Abstract
Background
Human umbilical cord-derived mesenchymal stem cell (hUC-MSC) sheets have recently attracted attention as an alternative approach to injected cell suspensions for stem cell therapy. However, cell engraftment and cytokine expression levels between hUC-MSC sheets and their cell suspensions in vivo have not yet been compared. This study compares hUC-MSC in vivo engraftment efficacy and cytokine expression for both hUC-MSC sheets and cell suspensions.
Methods
hUC-MSC sheets were prepared using temperature-responsive cell culture; two types of hUC-MSC suspensions were prepared, either by enzymatic treatment (trypsin) or by enzyme-free temperature reduction using temperature-responsive cell cultureware. hUC-MSC sheets and suspensions were transplanted subcutaneously into ICR mice through subcutaneous surgical placement and intravenous injection, respectively. hUC-MSC sheet engraftment after subcutaneous surgical transplantation was investigated by in vivo imaging while intravenously injected cell suspensions were analyzing using in vitro organ imaging. Cytokine levels in both transplant site tissues and blood were quantified by enzyme-linked immunosorbent assay.
Results
After subcutaneous transplant, hUC-MSC sheets exhibited longer engraftment duration than hUC-MSC suspensions. This was attributed to extracellular matrix (ECM) and cell–cell junctions retained in sheets but enzymatically altered in suspensions. hUC-MSC suspensions harvested using enzyme-free temperature reduction exhibited relatively long engraftment duration after intravenous injection compared to suspensions prepared using trypsin, as enzyme-free harvest preserved cellular ECM. High HGF and TGF-β1 levels were observed in sheet-transplanted sites compared to hUC-MSC suspension sites. However, no differences in human cytokine levels in murine blood were detected, indicating that hUC-MSC sheets might exert local paracrine rather than endocrine effects.
Conclusions
hUC-MSC sheet transplantation could be a more effective cell therapeutic approach due to enhanced engraftment and secretion of therapeutic cytokines over injected hUC-MSC suspensions.
Similar content being viewed by others
Introduction
Mesenchymal stem cell (MSC) therapies have been frequently investigated as effective stem cell therapies to address diverse pathologies since MSCs secrete diverse cytokines involved in cell proliferation, neoangiogenesis, inflammatory suppression, and immunoregulation [1,2,3,4,5]. MSCs from various tissues sources, including bone marrow, amniotic fluid, adipose tissue, dental pulp, and umbilical blood are applied in cell therapies [6]. Among these, human umbilical cord-derived mesenchymal stem cells (hUC-MSCs) have attracted recent attention for their higher proliferative capacity and cell viability compared to bone marrow or adipose tissue-derived MSCs [7,8,9,10,11]. Moreover, UC-MSCs secrete higher levels of therapeutic cytokines compared to the other two MSC types [8]. In addition, hUC-MSCs are obtained noninvasively from umbilical cords obtained postnatally as routine tissue discards from childbirth [12].
To exploit numerous MSC therapeutic benefits in vivo, cell administration and transplantation using cell suspension injections, both systemically and locally, and direct tissue transplantation of MSCs within various scaffolds and carriers have been extensively investigated. Nonetheless, administration of MSCs to humans clinically exhibits the requisite safety but generally fails to yield convincing therapeutic benefits observed in preclinical in vitro and in vivo models [7].
Despite over 900 MSC clinical trials describing these MSC delivery strategies for a multitude of different therapeutic goals, results are inconsistent [13], with only 3 human MSC therapies approved for immune-related diseases (i.e., graft-versus-host disease) globally to date (none approved in USA) [14]. Given these long-standing challenges to effective MSC therapies, current standard MSC dosing and administration practices utilizing suboptimal injection-based delivery of “naïve” (i.e., heterogeneous, non-standardized) MSC suspensions or carrier-based constructs, both autologous and allogenic, should be reconsidered and redesigned around critical quality attributes and delivery methods [15,16,17,18,19,20,21].
MSC sheets—contiguous, robust, viable monolayers of cultured MSCs—have been reported as an alternative implantable cell therapy delivery system [22,23,24,25]. Cell sheets are fabricated using thermoresponsive poly(N-isopropylacrylamide) (PNIPAAm)-modified commercial cell culture surfaces. PNIPAAm exhibits reversible hydration/dehydration changes in response to cell culture temperatures near 37°C [26,27,28,29,30,31,32,33,34,35,36,37], facilitating cell harvesting from culture as versatile single, scaffold-free sheets useful for cell therapy and tissue engineering [38,39,40,41,42,43,44,45]. Cell sheets harvested without use of destructive enzymes retain functional cell–cell junctions and endogenous extracellular matrix (ECM), unlike cells recovered using trypsin digestion [40]. Furthermore, sheets are readily handled and transplanted into patients, either ectopically or orthotopically without suturing, exploiting innate tissue adhesion enabled by sheet ECM.
MSC sheet transplantation is interesting for regenerative medicine applications due to known enhanced production of therapeutic cytokines over MSC suspensions [23, 46,47,48]. Most MSC sheet applications have used bone marrow- or adipose tissue- derived MSC sheets; UC-MSCs are more recently reported in MSC sheets. hUC-MSC sheets have been characterized in vitro by observing cellular microstructures, ECM, cell–cell junctions, cell–ECM junctions, layered sheet constructs, and various cytokine and chemokine production [49,50,51,52,53]. Further, hUC-MSC sheet interactions with tissue culture surfaces have been investigated in vitro [8]. Despite increasing hUC-MSC sheet in vitro analysis, hUC-MSC sheet tissue interactions after transplantation in vivo, including sheet engraftment behavior and in situ cytokine secretion critical to their therapeutic relevance, has not yet been reported.
