Abstract
Cartilage, an important connective tissue, provides structural support to other body tissues, and serves as a cushion against impacts throughout the body. Found at the end of the bones, cartilage decreases friction and averts bone-on-bone contact during joint movement. Therefore, defects of cartilage can result from natural wear and tear, or from traumatic events, such as injuries or sudden changes in direction during sports activities. Overtime, these cartilage defects which do not always produce immediate symptoms, could lead to severe clinical pathologies. The emergence of induced pluripotent stem cells (iPSCs) has revolutionized the field of regenerative medicine, providing a promising platform for generating various cell types for therapeutic applications. Thus, chondrocytes differentiated from iPSCs become a promising avenue for non-invasive clinical interventions for cartilage injuries and diseases. In this review, we aim to highlight the current strategies used for in vitro chondrogenic differentiation of iPSCs and to explore their multifaceted applications in disease modeling, drug screening, and personalized regenerative medicine. Achieving abundant functional iPSC-derived chondrocytes requires optimization of culture conditions, incorporating specific growth factors, and precise temporal control. Continual improvements in differentiation methods and integration of emerging genome editing, organoids, and 3D bioprinting technologies will enhance the translational applications of iPSC-derived chondrocytes. Finally, to unlock the benefits for patients suffering from cartilage diseases through iPSCs-derived technologies in chondrogenesis, automatic cell therapy manufacturing systems will not only reduce human intervention and ensure sterile processes within isolator-like platforms to minimize contamination risks, but also provide customized production processes with enhanced scalability and efficiency.
Graphical abstract

Similar content being viewed by others
Background
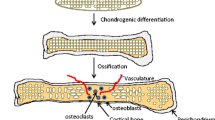
Cartilage is a semi-rigid, load-bearing, avascular connective tissue, formed solely by cells known as chondrocytes. These cells are loosely embedded in an extracellular matrix (ECM) composed predominantly of collagens and, in some cases, elastic fibers, hyaluronan and proteoglycans [1]. Cartilage formation, also known as chondrogenesis, is a dynamic cellular process of a condensed mesenchyme tissue derived from the mesoderm germ layer during embryogenesis. Cartilage represents the fetal precursor tissue for skeletal development. In adults, it persists at almost all joints between bones and in structures that must be deformable as well as strong such as in the respiratory system. Based on the structure and composition of their ECMs, chondrocytes form three different types of cartilage; namely, hyaline cartilage, fibrocartilage and elastic cartilage [2].
Cartilage exhibits diverse clinical aspects and relevance to various medical disciplines, including orthopedics, rheumatology, and respiratory medicine. Cartilage defects are associated with various clinical conditions such as osteoarthritis (OA), rheumatoid arthritis, and cartilage dysplasias [1]. Understanding the clinical significance of cartilage is critical for the development of effective therapeutics and interventions in various healthcare settings. Orthopedic surgeries such as joint arthroplasty and cartilage transplantation are the most commonly used therapeutic interventions for cartilage repair or replacement [3]. However, these surgical interventions are invasive or minimally invasive, and their ability to restore normal joint function, alleviate pain, and improve the quality of life for individuals with cartilage-related issues is limited.
Therefore, it is crucial to develop other non-invasive therapeutic approaches with high safety and efficacy. Theoretically and due to their ability to repair injured tissues, adult stem cells can be a good source for developing therapies for a large number of diseases [4]. Mesenchymal stem cells (MSCs) which can be derived from various tissues such as bone marrow, adipose tissu, placenta, umbilical cord blood, and multiple dental tissues, are multipotent cells that have the potential to differentiate into the mesenchymal lineages including osteocytes, chondrocytes, and adipocytes, as well as other non-mesenchymal lineages, such as cardiomyocytes, astrocytes, neural cells, and endothelial cells [5, 6]. Therefore, extensive efforts have been spent to develop MSCs-based cell therapies for a broad spectrum of diseases, encompassing cartilage and bone diseases, hematological diseases, inflammatory diseases, and graft-versus-host disease [7]. It is important to note that different transcription factors regulate the differentiation of MSCs to different lineages. Chondrogenic differentiation is determined by members the SOX (sex determining region Y (SRY)-related HMG-box) family of transcription factors SOX9, SOX5, and SOX6 while regulation of osteoblast differentiation involve the transcription factors runt-related transcription factor 2 (RUNX2), osterix, and β-catenin [8, 9]. Among the different sources of MSCs, bone marrow-derived MSCs (BM-MSCs) are the most commonly used MSCs in regenerative medicine, particularly for cartilage and bone regeneration [10]. Although significant strides have been taken to improve the chondrogenic differentiation from BM-MSCs and other cell sources, several obstacles persist complicating the achievement of consistent and effective chondrocytes required for clinical application [11]. Several factors may lead to the failure of utilizing BM-MSCs for efficient treatment of cartilage diseases including but not limited to the restricted proliferation capabilities in cultures [12], donor variations, and immunogenicity triggered during culture and cryopreservation [13].
These challenges could be addressed by the induced pluripotent stem cell (iPSC) technology. iPSCs are pluripoent cells which have the capacity for self-renewal and differentiation into almost all cell types [14]. The concept of self-renewal is the ability of the cells to undergo infinite cell divisions without differentiation into other cell types, while pluripotency is the ability of the cells to produce specialized cells of the three embryonic layers: ectoderm, mesoderm, and endoderm [15]. iPSCs can be generated from any type of cells through non-integrating reprogramming method using specific transcription factors known as Yamanaka factors namely, Octamer binding transcription factor 3/4 (OCT3/4), SOX2, Krüppel-like factor 4 (KLF4), and Cellular-Myelocytomatosis c-MYC [15]. Simplicity and reproducibility are the attractive features of the iPSC technology and have attracted the biomedical scientists to generate and differentiate iPSCs from numerous normal and disease-specific cell types for disease modeling and drug screening applications [16]. Syngeneic non-integrated iPSCs and their derivatives have no or minimal immunogenic effect supporting the notion that these cells could be used for cellular therapy without causing harmful immune responses [17]. Therefore, generation of iPSC-derived chondrocytes has become indispensable to advance our understanding of the mechanisms of cartilage-related disorders and represents an important avenue in regenerative medicine. In the following section, we will summarize different strategies developed to differentiate iPSCs into chondrocytes aiming to recapitulate the in vivo microenvironment that support chondrogenesis, and to generate functional and stable iPSC-derived chondrocytes.
Main text
Generation of iPSC-derived chondrocytes
Chondrocytes can be differentiated from iPSCs though different intermediate stages, such as iPSC-derived MSCs (iPSC-MSCs), embryoid bodies (EBs) formation, induction of neural crest cells (NCCs), and primitive streak-mesendoderm and mesodermal lineage. iPSC-MSCs are morphologically highly similar to BM-MSCs and their gene expression profiling is also comparable to that of BM-MSCs [18], and exhibit traits that encompass features of both iPSCs and MSCs. iPSC-MSCs show reduced immunogenicity as compared to iPSCs [19], which renders them appropriate for allogeneic transplantation and enables development of off-the-shelf therapies. Moreover, patient-specific iPSC-MSCs open up the potential for developing personalized medicine for autologous transplantation, in vitro disease modeling, and drug screening [20]. These iPSC-MSCs were reported to differentiate into chondrocytes with growth factors, such as transforming growth factor-beta 3 (TGF-β3) (Fig. 1A). Another commonly used approach to obtain chondrocytes from iPSCs in vitro is through formation of three-dimensional (3D) aggregates of pluripotent stem cells (PSCs) known as embryoid bodies (EBs) (Fig. 1B). The EB has the capacity to generate ectodermal, mesodermal and endodermal cells due to its initiation of a process that resembles gastrulation-like events in embryonic development [21]. Several protocols have been developed under this category with slight variations in the number and concentration of growth factors used, the number of days required and whether an additional step such as differentiation of EBs to MSCs or paraxial mesoderm cells, is needed to differentiate iPSCs to chondrocytes [22]. NCCs are a multipotent group of transient embryonic cells in the vertebrate. They are derived from the ectoderm and differentiate to the peripheral nervous system cells and several non-neural cell types including pigment cells, and the cranio-facial cartilage and bones [23]. Taking the advantage of being multipotent, chondrogenic cells could be differentiated from the NCC-derived MSCs [24] (Fig. 1C). Chondrocytes were also reported to be differentiated from human embryonic stem cells (hESCs) through primitive streak or mesendoderm to mesoderm [25]. Cheng et al. followed this method to differentiate iPSCs to chondrocyte in three short stages using different combination of growth factors in each stage [26] (Fig. 1D). iPSCs can also be differentiated to chondrocytes by co-culture with primary chondrocytes (Fig. 1D). This method is based on the fact that the primary chondrocytes secret paracrine factors which may induce chondrogenic differentiation of the stem cells by closely mimicking the in vivo tissue microenvironment for chondrogenesis [27]. Moreover, co-culture permits crosstalk between the stem cells and the primary chondrocytes influencing chondrocyte development. It facilitates physical contact between different cell types which stabilizes the cellular phenotype and allows for communication of molecular signals involved in chondrogenic differentiation [28].
