Abstract
Background
The appearance of skin scars is known as one of the main side effects of skin burns. Stromal vascular fraction (SVF), as a rich source of cell populations with tissue regeneration properties, plays an important role in the healing of skin lesions. Fractional CO2 lasers have occupied a special place in treating skin lesions, particularly skin scars, since their introduction. Our study aimed to compare the combination of SVF and fractional CO2 laser with fractional CO2 laser alone in the treatment of burn scars.
Method
This double-blind clinical trial study was conducted on ten patients with burn scars that were treated three times with a fractional CO2 laser at site of burn lesions, and one of the two areas studied was randomly injected with SVF. Two months after completion of the procedure, patients' scars were assessed using the Vancouver scar scale (VSS), biometric criteria, and physician and patient satisfaction ratings.
Results
The results confirmed a significant improvement in VSS, cutometry, R7 criteria, complete density sonography, and skin density sonography in the fractional CO2 laser-treated group. The VSS criteria, epidermal thickness sonography, complete density sonography, and skin density sonography in the group treated with the combination of fractional CO2 laser and SVF also showed significant improvement. The VSS criteria and melanin index of Mexameter in the group treated with SVF in combination with fractional CO2 laser were significantly better than the group treated with fractional CO2 laser alone. Also, physician and patient satisfaction in the group treated with SVF injection in combination with fractional CO2 laser was significantly higher than the other group.
Conclusion
The results confirm the efficacy of SVF injection in combination with fractional CO2 laser in the treatment of burn scars and can be considered as a treatment option for better management of these lesions.
Trial registration: The study protocol was retrospectively registered at Iranian Registry of Clinical Trials with code: IRCT20210515051307N1, Registration date: 2021-11-14, URL: https://www.irct.ir/trial/56337.
Similar content being viewed by others
Introduction
The most common causes of skin scars are burns, wounds, striae distensae, and acne. Burns include heat contact, radiation, and chemical or electrical contact that cause damage to the skin or other tissues. Scars caused by burn damage are not only deformed, but also cause shrinkage, hypertrophic changes, and keloid tissue, which can negatively affect quality of life. These scars often result in symptoms such as itching, persistent hyperemia, chronic folliculitis, and limited range of motion [1,2,3,4].
Common treatments for burn scars include silicone gel, pressure dressings, hydration, corticosteroid injections, massage therapy, cryotherapy, and surgery. However, new and advanced methods have been developed to treat burn scars. Lasers, especially fractional and ablative non-fractional lasers, can play an important role in the treatment of scars, especially burn scars [5,6,7]. On the other hand, autologous fat grafting is considered a new and promising method for skin rejuvenation and scar treatment [8].
Adipose tissue is a very complex tissue containing mature fat cells, adipocyte progenitor cells, fibroblasts, pericytes, vascular smooth muscle cells, endothelial cells, monocytes, macrophages, and lymphocytes, i.e., a heterogeneous cell population called stromal vascular fraction (SVF) [9]. The SVF is obtained after processing adipose tissue. Adipose-derived stem cells (ADSC) are isolated and cultured from this heterogeneous cell population, which have the ability to differentiate into mesodermal, ectodermal, and endodermal cells. ADSC stimulate angiogenesis and reduce fibrosis by releasing growth factors, cytokines, proteins, and exosomes, resulting in improved wound healing and scar regeneration [10].
To date, there is no gold standard for the treatment of scar tissue, and treatments are mostly based on the individual experience of physicians with variable success [11].
Moreover, in the treatment of scars and keloid tissue, the combination of several therapeutic interventions has been shown to be more effective than monotherapy [12]. Therefore, given the importance of burn scars and their consequences for patients, combined CO2 fractional laser treatment with SVF is designed as a new treatment option in this study.
Materials and methods
Patients
This study was a double-blind, randomized clinical trial of patients referred to the dermatology clinic from 2021 to 2022. It included ten patients with skin types 1 to 4 who had burn scars at more than one site that had been present for at least three months and were between 25 and 50 years of age. Exclusion criteria included laser treatment in the past three months, pregnancy and breastfeeding, coagulation and platelet disorders, use of anticoagulant medications, diabetes and connective tissue disease, active viral infections, history of malignancy, and use of chemotherapeutic agents. Before the start of the study, all patients were informed about the procedure and completed the informed consent form. Their information such as age, sex, location of the scar, time of its formation, and treatments received were recorded in the questionnaire. All ten participating patients had at least two burn scars on more than one extremity. The type of burn scar was an atrophic burn scar, and its extent varied among each patient. After the initial assessment, the burn scars of all patients was randomly divided into two parts, with one part considered as the intervention area and the other as the control area. The injection area had dimensions of 5 cm in length and width.