The aim of this study was to compare hUC-MSC sheets and two types of analogous cultured hUC-MSC suspensions in vivo in a murine subcutaneous tissue site to elucidate their respective in vivo therapeutic signals via local cell engraftment and cytokine production.
Materials and methods
Human umbilical cord MSC culture
Human MSCs derived from umbilical cord Wharton’s jelly were obtained from PromoCell (Heidelberg, Germany). hUC-MSCs were cultured in Dulbecco’s modified Eagle’s medium (DMEM) (Gibco, Waltham, MA, USA) supplemented with 10% fetal bovine serum, 1% MEM nonessential amino acids, 1% GlutaMAX, 100 units/mL penicillin, and 100 μg/mL streptomycin. hUC-MSCs were incubated at 37°C with 5% CO2 in a humidified chamber and passaged after cells reached confluence on 10-cm-diameter culture dishes (Thermo Fisher Scientific, Waltham, MA, USA). In passage culture, hUC-MSCs were recovered through a digestive proteolytic enzyme (TrypLE, Gibco) treatment for 5 min and seeded into other standard tissue culture dishes (Thermo Fisher Scientific) at a density of 4000–6000 cells/cm2; hUC-MSCs at passage 3–6 were used in this study.
Preparation of hUC-MSC sheets and suspensions
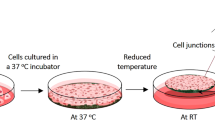
hUC-MSC sheets were prepared by the following procedure (Fig. 1): Cultured hUC-MSC were recovered from conventional 10-cm-diameter culture dishes using TrypLE treatment for 5 min. Then, recovered hUC-MSCs were seeded into 35-mm-diameter temperature-responsive culture dishes (UpCell™, CellSeed, Tokyo, Japan) at a density of 2 × 105 cells/dish. Next, hUC-MSCs were incubated until confluency for 5 days in DMEM before moving these culture dishes to an incubator set at 20°C, and incubating for 30 min. At this point, the hUC-MSC sheets spontaneously release from the culture surfaces and are recovered from these dishes as single units [54]. Cell sheets contained approximately 4 × 105 cells [8].
Schematic illustration for preparing (A) a human umbilical cord-derived mesenchymal stem cell sheet using a temperature-responsive cell culture dish; (B) a conventional cell suspension after enzyme treatment; and (C) a cell suspension by temperature treatment in a temperature-responsive cell culture dish; (D) transplantation of cell sheets or two different cell suspensions to the mouse.
Two types of hUC-MSC suspensions were prepared as follows: hUC-MSCs were seeded on conventional 35-mm-diameter cell culture dishes (Thermo Fisher Scientific) and incubated using DMEM for 5 days until confluency. Then, hUC-MSC suspensions were recovered from culture using 0.05% trypsin for 5 min. This harvested cell suspension was called as “enzyme treatment (ET).” Another cell suspension was seeded in 10-cm-diameter temperature-responsive cell culture dishes (UpCell™) in DMEM and incubated for 48 h (i.e., below cell confluence). Then, hUC-MSC suspensions were recovered from these dishes by changing culture temperature from 37°C to 20°C. Individual cells were released from these surfaces after 30 minutes and collected. This recovered cell suspension was called “temperature reduction (TR).” Cell counts in each suspension were approximately 4 × 105 cells.
Subcutaneous transplantation of hUC-MSC sheets and cell suspensions
The reporting of all animal experiments adheres to the ARRIVE guidelines. The Institutional Animal Care and Use Committee at Keio University approved this procedure. Female Crl:CD1 (ICR) mice (6–8 weeks old, Japan SLC, Hamamatsu, Japan) were used in this study. A murine disease model is frequently used to monitor and validate therapeutic efficacy of the transplanted cells; however, in this study we used a healthy mouse transplant model. This is because this study sought to compare in vivo survival and in vivo cytokine production of hUC-MSC sheets and two types of hUC-MSC suspensions, and not to assess any therapy or disease efficacy. Therefore, murine cell transplant experiments used healthy instead of diseased murine models in order to eliminate factors that might otherwise possibly confound interpretation of cell transplantation effects only. Mice were housed in a specific pathogen-free facility and fed alfalfa-free food (AIN-76A Rodent Diet, D10001; Research Diets, New Brunswick, USA) during the week before transplantation to reduce tissue autofluorescence sourced from the feed. The locations of all mouse cages were randomized to avoid confounding bias.
In this investigation, the following two forms of hUC-MSC transplantation were performed: intravenous cell suspension injection and subcutaneous sheet transplantation (Fig. 2). Three different transplantation groups—hUC-MSC sheets, ET hUC-MSC suspensions, and TR hUC-MSC suspensions—were transplanted subcutaneously (Fig. 2A). An additional sham control group was used. Two transplantation groups—ET hUC-MSC suspensions and TR hUC-MSC suspensions—were performed through intravenous injection (Fig. 2B). To assess the effectiveness of cell engraftment and cytokine expression, eight mice were employed per group, established by accounting for the reduction of errors related to individual variations in mice. For the duration of the cell transplant trial, a total of 48 mice were used. To prevent confounding bias, the placement of each mouse cage was randomized following cell transplantation.
hUC-MSC sheets were stained with fluorescent dye XenoLight DiR (DiIC18(7))(1,1′-dioctadecyltetramethylindotricarbocyanine iodide, Caliper Lifesciences, Hopkinton, USA) after 1-h incubation. Both hUC-MSC suspensions were stained with this same dye by a 30-min incubation. The difference in cell staining duration is due to different stain uptake efficiencies between cell sheet and cell suspension. hUC-MSC suspensions were stained with a fluorescent dye for 30 min, sufficient for saturated staining of the cell suspension in vivo. By contrast, cells within cell sheets do not stain consistently with fluorescent dye when compared with cell suspensions. Therefore, a longer staining duration (60 min) is required for saturated staining of cell sheets. This change in staining does not influence resulting fluorescent intensities because each fluorescent intensity is maximally saturated with each staining duration.
