Abstract
Background
Tongue necrosis is a rare and relatively uncommon condition, usually caused by vasculitis, thrombosis, severe hypotension due to septic or cardiogenic shock, vasopressor use, or intubation. Following damage such as necrosis, dystrophic calcification, a type of soft tissue calcification, can occur.
Case presentation: Herein, we present a unique case of bilateral tongue necrosis in a patient with nonintubated septic shock. A 70-year-old East Asian man with no significant medical history presented to the emergency department with postprandial epigastric pain. The patient was admitted to the intensive care unit with hypotension due to septic shock and disseminated intravascular coagulation. After a short course of vasopressors, the patient developed tongue discoloration and swelling without limb ischemia. Computed tomography was performed to observe the tongue necrosis, and calcification of the tongue was found. The patient was successfully treated by wiping the area with a hexamidine-soaked gauze.
Conclusion
Tongue necrosis remains a rare finding, and its occurrence as a complication of vasopressor use is even rarer. Therefore, even with relatively short courses of vasopressors in the intensive care unit, daily visualization of the tongue to check for discoloration, along with daily inspection and pulse checks of the limbs, can help identify vasospasms. These measures allow for prompt intervention, minimizing permanent damage and shortening the recovery time.
Similar content being viewed by others
Introduction
The tongue is a well-vascularized organ that rarely undergoes ischemic necrosis. It is supplied primarily by the lingual artery [1]. The lingual artery originates from the external carotid artery and branches into the dorsal lingual, sublingual, and deep lingual branches, forming a rich anastomosis that provides an arterial supply to the tongue and floor of the mouth. Venous drainage of the tongue was performed through the lingual vein, which subsequently drains into the internal jugular vein.
The most common etiology of tongue necrosis is vasculitis, such as giant cell arteritis (GCA) [2,3,4], with a few reports linked to severe hypotension, vasopressor use, and thrombosis. Vasopressors are commonly used in patients with septic/cardiogenic shock and may lead to peripheral ischemia. However, ischemic necrosis of a well-vascularized tongue is extremely rare. Therefore, we present a rare case of a patient who developed ischemic tongue necrosis without intubation. We present this article in accordance with the case report guidelines (CARE) reporting checklist.
Case report
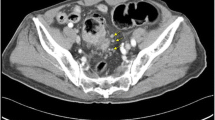
A 70-year-old East Asian male with no significant underlying medical history except for benign prostatic hyperplasia presented to the emergency department with postprandial epigastric pain. Abdomen–pelvis computed tomography (CT) revealed an enlarged mass in the liver, along with dilatation of the intrahepatic bile ducts, suggesting cholangiocarcinoma or cholangitis (Fig. 1). The patient was admitted to the general ward. Initially, the patient’s vital signs were relatively stable (blood pressure of 167/99 mmHg, heart rate of 95 beats per minute, respiratory rate of 20 per minute, body temperature of 36.4 ℃, saturation of 97% in room air); however, after 24 hours, the patient suddenly exhibited hypotension (80/55 mmHg) and an increased oxygen requirement (5 L/minute). Blood tests showed decreased platelet count (45,000/µL), elevated fibrin degradation products (99.39 µg/mL), significantly elevated d-dimer (> 3,200 ng/mL), and prolonged activated partial thromboplastin time (44.7 seconds) and prothrombin time (24.0 seconds). After percutaneous transhepatic biliary drainage insertion, Candida grew in the drainage fluid. The patient was suspected of having septic shock and disseminated intravascular coagulation (DIC). He was transferred to the intensive care unit (ICU) and was started on norepinephrine, reaching a maximum dose of 0.15 mcg/kg/min, used over a relatively short duration of 34 hours (1.5 days). The patient was treated with a high-flow nasal cannula (flow rate of 40 L/minute and fraction of inspired oxygen of 0.6) and continuous renal replacement therapy (CRRT) for approximately 2 weeks without intubation and showed gradual improvement of the septic condition.