Randomization and blinding
The simple randomization method was used for randomization. In this way, two scar areas were randomly named A and B in each patient, and patients were given four sealed envelopes with the letters AS, AL, BS, and BL. The first letter represents the desired area, and the second letter indicates that the procedure can be performed. If the letter S is present, the SVF injection is performed along with the fractional CO2 laser, and if the letter L is present, only the fractional CO2 laser is injected along with normal saline as a placebo. Once the procedure is established, the other area will undergo a different procedure than the specified area. This study is a double-blind clinical trial where the patient and physician evaluate the results, and the statisticians do not know which treatment was used for which lesion. Normal saline was injected as a placebo to blind the patients.
Preparation of SVF
First, 100 cc of fat was removed from the thigh area of each patient. The tissue was then washed with phosphate-buffered saline (PBS) (Miltenyi Biotec, Cologne, Germany) to remove red blood cells and leukocytes. The adipose tissue was digested with collagenase type I (Worthington Biochemical Corp, Lakewood, USA) for 20 min at 37 °C to produce a collagenase solution with a concentration of 0.1%. Enzyme digestion was prevented by washing with DMEM 10% FBS (Invitrogen, Carlsbad, USA), and floating and lysed fat cells were discarded. SVF cells were pelleted by centrifugation at 500g for 10 min. The pellet was resuspended in PBS, and an erythrocyte lysis buffer (Sigma-Aldrich Corp, St. Louis, USA) was added and incubated at 37 °C for 10 min. This cell suspension was centrifuged (500g, 5 min), and SVF cells were counted using an automatic cell counter.
The viability of isolated SVF cells was evaluated in the laboratory using an automatic cell counter. Flow cytometry was performed to analyze the surface marker expression of SVF cells. The data analyses were conducted using Partec—CyFlow ML. Data analysis was carried out using FloMax® software.
CO2 fractional laser settings
Patients were treated in the burn areas with a fractional CO2 laser (SmartXide DOT®, DEKA, USA), choosing a power 13, a stack 2, a spacing 800 µm, and a scanning dwell time 900 microseconds.
Intervention methods
In all patients, CO2 laser alone (together with injection of normal saline as placebo) was performed in one part of the burn scar, and the combination of CO2 laser and SVF injection was performed in the other lesion. The duration of treatment is three sessions, one month apart, as follows: First session: fractional CO2 laser for both lesions with placebo injection in one lesion and SVF in the other lesion, second session: fractional CO2 laser only for both lesions, and the third session: fractional CO2 laser for both lesions accompanied by placebo injection in one lesion and SVF injection in the other.
Assessment method
All patients were examined before the start of the study and two months after completion of the study as described below:
-
1.
Determination of the Vancouver scar scale for both groups, which assesses four characteristics of the lesion, including vascularity, pigmentation, height, and flexibility. According to the items listed in Fig. 1, a score is given for each characteristic.
The sum of all scores is examined to evaluate the improvement of the lesion (Table 1).
Table 1 Vancouver scar scale [13] -
2.
Biometric assessment in both groups before and 2 months after completion of treatment. For this purpose, the following quantitative parameters and a probe with a frequency of 75 Hz were used:
-
Corneometer: to measure tissue hydration (stratum corneum layer).
-
Mexameter: to measure the amount of melanin and erythema of the lesion.
-
Tewameter: to measure transepidermal water loss.
-
Colorimeter: to measure color changes of the skin.
-
Cutometer: to determine the elasticity of the tissue and includes the following parameters:
-
R2: viscoelasticity.
-
R5: pure elasticity.
-
R7: percentage of immediate recovery compared to amplitude after suction.
-
-
3.
Patient and physician satisfaction with treatment in both groups is based on the overall assessment of patients and physicians and includes the options of No Response, Little, Somewhat, Good, and Excellent, which are rated as 0, 1, 2, 3, and 4 points, respectively.