hUC-MSC sheet transplantation was performed using the following procedure. An ICR mouse was anesthetized with somnopentyl and the hair on its back removed. Then, an incision in the dorsal skin was lifted to expose the subcutaneous tissue. One side of a silicone membrane was sutured to the interior surface of the exposed skin. The fluorescently labeled hUC-MSC sheet was placed between the skin and the fixed silicone membrane, and then replaced gently with the membrane directly against the subcutaneous tissue surface, and the incision was closed with 5-0 nylon sutures. After 1 h of transplantation, and at 1, 7, 14, and 28 days, fluorescent images of the mouse were acquired noninvasively using an in vivo imaging system (IVIS Spectrum, Caliper Lifesciences) at 710-nm excitation, 760-nm emission. During image acquisition, the mouse was anesthetized with isoflurane. Images were analyzed using IVIS Living Image (Caliper Lifesciences).
Two types of fluorescently dyed hUC-MSC suspensions, “ET” or “TR” (see Figures 1 and 2), were transplanted into ICR mice in identical subcutaneous locations by subcutaneous injection as follows: ICR mice were anesthetized with isoflurane, and a given cell suspension containing 4 × 105 cells in DMEM was injected into dorsal subcutaneous tissues (Fig. 2A). After 1h of transplantation and at 1, 7, 14, and 28 days, fluorescent images were acquired noninvasively using IVIS in vivo imaging system, identically to the process for imaging cell sheets in vivo.
Two types of fluorescently dyed hUC-MSC suspensions, “ET” or “TR,” was transplanted into ICR mice by intravenous injection as follows: ICR mice were anesthetized with isoflurane, and a cell suspension containing 4 × 105 cells was injected into the tail vein. After transplantation for 60 min, 1, 7, and 14 days, mice were anesthetized with isoflurane and euthanized by cervical dislocation and their organs, brain, heart, kidney, stomach, lungs, spleen, and liver, were collected. Fluorescent images of the collected organs were obtained using IVIS imaging.
Cytokine assay from hUC-MSC sheets and cell suspensions in vivo
Human cytokines secreted by UC-MSCs in the subcutaneous transplant site or in murine plasma were measured by enzyme-linked immunosorbent assay (ELISA). Expression levels of the VEGF (vascular endothelial growth factor), HGF (hepatocyte growth factor), TGF-β1 (transforming growth factor beta 1), IL-10 (interleukin 10), and IL-6 (interleukin 6) were measured by ELISA. At 28 days post-transplantation, each mouse was anesthetized with isoflurane and its blood was collected from cardiac puncture. The mouse was then euthanized via cervical dislocation. The collected blood was centrifuged at 3000 rpm for 10 min, and the supernatant plasma was collected and frozen at − 80 °C until cytokine concentration assay was performed. After blood collection, dorsal subcutaneous tissues were also collected and placed in RIPA buffer (Wako, Osaka, Japan), with a protease inhibitor cocktail (Nacalai Tesque, Kyoto, Japan) added, and minced using scissors. Then, the tissue was sonicated at 4 °C for 10 min and repeated freeze–thawing of the tissue suspension (x3) was conducted to extract proteins, and stored at − 80 °C until cytokine concentration assay. Cytokine concentrations of the prepared plasma and tissue extract media suspension were quantified using a human cytokine ELISA assay kit (R&D Systems, Minneapolis, MN, USA). Protein concentration of each sample for ELISA was normalized by measuring plasma protein concentration with a BCA Protein Assay Kit (Thermo Fisher Scientific). Samples collected from mice without any hUC-MSC transplantation were used as negative control.
Statistical analysis
All values are expressed as average values and standard error (mean ± SEM). Differences were analyzed by Tukey’s test for multiple samples and by the Student’s t test for two groups. *p < 0.05 or **p < 0.01 were considered significant.
Results and Discussion
hUC-MSC engraftment duration in murine subcutaneous transplantation
hUC-MSC sheets and two types of hUC-MSC suspensions were prepared in cultures and harvested using either a commercial temperature-responsive cell culture surface or traditional enzymatic treatment with trypsin (Fig. 1). All MSCs were stained with fluorescence dye and transplanted into the dorsal subcutaneous tissues of ICR mice (Fig. 2A). Engraftment of transplanted hUC-MSC was monitored using an in vivo fluorescent imaging system at 60 min, and at 1, 7, 14, and 28 days (Fig. 3). At 28 days post-transplantation, the dorsal subcutaneous tissues were collected and hUC-MSC engraftment was observed by IVIS imaging (Fig. 3A). At 60 min and 1 day after transplantation, hUC-MSC engraftment was similar across all three MSC transplantation models. These results indicate that transplanted hUC-MSCs can survive in immune-competent murine host subcutaneous tissue at least until 1 day post-transplantation regardless of the cell preparation/implantation method.