About 10 days after admission, 7 days following 1.5 days of norepinephrine use, we observed a dark discoloration with significant swelling predominantly affecting the central and posterior regions of the tongue. This condition, which covered approximately thirty percent of its area, was not apparent upon admission (Fig. 2 A, B). The patient complained of pain and discomfort in the tongue. After consulting an oral and maxillofacial surgeon, the patient’s tongue was diagnosed with multiple ulcers and a necrotic surface. The treatment consisted of swabbing the area with a 0.12% chlorhexidine gluconate solution (hexamedine, Buk-wang Pharmaceutical, Seoul, South Korea)-soaked gauze twice a day and monitoring the progress. However, 1 week later, the nearly entire surface of the tongue had worsened, and the swelling had increased bilaterally (Fig. 2C, D). To investigate the potential primary causes of tongue necrosis, such as vasculitis and carotid artery stenosis, various diagnostic tests were performed, including autoimmune and lipid laboratory tests and brain computing tomography (CT) angiography. Laboratory tests showed weakly positive anticardiolipin antibody immunoglobulin M, but other tests, including antinuclear antibodies, antineutrophil cytoplasmic antibodies, and lupus anticoagulant, were all negative. A rheumatologist concluded that these findings are not indicative of rheumatoid diseases and suggested a low likelihood based on clinical symptoms, as the patient did not exhibit other vasculitis symptoms such as skin lesions, arthritis, or pain, aside from the condition of the tongue. Lipid laboratory results were unremarkable, and brain CT angiography revealed no severe atherosclerosis with well-detected lingual arteries. However, precontrast CT showed signs of tongue calcification due to ischemic changes (Fig. 3). After exclusively using 0.12% chlorhexidine gluconate solution-soaked gauze continuously, the patient’s tongue began to show gradual improvement 2 weeks later. Approximately 1.5 months after ICU admission, the tongue had almost returned to its normal state (Fig. 2E, F). The patient no longer reported tongue pain or discomfort while eating.
Serial images of tongue necrosis. A, B Necrotic change on tongue 10 days after admission. A darkish discoloration was observed in the center and back of the tongue, with significant swelling. C, D More severe necrotic change at 17 days. The surface of the tongue worsened, and the swelling intensified bilaterally. E, F Improvement of necrotic change of tongue at 50 days. Discoloration and swelling improved, and the patient reported no pain or discomfort
Discussion
Tongue necrosis is a rare occurrence. The tongue is a highly vascular organ that is generally tolerant of injury [5]. Few cases have been documented in literature, and most are typically caused by vasculitis such as GCA or polyarteritis nodosa [2,3,4, 6]. Some studies have described tongue necrosis caused by septic or cardiogenic shock. To date, only about ten cases of tongue necrosis due to septic shock and cardiogenic shock have been reported [7,8,9,10,11,12]. Other studies have reported other causes of tongue necrosis, such as prolonged oral intubation [13,14,15,16] and carotid artery stenosis [1, 17].
In patients with vasculitis, tongue necrosis is often unilateral and limited to the anterior half or tip of the tongue [1]. Involvement of the base or both sides of the tongue is rare. In this case, necrosis occurred in both the bilateral and posterior aspects of the tongue. Vasculitis and other rheumatic diseases were excluded based on autoimmune laboratory tests and expert assessments of clinical manifestations. Moreover, arterial stenosis or infarctions were excluded based on normal lipid laboratory test results and angiographic CT scans.
At the time of admission to the ICU, the blood pressure of the patient was low, and laboratory results indicated DIC. We initiated CRRT due to metabolic acidosis. To maintain the blood pressure, norepinephrine, a vasopressor, was administered for 1.5 days. After being transferred to the general ward, the patient continued dialysis because of kidney damage resulting from previous septic shock. Due to cancer progression, the lab data of the patient were similar to DIC condition, with low platelet counts and elevated prothrombin time and d-dimer levels. Additionally, while in the general ward, the patient experienced another infection, resulting in septic shock with low blood pressure. However, the family did not want to life-sustaining treatments anymore, and thus, vasopressors were not administered. Despite these conditions, the patient’s tongue remained in an improved state, clearly indicating that the changes in his tongue were caused by the short-term use of vasopressors, rather than by DIC or septic shock. Norepinephrine is structurally classified as a catecholamine, and the addition of a methyl group to amine group results in the formation of epinephrine. Norepinephrine binds to α- and β-adrenergic receptors in different tissues. In the blood vessels, it triggers vasoconstriction, which increases blood pressure [18]. This also results in decreased blood volume in dialysis patients, potentially causing poor perfusion or ischemia [19, 20].