Data analysis
Data were analyzed using SPSS statistical software. Results for quantitative variables were expressed as mean ± SD and for qualitative variables as percentage. Normality of the distribution of variables was checked using the K–S test of the SPSS software, and depending on whether the variable of interest was quantitative or qualitative, it was examined using the Mann–Whitney U test, the Student t test, or the chi-square test between two groups. Numerical values with a p value of less than 5% were considered statistically significant. All data were analyzed using SPSS version 22 software. Regression models were used to test for association with control of confounding factors.
Results
The mean yield of cells was 20 × 106 cells/mL from aspirated 100 cc of fat tissue, and the mean viability of these cells was 81.4%. SVF cell surface markers were evaluated using flow cytometry. The results demonstrated that the isolated SVF cells expressed CD44, CD90, CD105, and CD73 surface markers, while showing minimal expression of hematopoietic cell markers CD34/CD45 (Figs. 2, 3).
The average age of the studied subjects was 31.00 ± 9.67 years. Among the studied subjects, seven subjects (70.0%) were women and the rest were men. In the group treated with fractional CO2 laser, there was a significant improvement between the two groups before and after the procedure in the mean variables of the Vancouver scar scale (7.40 ± 1.35 vs. 5.90 ± 1.97, p value = 0.007), cutometry R7 (0.59 ± 0.17 vs. 0.48 ± 0.13, p value = 0.032), complete density sonography (10.89 ± 6.04 vs. 17.27 ± 8.19, p value = 0.018), and dermal density sonography (7.95 ± 5.29 vs. 14.18 ± 8.46, p value = 0.020) (Figs. 1, 4, 5).
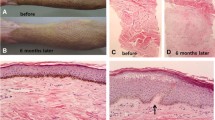
In the group treated with CO2 laser in combination with SVF, there was a significant improvement between the two groups before and after the procedure in the mean Vancouver scar scale variables (7.50 ± 1.35 vs. 4.80 ± 1.03, p value < 0.0001), epidermal thickness sonography (99.00 ± 15.50 vs. 111.50 ± 14.83, p value = 0.016), complete density sonography (12.01 ± 8.71 vs. 21.50 ± 5.97, p value = 0.003), and skin density sonography (9.32 ± 8.23 vs. 17.92 ± 6.40, p value = 0.002) (Figs. 6, 7, 8).
We will now compare in more detail the variables related to burn scar severity between patients treated with fractional CO2 laser and patients treated with SVF injection in combination with fractional CO2 laser. For this comparison, we first considered the primary variables for burn scar severity before the procedure as baseline values (Tables 2, 3, Figs. 9, 10). Figure 9 displays the average variables in the intervention group treated with CO2 fractional laser before and after the intervention. The error bars represent the mean ± standard deviation. Similarly, Fig. 10 presents the average variables in the intervention group treated with SVF alongside CO2 fractional laser before and after the intervention. Again, the error bars represent the mean ± standard deviation.
Comparing the two aforementioned groups, Vancouver scar scale and Mexameter melanin index were significantly better in the group treated with SVF and fractional CO2 laser than in the group treated with fractional CO2 laser only. To this end, the difference between the Vancouver scar scale and Mexameter's melanin index was significant when controlling for the values of before. When controlling the value of Vancouver scar scale before treatment, the mean Vancouver score in SVF group is 1.81 units lower than placebo group (p value = 0.032). When controlling for Mexameter melanin index, the average Mexameter melanin index is 33.69 units higher in the SVF group than in the control group (p value = 0.009) (Fig. 11).
In the group treated with a fractional CO2 laser in combination with SVF, patient and physician assessment scores were higher than in the group treated with a fractional CO2 laser alone, and this difference was significant (Table 4).
Discussion
From the introduction of SVF to the present day, numerous therapeutic applications have been reported, including its effective role in the treatment of retinopathy and nerve regeneration [14, 15], as well as its effective role in the treatment of osteochondral disease and the treatment of myocardial infarction [16, 17]. On the other hand, the use of fractional CO2 lasers is widely applied in dermatology, such as in the treatment of striae distensae [18,19,20,21], atrophic acne scars [22,23,24,25], and burn scars [26,27,28].