Schematic representation of the current strategies for in vitro differentiation of iPSCs to chondrocytes. A Via iPSC-derived MSCs. B Via EBs formation. C Via induction of NCCs. D Via primitive streak-mesendoderm and mesodermal lineage. E Via co-culture with primary chondrocytes. BMP4: bone morphogenetic protein 4; BMP7: bone morphogenetic protein 7; CHIR99021: glycogen synthase kinase 3 (GSK-3) inhibitor; DM: dorsomorphin; EB: embryoid body; EGF: epidermal growth factor; FGF2: fibroblast growth factor 2; GDF5: growth/differentiation factor-5; hESC: human embryonic stem cell; iPSC: induced pluripotent stem cell; MSC: mesenchymal stem cell; NCC: neural crest cell; NT4: neurotrophin-4; PDGF: platelet-derived growth factor; PSC: pluripotent stem cell; SB431542: transforming growth factor-beta receptor inhibitor; TGF-β3: transforming growth factor-beta 3; Wnt3a: Wingless/Int1 family member 3A
The above-mentioned studies showed that cartilage cells differentiated from human iPSCs represent a promising tool for regenerative medicine to treat cartilage-related diseases, however some challenges remain. The variability in the quality and characteristics of different iPSC lines affects the efficiency and consistency of chondrogenic differentiation [29]. Since the suspension culture promotes the chondrogenic differentiation and enables removal of non-chondrocytic cells, Yamashita and colleagues reported that homogenous chondrogenic nodules derived from iPSCs cultivated in suspension culture has the potential to form scaffold-free hyaline cartilage in animal models [30]. How to generate homogenous cartilage cells without formation of hypertrophic chondrocytes which have the potential to trigger the process of initiating endochondral ossification in vivo remains the main challenge. Moreover, iPSCs have the potential to form teratomas, therefore it is crucial to ensure complete elimination of undifferentiated iPSCs from chondrogenic cultures to prevent teratoma formation upon transplantation [31]. Obtaining fully mature chondrocytes from iPSCs with a phenotype comparable to native chondrocytes, is challenging [32]. In addition, undesired development of chondrogenic hypertrophy and fibrocartilage in vitro may require modification of the growth factors cocktail used [33]. Due to bovine xenoproteins, use of fetal bovine serum (FBS) in cell culture may induce adverse response in transplant patient upon injection of MSCs [34]. Additionally, there is a risk of infection because of viral and prion contamination [35]. Interestingly, MSC induction in xeno-free conditions may tackle these problems and promote the safety and efficiency of iPSC-MSCs for clinical applications [36].
Genome-edited iPSC-derived chondrocytes
In the last decade, the clustered regularly interspaced short palindromic repeats (CRISPR-Cas9) approach has become an efficient and indispensable tool in biomedical research, and has been extensively explored in bone and cartilage research [37, 38]. It has been used to edit genes associated with chondrogenic differentiation to enhance their expression [39] or to modify signaling pathways involved in chondrogenesis [40]. For example, chondrogenesis can be regulated by the expression of SOX9 and Stat3 [39]. Chondrogenic differentiation of MSCs can be promoted by knocking down the RUNX2, a key transcription factor associated with osteoblast differentiation [41]. Genomic editing in iPSC-derived chondrocytes has been also reported in disease modeling. Efficient editing of cartilage related genes enables to investigate in depth the mechanisms underlying cartilage disorders and to identify potential therapeutic agents [42]. An interesting genome editing study showed simultaneous SOX9 activation and peroxisome proliferator-activated receptor gamma (PPAR-γ) repression in rat BM-MSCs, which promoted chondrocytes differentiation and regeneration of calvarial bone [43]. Various studies have investigated diverse targets for regeneration, paving the way for potential clinical trials in the near future. Genome editing has been employed to boost the regenerative potential of chondrocytes. This may involve editing genes related to ECM production, cell proliferation, or resistance to hypertrophy [41, 44, 45]. Although numerous studies have been reported on the application of genome-edited chondrocytes for in vivo cartilage repair, drug screening, and disease modeling [39, 41, 43], relatively few studies have been conducted specifically on iPSC-derived chondrocytes [40, 46, 47]. It was revealed that mutations in TRPV4 disrupted the bone morphogenetic protein (BMP) signaling pathway in iPSC-derived chondrocytes and blocked formation of hypertrophic chondrocytes providing potential targets for drug development for TRPV4-associated skeletal dysplasias [48]. The existing methods for chondrogenic differentiation from iPSCs may generate heterogeneous cell populations. To resolve this problem, a collagen, type II, alpha 1- green fluorescent protein (COL2A1-GFP) knock-in reporter allele generated by CRISPR-Cas9 system was used to purify the cells. The purified chondroprogenitors exhibited enhanced chondrogenic potential in comparison to unselected groups [40].
Transplantation of allogeneic human iPSC-derived cartilage have shown to be more effective than allogeneic BM-MSC-derived cartilage [49]. However, these cartilage cells can trigger immunological reactions [50]. To overcome this issue, it is necessary to reduce the immunological reactions. The β2 microglobulin, a component of MHC class I molecules, was knocked down in monkey iPSCs before their differentiation into chondrocytes. As expected, the allogeneic iPSC-derived cartilage transplanted in osteochondral defects in monkey knee joints showed increased proliferation of natural killer cells and leukocytes surrounding the knocked down PSC-derived cartilage. This indicates the intricate processes in the immune response of the transplanted allogeneic cartilage in osteochondral defects in vivo [47]. These studies highlight the tremendous advantages of the CRISPR-Cas9 system in understanding the pathogenesis, identification of promising drug targets, and development of feasible treatment interventions for cartilage diseases.
Cartilage organoids formed and differentiated from iPSCs
iPSC-derived cartilage organoids are 3D cell clusters that are created by differentiation of iPSCs in vitro. To support formation of cartilage organoids and their ability to self-renewal and self-organization, a number of biocompatible materials are used, such as Matrigel and synthetic hydrogels [51]. Cartilage organoid technology has been developed to facilitate drug screening through identification of important signaling pathways, recapitulate joint developmental events during embryogenesis and cartilage regeneration. Li and colleagues showed that long-term culturing of hiPSC-derived multi-tissue organoids (MTOs) in E8 medium results in a spontaneous emergence of hyaline cartilage tissues. Moreover, a transcriptome analysis indicated a strong association between the expression of chondrogenic markers in MTOs and fetal lower limb chondrocytes [52]. Another intriguing research demonstrated that subcutaneous implantation of iPSC-derived cartilage microtissues combined with pre-hypertrophic cartilage organoids in nude mice results in formation of both cartilaginous and bony regions [53]. Similarly, O’Connor and colleagues established osteochondral organoids using murine iPSCs through time-dependent sequential exposure of TGF-β3 and BMP2, to mimic natural bone development through the process of endochondral ossification. The generated organoids showed dual tissues consisting of cartilaginous and calcified bony regions [54]. A recent study showed a sequential differentiation process to produce matrix-rich cartilage spheroids from iPSC-MSCs by inducing NCCs in xeno-free environments. Efficient chondrogenic differentiation was induced by a thienoindazole derivative, TD-198946, a small molecule used to enhance differentiation of various human progenitor cells to chondrocytes. No hypertrophy, fibrotic cartilage formation, or dedifferentiation detected in vivo in the generated cartilage spheroids. These chondrogenic spheroids can serve as building blocks for biofabrication of engineered cartilage tissues, as they have the ability to fuse within a short timeframe of a few days [24]. It is worth mentioning that iPSC-derived cartilage organoids have also been reported to recruit osteogenic precursors for bone repair [55]. A recent study has revealed that allogeneic iPSC-derived cartilage organoids transplanted in the knee joints of a primate model of chondral defects integrated with articular cartilage of the host and prevented further degeneration of the surrounding cartilage [49]. These findings open new horizons for development of complex tissue engineered implants to promote zone-specific functionality by using pre-differentiated organoids as building blocks to establish articular cartilage grafts. Even though the research on iPSC-derived cartilage organoids is still in its infancy and creating fully functional cartilage organoids is still challenging, it is evident that they have demonstrated promising applications in drug screening, disease modeling, regeneration, and repair. It is of note that application of 3D bioprinting technology in development of iPSC-derived cartilage organoids can create more complex cartilage organoids and heighten their structural organization [56].