Optical evaluation of the engraftment of transplanted mesenchymal stem cell sheets and suspensions prepared from human umbilical cord sources in an ICR mouse. Subcutaneous transplants of human cell sheets and cell suspensions (ET or TR) were performed (see Fig. 2). (A) In vivo imaging of cell survival during cell sheet transplantation and cell suspension injection (ET and TR). (B) A quantitative evaluation of the in vivo fluorescence intensity of transplanted cell sheets and cell suspension (ET or TR)
hUC-MSC sheets were retained continuously in subcutaneous engraftment up to 28 days post-transplantation (Fig. 3A). In contrast, ET MSC suspension injections exhibited decreased engraftment at 7 days, nearly disappearing at 28 days. Similarly, the TR MSC suspension injection also exhibited reduced engraftment over time. Distinct hUC-MSC engraftment duration was attributed to the endogenous MSC ECM and cell–cell junctions known to be retained for hUC-MSC sheet preparations [22, 53]. Improved MSC immunomodulatory properties in sheets versus dispersed cells might also contribute to this improved xenogenic MSC sheet retention [22]. Previously, endothelial and kidney cell sheets were also shown to maintain ECM and adhesive functions after culture recovery, with ECM fibronectin displayed basally under cell sheets [40, 55]. Furthermore, hUC-MSC sheets retain both structure and integrated function, including their ECM, cell–cell junctions, and cell–ECM junctions after culture harvest [49, 53]. This explains the strong spontaneous adhesion and retention in tissue sites without suturing observed for transplanted hUC-MSC sheets. In contrast, ET hUC-MSC suspensions lost both their ECM and cellular activity and could not effectively engraft into host subcutaneous tissue. However, the TR hUC-MSC suspension exhibited higher cell engraftment in vivo than the ET suspension as it retains its endogenous ECM and other surface proteins without proteolytic treatment.
These results support higher in vivo retention duration for xenogenic hUC-MSC sheet implants than both hUC-MSC suspension injections due to sheet integrity, ECM and cell–cell junctions retained from culture and harvest processing, and possibly enhanced MSC sheet immunomodulatory potential with host subcutaneous tissue compared to isolated injected MSCs.
As previous reports have indicated that tumorigenesis from transplanted human mesenchymal stem cells is negligible in an in vivo model [56,57,58,59,60], this risk at 28 days post-transplant was considered to be negligible.
Engraftment duration of hUC-MSCs after intravenous injection
In most clinical cases, MSCs cell suspensions have been introduced via intravenous or direct tissue injection. Thus, the two types of hUC-MSC suspensions were intravenously injected, and MSC engraftment efficiency in various organs was investigated (Fig. 4). For the ET hUC-MSC suspension, at 1 h after intravenous infusion, substantial cell engraftment was observed in the lung, and an even larger fraction in the spleen and liver. At 1 day post-infusion, the number of hUC-MSCs remaining in the lung notably decreased. Up to 7 days post-infusion, hUC-MSCs were present in the lung, spleen, and liver. However, at 14 days post-infusion, most fluorescent hUC-MSCs had cleared, indicating that hUC-MSC ET suspensions would only be present and active primarily in the lung, spleen, and liver up to 7 days post-infusion.
TR hUC-MSC suspension intravenous infusions produced similarly substantial hUC-MSC retention in the lung at 1 h post-infusion, while hUC-MSC presence in other organs was not observed (Fig.4). At 14 days post-infusion, hUC-MSCs were still observed in the lung, indicating that the TR hUC-MSC suspension infusion is retained longer in the lung (14 days) than the ET hUC-MSC suspension (7 days).
Compared with subcutaneous hUC-MSC tissue cell suspension injections, intravenous MSC infusions exhibited relatively low retention duration (compare Figures 3 and 4). Thus, intravenous MSC injection appears to be a less effective hUC-MSC administration or dosing method, similar to low infused MSC tissue site engraftment and retention observed in clinical studies [19].
Cytokine expression level comparisons of transplanted hUC-MSCs
Previous reports consistently indicate that hUC-MSCs secrete various therapeutic cytokines in vitro including HGF and TGF-β1 [8, 23, 24, 50,51,52,53]. However, cytokine secretion after in vivo hUC-MSC transplantation has not been reported. Hence, we measured human cytokine levels at both the MSC transplant tissue site and in blood at 28 days post-transplantation (Figs. 5 and 6). At the subcutaneous transplant site, hUC-MSC sheets exhibited higher HGF and TGF-β1 levels compared to those of both transplanted ET and TR cell suspensions (Fig. 5). This can be explained by higher MSC retention and engraftment duration for hUC-MSC sheets at these tissue sites (Fig. 3). HGF enhances cell viability, proliferation ability, migration capability, and inflammatory suppression [61,62,63,64] and has shown positive effects as treatment for multiple sclerosis and COPD [65, 66]. Thus, possible HGF therapeutic effects might be enhanced by transplantation of hUC-MSC sheets versus MSC suspension injections. In addition, TGF-β1 produces inflammatory suppression by inhibiting macrophage activation and secretion of inflammatory cytokines [61, 67, 68]. Thus, hUC-MSC sheets might better reduce host inflammatory response at cell transplant sites, even better assisting host xenogenic immunomodulation and human MSC tolerance in this murine model, as manifested by enhanced MSC sheet retention and reported sheet immunomodulatory phenotype [22]. In contrast, no obvious difference in human VEGF, IL-10, and IL-6 levels are detected, indicating that neither hUC-MSC sheets nor cell suspensions might be effective in these specific cytokine-mediated in vivo effects.
Human cytokine expression profiles in human MSC transplant sites in mice. Comparisons of subcutaneously transplanted human mesenchymal stem cell sheets and cell suspensions cord (ET or TR), all derived from human umbilical sources. Secreted cytokine levels in the subcutaneous human umbilical cord-derived mesenchymal stem cell sheet transplant site are examined using ELISA. Levels of VEGF, HGF, TGF-β1, IL-10, and IL-6 were measured. The subcutaneous region of sham-treated ICR mice was used as a negative control. (n = 3) * p < 0.05; ** p < 0.01.