Several studies have been performed on the methods used to treat skin scars [1, 5, 8, 9]. Among the methods used to treat skin scars in previous studies, the role of fractional CO2 laser should be mentioned [22, 23, 25, 28, 29]. Previous studies have also mentioned the efficacy of SVF in the treatment of skin scars [30,31,32]. Our study investigated the efficacy of combining the above two methods compared with using fractional CO2 laser alone for burn scars. The results of our study, which was designed as a double-blind clinical trial, showed significant improvement in burn scars in the group treated with fractional CO2 laser based on the average Vancouver scar scale, cutometer R7, complete density sonography, and skin density sonography. On the other hand, in the group treated with fractional CO2 laser along with SVF injection, the improvement of burn scar was significant based on average Vancouver scar scale, epidermal thickness sonography, complete density sonography, and dermal density sonography. And when comparing the above two groups based on the variables of Mexameter melanin index, Vancouver scar scale, and overall patient and physician assessment, the group treated with SVF injection combined with fractional CO2 laser showed a significant difference in burn scar healing.
Comparing the results of the present study with similar studies, a study of facial scars caused by trauma or burns conducted by Gentil et al. in Italy in 2014 showed that 63% of scars had healed in the group treated with SVF after one year, compared with 39% in the control group and 69% in patients treated with platelet-rich plasma (PRP) and nanofat [33].
In our study, the additional injection of SVF to fractional CO2 laser treatment was associated with an improvement in burn scar severity variables, which is consistent with the results of the above study on the role of SVF in the treatment of skin scars, including burn scars.
Other studies have been conducted on the performance of fractional CO2 laser in the treatment of skin scars. In one of these studies, the results of a meta-analysis showed that the fractional CO2 laser significantly improved the Vancouver scar scale score (VSS). Patient and physician scar rating scales also showed significant improvements with fractional CO2 laser treatment. In addition, the fractional CO2 laser significantly decreased the thickness of the scar measured by ultrasound [29]. In our study, the group treated with the fractional CO2 laser showed significant improvement in the Vancouver scar scale, patient global assessment score, and physician global assessment score.
In other results of this study, only R2 index (scar elasticity) in cutometry improved significantly with laser treatment, but measurement of R0 index (scar firmness) showed no significant improvement [29]. In our study, ultrasound and biometric findings are presented in more detail, and complete density sonography, dermal density sonography, and cutometry R7 were evaluated, which confirmed a significant difference after laser treatment.
In our study, the efficacy of SVF was also evaluated. There is an evaluation that was not investigated in the above study. In our study, there was no significant difference in the R2 variable in cutometry in patients before and after laser. This difference might be due to the different nature of the study. In contrast to the aforementioned study, our study was a clinical study, whereas the aforementioned study was a systematic review.
In a 2019 study conducted in South Korea, Kim and colleagues examined a skin defect on a patient's leg that occurred after an accident. The aforementioned lesion was covered by a skin graft, but the resulting scar was prominent and developed into a hypertrophic scar. In this study, the patient was treated with fractional CO2 laser in five sessions, and one month later, he was treated with SVF injection and ablative CO2 laser simultaneously. The result of the examination after one year of follow-up showed that the surface of the scar had been flattened and the pigment deposits had been removed [34]. The results of this study were also consistent with our study on the simultaneous use of fractional CO2 laser and SVF injection in scar healing.
In two separate studies, Lee and his colleagues in South Korea investigated the effect of SVF injection in the surgical treatment of depressed scars. In the first study, 17 patients underwent SVF injection concurrently with surgical scar reduction. In the second study, seven patients underwent scar revision surgery concurrently with SVF injection, and eight patients underwent surgical treatment alone as a control group. The OSAS (Observer Scar Assessment System), SBSES (Stony Brook Evaluation System), VSS (Vancouver Scar Scale), and VAS (Visual Analog Scale) scoring systems were used to evaluate response to treatment. All patients showed significant improvement based on all 4 scoring systems. Patients in the SVF group had a higher cure rate than the non-SVF group on all scoring systems except SBSES. The highest rate of improvement was also seen in scar height and flexibility, whereas a significant change was seen in vascularity [35].
