pdf. Accessed January 16, 2024.
National Institute for Health and Care Excellence. Health technology evaluation manual. 2022 Feb 1. https://www.nice.org.uk/about/what-we-do/our-programmes/nice-guidance/nice-technology-appraisal-guidance/changes-to-health-technology-evaluation. Accessed January 16, 2024.
National Institute for Health and Care Excellence. NICE health technology evaluation topic selection: the manual. 2022 Jan 31. https://www.nice.org.uk/process/pmg37/chapter/highly-specialised-technologies. Accessed January 16, 2024.
National Institute for Health and Care Excellence. NICE health technology evaluations: the manual, NICE Process and Methods. https://www.nice.org.uk/process/pmg36/chapter/committee-recommendations-2. Accessed January 16, 2024.
Centre for Evidence-Based Medicine. Defining value-based healthcare in the NHS. 2019 Apr. https://www.cebm.net/wp-content/uploads/2019/04/Defining-Value-based-healthcare-in-the-NHS-Final4-1.pdf. Accessed January 16, 2024.
Angelis A, Aggarwal A, Miners A, Grieve R, Cairns J, Briggs A. The innovative Medicines Fund: a universal model for faster and fairer access to new promising medicines or a trojan horse for low-value creep? J R Soc Med. 2023;116(10):324–30. https://doi.org/10.1177/01410768231192476.
Roberts M. Innovative Medicines Fund launched to fast-track drugs. BBC. 2022 Jun 7. https://www.bbc.com/news/health-61709542. Accessed January 16, 2024.
Guimaraes R. New challenges in health technology assessment (HTA): the case of Zolgensma. cien Saude Colet. 2023;28(7):1881–9.
Côté A, Keating B. What is wrong with orphan drug policies? Value Health. 2012;15(8):1185–91.
Chua KP, Conti RM. Trends in Orphan drug spending and Out-Of-Pocket spending among US children, 2013–18. Health Aff (Millwood). 2020;39(10):1806–11.
Pasquini TL, Goff SL, Whitehill JM. Navigating the US health insurance landscape for children with rare diseases: a qualitative study of parents’ experiences. Orphanet J Rare Dis. 2021;16(1):1–4.
National Organization for Rare Diseases. Protecting Patients in State-Regulated Insurance. https://rarediseases.org/policy-issues/state-regulated-insurance. Accessed January 16, 2024.
Fox AM, Feng W, Zeitlin J, Howell EA. Trends in State Medicaid Eligibility, Enrollment rules, and benefits. Health Aff (Millwood). 2020;39(11):1909–16. https://doi.org/10.1377/hlthaff.2019.01350.
Drell D, De Silva A, Lee C. What rare disease patient advocacy groups are doing to mitigate the effects of disparities. Adv Pulm Hypertens. 2022;21(2):35–43.
Wills A, Mitha A. Financial characteristics of outcomes-based agreements: what do Canadian Public Payers and Pharmaceutical Manufacturers Prefer? Value Health. 2024;27(3):340–6. https://doi.org/10.1016/j.jval.2023.12.011.
Brennan TA, Wilson JM. The special case of gene therapy pricing. Nat Biotechnol. 2014;32(9):874–6. https://doi.org/10.1038/nbt.3003.
Jørgensen J, Hanna E, Kefalas P. Outcomes-based reimbursement for gene therapies in practice: the experience of recently launched CAR-T cell therapies in major European countries. J Mark Access Health Policy. 2020;8(1):1715536. https://doi.org/10.1080/20016689.2020.1715536.
Alex Watt. Risk-sharing agreements are growing at a rate of 24%. Pharmaceutical Technology. February 10. 2023. https://www.pharmaceutical-technology.com/pricing-and-market-access/risk-sharing-agreements. Accessed January 30, 2024.
Michelsen S, Nachi S, Van Dyck W, Simoens S, Huys I. Barriers and opportunities for implementation of outcome-based spread payments for High-Cost, one-shot curative therapies. Front Pharmacol. 2020;11:594446. https://doi.org/10.3389/fphar.2020.594446.
Acknowledgements
We thank Mr Dongju Shin (Graduate Student, Yonsei University, Seoul, South Korea) for his invaluable assistance in translating and verifying the information sources in Korean.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
Conceptualization: QXN; Data curation: QXN, CO, KEC, TSKO, IJXL, ASPT and GCHK; Investigation: QXN, CO, KEC, TSKO, IJXL and ASPT; Formal analysis: QXN, CO, HWC and GCHK; Methodology: QXN, CO, HWC, KEC, TSKO, IJXL, ASPT and GCHK; Supervision: HWC and GCHK.; Writing – original draft: QXN and CO; Writing – review & editing: All authors. All authors have read and agreed to the final version of the manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable. No patients or participants were directly involved in this study as it was a review of published literature.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ng, Q.X., Ong, C., Chan, K.E. et al. Comparative policy analysis of national rare disease funding policies in Australia, Singapore, South Korea, the United Kingdom and the United States: a scoping review. Health Econ Rev 14, 42 (2024). https://doi.org/10.1186/s13561-024-00519-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13561-024-00519-1