Therapeutic applications of iPSC-derived chondrocytes
Advanced disease modeling
iPSC-derived chondrocytes have been utilized to recapitulate cartilage injuries and diseases in vitro (Table 1). The pluripotency and unlimited self-renewal capacity of the iPSCs make these cells vitally important for disease modeling, which permit us to investigate the mechanisms of various diseases, screen for potential treatment targets, and test therapeutic agents [57]. iPSC-derived disease models for both monogenic and complex cartilage diseases have been developed with more focus on single gene cartilage disorders [58]. Saitta et al. established an iPSC-based in vitro model of skeletal dysplasia to investigate the initial stages of abnormal cartilage formation. Mutations in the calcium channel gene TRPV4 lead to abnormal chondrogenesis during cartilage growth plate differentiation [59]. Isogenic iPSCs with wild-type or mutant NLRP3 have been generated from patients with neonatal-onset multisystem inflammatory disease. Both in vitro and in vivo chondrogenic differentiation were performed. Furthermore, immunodeficient mice that received mutant cartilaginous pellets in vivo experienced disordered endochondral ossification [60]. In vitro models of familial osteochondritis dissecans (FOCD) was developed using both patient BM-MSCs and iPSCs derived from patient fibroblasts to delineate the pathogenesis of this disease. The results showed that chondrogenic pellets with a high glycosaminoglycan (GAG) content but a poor structural integrity. Moreover, dysregulation of matrix production and assembly was evident. These findings show that how studying FOCD iPSC-derived chondrocytes can reveal insights into disease phenotype and pathogenesis offering a new in vitro model of OA and cartilage degeneration [61]. Esseltine et al. [62] converted fibroblasts from patient with oculodentodigital dysplasia (ODDD) into iPSCs, which provided a useful model for investigation of this disease. In this study, the iPSCs showed mutated Cx43 gene, decreased levels of Cx43 mRNA and protein, resulting in impaired channel function. Furthermore, the subcellular localization of Cx43 changed during the chondrogenic differentiation of ODDD-derived iPSCs. This altered localization may have contributed to the more compact cartilage pellet morphology observed in differentiated ODDD-derived iPSCs. Additionally, other research teams successfully developed iPSC-derived disease models for other genetic and complex multifactorial skeletal disorders including type II collagenopathy, fibrodysplasia ossificans progressive (FOP), OA, hand OA, and early-onset finger OA (efOA) [58]. Recently, a novel method was introduced to direct iPSC-derived sclerotome through a sequential transformation in a 3D pellet culture. The generated chondroprogenitors can further be differentiated into articular chondrocytes or, alternatively, transformed into hypertrophic chondrocytes capable of transitioning into osteoblasts. Moreover, distinctive gene expression signatures have been identified at critical developmental stages, highlighting the effectiveness of this system in modeling genetic disorders affecting cartilage and bone [63]. In general, these studies demonstrated that normal chondrogenesis can be recapitulated using an iPSC-derived model, and disease-specific iPSCs exhibit molecular evidence of aberrant chondrogenic developmental processes. These findings may be utilized to develop therapeutic strategies for cartilage-related disorders.
To overcome some limitations of scaffold-based 3D cell culture method, scaffold-free methods showed promising results as well. Nakumora et al. [64] reported efficient fabrication of unified, self-sufficient, and functional cartilaginous constructs by combining iPSCs and bio-3D printers using a Kenzan needle array technology. This approach may facilitate repairing of articular cartilage defects. Zhang et al. [65] established a rapid and efficient approach, employing a 3D rotary suspension culture system, to directly guide iPSC differentiation toward the chondrogenic mesoderm lineage. Subsequently, the research group introduced a tetracycline-controlled BMP4 gene regulation system for iPSCs, linking transcriptional activation of BMP4 with heightened chondrogenesis using the piggyBac (PB) transposon-based gene delivery system. Kotaka and associates used magnetically-labeled iPSCs and an external magnetic force to evaluate the safety and efficacy of magnetic field-mediated delivery of iPSCs for articular cartilage repair in nude rats. The results demonstrated the effectiveness and safety of this approach for in vivo cartilage repair [66].
Drug screening
Surgical interventions are performed to prevent progressing of focal articular cartilage defects [29], however, no effective drugs are available for treatment of cartilage regeneration. Using human MSCs for screening of compounds that promote chondrogenesis has limitations due to limited expansion of MSC passages, variations between donors and the high cost [67]. The development of the iPSC technology and advancement in genome editing approaches provide crucial tools for drug screening by establishing iPSC-derived chondrocytes. Using human iPSCs, a 96-well screening platform was developed to identify chondrogenesis-inducing agents that can be used separately or combined with other techniques for cartilage regeneration and repair. Due to their ability to promote chondrogenesis in vitro and in vivo, AB235 and NB61, two chimeric ligands of Activin/BMP2, were used and tested separately at two different doses for validation of the 96-well chondrogenic screening format. Strikingly, elevated concentrations of each of these two agents resulted in improved chondrogenic differentiation [68]. Another OA drug screening study was conducted on iPSC-derived or native mouse cartilage samples. The inflammatory environment of OA was induced in these cells by interleukin-1α (IL-1α), and a 96-well plate format was used for screening of OA drug candidates. The high-throughput screening revealed that the nuclear factor kappa-light-chain-enhancer of activated B cells (NF-κB) inhibitor SC514 was the most effective drug candidate to reduce cartilage loss induced by IL-1α [69]. Increased mineralization in the FOP-derived iPSCs has been detected, a phenomenon that could be mitigated by the use of the BMP inhibitor DMH1 [70]. It has been demonstrated that statins could effectively rectify the degraded cartilage observed in both chondrogenically differentiated thanatophoric dysplasia type 1 (TD1)- and achondroplasia (ACH)-specific iPSCs [71]. These studies illustrate the potential of iPSCs to provide a suitable platform to identify novel therapeutic agents for cartilage-related disorders and facilitate development of personalized regenerative medicine.
Preclinical studies
Chondrocytes derived from iPSCs have demonstrated great promise in a variety of regenerative medicine applications, especially in relation to cartilage regeneration and repair [49, 64, 72]. These cells offer regenerative treatments for diseases such as OA and cartilage injuries (Table 1). They can be combined with biomaterial scaffolds or scaffold-free methods to create engineered cartilage grafts for transplantation [73]. Generation of cartilage tissues from patient-specific iPSCs reduces the risk of immunological rejection, thus this personalized strategy has a potential for treating diseases such as OA [19]. Before their clinical application, preclinical studies of the iPSC-derived chondrocytes are crucial to assess their viability, functionality, and safety [74]. iPSC-MSCs were used to repair cartilage defects in a rabbit model. Macroscopic and histological assessment revealed more cartilage repair in the experimental group as compared to both the control and scaffold implantation group. Furthermore, no teratoma formation detected in all the three groups indicating the safety and potential of iPSC-MSCs for cartilage regeneration [75]. Ko et al. [76] implanted iPSC-derived chondrocytes in osteochondral defects in immunosuppressed rats. The defects exhibited a significantly higher quality of cartilage repair than in the control. In another study, homogenous cartilaginous particles derived from chondrocyte-specific reporter hiPSC lines were transplanted into joint surface defects in immunodeficient rat and immunosuppressed mini-pig models. The neocartilage survived and integrated into native cartilage, and no tumor formation was observed in all the animal models following the transplantation [30]. The potential of MSC-based therapies is attributed to the release of trophic factors via paracrine signaling, with small extracellular vesicles (sEVs) potentially playing a significant role [77]. Zhu et al. [78] investigated the therapeutic efficacy of exosomes derived from synovial membrane MSCs (SM-MSC-Exos) and iPSC-MSCs (iPSC-MSC-Exos) in treatment of OA. The injected exosomes in an OA mouse model showed that iPSC-MSC-Exos exhibit a stronger therapeutic impact on OA compared to SM-MSC-Exos. Similarly, iPSC-MSC-derived sEVs injected in degenerative discs of intervertebral disc degeneration (IVDD) rat models revealed significant improvement in IVDD and senescence of nucleus pulposus cells of the IVD [79]. Given the poliferative capacity of autologous iPSC-MSCs, these cells ensure a consistent and abundant source of therapeutic sEVs, which could introduce a new therapeutic strategy for OA and IVDD treatment [78, 79]. As previousely mentioned, Nejadnik et al. developed an effective method to directly differentiate human iPSCs (hiPSCs) into MSCs and chondrocytes without the need for EBs formation. Transplantation of these cells in OA rat models successfully repaired the osteochondral defects [33]. However, the traces of fibrocartilage and hypertrophic cartilage detected in the generated chondrocytes in vitro and use of FBS in the chondrogenic medium may prevent their clinical application. Use of Xeno-free media and thorough characterization of hiPSC-derived MSCs and chondrocytes will be essential prior to transplantation [33]. An intriguing study has demonestrated that chondrogenic spheroids derived from iPSC-MSCs retain cartilage phenotype in vivo comparable to the chondrogenic-like tissues generated from the same cell spheroids in vitro. In contrast to spheroids obtained from iPSC-MSCs, distinct bone-like tissue formation was evident in BM-MSC spheroids. This may prove the capacity of iPSC-MSC-derived chondrogenic spheroids to form cartilage-like tissues without endochondral ossification for treatment of cartilage defects in vivo [24]. Additionally, due to the ability of chondrogenic spheroids to fuse rapidly within a short timeframe, they can serve as as building blocks for constructing larger cartilage tissues using techniques like the Kenzan bioprinting method [56]. Current focus tends to shift towards investigating immune reactions in the context of allogeneic cartilage transplantation. Abe and colleagues were the first to conduct allogeneic cartilage transplantation into a primate model using major histocompatibility complex (MHC)-mismatched iPSC-derived cartilage organoids without the need for immunosuppressive drugs [49]. Remarkably, the transplanted organoids exhibited successful engraftment into chondral defects on the knee joint surface of the primate model, demonstrating survival, integration, and remodeling similar to native cartilage, without any observed immune reactions [49]. The findings of these preclinical studies demonstrate effective and clinically translatable approaches for regenerating cartilage tissue using hiPSC-derived MSCs and chondrocytes, offering potential enhancements in cartilage regeneration outcomes in cartilage diseases.