In addition to the above studies, some studies have also investigated the effect of fractional CO2 laser in the treatment of other types of skin scars [22, 23, 25]. Nilforoushzadeh and colleagues compared two treatment methods, including fractional CO2 laser alone and fractional CO2 laser combined with subcision, in the treatment of atrophic acne scars in a clinical trial. In this study, patients with atrophic acne scars were treated with two methods, including fractional CO2 laser alone (5 sessions 3 weeks apart) on the right side of the face and fractional CO2 laser combined with subcision (subcision combined with laser in the first session and 4 fractional CO2 laser sessions 3 weeks apart after 3 weeks) on the left side of the face. Patient satisfaction was measured 6 months after treatment, and side effects were compared in two treatment groups. The results showed that therapeutic efficacy was 54.7% for the combined method and 43% for the fractional CO2 laser alone method. Mean patient satisfaction based on the method VAS (visual analog scale) was 6.6 for the combined method and 5.2 for the laser alone method. Erythema formation was observed with both methods. PIP (Postinflammatory pigmentation) and hyperpigmentation were observed only with the combined method, but after 6 months, complications did not occur in either group. The results show that the combined method achieved more effective results in improving scars and patient satisfaction. The researchers concluded that this method can be used as an efficient treatment method. However, complications such as bruising and hyperpigmentation occurred with this method, which did not occur with laser treatment alone [36]. The above results are in agreement with our study regarding the efficacy of CO2 fractional laser in the treatment of skin scars. On the other hand, it has been pointed out that the simultaneous application of multiple treatment methods is more effective in healing scars. In our study, the results confirmed the more effective use of SVF injection in combination with fractional CO2 laser compared to fractional CO2 laser alone in the treatment of burn scars.
Another study by Khan Ali and his colleagues showed that fractional CO2 laser was more effective than microneedling in reducing patients' acne scar scores. In addition, few side effects occurred with either treatment method. In addition, there was no significant difference in physician and patient satisfaction with either method [37]. The results of this study are consistent with our study regarding the efficacy of CO2 fractional laser in the treatment of skin scars. Therefore, it can be concluded that CO2 fractional laser is effective in the treatment of both burn scars and acne.
In Galal and colleagues' study of 30 patients with acne scars, the two methods of fractional CO2 laser alone and fractional CO2 laser combined with platelet-rich plasma injection (PRP) were compared, and the results of the study showed significant improvement in scar depth on both sides of the patients' faces. However, the simultaneous use of laser and PRP resulted in greater improvement in patients than laser alone. And although 70% of the patients in this study had a dark skin type, no hyperpigmentation was noted in the patients [38]. The results of this study are also consistent with our study in terms of both the efficacy of using fractional CO2 laser in scar treatment and the greater efficacy of the combined treatment compared to laser treatment alone, and in our study, the combined treatment of SVF injection and fractional CO2 laser was a significant difference in improvement in terms of Vancouver scar scale, Mexameter melanin index, patient global assessment score, and physician global assessment score compared to fractional CO2 laser treatment alone.
In the study by Behrangi et al. performed in 2022 on seven patients with acne scar complaints, all patients were treated with SVF injection in one half of the face, while the other half of the face served as a control group. The results of the evaluation after 3 months confirmed a significant improvement in sonographic variables such as skin thickness and total skin thickness compared to baseline values at the beginning of the study. In contrast, the improvement in the sonographic variable of epidermis thickness was not significant [30]. In our study, the results in the group treated with SVF in combination with fractional CO2 laser confirmed a significant improvement in melanin Mexameter and Vancouver scar scale compared with fractional CO2 laser alone. There was no significant difference in the changes in skin thickness and total thickness of skin variables in the two groups. The existence of this difference could be due to the time interval between intervention and assessment. In the aforementioned study, the period between SVF injection and evaluation was three months, whereas in our study, this period was two months. On the other hand, part of this difference could be due to the different nature of the scars. The mentioned study was performed on acne scars, while in our study, burn scars were investigated.
Finally, it is important to mention that several studies have mentioned the efficacy of SVF in the treatment of various diseases as well as different skin lesions, including burn scars and acne scars [30, 32, 35]. The therapeutic effect of SVF is based on several mechanisms, including angiogenesis, inhibition of apoptosis, and anti-inflammatory effect [39]. And it seems that its efficacy in healing burn scars in our study is also consistent with the above effects. Based on the results of this study and other studies, the combined treatment method of CO2 laser and SVF seems to be more effective than other methods in treating scars caused by burns or other factors. The above method can be used as an alternative method in the treatment of these lesions. It should be mentioned that one of the limitations of the present study is the small sample size, which may affect the results. Therefore, conducting clinical trials with a larger sample may provide more reliable results.
Conclusion
The results of the present study show that the combined treatment of fractional CO2 laser and SVF as a new treatment has acceptable efficacy in the treatment of burn scars. Also, the patient and physician satisfaction with the treatment of this method was higher than that of the control group. Based on the above results, it can be concluded that the application of this method can be used as an effective method in the treatment of all types of skin scars, especially burn scars. It is worth mentioning that due to the small sample size in the current study, it is recommended to conduct a similar study with a larger sample to confirm the results.
