Abstract
Objectives
The association between habitual glucosamine use and incident gout has not been examined in previous studies. We aimed to evaluate the association of habitual use of glucosamine with the risk of gout in general population.
Methods
A total of 436,594 participants (55.4% female) without prior gout at baseline who completed a questionnaire on supplementation use, which included glucosamine, in the UK Biobank were enrolled. Incident gout was recorded from self-report, death register, primary care, and hospital admission data.
Results
At baseline, 53,433 (22.1%) females and 30,685 (15.8%) males reported habitual glucosamine use. During a median follow-up period of 12.1 years, 1718 (0.7%) females and 5685 (2.9%) males developed gout. After multivariable adjustment for major risk factors, glucosamine use was associated with a significantly lower risk of incident gout in females (hazard ratio [HR], 0.81, 95% confidence interval [CI], 0.71–0.92), but not in males (HR, 1.05, 95% CI, 0.97–1.13), compared with non-use (P-interaction < 0.001). Among females, the inverse association between glucosamine use and gout was stronger in participants with diuretics use (HR, 0.64, 95% CI, 0.50–0.81) than those without diuretics use (HR, 0.89, 95% CI, 0.77–1.03) (P-interaction = 0.015). Moreover, gout genetic risk scores did not significantly modify the association between glucosamine use and the risk of incident gout in males (P-interaction = 0.548) or females (P-interaction = 0.183).
Conclusions
Habitual glucosamine use to relieve osteoarthritis pain was related to lower risk of gout in females, but not in males.
Highlights
-
1.
Glucosamine use was associated with lower risk of incident gout in females.
-
2.
The inverse association between glucosamine use and gout was stronger in females with diuretics use.
-
3.
Gout genetic risk scores did not significantly modify the association.
Similar content being viewed by others
Introduction
Gout, an inflammatory crystal-induced arthritis caused by the deposition of monosodium urate crystals in articular and non-articular structures, affects approximately 41.2 million adults worldwide [1, 2]. The effects of gout include not only acute pain, functional disability, and permanent joint damage, but also significant long-term illness and costs [3, 4]. Due to the increasing prevalence and incidence of gout, as well as the suboptimal management of gout in many countries [5], identifying more effective, safe and economical primary prevention measures has important clinical value.
Glucosamine is a popular non-vitamin, non-mineral dietary supplement widely used to relieve osteoarthritis and joint pain [6, 7], with a high safety profile, and has recently garnered interest for their potential anti-inflammatory effects [7]. Inflammation plays an essential role in gout [8]. Accordingly, a recent study found that the IL-1β inhibitor canakinumab administration was associated with significantly reduced risk for gout attacks in patients with a prior myocardial infarction [9]. Therefore, given the anti-inflammatory properties of glucosamine, we hypothesized that habitual glucosamine use may be also related to decreased gout risk. However, no studies have analyzed the association between habitual glucosamine use and incident gout in prospective cohorts.
To address these aforementioned gaps in knowledge, the present study aimed to evaluate the association of habitual use of glucosamine with the risk of gout in general population, using population-based cohort data from nearly half a million adults in the UK Biobank study. We also assessed the joint association of glucosamine use and genetic susceptibility with the risk of gout.
Methods
Data source and study population
The UK Biobank is a large prospective, observational, population-based cohort of half a million adult residents of the United Kingdom, aged 37–73 years, from 22 assessment centers across England, Wales, and Scotland between 2006 and 2010. Participants were asked to complete a touch screen questionnaire, a face-to-face interview and a series of physical measurements, as well as provide biological samples for laboratory analysis. The details of the study design have been described previously [10, 11]. The UK Biobank was approved by the North West Research Ethics Committee (06/MRE08/65) and all participants signed an informed consent.
In this study, we restricted our analysis to participants who had complete information on the use of glucosamine and were free of gout (n = 484,720). We also excluded participants with unavailable genetic data and data on the important covariates (n = 48,126). Therefore, a total of 436,594 participants were enrolled in the present analysis (Additional file 1: Fig. S1).
Ascertainment of exposure and covariates
At baseline, habitual glucosamine information was collected through a touch-screen questionnaire. Participants were asked, “Do you regularly take any of the following?” and could select their answer from a list of supplementations, including vitamin, mineral, fish oil and glucosamine. From this information, regular use of glucosamine was defined as “1 = yes” and “0 = no”.