To our knowledge, this is one of the rare reported cases of bilateral tongue necrosis in a patient with nonintubated septic shock without a significant surgical history. All previously reported cases of tongue necrosis due to cardiogenic or septic causes involved patients who underwent surgical procedures, such as coronary artery bypass or intra-aortic balloon pumps. And they were all intubated [8, 10]. In contrast, in this study, the patient had septic shock but did not undergo any surgical or medical procedures. Moreover, intubation, a possible cause of tongue necrosis, was not performed. Endotracheal intubation is associated with many oral complications, such as damage to the lips, teeth, gums, and tongue [13]. Instead, the patient used a high-flow nasal cannula. This could avoid potential damage or pressure effects associated with the endotracheal tube. In other studies, patients with septic shock who were treated with vasopressors developed not only tongue necrosis but also peripheral limb ischemia [7, 10, 12]. However, in the present case, no signs of peripheral limb ischemia or tongue necrosis were observed.
In addition, this study reported the use of CT to observe tongue necrosis and complete healing in patients with sepsis. In previous studies, CT was not used to evaluate tongue necrosis in patients with cardiogenic or septic shock. In our case, CT imaging was used to evaluate the condition of the tongue, which showed intact vessels and calcified tongues despite normal calcium and phosphorus levels.
Oral ulcers are common lesions of the oral mucosa resulting from various mechanical or chemical injuries. Bacterial contamination of these lesions can adversely affect the healing process, leading to prolonged healing times and the formation of exuberant granulation tissue [21, 22]. Chlorhexidine gluconate solution has been found to reduce the incidence, duration, and severity of many types of oral ulcers [23]. In this case, we propose that the use of chlorhexidine gluconate solution reduced bacterial contamination of the tongue ulcer and accelerated the healing process.
Dystrophic calcification is a type of soft tissue calcification that occurs in damaged or necrotic tissue when serum levels of calcium and phosphorus are normal [24, 25]. There are some reports of patients who were diagnosed with ischemic stroke and developed calcification in the brain tissue [26,27,28,29]. Moreover, calcification can be observed in the oral cavity [30], muscles [31], and subcutaneous tissues [32] after damage. Common sites of soft-tissue calcification in the intraoral area include the gingiva, tongue, lymph nodes, and cheeks. To our knowledge, this is the first study of calcified tongues after tongue necrosis. Similar to heterotopic ossification, which is the presence of bone in soft tissues where bone is not normally found, these calcifications can range from small, clinically insignificant foci to large deposits that cause pain and limit function [33, 34]. In our patient, the ischemic damage to the tongue likely led to calcification, potentially causing pain and dysfunction.
The prognosis for the tongue in previously known cases of tongue necrosis caused by septic or cardiogenic shock has generally been poor. This case is exceptionally rare because the tongue had almost completely returned to normal. Owing to the rich blood supply to the tongue, it has been suggested that the tongue gradually recovers over time following transient ischemic damage. Despite the patient’s tongue returning to normal, he was eventually diagnosed with cholangiocarcinoma and passed away due to cancer progression 3 months after admission. Consequently, a follow-up CT for tongue calcification could not be performed. However, considering the apparent normalization of tongue appearance, it is likely that CT imaging would have shown an improvement in calcification.
Conclusion
Tongue necrosis is mainly associated with vasculitis, but it remains a rare finding, and its occurrence as a complication of vasopressor use is even rarer. However, clinicians should be aware that even with relatively short courses of vasopressors in the ICU, daily visualization of the tongue during physical examinations to check for discoloration, along with daily inspection and pulse checks of the limbs, can help identify vasospasms. These measures allow for prompt intervention, minimizing permanent damage and shortening recovery time.