Availability of data and materials
The data that support the findings of this study are available from the corresponding author, [M.A.N], upon reasonable request.
Abbreviations
- SVF:
-
Stromal vascular fraction
- VSS:
-
Vancouver scar scale
- ADSC:
-
Adipose tissue-derived stem cells
- PBS:
-
Phosphate-buffered saline
References:
Zhang C, Yin K, Shen Y-M. Efficacy of fractional carbon dioxide laser therapy for burn scars: a meta-analysis. J Dermatol Treat. 2021;32(7):845–50.
Behrangi E, Goodarzi A, Roohaninasab M, Sadeghzadeh-Bazargan A, Nobari NN, Ghassemi M. A review of scar treatment related to acne and burn. J Crit Rev. 2020;7(4):714–22.
Goodarzi A, Behrangi E, Ghassemi M, Nobari NN, Sadeghzadeh-Bazargan A, Roohaninasab M. Acne scar; a review of classification and treatment. J Crit Rev. 2020;7(5):815–23.
Seirafianpour F, Sodagar S, Mozafarpoor S, Baradaran HR, Panahi P, Hassanlouei B, et al. Systematic review of single and combined treatments for different types of striae: a comparison of striae treatments. J Eur Acad Dermatol Venereol. 2021;35(11):2185–98.
Douglas H, Lynch J, Harms K-A, Krop T, Kunath L, van Vreeswijk C, et al. Carbon dioxide laser treatment in burn-related scarring: a prospective randomised controlled trial. J Plast Reconstr Aesthet Surg. 2019;72(6):863–70.
Golnaz M, Mahrokh F, Azadeh G, Siamak Farokh F, Masoomeh R, Mohammadreza G, et al. Comparison of the therapeutic effect of microneedling with carbon dioxide laser in hypertrophic burn scars: a randomized clinical trial. Iran J Dermatol. 2019;22(2):53–7.
Seirafianpour F, Pour Mohammad A, Moradi Y, Dehghanbanadaki H, Panahi P, Goodarzi A, et al. Systematic review and meta-analysis of randomized clinical trials comparing efficacy, safety, and satisfaction between ablative and non-ablative lasers in facial and hand rejuvenation/resurfacing. Lasers Med Sci. 2022;37(4):2111–22.
Spiekman M, van Dongen JA, Willemsen JC, Hoppe DL, van der Lei B, Harmsen MC. The power of fat and its adipose-derived stromal cells: emerging concepts for fibrotic scar treatment. J Tissue Eng Regen Med. 2017;11(11):3220–35.
Gentile P, Scioli MG, Bielli A, Orlandi A, Cervelli V. Comparing different nanofat procedures on scars: role of the stromal vascular fraction and its clinical implications. Regen Med. 2017;12(8):939–52.
Franck CL, Senegaglia AC, Leite LMB, de Moura SAB, Francisco NF, Ribas Filho JM. Influence of adipose tissue-derived stem cells on the burn wound healing process. Stem Cells Int. 2019;2019:2340725.
Negenborn VL, Groen J-W, Smit JM, Niessen FB, Mullender MG. The use of autologous fat grafting for treatment of scar tissue and scar-related conditions: a systematic review. Plast Reconstr Surg. 2016;137(1):31e–43e.
Shin J, Cho JT, Park SI, Jung SN. Combination therapy using non-ablative fractional laser and intralesional triamcinolone injection for hypertrophic scars and keloids treatment. Int Wound J. 2019;16(6):1450–6.
Baryza MJ, Baryza GA. The Vancouver Scar Scale: an administration tool and its interrater reliability. J Burn Care Rehabil. 1995;16(5):535–8.
Rajashekhar G, Ramadan A, Abburi C, Callaghan B, Traktuev DO, Evans-Molina C, et al. Regenerative therapeutic potential of adipose stromal cells in early stage diabetic retinopathy. PLoS ONE. 2014;9(1):e84671.
Mohammadi R, Sanaei N, Ahsan S, Rostami H, Abbasipour-Dalivand S, Amini K. Repair of nerve defect with chitosan graft supplemented by uncultured characterized stromal vascular fraction in streptozotocin induced diabetic rats. Int J Surg. 2014;12(1):33–40.