Human cytokine expression in murine blood samples after subcutaneous transplants of human umbilical cord-derived mesenchymal stem cell sheets and injected cell suspensions (ET or TR). Secreted human cytokine levels of VEGF, HGF, TGF-β1, IL-10, and IL-6 in blood were evaluated by ELISA. Sham-treated ICR mice were used as a negative control (n = 3)
Human cytokine levels in blood were measured at 28 days after subcutaneous MSC transplantation (Fig. 6). No differences in levels of any tested cytokine between groups are observed, probably because they are either absent, or sufficiently dilute in blood to remain below the ELISA assay detection limit in blood. This indicates that hUC-MSC transplantation affects only the local tissue transplant environment, using paracrine signaling rather than endocrine effects. This result has important implications for possible future applications in MSC cell sheet therapy.
These collective results demonstrate that surgically placed hUC-MSC sheets remain engrafted longer and in higher viable cell numbers in tissue implant sites than injected hUC-MSC suspensions. In addition, hUC-MSC sheets in vivo secrete higher levels of select cytokines to local tissue sites than either injected hUC-MSC suspension. Thus, hUC-MSC sheet transplantation represents an improved alternative approach for enhancing MSC-based cell therapies based on this preclinical murine xeno-transplant in vivo analysis.
Conclusions
We report comparisons for murine subcutaneous engraftment of surgically placed subcutaneous hUC-MSC sheets and injected cell suspensions after transplantation, and resulting select human cytokine secretion profiles in vivo resulting from transplanted hUC-MSC. Subcutaneous hUC-MSC sheets exhibit higher engraftment with longer retention compared to hUC-MSC suspensions prepared either by conventional enzyme treatment or harvested by temperature reduction without trypsin treatment. This difference is attributed to retention of endogenous ECM and cell–cell junctions in sheets but not in suspension forms, and perhaps also improved immunomodulatory properties of human MSC sheets versus their suspensions in this murine xenograft model. Human cytokine secretion from each form of transplanted hUC-MSC to local subcutaneous tissue and to systemic blood circulation was also investigated. Significant amounts of HGF and TGF-β1 were observed in local tissue sites transplanted with hUC-MSC sheets compared to sites bearing either hUC-MSC suspension. This difference may be attributed to longer retention of larger amounts of MSCs in sheet-transplanted sites at assay time points. On the contrary, no intergroup differences were observed in levels of any tested cytokines in blood. This indicates that hUC-MSC transplantation only affects the local tissue environment at transplant sites, using paracrine signals rather than endocrine effects. This result has important implications for possible future applications in MSC cell sheet therapy. If these xenogenic murine cell implant model data reflect human allogenic MSC results, then transplantation of hUC-MSC sheets may offer a more effective therapeutic approach due to enhanced, local MSC engraftment with more substantial, more sustained secretion of human cytokines useful for various cell therapies and regenerative medicine.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- COPD:
-
Chronic obstructive pulmonary disease
- DMEM:
-
Dulbecco’s modified Eagle’s medium
- ECM:
-
Extracellular matrix
- ELISA:
-
Enzyme-linked immunosorbent assay
- ET:
-
Enzyme treatment
- HGF:
-
Hepatocyte growth factor
- hUC-MSC:
-
Human umbilical cord-derived mesenchymal stem cell
- IL-6:
-
Interleukin 6
- IL-10:
-
Interleukin 10
- IVIS:
-
In vivo imaging system
- MEM:
-
Minimum essential medium
- MSC:
-
Mesenchymal stem cells
- PNIPAAm:
-
poly(N-isopropylacrylamide)
- TGF-β1:
-
Transforming growth factor beta 1
- TR:
-
Temperature reduction
- VEGF:
-
Vascular endothelial growth factor
References
Wei X, Yang X, Han Z-P, Qu F-F, Shao L, Shi Y-F. Mesenchymal stem cells: a new trend for cell therapy. Acta Pharmacol Sin. 2013;34:747–54.
Aggarwal S, Pittenger MF. Human mesenchymal stem cells modulate allogeneic immune cell responses. Blood. 2005;105:1815–22.
Song N, Scholtemeijer M, Shah K. Mesenchymal stem cell immunomodulation: mechanisms and therapeutic potential. Trends Pharmacol Sci. 2020;41:653–64.
Margiana R, Markov A, Zekiy AO, Hamza MU, Al-Dabbagh KA, Al-Zubaidi SH, Hameed NM, Ahmad I, Sivaraman R, Kzar HH, Al-Gazally ME, Mustafa YF, Siahmansouri H. Clinical application of mesenchymal stem cell in regenerative medicine: a narrative review. Stem Cell Res Ther. 2022;13:366.
Liu J, Gao J, Liang Z, Gao C, Niu Q, Wu F, Zhang L. Mesenchymal stem cells and their microenvironment. Stem Cell Res Ther. 2022;13:429.
Secunda R, Vennila R, Mohanashankar AM, Rajasundari M, Jeswanth S, Surendran R. Isolation, expansion and characterisation of mesenchymal stem cells from human bone marrow, adipose tissue, umbilical cord blood and matrix: a comparative study. Cytotechnology. 2015;67:793–807.
Guo R, Morimatsu M, Feng T, Lan F, Chang D, Wan F, Ling Y. Stem cell-derived cell sheet transplantation for heart tissue repair in myocardial infarction. Stem Cell Res Ther. 2020;11:19.
Nakao M, Inanaga D, Nagase K, Kanazawa H. Characteristic differences of cell sheets composed of mesenchymal stem cells with different tissue origins. Regen Ther. 2019;11:34–40.
Chetty S, Yarani R, Swaminathan G, Primavera R, Regmi S, Rai S, Zhong J, Ganguly A, Thakor AS. Umbilical cord mesenchymal stromal cells—from bench to bedside. Front Cell Dev Biol. 2022;10:1006295.