Availability of data and materials
Not applicable.
Abbreviations
- CT:
-
Computed tomography
- DIC:
-
Disseminated intravascular coagulation
- GCA:
-
Giant cell arteritis
- ICU:
-
Intensive care unit
- CRRT:
-
Continuous renal replacement therapy
References
Amen F, Amen AA. Tongue ischaemia in a patient with external carotid artery stenosis. J Laryngol Otol. 2002;116:1053–4.
Cho YM, El Khoury L, Paramo J, Horowitz DM, Li JY, Kello N. Tongue necrosis secondary to giant cell arteritis, successfully treated with tocilizumab: a case report. BMC Musculoskelet Disord. 2023;24(1):382.
Zadik Y, Findler M, Maly A, Rushinek H, Czerninski R. A 78-year-old woman with bilateral tongue necrosis. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2011;111(1):15–9.
Kitamura N, Sento S, Yoshizawa Y, Sasabe E, Yamamoto T. Tongue necrosis caused by systemic vascular diseases: a systematic review of the literature. Oral Sci Int. 2020;17(2):51–8.
Dolina M, Foster JD, Isaacson J, Ruggiero F, Wojnar M. Sepsis from necrotic tongue as an unusual complication of Seisure disorder. Chest. 2005. https://doi.org/10.1378/chest.128.4_MeetingAbstracts.479S-a.
Raveendran R. On the tip of the tongue: Tongue necrosis as the initial presentation of systemic vasculitis in adult and pediatric patients - case reports and literature review. J Family Med Dis Prev. 2016. https://doi.org/10.23937/2469-5793/1510047.
Cho J, Sung K, Lee D. Ischemic necrosis of the tongue in surgical patients with septic shock: a case report. BMC Surg. 2016;16(1):48.
Hulstaert E, Roggeman E, Beeckman AS, Moerman M, Vanderstraeten E, Rasquin K, et al. Ischaemic necrosis of the tongue as a rare complication of cardiogenic shock. Acta Clin Belg. 2016;70(6):436–9.
McGoldrick DM, Khan I, Cotter CJ. Ischaemic necrosis of the tongue. BMJ Case Rep. 2015. https://doi.org/10.1136/bcr-2014-208330.
Roman BR, Immerman SB, Morris LG. Ischemic necrosis of the tongue in patients with cardiogenic shock. Laryngoscope. 2010;120(7):1345–9.
Noordally SO, Sohawon S, Duttmann R, Gottignies P, Devriendt J. Tongue necrosis as a complication of vasoconstrictor agents in the intensive care setting. Intern Emerg Med. 2011;6(2):183–5.
Arian MU, Medina CS, Matus G, Hazari AD, Chozet L, Omar F. Systemic vasospasms induced by vasopressor therapy resulting in diffuse tissue necrosis and death: a case report and review of the literature. J Emerg Criti Care Med. 2022. https://doi.org/10.21037/jeccm-20-161.
Al Y, Hamdi M, Kammasha A, Nashawi FE, Ashreefa R, Yousfan A. Bilateral tongue necrosis in a young patient as a complication of prolonged oral endotracheal intubation: a case report. Ear Nose Throat J. 2023. https://doi.org/10.1177/1742271X19840271.
Adegbite NA, Avery C, Rajaram K, Mohamed AM. Tongue necrosis: a rare complication of prolonged oral intubation. J Surg Case Rep. 2019. https://doi.org/10.1177/1742271X19840271.
Haider S, Kumar K, Cramer C, Garcia C, El-Hosni M, Levine D. A rare case of lingual necrosis secondary to prolonged endotracheal intubation. J Med Cases. 2016;7(10):429–31.
Kamatani T, Yamashita K, Okabayashi T, Maeda H, Toi M, Yamamoto T. Bilateral ischemic necrosis of the tongue due to disseminated intravascular coagulation. Int J Oral Maxillofac Surg. 2008;37(8):777–9.
Bjordahl PM, Ammar AD. Tongue necrosis as an unusual presentation of carotid artery stenosis. J Vasc Surg. 2011;54(3):837–9.