Van Dijk A, Naaijkens B, Jurgens W, Nalliah K, Sairras S, Van der Pijl R, et al. Reduction of infarct size by intravenous injection of uncultured adipose derived stromal cells in a rat model is dependent on the time point of application. Stem Cell Res. 2011;7(3):219–29.
Jurgens WJ, Kroeze RJ, Zandieh-Doulabi B, van Dijk A, Renders GA, Smit TH, et al. One-step surgical procedure for the treatment of osteochondral defects with adipose-derived stem cells in a caprine knee defect: a pilot study. BioResearch Open Access. 2013;2(4):315–25.
Kim BJ, Lee DH, Kim MN, Song KY, Cho WI, Lee CK, et al. Fractional photothermolysis for the treatment of striae distensae in Asian skin. Am J Clin Dermatol. 2008;9(1):33–7.
Katz TM, Goldberg LH, Friedman PM. Nonablative fractional photothermolysis for the treatment of striae rubra. Dermatol Surg. 2009;35(9):1430–3.
Bak H, Kim BJ, Lee WJ, Bang JS, Lee SY, Choi JH, et al. Treatment of striae distensae with fractional photothermolysis. Dermatol Surg. 2009;35(8):1215–20.
Lee SE, Kim JH, Lee SJ, Lee JE, Kang JM, Kim YK, et al. Treatment of striae distensae using an ablative 10,600-nm carbon dioxide fractional laser: a retrospective review of 27 participants. Dermatol Surg. 2010;36(11):1683–90.
Manuskiatti W, Triwongwaranat D, Varothai S, Eimpunth S, Wanitphakdeedecha R. Efficacy and safety of a carbon-dioxide ablative fractional resurfacing device for treatment of atrophic acne scars in Asians. J Am Acad Dermatol. 2010;63(2):274–83.
Cho SB, Lee SJ, Kang JM, Kim YK, Chung WS, Oh SH. The efficacy and safety of 10,600-nm carbon dioxide fractional laser for acne scars in Asian patients. Dermatol Surg. 2009;35(12):1955–61.
Lee JW, Kim BJ, Kim MN, Mun SK. The efficacy of autologous platelet rich plasma combined with ablative carbon dioxide fractional resurfacing for acne scars: a simultaneous split-face trial. Dermatol Surg. 2011;37(7):931–8.
Ong M, Bashir S. Fractional laser resurfacing for acne scars: a review. Br J Dermatol. 2012;166(6):1160–9.
Qu L, Liu A, Zhou L, He C, Grossman PH, Moy RL, et al. Clinical and molecular effects on mature burn scars after treatment with a fractional CO2 laser. Lasers Surg Med. 2012;44(7):517–24.
Lee S-J, Suh D-H, Lee JM, Song K-Y, Ryu HJ. Dermal remodeling of burn scar by fractional CO2 laser. Aesthet Plast Surg. 2016;40(5):761–8.
Choi KJ, Williams EA, Pham CH, Collier ZJ, Dang J, Yenikomshian HA, et al. Fractional CO2 laser treatment for burn scar improvement: a systematic review and meta-analysis. Burns J Int Soc Burn Inj. 2021;47(2):259–69.
Peng W, Zhang X, Kong X, Shi K. The efficacy and safety of fractional CO2 laser therapy in the treatment of burn scars: a meta-analysis. Burns J Int Soc Burn Inj. 2021;47(7):1469–77.
Behrangi E, Moradi S, Ghassemi M, Goodarzi A, Hanifnia A, Zare S, et al. The investigation of the efficacy and safety of stromal vascular fraction in the treatment of nanofat-treated acne scar: a randomized blinded controlled clinical trial. Stem Cell Res Ther. 2022;13(1):1–11.
Roohaninasab M, Seifadini A, Atefi N, Sadeghzadeh-Bazargan A, Goodarzi A, Hanifnia AR, et al. Evaluating the effectiveness of stromal-vascular fraction (SVF) cells along with subcision method in the treatment of acne scars: a double-blind randomized controlled clinical trial study. J Cosmet Dermatol. 2022;21:6928–38.
Nilforoushzadeh MA, Heidari-Kharaji M, Alavi S, Nouri M, Nikkhah N, Jahangiri F, et al. Transplantation of autologous fat, stromal vascular fraction (SVF) cell, and platelet-rich plasma (PRP) for cell therapy of atrophic acne scars: clinical evaluation and biometric assessment. J Cosmet Dermatol. 2022;21(5):2089–98.