Detailed information on covariates was available through standardized questionnaires, including age, sex, race, Townsend Deprivation Index (TDI), smoking status, alcohol consumption, comorbidities (hypertension, diabetes, high cholesterol, osteoarthritis, rheumatoid arthritis, and joint pain), and drug use (cholesterol lowering medication, anti-hypertensive drug, insulin, aspirin, ibuprofen, paracetamol, and diuretics). Body mass index (BMI) (kg/m2) was calculated based on measured weight and height. Prevalent diabetes at baseline was identified through multiple procedures considering type of diabetes and sources of the diagnosis [12]. A healthy diet score was evaluated using a more recent dietary recommendation for cardiovascular health, which considered adequate consumption of fruit, vegetables, whole grains, fish, shellfish, dairy products, and vegetable oils and reduced consumption of refined grains, processed meats, unprocessed meats, and sugar sweetened beverages, and a healthy diet was defined as meeting at least five items of the recommendations [13]. In addition, biochemistry measures were performed at a dedicated central laboratory, including creatinine, urate and C-reactive protein (CRP). Estimated glomerular filtration rate (eGFR) was calculated by Chronic Kidney Disease–Epidemiology Collaboration equation (CKD–EPI) using serum creatinine [14].
Definition of genetic risk score
Detailed information about genotyping and quality control in the UK Biobank study has been described previously [15]. We selected 13 single nucleotide polymorphisms (SNPs) which showed independently significant genome-wide association with gout in recent published genome-wide associations studies (Additional file 1: Table S1) [16]. Genetic risk score (GRS) was calculated using a weighted method [17] and a higher score indicates a higher genetic predisposition to gout, and participants were divided into low, intermediate, or high genetic risk for gout according to the tertiles of GRS.
Ascertainment of outcomes
The primary outcome of the study was the incidence of gout, and gout diagnosis was extracted from “first occurrence of health outcomes defined by a 3-character International Statistical Classification of Diseases and Related Health Problems 10th Revision code (M10)” based on self-report or linkage to death register and/or primary care and/or hospital admission data. The follow-up person-time for each participant was calculated from the date of first assessment until the date of death, first date of outcome diagnosis, date of lose to follow-up, or end of follow-up, whichever came first.
Statistical analysis
Population characteristics are presented as mean ± standard deviation (SD) for continuous variables and proportions for categorical variables. Comparisons of characteristics according to glucosamine use (yes or no) by sex were performed by chi-square tests for categorical variables and t tests for continuous variables.
Cox proportional hazards models were used to estimate hazard ratio (HR) and 95% confidence interval (CI) of gout for habitual glucosamine use (yes vs. no). The proportional hazard assumption was evaluated by the interaction between exposures and follow-up time and no violation of this assumption was detected. In multivariable models, potential confounders that were known to be traditional or suspected risk factors for gout were adjusted for, including age, sex, race, TDI, BMI, smoking status, alcohol consumption, healthy diet score, vitamin or mineral supplementation, fish oil supplementation, comorbidities (hypertension, diabetes, high cholesterol, osteoarthritis, rheumatoid arthritis, and joint pain), drug uses (cholesterol lowering medication, anti-hypertensive drug, insulin, aspirin, ibuprofen, paracetamol, and diuretics), eGFR, and urate. To control the potential influence of genetic predisposition to gout, we further adjusted for gout GRS, as well as estimated the joint association of glucosamine use and gout GRS with the risk of incident gout using glucosamine non-users with low genetic risk as reference.
Stratified analysis was conducted to assess potential modification effects of glucosamine use according to age (< 60 or ≥ 60 years), BMI (< 30 or ≥ 30 kg/m2), smoking status (never or ever), alcohol consumption (< 1 or ≥ 1 times/week), health diet (yes or no), supplementation use (yes or no), diabetes (yes or no), hypertension (yes or no), diuretics use (yes or no), aspirin use (yes or no), paracetamol or ibuprofen use (yes or no), and CRP (tertiles). Potential modifying effects were assessed by modelling the cross product term of the stratifying variable with glucosamine use.
A two-tailed P < 0.05 was considered to be statistically significant in all analyses. Analyses were performed using R 4.1.1 software (http://www.R-project.org/).
Results
Study participants and baseline characteristics
Among 436,594 participants in the current study, 242,009 (55.4%) were females, with a mean age of 56.5 years. Overall, 53,433 (22.1%) females and 30,685 (15.8%) males reported habitual glucosamine supplementation at baseline.