Bylund DB. Norepinephrine. In: Enna SJ, Bylund DB, editors. xPharm: The Comprehensive Pharmacology Reference. New York: Elsevier; 2007. p. 1–5.
Nette RW, Ie EH, Vletter WB, Krams R, Weimar W, Zietse R. Norepinephrine-induced vasoconstriction results in decreased blood volume in dialysis patients. Nephrol Dial Transplant. 2006;21(5):1305–11.
Persichini R, Silva S, Teboul JL, Jozwiak M, Chemla D, Richard C, et al. Effects of norepinephrine on mean systemic pressure and venous return in human septic shock. Crit Care Med. 2012;40(12):3146–53.
Addy M, Hunter L. The effects of a chlorhexidine gluconate mouthrinse on plaque toothstaining and candida in aphthous ulcer patients. J Clin Periodontol. 1987;14(5):267–73.
Shaw WC, Addy M, Griffiths S, Price C. Chlorhexidine and traumatic ulcers in orthodontic patients. Euro J Orthodontic. 1984;6(2):137–40.
Porter SR, Leao JC. Review article: oral ulcers and its relevance to systemic disorders. Aliment Pharmacol Ther. 2005;21(4):295–306.
Hwang ZA, Suh KJ, Chen D, Chan WP, Wu JS. Imaging features of soft-tissue calcifications and related diseases: a systematic approach. Korean J Radiol. 2018;19(6):1147–60.
Jones JRP, Bell D, et al. Dystrophic soft tissue calcification. Radiopaediaorg. 2024. https://doi.org/10.1177/1742271X19840271.
Mohammed Q, Ansari M, Chincanchan CA, Armstrong DL. Brain calcification in hypoxic-ischemic lesion: an autopsy review. Pediat Neurol. 1990;6:94–101.
Wityk RJ, Barry D, Stein M. Rapid brain calcification after ischemic stroke. Ann Intern Med. 1993;119:490–1.
Parralo-Lopez A, Hernandez-Gonzalez A, Bravo-Gomez JJ, de Leon SC, Nieto AC. Early extensive gyral calcification in ischemic stroke. Acta Neurol Belg. 2020;120(2):499–501.
Dorfman K. Cortical calcifications in ischemic stroke. Case study. Radiopaediaorg. 2024.
Kumar GA, Deora SS. Dystrophic calcification in the oral cavity resulting in mechanical dysphagia: a case report and review of calcification in the head and neck region. Cureus. 2020;12(3): e7469.
Kim HY, Park JH, Lee JB, Kim SJ. A case of dystrophic calcification in the masseter muscle. Maxillofac Plast Reconstr Surg. 2017;39(1):31.
Guo J, Shi W, Zhang G, Zhu C. Dystrophic calcification of the lower leg in a patient with chronic lower extremity venous insufficiency and diabetes mellitus: a case report and literature review. Adv Skin Wound Care. 2023;36(1):1–7.
Mori M, Kasai T, Shrestha P, Upadhyaya C, Ohta T, Amano O, et al. Heterotopic ossifying tumors in head and neck and heterotopic ossification and calcification. J Oral Maxillof Surg Med Pathol. 2012;24(4):222–36.
Zychowicz ME. Pathophysiology of heterotopic ossification. Orthop Nurs. 2013;32(3):173–7.
Acknowledgements
We thank the patients who participated in this study.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
Conception and design: SYK, SHK, and SIL. Administrative support: SHK, HL, and SIL. Provision of study materials or patients: HL. Collection and assembly of data: SYK and SIL. Data analysis and interpretation: SYK and SHK. Manuscript writing: all authors. Final approval of manuscript: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the local ethics review board in accordance with the Declaration of Helsinki.
Consent for publication
Written informed consent was obtained from the patient's next-of-kin for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Kim, Sy., Kim, SH., Lee, H.S. et al. Calcification following tongue necrosis induced by vasopressor use in a nonintubated patient with septic shock: a case report. J Med Case Reports 18, 458 (2024). https://doi.org/10.1186/s13256-024-04796-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-024-04796-6