Feng H, Liu Q, Deng Z, Li H, Zhang H, Song J, Liu X, Liu J, Wen B, Wang T. Human umbilical cord mesenchymal stem cells ameliorate erectile dysfunction in rats with diabetes mellitus through the attenuation of ferroptosis. Stem Cell Res Ther. 2022;13:450.
Sun Z, Gu P, Xu H, Zhao W, Zhou Y, Zhou L, Zhang Z, Wang W, Han R, Chai X, An S. Human umbilical cord mesenchymal stem cells improve locomotor function in parkinson’s disease mouse model through regulating intestinal microorganisms. Front Cell Dev Biol. 2022;9:808905.
Nagamura-Inoue T, He H. Umbilical cord-derived mesenchymal stem cells: Their advantages and potential clinical utility. World J Stem Cells. 2014;6:195–202.
Shi Y, Wang Y, Li Q, Liu K, Hou J, Shao C, Wang Y. Immunoregulatory mechanisms of mesenchymal stem and stromal cells in inflammatory diseases. Nat Rev Nephrol. 2018;14:493–507.
Wright A, Arthaud-Day ML, Weiss ML. Therapeutic use of mesenchymal stromal cells: the need for inclusive characterization guidelines to accommodate all tissue sources and species. Frontiers in Cell and Developmental Biology. 2021;9:632717.
Wobma HM, Liu D, Vunjak-Novakovic G. Paracrine effects of mesenchymal stromal cells cultured in three-dimensional settings on tissue repair. ACS Biomater Sci Eng. 2018;4:1162–75.
Ferreira JR, Teixeira GQ, Santos SG, Barbosa MA, Almeida-Porada G, Gonçalves RM. Mesenchymal stromal cell secretome: influencing therapeutic potential by cellular pre-conditioning. Front in Immunol. 2018;9:2837.
Galipeau J, Sensébé L. Mesenchymal stromal cells: clinical challenges and therapeutic opportunities. Cell Stem Cell. 2018;22:824–33.
Galipeau J, Krampera M, Leblanc K, Nolta JA, Phinney DG, Shi Y, Tarte K, Viswanathan S, Martin I. Mesenchymal stromal cell variables influencing clinical potency: the impact of viability, fitness, route of administration and host predisposition. Cytotherapy. 2021;23:368–72.
Schrepfer S, Deuse T, Reichenspurner H, Fischbein MP, Robbins RC, Pelletier MP. Stem cell transplantation: the lung barrier. Transplant Proc. 2007;39:573–6.
Yi T, Kim S-N, Lee H-J, Kim J, Cho Y-K, Shin D-H, Tak S-J, Moon S-H, Kang J-E, Ji I-M, Lim H-J, Lee D-S, Jeon M-S, Song SU. Manufacture of clinical-grade human clonal mesenchymal stem cell products from single colony forming unit-derived colonies based on the subfractionation culturing method. Tissue Eng C. 2015;21:1251–62.
Dunn CM, Kameishi S, Grainger DW, Okano T. Strategies to address mesenchymal stem/stromal cell heterogeneity in immunomodulatory profiles to improve cell-based therapies. Acta Biomater. 2021;133:114–25.
Dunn CM, Kameishi S, Cho Y-K, Song SU, Grainger DW, Okano T. Interferon-gamma primed human clonal mesenchymal stromal cell sheets exhibit enhanced immunosuppressive function. Cells. 2022;11:3738.
Imafuku A, Oka M, Miyabe Y, Sekiya S, Nitta K, Shimizu T. Rat mesenchymal stromal cell sheets suppress renal fibrosis via microvascular protection. Stem Cells Transl Med. 2019;8:1330–41.
Kim K, Bou-Ghannam S, Kameishi S, Oka M, Grainger DW, Okano T. Allogeneic mesenchymal stem cell sheet therapy: a new frontier in drug delivery systems. J Control Rel. 2021;330:696–704.
Kondo M, Kameishi S, Grainger DW, Okano T. Novel therapies using cell sheets engineered from allogeneic mesenchymal stem/stromal cells. Emerg Top Life Sci. 2020;4:677–89.
Heskins M, Guillet JE. Solution properties of Poly(N-isopropylacrylamide). J Macromol Sci A. 1968;2:1441–55.
Nagase K, Onuma T, Yamato M, Takeda N, Okano T. Enhanced wettability changes by synergistic effect of micro/nanoimprinted substrates and grafted thermoresponsive polymer brushes. Macromol Rapid Commun. 2015;36:1965–70.
Nagase K, Matsuda J, Takeuchi A, Ikemoto Y. Hydration and dehydration behaviors of poly(N-isopropylacrylamide)-grafted silica beads. Surf Interfaces. 2023;40:103058.
Nagase K, Wakayama H, Matsuda J, Kojima N, Kanazawa H. Thermoresponsive mixed polymer brush to effectively control the adhesion and separation of stem cells by altering temperature. Mater Today Biol. 2023;20:100627.
Nagase K, Inanaga D, Ichikawa D, Mizutani Akimoto A, Hattori Y, Kanazawa H. Temperature-modulated cell-separation column using temperature-responsive cationic copolymer hydrogel-modified silica beads. Colloids Surf B. 2019;178:253–62.
Nagase K. Thermoresponsive interfaces obtained using poly(N-isopropylacrylamide)-based copolymer for bioseparation and tissue engineering applications. Adv Colloid Interface Sci. 2021;295:102487.
Nagase K, Edatsune G, Nagata Y, Matsuda J, Ichikawa D, Yamada S, Hattori Y, Kanazawa H. Thermally-modulated cell separation columns using a thermoresponsive block copolymer brush as a packing material for the purification of mesenchymal stem cells. Biomater Sci. 2021;9:7054–64.