As shown in Table 1, compared with nonusers, glucosamine users were older, more likely to be White, non-current smokers, dietary supplementation users, and tended to have lower TDI, higher alcohol intake and healthy diet, higher prevalence of high cholesterol, osteoarthritis and joint pain, but a lower prevalence of diabetes, as well as more likely to take aspirin, ibuprofen, and paracetamol. In addition, glucosamine users tended to have higher prevalence of hypertension and more likely to take antihypertensive drugs among females, while glucosamine users tended to have lower prevalence of hypertension and less likely to take antihypertensive drugs among males.
Association between glucosamine use and risk of incident gout
During a median follow-up period of 12.1 years (5,124,432 person-years), a total of 7403 (1.7%) participants, including 1718 (0.7%) females and 5685 (2.9%) males, developed gout.
After adjustment for important covariates including socioeconomic and behavioral factors, comorbidities, and drug uses, glucosamine use was associated with lower risks of gout in all participants (HR, 0.87, 95% CI, 0.81–0.93), females (HR, 0.75, 95% CI, 0.66–0.85), and males (HR, 0.92, 95% CI, 0.85–0.99) (Table 2). However, when further adjusted for eGFR and urate, the association only persisted in females (HR, 0.81, 95% CI, 0.71–0.92), but not in males (HR, 1.05, 95% CI, 0.97–1.13) (P-interaction < 0.001). Further adjustment for gout GRS did not materially change the magnitude and the significance (Table 2).
Joint association of glucosamine use and gout GRS with the risk of incident gout
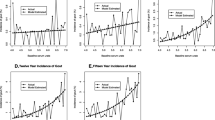
In the joint analysis, as expected, higher gout GRS was significantly associated with higher risk of incident gout (Fig. 1).
Joint association of glucosamine use and genetic risk in relation to risk of gout. Adjusted for age, sex (only for total population), race, Townsend Deprivation Index, body mass index, smoking status, alcohol consumption, healthy diet score, vitamin or mineral supplementation, fish oil supplementation, comorbidities (hypertension, diabetes, high cholesterol, osteoarthritis, rheumatoid arthritis, and joint pain), drug use (cholesterol lowering medication, anti-hypertensive drug, insulin, aspirin, ibuprofen, paracetamol, and diuretics), estimated glomerular filtration rate and urate
However, gout GRS did not significantly modify the association between glucosamine use and the risk of incident gout in males (P-interaction = 0.548) or females (P-interaction = 0.183). Therefore, among females, glucosamine non-users with a high genetic risk had the highest risk of gout (HR, 1.29, 95% CI, 1.13–1.48), compared with glucosamine non-user with a low genetic risk (Fig. 1).
Stratified analyses
Stratified analyses were separately performed by sex to further assess the relation of regular glucosamine supplementations with the risk of incident gout in various subgroups (Fig. 2).
Association of glucosamine use and the risk of gout stratified by potential risk factors in females. Results were adjusted for age, race, Townsend Deprivation Index, body mass index, smoking status, alcohol consumption, healthy diet score, vitamin or mineral supplementation, fish oil supplementation, comorbidities (hypertension, diabetes, high cholesterol, osteoarthritis, rheumatoid arthritis, and joint pain), drug use (cholesterol lowering medication, anti-hypertensive drug, insulin, aspirin, ibuprofen, paracetamol, and diuretics), estimated glomerular filtration rate and urate, if not already stratified
Among females, the inverse association was stronger with diuretics uses (P-interaction = 0.015; Fig. 2). No other significant variables, including age, BMI, smoking status, alcohol consumption, health diet, supplementation use, diabetes, hypertension, diuretics use, aspirin use, paracetamol or ibuprofen use, and CRP showed significant effect modifications on the association of glucosamine use with gout incidence in females (all P for interaction ≥ 0.05; Fig. 2). Notably, none of the above variables significantly modified the association between glucosamine use and the risk of incident gout in males (all P for interaction ≥ 0.05; Additional file 1: Fig. S2).
Discussion
In this large population-based cohort of individuals, habitual glucosamine use was associated with a significantly lower risk of incident gout in females but not in males, independent of traditional risk factors and genetic risk factors. Furthermore, the protective associations of glucosamine use with gout risk appeared to be somewhat stronger in females who took diuretics medications.