Clinical studies
Over the past decade, iPSCs have shown significant advancements, offering new prospects for personalized cell therapy. Patient-derived iPSCs exhibit a lower risk of rejection compared to allogeneic iPSCs. Therefore, some challenges such as tumorigenicity or immunogenicity must be addressed before the iPSCs can be extensively utilized in clinical therapy. To date, 89 clinical trials referenced under “induced pluripotent stem cells” have been registered on the World Health Organization (WHO)-managed main databases (https://clinicaltrials.gov/, International Clinical Trials Registry Platform (ICTRP), https://trialsearch.who.int/). Several studies from the Japan Primary Registries Network (https://rctportal.niph.go.jp/en) can be added to the list since most of their 21 iPSCs trials are not cross-referenced with the WHO’s platforms. Among the total 110 identified clinical trials, 51 trials were registered as interventional and the remaining as observational. Despite the low rejection risk, slow shifting from autologous to allogenic iPSC-derived therapy approach has been crucial due to the time and cost required for characterization and safety testing of each cell line. Furthermore, allogeneic iPSCs approach allow more time for the testing process, and once an approved cell line is established, it can be used to treat multiple patients. Opting for allogeneic cell therapy would result in a readily accessible therapeutic product for interventions [80].
Until recently, pluripotent cell-derived MSCs were not a popular focus in clinical research, with only a small number of studies exploring this area, despite the wide variety of potential tissues that could be produced. Currently, only three clinical trials involving ESC-derived MSCs [81,82,83], and six iPSC-MSCs clinical trials have been reported (Table 2) [84, 85]. It is important to note that from the six clinical trials, cartilage regeneration through iPSC-MSCs was only addressed in two studies. In 2020, the University of Sydney and Cynata Therapeutics conducted phase 1 clinical trial to evaluate the safety, efficacy, and cost-effectiveness of an allogenic MSCs therapy (Cymerus MSCs) for tibiofemoral knee OA [86]. Lately, Cynata Therapeutics has reported that 321 subjects were recruited for the phase 3 SCUlpTOR clinical trial which will start in 2024 for 24 months (Trial ID: ACTRN12620000870954). In the foreseeable future, the phase 1 clinical trial sponsored by the Chinese Nuwacell Biotechnology company will investigate the safety and efficacy of the NCR100 allogenic iPSC-MSCs intra-articular injection for treatment of knee OA (Trial ID: NCT06049342). This is the first Chinese iPSC-derived cell product approved to be used in phase 1 clinical trial following six years of research and development, (https://en.nuwacell.com/news). It is to be noted that a study tried to directly differentiate allogenic iPSCs into chondrocytes without intermediate MSCs differentiation, to treat knee OA as well (Trial ID: jRCTa050190104). The 2020 Japanese interventional trial from Kyoto University was followed by a second observational trial in 2020 for post-treatment evaluation on the subject’s knees (Trial ID: jRCT1050220051).
As a concluding remark, there have been no results regarding cartilage regeneration through iPSC-derived cell therapy in these trials so far. The scarcity of iPSC-MSCs and cartilage-oriented clinical trials indicates significant potential for further advancement and enhancement. Hopefully with the extensively growing iPSCs research, cartilage regeneration for condition such as OA will receive greater attention.
Limitations of iPSC-derived chondrocyte in vitro models
Throughout this review, numerous studies have demonstrated the tremendous advantages offered by iPSC-derived chondrocytes for cartilage research. However, there are some limitations associated with iPSC-derived chondrocyte in vitro models. The first limitation is that the iPSC-derived chondrocytes may show an immature phenotype, and it is still challenging to obtain iPSC-derived chondrocytes with full maturation and stability [87]. The second limitation is the possibility to generate diverse cell populations with variation in maturation stages. This heterogeneity might complicate result interpretation and compromise the validity and reproducibility of experimental results [22]. Due to the potential of iPSCs to form teratomas, residual undifferentiated iPSCs in iPSC-derived cartilage grafts may pose a risk of tumor formation in transplantation studies [88]. Another main challenge is the variability in the efficiency of chondrogenic differentiation among different iPSC lines and even among clones of the same line [31]. Moreover, the culture conditions for differentiation of iPSCs to chondrocytes may not fully replicate the complex microenvironment of native cartilage tissue. The artificial culture conditions can influence cellular behavior and might not fully capture the in vivo physiological and mechanical complexity of chondrocytes [18, 24]. Even though patient-derived iPSCs can potentially reduce the immunological rejection [89], the in vitro differentiation and manipulation processes may introduce foreign antigens, raising concerns about the immunogenicity of the generated chondrocytes [19]. In addition, the ability of iPSC-derived chondrocytes to produce a mature and robust ECM may be limited. The structure and organization of the ECM are essential for the functionality and integrity of cartilage tissue. Therefore, ECM defects may affect the utility of in vitro models [90]. Last, but not the least, the robustness of cartilage in vitro models may be affected by the technical aspects of iPSC maintenance, differentiation, and characterization, which may introduce variability [32]. These limitations illuminate the challenges associated with iPSC-derived chondrocyte in vitro models. Improvement and optimization of chondrogenic differentiation protocols may overcome these limitations and ensure reliable and comparable results across various studies.
Scaling-up of iPSC-derived cells
The potential of iPSC-derived technologies in chondrogenesis, offering significant benefits for OA and other medical conditions, is evident. However, unlocking these benefits encounters hurdles such as limited process understanding, outdated manufacturing techniques, and insufficient automation. Manual manufacturing and quality control processes prove labor-intensive and error prone. To address the anticipated demand for iPSC-derived cells, scalable production methods must be developed to uphold clinical-grade yields and immunomodulatory properties. Moreover, research indicates that human iPSCs might present an epigenetic edge compared to adult stem cells in producing chondrocytes on a large scale without a tendency towards hypertrophy. Ko and his team showcased heightened expression of key chondrogenic markers such as SOX9, COL2A1, and aggrecan (ACAN), alongside decreased levels of hypertrophic markers like COL10A1 and RUNX2 in iPSC-derived chondrocytes when compared to BM-MSC pellets [76].
It is crucial to establish robust protocols for large-scale iPSC production to support tasks like cell banking. Thorough evaluations of iPSC-derived chondrocytes in large-scale production settings are essential for consistent quality outcomes and to tackle the challenge of spontaneous differentiation. Closing the gap between research and clinical application necessitates the development of scaled production technologies spanning from initial seeding to final fill-and-finish stages. Embracing full automation in iPSCs cell therapy manufacturing and quality control is paramount for enhancing both product quality and production efficiency in this rapidly evolving field [91]. A recent study developed hiPSC-derived limb bud mesenchymal cells (ExpLBM cells) with strong chondrogenic potential and stable proliferation. Using a stirred bioreactor, this method outperformed conventional culture plate methods by yielding significant cartilage tissue with just 1 × 106 cells. This produced significant amounts of cartilaginous particles, suggesting a scalable method for cartilage regeneration without immune rejection. This efficient approach requires minimal cell quantities and offers potential scalability through adjustments in medium volume and cell numbers [92]. Another recent study has introduced GelMA microcarriers developed via step emulsification microfluidic devices as a degradable platform for amplifying iPSC-MSCs in scalable bioreactors, while maintaining typical MSC traits and immune-modulatory capabilities. These GelMA microcarriers, manufactured with efficiency and reproducibility in mind, facilitate substantial expansion of iPSC-MSCs (up to 16 times within 8 days) in vertical wheel bioreactors, with a post-digestion viability exceeding 95%. When compared to monolayer culture, iPSC-MSCs expanded on GelMA microcarriers exhibit at least similar, if not superior, immune-modulatory potential. This approach marks a notable progression in producing immune-modulatory iPSC-MSCs, providing scalability, cost-efficiency, and simplified cell retrieval through direct dissolution of microcarriers, thereby minimizing cell wastage [93].