Nagase K, Shimura M, Shimane R, Hanaya K, Yamada S, Akimoto AM, Sugai T, Kanazawa H. Selective capture and non-invasive release of cells using a thermoresponsive polymer brush with affinity peptides. Biomater Sci. 2021;9:663–74.
Nagase K, Okada A, Matsuda J, Ichikawa D, Hattori Y, Kanazawa H. A thermoresponsive cationic block copolymer brush-grafted silica bead interface for temperature-modulated separation of adipose-derived stem cells. Colloids Surf B. 2022;220:112928.
Nagase K, Kojima N, Goto M, Akaike T, Kanazawa H. Thermoresponsive block copolymer brush for temperature-modulated hepatocyte separation. J Mater Chem B. 2022;10:8629–41.
Nagase K, Ota A, Hirotani T, Yamada S, Akimoto AM, Kanazawa H. Thermoresponsive cationic block copolymer brushes for temperature-modulated stem cell separation. Macromol Rapid Commun. 2020;41:2000308.
Nagase K, Uchikawa N, Hirotani T, Akimoto AM, Kanazawa H. Thermoresponsive anionic copolymer brush-grafted surfaces for cell separation. Colloids Surf B. 2020;185:110565.
Yamada, N., Okano, T., Sakai, H., Karikusa, F., Sawasaki, Y., Sakurai, Y., Thermo-responsive polymeric surfaces; control of attachment and detachment of cultured cells, Makromol. Chem., Rapid Commun. 1990; 11: 571-576.
Kikuchi A, Okuhara M, Karikusa F, Sakurai Y, Okano T. Two-dimensional manipulation of confluently cultured vascular endothelial cells using temperature-responsive poly(N-isopropylacrylamide)-grafted surfaces. J Biomater Sci Polym Ed. 1998;9:1331–48.
Kushida A, Yamato M, Konno C, Kikuchi A, Sakurai Y, Okano T. Decrease in culture temperature releases monolayer endothelial cell sheets together with deposited fibronectin matrix from temperature-responsive culture surfaces. J Biomed Mater Res. 1999;45:355–62.
Akiyama Y, Kikuchi A, Yamato M, Okano T. Ultrathin Poly(N-isopropylacrylamide) grafted layer on polystyrene surfaces for cell adhesion/detachment control. Langmuir. 2004;20:5506–11.
Takahashi H, Nakayama M, Yamato M, Okano T. Controlled chain length and graft density of thermoresponsive polymer brushes for optimizing cell sheet harvest. Biomacromolecules. 2010;11:1991–9.
Nagase K, Watanabe M, Kikuchi A, Yamato M, Okano T. Thermo-responsive polymer brushes as intelligent biointerfaces: preparation via ATRP and characterization. Macromol Biosci. 2011;11:400–9.
Nagase K, Yamato M, Kanazawa H, Okano T. Poly(N-isopropylacrylamide)-based thermoresponsive surfaces provide new types of biomedical applications. Biomaterials. 2018;153:27–48.
Nagase K, Okano T, Kanazawa H. Poly(N-isopropylacrylamide) based thermoresponsive polymer brushes for bioseparation, cellular tissue fabrication, and nano actuators. Nano-Struct Nano-Objects. 2018;16:9–23.
Miyahara Y, Nagaya N, Kataoka M, Yanagawa B, Tanaka K, Hao H, Ishino K, Ishida H, Shimizu T, Kangawa K, Sano S, Okano T, Kitamura S, Mori H. Monolayered mesenchymal stem cells repair scarred myocardium after myocardial infarction. Nat Med. 2006;12:459–65.
Kato Y, Iwata T, Morikawa S, Yamato M, Okano T, Uchigata Y. Allogeneic transplantation of an adipose-derived stem cell sheet combined with artificial skin accelerates wound healing in a rat wound model of Type 2 diabetes and obesity. Diabetes. 2015;64:2723–34.
Kaibuchi N, Iwata T, Yamato M, Okano T, Ando T. Multipotent mesenchymal stromal cell sheet therapy for bisphosphonate-related osteonecrosis of the jaw in a rat model. Acta Biomater. 2016;42:400–10.
Nakao M, Kim K, Nagase K, Grainger DW, Kanazawa H, Okano T. Phenotypic traits of mesenchymal stem cell sheets fabricated by temperature-responsive cell culture plate: structural characteristics of MSC sheets. Stem Cell Res Ther. 2019;10:353.
Kim K, Thorp H, Bou-Ghannam S, Grainger DW, Okano T. Stable cell adhesion affects mesenchymal stem cell sheet fabrication: effects of fetal bovine serum and human platelet lysate. J Tissue Eng Regen Med. 2020;14:741–53.
Bou-Ghannam S, Kim K, Kondo M, Grainger DW, Okano T. Mesenchymal stem cell sheet centrifuge-assisted layering augments pro-regenerative cytokine production. Cells. 2022;11:2840.
Thorp H, Kim K, Bou-Ghannam S, Kondo M, Maak T, Grainger DW, Okano T. Enhancing chondrogenic potential via mesenchymal stem cell sheet multilayering. Regen Ther. 2021;18:487–96.
Bou-Ghannam S, Kim K, Grainger DW, Okano T. 3D cell sheet structure augments mesenchymal stem cell cytokine production. Sci Rep. 2021;11:8170.
Okano T, Yamada N, Okuhara M, Sakai H, Sakurai Y. Mechanism of cell detachment from temperature-modulated, hydrophilic-hydrophobic polymer surfaces. Biomaterials. 1995;16:297–303.
Kushida A, Yamato M, Kikuchi A, Okano T. Two-dimensional manipulation of differentiated Madin-Darby canine kidney (MDCK) cell sheets: the noninvasive harvest from temperature-responsive culture dishes and transfer to other surfaces. J Biomed Mater Res. 2001;54:37–46.