To the best of our knowledge, the current study is the first one to explore the association of regular glucosamine use with risk of incident gout in a prospective cohort. Based on the UK Biobank cohort, several previous studies have demonstrated that habitual use of glucosamine was associated with lower risk of 17% for incident type 2 diabetes, 15% for cardiovascular disease events, 20% for chronic obstructive pulmonary disease, 15% for all-cause mortality, 18% for mortality from cardiovascular disease, 6% for mortality from cancer, and 27% for mortality from respiratory mortality [18,19,20,21]. Consistently, our study first observed 19% lower risk of gout associated with glucosamine use in females. In addition, although the interaction was not statistically significant, the reduced risk with glucosamine appeared to be more pronounced in women with a higher genetic risk.
The precise biological mechanisms underlying the inverse association between glucosamine use and risk of gout in females is not fully understood. Evidences from previous studies have shown that glucosamine has anti-inflammatory properties [22, 23]. Given the detrimental roles of inflammation in the development of gout, we assumed that glucosamine supplementation might reduce the gout risk partly through the anti-inflammatory effect. Interestingly, our findings showed that females are more likely to benefit from glucosamine in terms of risk of gout, which may be partly explained by the sex differences in inflammation. For example, estrogen can either promote inflammation by enhancing Th1 and/or Th17 responses though transcriptional activation of NFκB or suppress the expression of cyclooxygenase-2 [24, 25], while glucosamine could oppose NFκB activation via O-GlcNAcylation of the anti-inflammatory protein A20 and decrease the production of inflammatory cytokines related to NF-kB activation [22, 26, 27]. In addition, glucosamine could mediate alternative macrophage activation in vivo and the production of leukotriene B(4) [28]. Previous evidence that androgens suppress leukotriene biosynthesis along with lower leukotriene production in males [25] suggested that anti-leukotriene therapy might be more relevant and effective for females, which was consistent with our findings that sex modified the inverse association between glucosamine use and gout. However, other mechanisms may be also involved and needed to be further examined.
Of note, diuretics are the well-known medications to be associated with gout, since diuretics could raise serum uric acid levels by increasing uric acid reabsorption and decreasing uric acid secretion in the kidneys. In our study, we observed a stronger inverse association of regular glucosamine use with risk of gout in participants with the usage of diuretics in females. It's biologically plausible considering that glucosamine could disrupt monosodium urate crystals-induced activation of the NLRP3 inflammasome by reducing mitochondrial reactive oxygen species generation inhibiting NLRP3 binding to PKR, NEK7 and ASC [1, 27, 29]. Taken together, glucosamine seems promising as a recommended protective agent for prevention of gout, especially for females taking diuretics.
The main advantages of this study include a large-scale population-based prospective study design with a long follow-up period, which shows the effectiveness of glucosamine supplementation in the real-life environment. However, several potential limitations should also be considered. First, it is difficult to distinguish the effects of a healthy lifestyle from habitual glucosamine use in this observational study. Although we carefully controlled for potential confounding factors and performed stratified analysis, the observed inverse associations might be driven by unmeasured or unknown health-related factors. Second, the lack of detailed information on the use of glucosamine supplementation, such as the dose, formulation (glucosamine sulfate, glucosamine hydrochloride, N-acetyl glucosamine), frequency and duration, precluded us from assessing the dose–response relationships of glucosamine supplementation and the appropriate duration of supplementation. Third, the participants were predominantly of European descent and healthier than the UK general population, which may limit generalizability of the findings to other populations. Owing to these limitations, further confirmation of the reported findings in future studies is necessary.
Perspectives and significance
This large-scale prospective study found that glucosamine might be more relevant and effective for females and seems promising as a recommended protective agent for prevention of gout in female, but not in males, especially for those taking diuretics. Therefore, further clinical trials are needed to explore the effect of glucosamine supplementation on the occurrence of gout in females and encourage researchers to dissect the molecular mechanisms involved.
Conclusions
In conclusion, this large-scale prospective study showed that regular glucosamine use is inversely associated with incident gout and the inverse association was modified by sex and diuretics use. These findings provide support that glucosamine may act as a potential supplementation for preventing gout in general population, and further clinical trials are needed to test this hypothesis.
Availability of data and materials
The UK Biobank data are available on application to the UK Biobank, and the analytic methods, and study materials that support the findings of this study will be available from the corresponding authors on request.
References
Dalbeth N, Gosling AL, Gaffo A, Abhishek A. Gout. Lancet. 2021;397(10287):1843–55.
Safiri S, Kolahi AA, Cross M, Carson-Chahhoud K, Hoy D, Almasi-Hashiani A, Sepidarkish M, Ashrafi-Asgarabad A, Moradi-Lakeh M, Mansournia MA, Kaufman JS, Collins G, Woolf AD, March L, Smith E. Prevalence, incidence, and years lived with disability due to gout and its attributable risk factors for 195 countries and territories 1990–2017: a systematic analysis of the global burden of disease study 2017. Arthritis Rheumatol. 2020;72(11):1916–27.