A novel, good manufacturing practice (GMP)-compliant scalable manufacturing procedure is introduced for the fabrication of iPSC-MSCs, tackling the aforementioned hurdles. By employing xenogeneic-, serum-, and feeder-free conditions, alongside chemically defined maintenance for iPSCs, the process eliminates the necessity for murine feeders and accomplishes mesoderm induction, resulting in heightened performance of MSCs in immunopotency assessments. The manufacturing process comprises three phases: iPSC banking, iPSC expansion and differentiation into MSCs, and MSC expansion and formulation of the final clinical product. Impressively, one vial of iPSCs can yield an average of 3.2 × 1010 MSCs, and the complete iPSC bank has the potential to generate 2.9 × 1015 MSCs, equating to 29 million clinical doses, each containing 1 × 108 MSCs. This method presents a promising resolution to the challenges of supply, scalability, and consistency in iPSC-MSC production, paving the way for their utilization in clinical applications with heightened efficacy and safety. This optimized manufacturing process for iPSC-MSCs has been applied in treating steroid-resistant acute graft versus host disease (SR-aGvHD) in a phase 1 clinical trial but could be similarly employed in the iPSC-MSCs-Chondrocyte approach for chondrogenesis [84].
The aim of automating cell therapy manufacturing is to reduce human intervention, ensuring sterile processes within isolator-like platforms to minimize contamination risks. Despite notable advancements, challenges persist, including difficulties in executing specific biological procedures with robotic assistance, prompting the need for exploring new solutions and standardization. Establishing an automated manufacturing platform requires precise definition of process parameters and configurations through validated standard operating procedures (SOPs). To address these needs, an advanced automated cell manufacturing platform was employed to produce both equine and human iPSC-MSCs via EBs [94]. These iPSC-MSCs were further demonstrated their ability to differentiate into adipogenic, osteogenic, and chondrogenic lineages proficiently. The main goal of this study was to develop a simplified and uniform procedure for isolating MSCs from peripheral blood under GMP conditions, ensuring their viability and purity. Compared to existing protocols documented in the literature, this approach offers simplicity, scalability and consistently delivering robust cell purity [94]. Recently, another automatic system was reported to produce iPSC-derived therapies, covering a range of cell types including iPSC-MSCs, iPSC-derived chondrocytes, and extracellular vesicles [95]. iPSC expansion and differentiation into MSCs and chondrocytes take place in plates, while expansion of iPSC-derived MSCs and production of extracellular vesicles utilize microcarriers within stirred tank bioreactors. The system is designed to oversee iPSC expansion, differentiation, and the fill and finish of the products. Furthermore, this platform including a range of quality control assays such as microscopy, cell counting, viability assessment, qPCR, and endotoxin assays, aims to address these challenges by establishing an automated platform for producing cell therapies specifically targeting OA, and serves as an example of how existing automation technology can be customized and improved to enhance scalability and efficiency.
Conclusions
Genomic abnormalities detected during the reprogramming and subsequent expansion of iPSCs raised serious safety concerns [96]. Therefore, several factors including starting cell source, method of delivery, reprogramming factor and cell passage, should be taken into consideration for the generation of iPSCs in order to reduce not only genomic instability [97], but also immunogenicity [98, 99].
The field of iPSC-derived cartilages is rapidly evolving, and several approaches and perspectives have been explored to tackle limitations and enhance the potential applications of these cells in regenerative medicine. Development of new or optimization of the current differentiation protocols to improve the maturation and stability of iPSC-derived chondrocytes is critical [25]. This can be achieved by further research on signaling pathways, culture conditions, and other factors that facilitate the maturation of iPSC-derived chondrocytes. It is significantly important to implement cutting-edge 3D culture systems combined with ink-free bioprinting technique to more closely mimic the in vivo microenvironment of cartilage tissue [56]. Using bioreactors, biomimetic scaffolds, 3D bioprinting and other advanced technologies can improve the functional characteristics of iPSC-derived chondrocytes for cartilage repair. Generation of heterogeneous cell populations remains one of the major challenges in development of efficient cartilage grafts [100]. To eliminate undesired cells and promote the homogeneity of iPSC-derived chondrocyte populations, sustained development of precise genome editing tools is quite essential. Moreover, it is necessary to identify the sources of heterogeneity in iPSC-derived chondrocyte populations to reduce variability and improve reproducibility [101]. Tumorigenicity associated with residual undifferentiated iPSCs can be addressed by advancements in purification methods and genetic modifications to increase the safety of iPSC-derived chondrocytes for clinical applications [102]. Moreover, scalability and cost-effectiveness of the methods used for generation of iPSC-derived chondrocytes should be improved by simplifying the differentiation protocols, optimizing culture conditions, and utilizing automation technologies [95]. Additionally, it is very crucial to enhance the development of in vivo models to investigate the safety and efficacy of iPSC-derived chondrocytes in preclinical studies [103]. Successful preclinical studies should be followed by well-designed clinical trials in patients with cartilage-related disorders. Furthermore, for personalized regenerative medicine, the design of preclinical and clinical trials should focus on the integration of patient-specific iPSCs with advanced gene editing technologies and highly efficient chondrogenic differentiation protocols. These future perspectives reflect the continuous endeavors to harness the full potential of iPSC-derived chondrocytes, opening the door for innovative approaches in cartilage regeneration and repair. Since this field is advancing rapidly, interdisciplinary collaborations and advancement in technologies will play a vital role in shaping the future of iPSC-based cartilage regeneration research.
Abbreviations
- 2D:
-
Two dimentional
- 3D:
-
Three dimentional
- ACH:
-
Achondroplasia
- BM-MSCs:
-
Bone marrow-derived Mesenchymal stem cells
- BMP2:
-
Bone morphogenetic protein 2
- BMP4:
-
Bone morphogenetic protein 4
- CBMC:
-
Umbilical cord blood mononuclear cell
- c-MYC:
-
Cellular-Myelocytomatosis
- COL2A1:
-
Collagen, type II, alpha 1
- COL2A1-GFP:
-
Collagen, type II, alpha 1-green fluorescent protein
- CRISPR:
-
Clustered regularly interspaced short palindromic repeats
- CS:
-
Chitosan
- DMH1:
-
Dorsomorphin homolog 1
- EBs:
-
Embryoid bodies
- ECM:
-
Extracellular matrix
- efOA:
-
Early-onset finger osteoarthritis
- FOP:
-
Fibrodysplasia ossficans progressive
- GMP:
-
Good manufacturing practice
- hESCs:
-
Human embryonic stem cells
- hiPSCs:
-
Human induced pluripotent stem cells
- HOA:
-
Hand osteoarthritis
- ID:
-
Identification number
- iPSCs:
-
Induced pluripotent stem cells
- IVDD:
-
Intervertebral disc degeneration
- KLF4:
-
Krüppel-like factor 4
- KOA:
-
Knee osteoarthritis
- MCDS:
-
Metaphyseal chondrodysplasia type Schmid
- MED:
-
Multiple epiphyseal dysplasia
- MSCs:
-
Mesenchymal stem cell
- N/A:
-
Not applicable
- NCCs:
-
Neural crest cells
- NF-κB:
-
Kappa-light-chain-enhancer of activated B cells
- NHEKs:
-
Normal human epidermal keratinocytes
- OA:
-
Osteoarthritis
- OCT3/4:
-
Octamer binding transcription factor 3/4
- PBMCs:
-
Peripheral blood mononuclear cells
- PSCs:
-
Pluripotent stem cells
- RUNX2:
-
Runt-related transcription factor 2
- sEVs:
-
Small extracellular vesicles
- SOPs:
-
Standard operating procedures
- SOX:
-
SRY-related high mobility group box
- SRY:
-
Sex determining region Y
- TD1:
-
Thanatophoric dysplasia type 1
- TGF-β3:
-
Transforming growth factor-beta 3
References
Krishnan Y, Grodzinsky AJ. Cartilage diseases. Matrix Biol. 2018;71–72:51–69.