Barkholt L, Flory E, Jekerle V, Lucas-Samuel S, Ahnert P, Bisset L, Büscher D, Fibbe W, Foussat A, Kwa M, Lantz O, Mačiulaitis R, Palomäki T, Schneider CK, Sensebé L, Tachdjian G, Tarte K, Tosca L, Salmikangas P. Risk of tumorigenicity in mesenchymal stromal cell–based therapies—bridging scientific observations and regulatory viewpoints. Cytotherapy. 2013;15:753–9.
Tayebi B, Babaahmadi M, Pakzad M, Hajinasrollah M, Mostafaei F, Jahangiri S, Kamali A, Baharvand H, Baghaban Eslaminejad M, Hassani S-N, Hajizadeh-Saffar E. Standard toxicity study of clinical-grade allogeneic human bone marrow-derived clonal mesenchymal stromal cells. Stem Cell Res Ther. 2022;13:213.
Oka M, Kameishi S, Cho Y-K, Song SU, Grainger DW, Okano T. Clinically relevant mesenchymal stem/stromal cell sheet transplantation method for kidney disease. Tissue Eng C. 2023;29:54–62.
Kameishi S, Dunn CM, Oka M, Kim K, Cho Y-K, Song SU, Grainger DW, Okano T. Rapid and effective preparation of clonal bone marrow-derived mesenchymal stem/stromal cell sheets to reduce renal fibrosis. Sci Rep. 2023;13:4421.
Kuramoto G, Hammad IA, Einerson BD, Allshouse AA, Debbink M, Grainger DW, Silver RM, Okano T. Human mesenchymal stem cell sheets improve uterine incision repair in a rodent hysterotomy model. Am J Perinatol. 2022;39:1212–22.
Madrigal M, Rao KS, Riordan NH. A review of therapeutic effects of mesenchymal stem cell secretions and induction of secretory modification by different culture methods. J Transl Med. 2014;12:260.
Benkhoucha M, Santiago-Raber M-L, Schneiter G, Chofflon M, Funakoshi H, Nakamura T, Lalive PH. Hepatocyte growth factor inhibits CNS autoimmunity by inducing tolerogenic dendritic cells and CD25+Foxp3+ regulatory T cells. Proc Natl Acad Sci USA. 2010;107:6424.
Ito W, Kanehiro A, Matsumoto K, Hirano A, Ono K, Maruyama H, Kataoka M, Nakamura T, Gelfand EW, Tanimoto M. Hepatocyte growth factor attenuates airway hyperresponsiveness, inflammation, and remodeling. Am J Respir Cell Mol Biol. 2005;32:268–80.
Rutella S, Bonanno G, Procoli A, Mariotti A, de Ritis DG, Curti A, Danese S, Pessina G, Pandolfi S, Natoni F, Di Febo A, Scambia G, Manfredini R, Salati S, Ferrari S, Pierelli L, Leone G, Lemoli RM. Hepatocyte growth factor favors monocyte differentiation into regulatory interleukin (IL)-10++IL-12low/neg accessory cells with dendritic-cell features. Blood. 2006;108:218.
Bai L, Lennon DP, Caplan AI, DeChant A, Hecker J, Kranso J, Zaremba A, Miller RH. Hepatocyte growth factor mediates mesenchymal stem cell–induced recovery in multiple sclerosis models. Nat Neurosci. 2012;15:862–70.
Kennelly H, Mahon BP, English K. Human mesenchymal stromal cells exert HGF dependent cytoprotective effects in a human relevant pre-clinical model of COPD. Sci Rep. 2016;6:38207.
Wahl SM, Orenstein JM, Chen W. TGF-β influences the life and death decisions of T lymphocytes. Cytokine Growth Factor Rev. 2000;11:71–9.
Niu J, Yue W, Le-Le Z, Bin L, Hu X. Mesenchymal stem cells inhibit T cell activation by releasing TGF-β1 from TGF-β1/GARP complex. Oncotarget. 2017;8:99784.
Acknowledgments
The authors thank Mr. Daimu Inanaga (Keio University) for assistance with ELISA studies.
Funding
This work was partially supported by a Grant-in-Aid for Scientific Research (grant numbers 19H02447, 21KK0199, 22K19899, 18K19938, 20H05233, and 22H04560), from the Japan Society for the Promotion of Science, Japan, a research grant of Terumo Life Science Foundation, and the University of Utah Health Sciences (USA). These funding bodies played no role in the design of the study, the collection, analysis, and interpretation of data, or in writing the manuscript.
Author information
Authors and Affiliations
Contributions
MN and KN conceived the idea for the study, designed the animal experiment, and were aware of the group allocation at the different stages. KN supervised the project. MN, MM, and KN designed the experiments. MN and KN wrote the main manuscript text. KK, NN, DG, TO, and HK extensively reviewed and edited the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
All animal procedures were approved by the Keio University Institutional Animal Care and Use Committee. Project title: Cell sheet transplantation for efficient regenerative therapy. Approved number: 18028. Approved Date: July 8th, 2018.
Consent for publication
Not applicable.
Competing interests
Teruo Okano holds equity in CellSeed, Inc. (Japan) as an investor/developer designated on the patent for temperature-responsive culture surfaces. No other competing financial interests exist. The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nakao, M., Matsui, M., Kim, K. et al. Umbilical cord-derived mesenchymal stem cell sheets transplanted subcutaneously enhance cell retention and survival more than dissociated stem cell injections. Stem Cell Res Ther 14, 352 (2023). https://doi.org/10.1186/s13287-023-03593-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-023-03593-0