Gentile P, De Angelis B, Pasin M, Cervelli G, Curcio CB, Floris M, et al. Adipose-derived stromal vascular fraction cells and platelet-rich plasma: basic and clinical evaluation for cell-based therapies in patients with scars on the face. J Craniofac Surg. 2014;25(1):267–72.
Kim DG, Park ES, Kim SH. Combined treatment of stromal vascular fraction and ablative fractional CO2 laser for hypertrophic foot scar. Med Lasers Eng Basic Res Clin Appl. 2019;8(2):90–3.
Lee JW, Park SH, Lee SJ, Kim SH, Suh IS, Jeong HS. Clinical impact of highly condensed stromal vascular fraction injection in surgical management of depressed and contracted scars. Aesthet Plast Surg. 2018;42(6):1689–98.
Nilforoushzadeh MA, Faghihi G, Jafari F, Haftbaradaran E, Hoseini SM, Mazaheri N. Comparison of fractional carbon dioxide laser alone and in combination with subcision in improving atrophic acne scars. J Isfahan Med Sch. 2013;31(226):131–7.
Khanali S, Pedram A, Poorolajal J. Comparison of the efficacy of fractional CO2 laser with microneedling in management of patients with atrophic acne scars: a single-blind clinical trial. J Dermatol Cosmet. 2021;11(4):282–91.
Galal O, Tawfik AA, Abdalla N, Soliman M. Fractional CO2 laser versus combined platelet-rich plasma and fractional CO2 laser in treatment of acne scars: image analysis system evaluation. J Cosmet Dermatol. 2019;18(6):1665–71.
Andia I, Maffulli N, Burgos-Alonso N. Stromal vascular fraction technologies and clinical applications. Expert Opin Biol Ther. 2019;19(12):1289–305.
Acknowledgements
The authors would like to express their gratitude to the staff of the Rasool Akram Medical Complex Clinical Research Development Center (RCRDC) specially Mrs. Farahnaz Nikkhah, Iran University of Medical Sciences and the Skin and Stem Cell Research Center at Tehran University of Medical Sciences for their technical and editorial assistance.
Funding
This research was supported by the Skin and Stem Cell Research Center, Tehran University of Medical Sciences. The funding body played no role in the design of the study and collection, analysis, and interpretation of data and in writing the manuscript.
Author information
Authors and Affiliations
Contributions
Contributions to the current study includes FKH and MR and MG and AS in study idea and design and in the literature review, and drafting and revising the manuscript critically for importance intellectual content. NA and SZ involved in conducting the trial, data gathering, drafting the proposal, following up with ethical committee for approval, and revising the manuscript critically for importance intellectual content. AJ, ST, and MN involved in drafting the revised manuscript and literature review, and analysis and interpretation of revised version and drafting the manuscript. EB involced in the proposal preparation and statistics and analysis and drafting the revised manuscript. MAN and MR involved in the study supervision, data gathering and literature review, and drafting the manuscript, and both are corresponding authors. All authors have read and approved the final version to be published and agreed to be accountable for all aspects of the work. All authors agreed on the order in which their names are listed in the revised manuscript.
Corresponding authors
Ethics declarations
Ethical principles and consent to participate
All information obtained from patients was kept confidential and evaluated anonymously. All patients studied adhered to the Helsinki ethical principles, and the study protocol was registered at Iranian Registry of Clinical Trials with code: IRCT20210515051307N1, Registration date: 2021-11-14, URL: https://www.irct.ir/trial/56337. This project was approved by the Ethics Committee of Iran University of Medical Sciences with the title: Evaluation of the effectiveness and satisfaction of fractional CO2 laser and stromal vascular fraction in comparison with fractional CO2 laser alone in the treatment of burn scars,” with the ethical code IR.IUMS.FMD.REC.1400.099, date of approval: 2021-05-03. The patients were signed informed consent for participating in the study.
Consent for publication
Written informed consent was obtained from the patients for their anonymized information to be published in this article.
Competing interests
All the authors declare that there is no conflict of interest for this project.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Roohaninasab, M., Khodadad, F., Sadeghzadeh-Bazargan, A. et al. Efficacy of fractional CO2 laser in combination with stromal vascular fraction (SVF) compared with fractional CO2 laser alone in the treatment of burn scars: a randomized controlled clinical trial. Stem Cell Res Ther 14, 269 (2023). https://doi.org/10.1186/s13287-023-03480-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13287-023-03480-8