Sha’ban M. Histology and biomechanics of cartilage. Cartil Tissue Knee Jt Biomech [Internet]. Elsevier; 2024 [cited 2024 Feb 9]. pp. 25–35. Available from: https://linkinghub.elsevier.com/retrieve/pii/B9780323905978000013
Tokgoz E, Levitt S, Sosa D, Carola NA, Patel V. Robotics applications in total knee arthroplasty. Total knee arthroplasty. Cham: Springer Nature Switzerland; 2023. p. 155–74.
Trounson A, McDonald C. Stem cell therapies in clinical trials: progress and challenges. Cell Stem Cell. 2015;17:11–22.
Pittenger MF, Discher DE, Péault BM, Phinney DG, Hare JM, Caplan AI. Mesenchymal stem cell perspective: cell biology to clinical progress. NPJ Regen Med. 2019;4:22.
Uccelli A, Moretta L, Pistoia V. Mesenchymal stem cells in health and disease. Nat Rev Immunol. 2008;8:726–36.
Squillaro T, Peluso G, Galderisi U. Clinical trials with mesenchymal stem cells: an update. Cell Transpl. 2016;25:829–48.
Nakashima K, Zhou X, Kunkel G, Zhang Z, Deng JM, Behringer RR, et al. The novel zinc finger-containing transcription factor osterix is required for osteoblast differentiation and bone formation. Cell. 2002;108:17–29.
Yoshida CA, Furuichi T, Fujita T, Fukuyama R, Kanatani N, Kobayashi S, et al. Core-binding factor β interacts with Runx2 and is required for skeletal development. Nat Genet. 2002;32:633–8.
Kangari P, Talaei-Khozani T, Razeghian-Jahromi I, Razmkhah M. Mesenchymal stem cells: amazing remedies for bone and cartilage defects. Stem Cell Res Ther. 2020;11:492.
Somoza RA, Welter JF, Correa D, Caplan AI. Chondrogenic differentiation of mesenchymal stem cells: challenges and unfulfilled expectations. Tissue Eng Part B Rev. 2014;20:596–608.
Kim HJ, Park J-S. Usage of human mesenchymal stem cells in cell-based therapy: advantages and disadvantages. Dev Reprod. 2017;21:1–10.
Galipeau J. The mesenchymal stromal cells dilemma—does a negative phase III trial of random donor mesenchymal stromal cells in steroid-resistant graft-versus-host disease represent a death knell or a bump in the road? Cytotherapy. 2013;15:2–8.
Takahashi K, Yamanaka S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell. 2006;126:663–76.
Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K, et al. Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell. 2007;131:861–72.
Karagiannis P, Takahashi K, Saito M, Yoshida Y, Okita K, Watanabe A, et al. Induced pluripotent stem cells and their use in human models of disease and development. Physiol Rev. 2019;99:79–114.
Guha P, Morgan JW, Mostoslavsky G, Rodrigues NP, Boyd AS. Lack of immune response to differentiated cells derived from syngeneic induced pluripotent stem cells. Cell Stem Cell. 2013;12:407–12.
Guzzo RM, Gibson J, Xu R, Lee FY, Drissi H. Efficient differentiation of human iPSC-derived mesenchymal stem cells to chondroprogenitor cells. J Cell Biochem. 2013;114:480–90.
Diekman BO, Christoforou N, Willard VP, Sun H, Sanchez-Adams J, Leong KW, et al. Cartilage tissue engineering using differentiated and purified induced pluripotent stem cells. Proc Natl Acad Sci. 2012;109:19172–7.
Walters-Shumka JP, Sorrentino S, Nygaard HB, Willerth SM. Recent advances in personalized 3D bioprinted tissue models. MRS Bull. 2023;48:632–42.
Schell JP. Spontaneous differentiation of human pluripotent stem cells via embryoid body formation. Hum stem cell man. Elsevier; 2012. p. 363–73.
De Kinderen P, Meester J, Loeys B, Peeters S, Gouze E, Woods S, et al. Differentiation of Induced pluripotent stem cells into chondrocytes: methods and applications for disease modeling and drug discovery. J Bone Miner Res. 2020;37:397–410.
Gammill LS, Bronner-Fraser M. Neural crest specification: migrating into genomics. Nat Rev Neurosci. 2003;4:795–805.
Zujur D, Al-Akashi Z, Nakamura A, Zhao C, Takahashi K, Aritomi S, et al. Enhanced chondrogenic differentiation of iPS cell-derived mesenchymal stem/stromal cells via neural crest cell induction for hyaline cartilage repair. Front Cell Dev Biol. 2023;11:1140717.
Oldershaw RA, Baxter MA, Lowe ET, Bates N, Grady LM, Soncin F, et al. Directed differentiation of human embryonic stem cells toward chondrocytes. Nat Biotechnol. 2010;28:1187–94.
Cheng A, Kapacee Z, Peng J, Lu S, Lucas RJ, Hardingham TE, et al. Cartilage repair using human embryonic stem cell-derived chondroprogenitors. Stem Cells Transl Med. 2014;3:1287–94.
Aung A, Gupta G, Majid G, Varghese S. Osteoarthritic chondrocyte–secreted morphogens induce chondrogenic differentiation of human mesenchymal stem cells. Arthritis Rheum. 2011;63:148–58.
Heng BC, Cao T, Lee EH. Directing stem cell differentiation into the chondrogenic lineage in vitro. Stem Cells. 2004;22:1152–67.
Tsumaki N, Okada M, Yamashita A. iPS cell technologies and cartilage regeneration. Bone. 2015;70:48–54.
Yamashita A, Morioka M, Yahara Y, Okada M, Kobayashi T, Kuriyama S, et al. Generation of scaffoldless hyaline cartilaginous tissue from human iPSCs. Stem Cell Rep. 2015;4:404–18.
Koyama N, Miura M, Nakao K, Kondo E, Fujii T, Taura D, et al. Human induced pluripotent stem cells differentiated into chondrogenic lineage via generation of mesenchymal progenitor cells. Stem Cells Dev. 2013;22:102–13.
Castro-Viñuelas R, Sanjurjo-Rodríguez C, Piñeiro-Ramil M, Hermida-Gómez T, Fuentes-Boquete IM, de Toro-Santos FJ, et al. Induced pluripotent stem cells for cartilage repair: current status and future perspectives. Eur Cell Mater. 2018;36:96–109.
Nejadnik H, Diecke S, Lenkov OD, Chapelin F, Donig J, Tong X, et al. Improved approach for chondrogenic differentiation of human induced pluripotent stem cells. Stem Cell Rev Rep. 2015;11:242–53.
Hemeda H, Giebel B, Wagner W. Evaluation of human platelet lysate versus fetal bovine serum for culture of mesenchymal stromal cells. Cytotherapy. 2014;16:170–80.
Marcus-Sekura C, Richardson JC, Harston RK, Sane N, Sheets RL. Evaluation of the human host range of bovine and porcine viruses that may contaminate bovine serum and porcine trypsin used in the manufacture of biological products. Biologicals. 2011;39:359–69.
Kamiya D, Takenaka-Ninagawa N, Motoike S, Kajiya M, Akaboshi T, Zhao C, et al. Induction of functional xeno-free MSCs from human iPSCs via a neural crest cell lineage. Npj Regen Med. 2022;7:47.
Fitzgerald J. Applications of CRISPR for musculoskeletal research. Bone Jt Res. 2020;9:351–9.
Vlashi R, Zhang X, Li H, Chen G. Potential therapeutic strategies for osteoarthritis via CRISPR/Cas9 mediated gene editing. Rev Endocr Metab Disord. 2023;25:339.
Mochizuki Y, Chiba T, Kataoka K, Yamashita S, Sato T, Kato T, et al. Combinatorial CRISPR/Cas9 approach to elucidate a far-upstream enhancer complex for tissue-specific Sox9 expression. Dev Cell. 2018;46:794-806.e6.
Adkar SS, Wu C-L, Willard VP, Dicks A, Ettyreddy A, Steward N, et al. Step-wise chondrogenesis of human induced pluripotent stem cells and purification via a reporter allele generated by CRISPR-Cas9 genome editing. Stem Cells. 2019;37:65–76.
Kim HJ, Park JM, Lee S, Cho HB, Park J-I, Kim J-H, et al. Efficient CRISPR-Cas9-based knockdown of RUNX2 to induce chondrogenic differentiation of stem cells. Biomater Sci. 2022;10:514–23.
Lilianty J, Bateman JF, Lamandé SR. Generation of a heterozygous COL2A1 (pG1113C) hypochondrogenesis mutation iPSC line, MCRIi019-A-7, using CRISPR/Cas9 gene editing. Stem Cell Res. 2021;56:102515.
