Abstract
Background
Osteopoikilosis, also referred to as disseminated condensing osteopathy, spotted bone disease, or osteopecilia, is a rare bone disorder. The case presented here showcases multiple disc lesions in the spine, extensive multifocal skin lesions, and positive test results for dermatomyositis and multifocal enthesopathy, accompanied by neurological symptoms. This manifestation represents a novel variant of the disease.
Case presentation
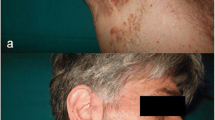
Our patient is a 46-year-old mosque Kurdish servant presenting with complaints of pain in the right leg, lower back, right hand, and neck. Additionally, the patient has been experiencing redness in the right buttock and ipsilateral thigh, as well as gradually expanding and stiffening skin lesions on the left shin for the past 3 weeks. Painful neck movements and a positive Lasegue test were also observed in the right leg. The patient reports pain in the right buttock accompanied by a substantial erythematous area with induration measuring 8 × 15 cm, as well as an erythematous and maculopapular lesion measuring 6 × 18 cm on the left shin.
Conclusions
Our patient is a 46-year-old man presenting with complaints of skin lesions and pain in the lower back, pelvis, neck, and limbs. The X-ray reveals shoulder, pelvis, knee, and ankle involvement, while spinal involvement is observed in the neck and lumbar region. Furthermore, the bone scan indicates extensive enthesopathy in various regions, a unique manifestation not previously reported in similar cases.
Similar content being viewed by others
Introduction
Osteopoikilosis is a rare bone disease initially described by Albers-Schonberg in 1915 [1]. It has an estimated prevalence of 1 per 50,000 individuals and is classified as an autosomal dominant osteosclerotic (ADO) dysplasia characterized by a distinct radiological appearance [2]. This condition is also called disseminated condensing osteopathy, spotted bone disease, and osteopecilia [3]. There are three forms of the disease: speckled type, striated type, and mixed type [3]. Autosomal dominant osteopoikilosis is associated with heterogeneous mutations in the LEMD3 gene [4]. The primary pathology of this condition involves disruptions in the bone maturation process, classifying it as a form of bone dysplasia [5]. The Buschke–Ollendorff syndrome is characterized by concurrent skin involvement, with skin biopsies and pathological examinations revealing an abundance of fibroelastins in the middle and deep dermis [6]. Rare complications associated with this syndrome include spinal canal stenosis, dacryocystitis, and malignant transformation [7]. Approximately 25% of Buschke–Ollendorff syndrome cases exhibit dermatofibrosis lenticularis disseminata, which exhibits colloid formation and resembles scleroderma. This manifestation is attributed to the proliferation of activated fibroblasts and may occasionally result in palmar-plantar keratoderma [2, 3, 8]. Bone densitometry typically shows normal results [9]. The condition is characterized by the presence of elastic connective tissue in this diffuse syndrome [10]. The current case involves multiple disc lesions in the spine, extensive multifocal skin lesions, positive findings for dermatomyositis and multifocal enthesopathy, and accompanying neurological symptoms. This presentation represents a novel variant of the disease.
Case report
The patient is a 46-year-old Kurdish male mosque servant presenting with pain in the right leg, lower back, right hand, and neck. The patient reported experiencing symptoms of redness in the right buttock and ipsilateral thigh, as well as skin lesions in the left shin, which started gradually, expanded, and became stiff over the course of 3 weeks. Additionally, the patient complained of pain in the lower back and pelvis that worsened with walking, significantly affecting his ability to walk normally. Two years prior, the patient underwent surgery for cervical disc herniation and was subsequently treated with acetaminophen and chlordiazepoxide but experienced no improvement in symptoms. The patient had a history of smoking 20 packs of cigarettes per year but quit smoking 8 years ago. At the time of the study, the patient admitted to using a small amount of opium. During the examination, the patient’s vital signs were stable, and a surgical scar from the disc surgery was noted on his neck. The patient reported painful neck movements, and the Lasegue test of the right leg yielded a positive result. He also experienced pain in the right buttock, and an area of erythema with firm induration measuring 8 × 15 cm was observed. Furthermore, an erythematous and maculopapular lesion measuring 6 × 18 cm was present on the left shin. The right proximal muscle strength was assessed as 4.5, as was the strength of the right lower limb. Deep tendon reflexes (DTR) in the right upper limb were + 3, while in the Achilles lower limb, they were + 4 with clonus.
Preoperative Magnetic resonance imaging (MRI) of the neck revealed the following findings: Cervical lordosis with spondylolysis changes, posterior bulging disk in C3–C4, C4–C5, and C5–C6, resulting in compression of the thecal sac at the affected levels. Additionally, there was evidence of myelomalacia in the cervical cord at the C4 level. Furthermore, a hemangioma was observed in the T1 vertebral body.
Pelvic MRI: Multiple enumerable low signal foci in bilateral femoral head compatible with benign sclerotic lesions such as osteopoikilosis.
Brain MRI: Normal.
Back MRI: Decreased lordosis and dehydration, bulging in L4–L5 level, and bared base seen in L4–L5 and central L5–S1.
Triphsic whole body scan: Enteropathy involving the upper portion of right SI joint, left anterior superior iliac spine, right pelvic brim, bilateral patella, right tibia tuberosity, and bilateral medial malleoli.
Main symptom: Pain in limbs, neck, and lumbar spine, and skin lesion as erythema and warmness in the upper tie, buttock, and leg.