Lim SY, Lu N, Oza A, Fisher M, Rai SK, Menendez ME, Choi HK. Trends in gout and rheumatoid arthritis hospitalizations in the United States, 1993–2011. JAMA. 2016;315(21):2345–7.
Wu EQ, Patel PA, Yu AP, Mody RR, Cahill KE, Tang J, Krishnan E. Disease-related and all-cause health care costs of elderly patients with gout. J Manag Care Pharm. 2008;14(2):164–75.
Dehlin M, Jacobsson L, Roddy E. Global epidemiology of gout: prevalence, incidence, treatment patterns and risk factors. Nat Rev Rheumatol. 2020;16(7):380–90.
Jordan KM, Arden NK, Doherty M, Bannwarth B, Bijlsma JW, Dieppe P, Gunther K, Hauselmann H, Herrero-Beaumont G, Kaklamanis P, Lohmander S, Leeb B, Lequesne M, Mazieres B, Martin-Mola E, Pavelka K, Pendleton A, Punzi L, Serni U, Swoboda B, Verbruggen G, Zimmerman-Gorska I, Dougados M; Standing Committee for International Clinical Studies Including Therapeutic Trials ESCISIT. EULAR Recommendations 2003: an evidence based approach to the management of knee osteoarthritis: Report of a Task Force of the Standing Committee for International Clinical Studies Including Therapeutic Trials (ESCISIT). Ann Rheum Dis. 2003;62(12):1145–55.
Dahmer S, Schiller RM. Glucosamine. Am Fam Physician. 2008;78:471–6.
So AK, Martinon F. Inflammation in gout: mechanisms and therapeutic targets. Nat Rev Rheumatol. 2017;13(11):639–47.
Schlesinger N. Relationship of interleukin-1beta blockade with incident gout and serum uric acid levels. Ann Intern Med. 2019;170:737–8.
Sudlow C, Gallacher J, Allen N, Beral V, Burton P, Danesh J, Downey P, Elliott P, Green J, Landray M, Liu B, Matthews P, Ong G, Pell J, Silman A, Young A, Sprosen T, Peakman T, Collins R. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 2015;12(3): e1001779.
Collins R. What makes UK Biobank special? Lancet. 2012;379:1173–4.
Eastwood SV, Mathur R, Atkinson M, Brophy S, Sudlow C, Flaig R, de Lusignan S, Allen N, Chaturvedi N. Algorithms for the capture and adjudication of prevalent and incident diabetes in UK Biobank. PLoS ONE. 2016;11(9): e0162388.
Zhang YB, Chen C, Pan XF, Guo J, Li Y, Franco OH, Liu G, Pan A. Associations of healthy lifestyle and socioeconomic status with mortality and incident cardiovascular disease: two prospective cohort studies. BMJ. 2021;373: n604.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, Kusek JW, Eggers P, Van Lente F, Greene T, Coresh J; CKD-EPI (Chronic Kidney Disease Epidemiology Collaboration). A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Bycroft C, Freeman C, Petkova D, Band G, Elliott LT, Sharp K, Motyer A, Vukcevic D, Delaneau O, O’Connell J, Cortes A, Welsh S, Young A, Effingham M, McVean G, Leslie S, Allen N, Donnelly P, Marchini J. The UK Biobank resource with deep phenotyping and genomic data. Nature. 2018;562(7726):203–9.
Sandoval-Plata G, Morgan K, Abhishek A. Variants in urate transporters, ADH1B, GCKR and MEPE genes associate with transition from asymptomatic hyperuricaemia to gout: results of the first gout versus asymptomatic hyperuricaemia GWAS in Caucasians using data from the UK Biobank. Ann Rheum Dis. 2021;80(9):1220–6.
Khera AV, Emdin CA, Drake I, Natarajan P, Bick AG, Cook NR, Chasman DI, Baber U, Mehran R, Rader DJ, Fuster V, Boerwinkle E, Melander O, Orho-Melander M, Ridker PM, Kathiresan S. Genetic risk, adherence to a healthy lifestyle, and coronary disease. N Engl J Med. 2016;375(24):2349–58.
Ma H, Li X, Zhou T, Sun D, Liang Z, Li Y, Heianza Y, Qi L. Glucosamine use, inflammation, and genetic susceptibility, and incidence of type 2 diabetes: a prospective study in UK Biobank. Diabetes Care. 2020;43(4):719–25.