Truong VA, Hsu M-N, Kieu Nguyen NT, Lin M-W, Shen C-C, Lin C-Y, et al. CRISPRai for simultaneous gene activation and inhibition to promote stem cell chondrogenesis and calvarial bone regeneration. Nucl Acids Res. 2019;47:e74–e74.
Bonato A, Fisch P, Ponta S, Fercher D, Manninen M, Weber D, et al. Engineering inflammation-resistant cartilage: bridging gene therapy and tissue engineering. Adv Healthc Mater. 2023;12:2202271.
Farhang N, Davis B, Weston J, Ginley-Hidinger M, Gertz J, Bowles RD. Synergistic CRISPRa-regulated chondrogenic extracellular matrix deposition without exogenous growth factors. Tissue Eng Part A. 2020;26:1169–79.
Dicks A, Wu C-L, Steward N, Adkar SS, Gersbach CA, Guilak F. Prospective isolation of chondroprogenitors from human iPSCs based on cell surface markers identified using a CRISPR-Cas9-generated reporter. Stem Cell Res Ther. 2020;11:66.
Okutani Y, Abe K, Yamashita A, Morioka M, Matsuda S, Tsumaki N. Generation of monkey induced pluripotent stem cell-derived cartilage lacking major histocompatibility complex class I molecules on the cell surface. Tissue Eng Part A. 2022;28:94–106.
Dicks AR, Maksaev GI, Harissa Z, Savadipour A, Tang R, Steward N, et al. Skeletal dysplasia-causing TRPV4 mutations suppress the hypertrophic differentiation of human iPSC-derived chondrocytes. Elife. 2023;12:e71154.
Abe K, Yamashita A, Morioka M, Horike N, Takei Y, Koyamatsu S, et al. Engraftment of allogeneic iPS cell-derived cartilage organoid in a primate model of articular cartilage defect. Nat Commun. 2023;14:804.
Kimura T, Yamashita A, Ozono K, Tsumaki N. Limited immunogenicity of human induced pluripotent stem cell-derived cartilages. Tissue Eng Part A. 2016;22:1367–75.
Crispim JF, Ito K. De novo neo-hyaline-cartilage from bovine organoids in viscoelastic hydrogels. Acta Biomater. 2021;128:236–49.
Li M, Abrahante JE, Vegoe A, Chai YW, Lindborg B, Toth F, et al. Self-organized emergence of hyaline cartilage in hiPSC-derived multi-tissue organoids. Cell Biol. 2021;2014:272481. https://doi.org/10.1101/2021.09.21.461213.
Hall GN, Tam WL, Andrikopoulos KS, Casas-Fraile L, Voyiatzis GA, Geris L, et al. Patterned, organoid-based cartilaginous implants exhibit zone specific functionality forming osteochondral-like tissues in vivo. Biomaterials. 2021;273:120820.
O’Connor SK, Katz DB, Oswald SJ, Groneck L, Guilak F. Formation of osteochondral organoids from murine induced pluripotent stem cells. Tissue Eng Part A. 2021;27:1099–109.
Tam WL, Freitas Mendes L, Chen X, Lesage R, Van Hoven I, Leysen E, et al. Human pluripotent stem cell-derived cartilaginous organoids promote scaffold-free healing of critical size long bone defects. Stem Cell Res Ther. 2021;12:513.
Vignes H, Smaida R, Conzatti G, Hua G, Benkirane-Jessel N. Custom-made meniscus biofabrication. Trends Biotechnol. 2023;41:1467–70.
Singh VK, Kalsan M, Kumar N, Saini A, Chandra R. Induced pluripotent stem cells: applications in regenerative medicine, disease modeling, and drug discovery. Front Cell Dev Biol. 2015. https://doi.org/10.3389/fcell.2015.00002/abstract.
Lach MS, Rosochowicz MA, Richter M, Jagiełło I, Suchorska WM, Trzeciak T. The induced pluripotent stem cells in articular cartilage regeneration and disease modelling: are we ready for their clinical use? Cells. 2022;11:529.
Saitta B, Passarini J, Sareen D, Ornelas L, Sahabian A, Argade S, et al. Patient-derived skeletal dysplasia induced pluripotent stem cells display abnormal chondrogenic marker expression and regulation by BMP2 and TGFβ1. Stem Cells Dev. 2014;23:1464–78.
Yokoyama K, Ikeya M, Umeda K, Oda H, Nodomi S, Nasu A, et al. Enhanced chondrogenesis of induced pluripotent stem cells from patients with neonatal-onset multisystem inflammatory disease occurs via the caspase 1–independent cAMP/protein kinase A/CREB pathway. Arthritis Rheumatol. 2015;67:302–14.
Xu M, Stattin E-L, Shaw G, Heinegård D, Sullivan G, Wilmut I, et al. Chondrocytes derived from mesenchymal stromal cells and induced pluripotent cells of patients with familial osteochondritis dissecans exhibit an endoplasmic reticulum stress response and defective matrix assembly. Stem Cells Transl Med. 2016;5:1171–81.
Esseltine JL, Shao Q, Brooks C, Sampson J, Betts DH, Séguin CA, et al. Connexin43 mutant patient-derived induced pluripotent stem cells exhibit altered differentiation potential. J Bone Miner Res Off J Am Soc Bone Miner Res. 2017;32:1368–85.
Lamandé SR, Ng ES, Cameron TL, Kung LHW, Sampurno L, Rowley L, et al. Modeling human skeletal development using human pluripotent stem cells. Proc Natl Acad Sci. 2023;120:e2211510120.
Nakamura A, Murata D, Fujimoto R, Tamaki S, Nagata S, Ikeya M, et al. Bio-3D printing iPSC-derived human chondrocytes for articular cartilage regeneration. Biofabrication. 2021;13:044103.
Zhang M, Niibe K, Kondo T, Limraksasin P, Okawa H, Miao X, et al. Rapid and efficient generation of cartilage pellets from mouse induced pluripotent stem cells by transcriptional activation of BMP-4 with shaking culture. J Tissue Eng. 2022;13:20417314221114616.
Kotaka S, Wakitani S, Shimamoto A, Kamei N, Sawa M, Adachi N, et al. Magnetic targeted delivery of induced pluripotent stem cells promotes articular cartilage repair. Stem Cells Int. 2017;2017:9514719.
Siddappa R, Licht R, Van Blitterswijk C, De Boer J. Donor variation and loss of multipotency during in vitro expansion of human mesenchymal stem cells for bone tissue engineering. J Orthop Res. 2007;25:1029–41.
Yang S-L, Harnish E, Leeuw T, Dietz U, Batchelder E, Wright PS, et al. Compound screening platform using human induced pluripotent stem cells to identify small molecules that promote chondrogenesis. Protein Cell. 2012;3:934–42.
Willard VP, Diekman BO, Sanchez-Adams J, Christoforou N, Leong KW, Guilak F. Use of cartilage derived from murine induced pluripotent stem cells for osteoarthritis drug screening. Arthritis Rheumatol. 2014;66:3062–72.
Matsumoto Y, Hayashi Y, Schlieve CR, Ikeya M, Kim H, Nguyen TD, et al. Induced pluripotent stem cells from patients with human fibrodysplasia ossificans progressiva show increased mineralization and cartilage formation. Orphanet J Rare Dis. 2013;8:190.
Yamashita A, Morioka M, Kishi H, Kimura T, Yahara Y, Okada M, et al. Statin treatment rescues FGFR3 skeletal dysplasia phenotypes. Nature. 2014;513:507–11.
Chang Y-H, Wu K-C, Ding D-C. Induced pluripotent stem cell-differentiated chondrocytes repair cartilage defect in a rabbit osteoarthritis model. Stem Cells Int. 2020;2020:1–16.
Lammi M, Piltti J, Prittinen J, Qu C. Challenges in fabrication of tissue-engineered cartilage with correct cellular colonization and extracellular matrix assembly. Int J Mol Sci. 2018;19:2700.
Yamashita A, Tsumaki N. Recent progress of animal transplantation studies for treating articular cartilage damage using pluripotent stem cells. Dev Growth Differ. 2021;63:72–81.
Xu X, Shi D, Liu Y, Yao Y, Dai J, Xu Z, et al. In vivo repair of full-thickness cartilage defect with human iPSC-derived mesenchymal progenitor cells in a rabbit model. Exp Ther Med. 2017;14:239–45.
Ko J-Y, Kim K-I, Park S, Im G-I. In vitro chondrogenesis and in vivo repair of osteochondral defect with human induced pluripotent stem cells. Biomaterials. 2014;35:3571–81.
Liang X, Ding Y, Zhang Y, Tse H-F, Lian Q. Paracrine mechanisms of mesenchymal stem cell-based therapy: current status and perspectives. Cell Transpl. 2014;23:1045–59.