Medical, family, and psychological history: Surgery for disk herniation in the neck spine, diabetes mellitus in his mother and mild hypertension in his father, a history of cigarette smoking (18 packs per year), a history of inhalational opioid use, and no history of psychological disorders.








Discussion
Some studies have reported a similar prevalence of the disease in men and women, while others have indicated a higher prevalence in men. This difference may be attributed to referral bias, as more men tend to visit the emergency department for traumatic accidents and injuries requiring X-rays. In reality, the incidence of the disease is similar in both genders [11]. There are reports of this syndrome coexisting with other conditions such as dwarfism, dystocia, coarctation of the aorta, double urethra, spinal canal stenosis, tuberous sclerosis, scleroderma, dystocia, precocious puberty, endocrine disorders (e.g., diabetes mellitus), fibromyalgia, facial anomalies, reactive arthritis, discoid lupus erythematosus (DLE), familial Mediterranean fever (FMF), and psoriatic arthritis [2, 3, 7, 8]. In bone histopathology, visible are lesions related to the lamellar osseous tissue containing the Haversian system and focal condensation of compact lamellar bone in the spongiest [3, 8]. The prevalence of bone involvement is as follows: phalanx (100%), carpal bone (97.4%), metacarpal (92.5%), toes (87.2%), metatarsus (84.4%), tarsus (84.6%), pelvis (74.4%), femur (74.4%), radius (66.7%), ulna (66.7%), sacrum (58.9%), humerus (28.2%), tibia (20.5%), and fibula (2.8%) [5, 8]. The most common anatomical locations of bone involvement are the epiphysis or metaphysis regions of the long bones [3]. Differential diagnoses of the disease include osteoblastic metastasis, primary bone tumor, mastocytosis, tuberous sclerosis, synovial chondromatosis, osteopathia striata, and melorheostosis [2, 3]. No specific point is observed in the bone scan with Technetium-99m, and the scans are often normal. However, the abnormality in the scan does not definitively rule out the diagnosis of osteopoikilosis [1, 2, 5, 7]. To date, four cases of osteopoikilosis with abnormal bone scans have been reported (2).
Conclusions:
The patient is a 46-year-old man presenting with skin lesions and pain in the lower back, pelvis, neck, and limbs. The X-ray reveals shoulder, pelvis, knee, and ankle involvement. Spinal involvement is observed in the neck and lumbar region. The bone scan shows extensive enthesopathy in various regions, which is unique compared to previous cases and has not been reported thus far.
Availability of data and materials
All data generated or analyzed during this study were included in this article but the raw data are available from the corresponding author on reasonable request.
References
Ruci V, Serani D. Osteopoikilosis—case report. Open Access Maced J Med Sci. 2014;2(1):132–4.
Kucukcakir N, Inceoglu LA, Raif SL. Osteopoikilosis—a case report. Turk J Phys Med Rahab. 2015;61:376–9.
Ruaro B, Sulli A, Alessandria E, Ravera F, Culolo M. Coexistence of osteopoikilosis with seronegative and Reynoud’s phenomenon. First case report with evaluation of the nailfold capillary bed and literature review. Reumatismo. 2012;64(5):335–9.
Baasanjav S, Jamsheer A, Kolanczyk M, Horn D, Latos T, Hoffmann K, Latos-Bielenska A, Mundlos S. Osteopoikilosis and multiple exostoses caused by novel mutations in LEMD3 and EXT1 genes respectively—coincidence within one family. BMC Med Genet. 2010;11(110):1–8.
Ahgdashi MA, Aghdashi MM, Rabiepour M. Osteopoikilosis: pain as presenting symptom in three family members. Clin Med Insight Arthritis Musculoskel Disord. 2012;4:29–32.
Hellemans J, Preobrazhenska O, Willaert A, Debeer P, Verdonk PCM, Costa T, Janssens K, Menten B, Van Roy N, Vermeulen SJT, Savarirayan R, Van Hul W, Vanhoenacker F, Huylebroeck D, De Paepe A, Naeyaert J-M, Vandesompele J, Speleman F, Verschueren K, Coucke PJ, Mortier GR. Loss of function mutation in LEMD3 result in osteopoikilosis, Buschke–Ollendroff syndrome and melorheostosis. Nat Genet. 2004;36(11):1213–8.
Krishna D. Osteopoikilosia: a case report with review of literature. J Orthop Traumatol Rehabil. 2013;6(1):84–6.
Negi RS, Manchanda KL, Sanga S, Chand S, Goswami G. Osteopoikilosis-spotted bone disease. Med J Armed Forces India. 2013;69:196–8.
Tolunay T, Arslan AK, Bingol I, Bicici V, Eren M, Lemine CMM, Kilicarslan K. Bone pathology: osteopoikilosis. Open J Orthop. 2013;3:217–9.
Ellanti P, Clarke B, Gray J. Osteopoikilosis. Ir J Med Sci. 2010;179:615–6.
Rajkumar Jangir R, Laxmikant Mishra D, Kumar M, Mathur AK. Osteopoikilosis and its clinical significance: a review literature. PRJMHS. 2014;3(4):11–20.
Acknowledgements
We would like to thank Kurdistan University of Medical Sciences and Research Deputy of Kurdistan University of Medical Sciences.
Funding
No funding.
Author information
Authors and Affiliations
Contributions
AA, BM: writing—original draft. Both the authors studied and approved the content of the present manuscript and participated in revising the paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mohsenpour, B., Ahmadi, A. Osteopoikilosis: a case report. J Med Case Reports 17, 292 (2023). https://doi.org/10.1186/s13256-023-04025-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-023-04025-6