Ma H, Li X, Sun D, Zhou T, Ley SH, Gustat J, Heianza Y, Qi L. Association of habitual glucosamine use with risk of cardiovascular disease: prospective study in UK Biobank. BMJ. 2019;365: l1628.
Li ZH, Gao X, Chung VC, Zhong WF, Fu Q, Lv YB, Wang ZH, Shen D, Zhang XR, Zhang PD, Li FR, Huang QM, Chen Q, Song WQ, Wu XB, Shi XM, Kraus VB, Yang X, Mao C. Associations of regular glucosamine use with all-cause and cause-specific mortality: a large prospective cohort study. Ann Rheum Dis. 2020;79(6):829–36.
Zhang XR, Zhang PD, Li ZH, Yang P, Wang XM, Liu HM, Liang F, Wang JD, Sun Y, Shen D, Chen PL, Zhong WF, Huang QM, Liu D, Wang ZH, Kraus VB, Mao C. Glucosamine use, smoking and risk of incident chronic obstructive pulmonary disease: a large prospective cohort study. Br J Nutr. 2021:1–12.
Largo R, Alvarez-Soria MA, Díez-Ortego I, Calvo E, Sánchez-Pernaute O, Egido J, Herrero-Beaumont G. Glucosamine inhibits IL-1beta-induced NFkappaB activation in human osteoarthritic chondrocytes. Osteoarthr Cartil. 2003;11(4):290–8.
Yomogida S, Hua J, Sakamoto K, Nagaoka I. Glucosamine suppresses interleukin-8 production and ICAM-1 expression by TNF-alpha-stimulated human colonic epithelial HT-29 cells. Int J Mol Med. 2008;22:205–11.
Di Florio DN, Sin J, Coronado MJ, Atwal PS, Fairweather D. Sex differences in inflammation, redox biology, mitochondria and autoimmunity. Redox Biol. 2020;31: 101482.
Pace S, Sautebin L, Werz O. Sex-biased eicosanoid biology: impact for sex differences in inflammation and consequences for pharmacotherapy. Biochem Pharmacol. 2017;145:1–11.
Imagawa K, de Andrés MC, Hashimoto K, Pitt D, Itoi E, Goldring MB, Roach HI, Oreffo RO. The epigenetic effect of glucosamine and a nuclear factor-kappa B (NF-kB) inhibitor on primary human chondrocytes—implications for osteoarthritis. Biochem Biophys Res Commun. 2011;405(3):362–7.
McCarty MF, Iloki Assanga SB, Lewis Luján L, O Keefe JH, DiNicolantonio JJ. Nutraceutical strategies for suppressing NLRP3 inflammasome activation: pertinence to the management of COVID-19 and beyond. Nutrients. 2021;13:47.
Reese TA, Liang HE, Tager AM, Luster AD, Van Rooijen N, Voehringer D, Locksley RM. Chitin induces accumulation in tissue of innate immune cells associated with allergy. Nature. 2007;447(7140):92–6.
Chiu HW, Li LH, Hsieh CY, Rao YK, Chen FH, Chen A, Ka SM, Hua KF. Glucosamine inhibits IL-1β expression by preserving mitochondrial integrity and disrupting assembly of the NLRP3 inflammasome. Sci Rep. 2019;9(1):5603.
Acknowledgements
We specially thank the all the participants of UK Biobank and all the people involved in building the UK Biobank study.
Funding
The study was supported by the National Natural Science Foundation of China (81973133, 81730019); the National Key Research and Development Program (2022YFC2009600).
Author information
Authors and Affiliations
Contributions
ML and XQ designed and conducted the research; ML, ZY, and YZ performed the data management and statistical analyses; ML and XQ wrote the manuscript. All authors reviewed/edited the manuscript for important intellectual content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The UK Biobank was approved by the North West Research Ethics Committee (06/MRE08/65) and all participants signed an informed consent.
Consent for publication
Not applicable.
Competing interests
No disclosure was reported.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Figure S1.
Flow chart of study participants. Figure S2. Association of glucosamine use and the risk of gout stratified by potential risk factors in males. Table S1. Single nucleotide polymorphisms used to build the genetic risk score for gout.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Liu, M., Ye, Z., Zhang, Y. et al. Associations of habitual glucosamine supplementation with incident gout: a large population based cohort study. Biol Sex Differ 13, 52 (2022). https://doi.org/10.1186/s13293-022-00461-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13293-022-00461-z