Zhu Y, Wang Y, Zhao B, Niu X, Hu B, Li Q, et al. Comparison of exosomes secreted by induced pluripotent stem cell-derived mesenchymal stem cells and synovial membrane-derived mesenchymal stem cells for the treatment of osteoarthritis. Stem Cell Res Ther. 2017;8:64.
Sun Y, Zhang W, Li X. Induced pluripotent stem cell-derived mesenchymal stem cells deliver exogenous miR-105-5p via small extracellular vesicles to rejuvenate senescent nucleus pulposus cells and attenuate intervertebral disc degeneration. Stem Cell Res Ther. 2021;12:286.
Blair NF, Barker RA. Making it personal: the prospects for autologous pluripotent stem cell-derived therapies. Regen Med. 2016;11:423–5.
Yan L, Wu Y, Li L, Wu J, Zhao F, Gao Z, et al. Clinical analysis of human umbilical cord mesenchymal stem cell allotransplantation in patients with premature ovarian insufficiency. Cell Prolif. 2020;53:e12938.
Shin JH, Ryu C-M, Yu HY, Park J, Kang AR, Shin JM, et al. Safety of human embryonic stem cell-derived mesenchymal stem cells for treating interstitial cystitis: a phase I study. Stem Cells Transl Med. 2022;11:1010–20.
Guo B, Duan Y, Li Z, Tian Y, Cheng X, Liang C, et al. High-strength cell sheets and vigorous hydrogels from mesenchymal stem cells derived from human embryonic stem cells. ACS Appl Mater Interfaces. 2023;15:27586–99.
Bloor AJC, Patel A, Griffin JE, Gilleece MH, Radia R, Yeung DT, et al. Production, safety and efficacy of iPSC-derived mesenchymal stromal cells in acute steroid-resistant graft versus host disease: a phase I, multicenter, open-label, dose-escalation study. Nat Med. 2020;26:1720–5.
Rasko JEJ, Patel A, Griffin JE, Gilleece MH, Radia R, Yeung DT, et al. Results of the first completed clinical trial of an iPSC-derived product: CYP-001 in steroid-resistant acute GvHD. Biol Blood Marrow Transpl. 2019;25:S255–6.
Liu X, Robbins S, Wang X, Virk S, Schuck K, Deveza LA, et al. Efficacy and cost-effectiveness of stem cell injections for symptomatic relief and structural improvement in people with tibiofemoral knee OsteoaRthritis: protocol for a randomised placebo-controlled trial (the SCUlpTOR trial). BMJ Open. 2021;11:e056382.
Graceffa V, Vinatier C, Guicheux J, Stoddart M, Alini M, Zeugolis DI. Chasing chimeras–the elusive stable chondrogenic phenotype. Biomaterials. 2019;192:199–225.
Wang Z. Assessing tumorigenicity in stem cell-derived therapeutic products: a critical step in safeguarding regenerative medicine. Bioengineering. 2023;10:857.
Abe K, Tsumaki N. Regeneration of joint surface defects by transplantation of allogeneic cartilage: application of iPS cell-derived cartilage and immunogenicity. Inflamm Regen. 2023;43:56.
Saito T, Yano F, Mori D, Kawata M, Hoshi K, Takato T, et al. Hyaline cartilage formation and tumorigenesis of implanted tissues derived from human induced pluripotent stem cells. Biomed Res. 2015;36:179–86.
Dupuis V, Oltra E. Methods to produce induced pluripotent stem cell-derived mesenchymal stem cells: Mesenchymal stem cells from induced pluripotent stem cells. World J Stem Cells. 2021;13:1094–111.
Fujisawa Y, Takao T, Yamada D, Takarada T. Development of cartilage tissue using a stirred bioreactor and human iPSC-derived limb bud mesenchymal cells. Biochem Biophys Res Commun. 2023;687:149146.
Rogers RE, Haskell A, White BP, Dalal S, Lopez M, Tahan D, et al. A scalable system for generation of mesenchymal stem cells derived from induced pluripotent cells employing bioreactors and degradable microcarriers. Stem Cells Transl Med. 2021;10:1650–65.
Vieira CP, McCarrel TM, Grant MB. Novel methods to mobilize, isolate, and expand mesenchymal stem cells. Int J Mol Sci. 2021;22:5728.
Herbst L, Groten F, Murphy M, Shaw G, Nießing B, Schmitt RH. Automated production at scale of induced pluripotent stem cell-derived mesenchymal stromal cells, chondrocytes and extracellular vehicles: towards real-time release. Processes. 2023;11:2938.
Pera MF. The dark side of induced pluripotency. Nature. 2011;471:46–7.
Yoshihara M, Hayashizaki Y, Murakawa Y. Genomic Instability of iPSCs: challenges towards their clinical applications. Stem Cell Rev Rep. 2017;13:7–16.
Apostolou E, Hochedlinger K. iPS cells under attack. Nature. 2011;474:165–6.
Liu X, Li W, Fu X, Xu Y. The immunogenicity and immune tolerance of pluripotent stem cell derivatives. Front Immunol. 2017;8:645.
Murphy C, Mobasheri A, Táncos Z, Kobolák J, Dinnyés A. The potency of induced pluripotent stem cells in cartilage regeneration and osteoarthritis treatment. In: Turksen K, editor. Cell biology and translational medicine, vol. 1. Cham: Springer International Publishing; 2017. p. 55–68.
Kim IG, Park SA, Lee S-H, Choi JS, Cho H, Lee SJ, et al. Transplantation of a 3D-printed tracheal graft combined with iPS cell-derived MSCs and chondrocytes. Sci Rep. 2020;10:4326.
Okita K, Matsumura Y, Sato Y, Okada A, Morizane A, Okamoto S, et al. A more efficient method to generate integration-free human iPS cells. Nat Methods. 2011;8:409–12.
Lo Monaco M, Merckx G, Ratajczak J, Gervois P, Hilkens P, Clegg P, et al. Stem cells for cartilage repair: preclinical studies and insights in translational animal models and outcome measures. Stem Cells Int. 2018;2018:1–22.
Castro-Viñuelas R, Sanjurjo-Rodríguez C, Piñeiro-Ramil M, Hermida-Gómez T, Rodríguez-Fernández S, Oreiro N, et al. Generation and characterization of human induced pluripotent stem cells (iPSCs) from hand osteoarthritis patient-derived fibroblasts. Sci Rep. 2020;10:4272.
Rim YA, Nam Y, Park N, Jung H, Lee K, Lee J, et al. Chondrogenic differentiation from induced pluripotent stem cells using non-viral minicircle vectors. Cells. 2020;9:582.
Ozaki T, Kawamoto T, Iimori Y, Takeshita N, Yamagishi Y, Nakamura H, et al. Evaluation of FGFR inhibitor ASP5878 as a drug candidate for achondroplasia. Sci Rep. 2020;10:20915.
Rim YA, Nam Y, Park N, Lee K, Jung H, Jung SM, et al. Characterization of early-onset finger osteoarthritis-like condition using patient-derived induced pluripotent stem cells. Cells. 2021;10:317.
Pretemer Y, Kawai S, Nagata S, Nishio M, Watanabe M, Tamaki S, et al. Differentiation of hypertrophic chondrocytes from human iPSCs for the in vitro modeling of chondrodysplasias. Stem Cell Rep. 2021;16:610–25.
Kimura T, Bosakova M, Nonaka Y, Hruba E, Yasuda K, Futakawa S, et al. An RNA aptamer restores defective bone growth in FGFR3-related skeletal dysplasia in mice. Sci Transl Med. 2021;13:eaba4226.
Lee SJ, Nam Y, Rim YA, Lee K, Ju JH, Kim DS. Perichondrium-inspired permeable nanofibrous tube well promoting differentiation of hiPSC-derived pellet toward hyaline-like cartilage pellet. Biofabrication. 2021;13:045015.
Acknowledgements
We thank the support of Institut national de la santé et de la recherche médicale (INSERM), Faculté de médecine et Faculté de chirurgie dentaire de Université de Strasbourg, and Lamina therapeutics. EAMA is financially supported by ANR ARTiTHERA, WO was supported by Chinese Scholarship Council (CSC N° 202309240005). We also thank Servier Medical ART for free medical images.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
EAMA, RS, MM and WO wrote the draft of the manuscript. ZL, ZH, NBJ, JEG and GH revised the manuscript. All authors reviewed and approved the final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ali, E.A.M., Smaida, R., Meyer, M. et al. iPSCs chondrogenic differentiation for personalized regenerative medicine: a literature review. Stem Cell Res Ther 15, 185 (2024). https://doi.org/10.1186/s13287-024-03794-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-024-03794-1