Abstract
Background
Patients with underlying cardiovascular risk factors have worse clinical outcomes when they have coronavirus disease. In addition, a reduced workload of cardiovascular emergencies has been reported during the coronavirus pandemic due to patients’ reluctance to attend hospitals for fear of contracting the disease. Regional health service reorganization, separating hospitals into coronavirus and non-coronavirus can mitigate this effect. However, the effectiveness of this approach on outcomes and patient satisfaction is unknown.
Case presentation
A 35-year-old Pakistani man with acute ST myocardial infarction was found to have thrombosis of the right coronary artery aneurysm and concomitant coronavirus disease. He had percutaneous coronary angiography and thrombus removal, and was transferred to a coronavirus hospital for the management of the infection. Due to the large size of the aneurysm, he was considered for surgical intervention. Following discharge from the coronavirus hospital and a period of stay at the isolation center, he failed to keep his cardiology follow-up appointment.
Conclusion
This case illustrates an unusual cause of myocardial infarction in a patient with coronavirus infection whose care may have been adversely affected by the healthcare system restructuring.
Similar content being viewed by others
Background
The recent coronavirus disease 2019 (COVID-19) pandemic has had a major impact on healthcare provision and resource utilization. COVID-19 patients with underlying cardiovascular risk factors have worse clinical outcomes [1]. In addition, reduced cardiovascular emergency workload due to patients’ reluctance to attend hospitals for fear of contracting COVID-19 has been reported [2]. One way to mitigate this is regional health service reorganization, separating hospitals into COVID-19 and non-COVID-19. The effectiveness of this approach on clinical outcomes and patient satisfaction is unknown.
Our city has two major hospitals, and both receive acute cardiovascular emergencies. Following the outbreak of the COVID-19 pandemic, the hospitals were redesignated as COVID and non-COVID. All patients with COVID-19 disease are managed at the COVID hospital. Patients who present at the non-COVID hospital with a cardiovascular emergency such as ST myocardial infarction underwent percutaneous coronary intervention before transfer to the COVID hospital if they had a positive polymerase chain reaction (PCR) test.
We present a case report of a man with acute ST-elevation myocardial infarction resulting from coronary artery aneurysms and concomitant COVID-19, whose care may have been compromised by the regional healthcare reorganization as a result of the COVID-19 pandemic.
Case presentation
A 35-year-old Pakistani man presented to our emergency department with a 1 h history of central chest pain radiating to the left arm with associated nausea and diaphoresis.
He was an ex-smoker of 10 pack/years, and he suffered from hyperlipidemia, for which he had been on lifestyle modifications and statin for the last 2 years. He had a positive family history of coronary artery disease. He denied any history of acute illness or hospital admission in his childhood.
On examination, the patient was sweating and in pain, with a pain score of 8/10. He was conscious and alert with no neurological deficit. His initial vital signs were as follows: heart 63 beats per minute, regular; blood pressure, 126/81 mmHg, and respiratory rate of 20 per minute. He was afebrile, and had normal breath sounds and normal heart sounds with no murmur. His abdominal examination was normal. His 12-lead electrocardiogram showed ST-segment elevation in the inferior leads, with reciprocal changes in the anterior charges (Fig. 1). A diagnosis of an acute ST-elevation myocardial infarction was made, and he was transferred for percutaneous coronary intervention. He received 5000 units of unfractionated heparin, 300 mg of aspirin, 80 mg of atorvastatin, 180 mg of ticagrelor, and 5 mg of intravenous morphine.
Laboratory findings were remarkable for initial troponin T 9.6 ng/L (< 14 ng/L), low-density lipoprotein 6.56 mmol/L (< 3.36 mmol/L), triglyceride 1.73 mmol/L (0.45–1.69 mmol/L), cholesterol/high-density lipoprotein 9.96 (3.35).
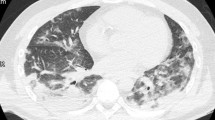
A portable chest radiograph was normal.
His angiogram showed a medium-size aneurysm in the circumflex artery, and a large aneurysm (14.46 mm) in the proximal right coronary, followed by multiple sequential aneurysms and 100% clot occlusion (Fig. 2). His left main and anterior descending arteries were normal. The clot was removed with an aspiration catheter. Thrombolysis in myocardial infarction (TIMI) grade 2 flow was established (Fig. 3). The ostium was dilated but not stented. He was placed on statin, ezetimibe, angiotensin-converting enzyme inhibitor (ACE-I), beta-blocker, and dual antiplatelet therapy.
Six hours later, and while recovering in the high dependency unit, his polymerase chain reaction (PCR) test for COVID-19 came back positive. The patient was informed of the findings of his PCR and the result of his positive COVID-19 PCR test. He was also made aware of the medical and surgical options for the management of his coronary artery aneurysms and that these would be discussed with him after he had recovered from COVID-19. The hospital policy for managing COVID-19 was explained to him, and he was subsequently transferred to the regional COVID-19 hospital. This was in accordance with our healthcare service reorganization plan to manage all COVID-19 patients at dedicated facilities to protect the non-COVID hospitals. He remained asymptomatic at the COVID hospital and was later discharged to an isolation facility. He did not keep his cardiology clinic follow-up appointment at our institution on two separate occasions. Following a telephone inquiry, he claimed to be stressed due to his experience at the COVID hospital and was unwilling to return for a follow-up. He presented again to the emergency department of our hospital 2 months after with symptoms suggestive of an acute stress reaction secondary to COVID-19 infection and hospital experience. He was managed for stress and was discharged home. The patient has provided a written consent for this publication.
Discussion
Our patient had an unusual combination of acute STEMI resulting from thrombotic occlusion of the right coronary artery aneurysm and concomitant COVID-19. This combination led to competing clinical priorities and a potentially poor outcome for the patient.
The incidence of acute myocardial infarction (MI) in patients with COVID-19 is 4.2%, and there is evidence that COVID-19 worsen outcomes in patients with cardiovascular diseases [1]. In addition, COVID-19 can precipitate cardiac injuries such as nonspecific myocardial injury, coronary spasm, non-ischemic cardiomyopathy, and myocardial infarction [3].
Coronary artery aneurysm (CAA) occurs in approximately 4.5% of coronary artery angiographies. It is associated with arteriosclerosis in older patients, but in children, it is often the result of Kawasaki disease, where up to 20% of incidences have been reported in untreated cases [4]. Other causative factors are Takayasu arteritis, coronary artery stent complications, and genetics [5]. Coronary artery aneurysm is often an incidental finding but can occasionally present with complications such as angina, rupture, and STEMI. The reduced blood flow in the aneurysm predisposes to clot formation, leading to partial or complete occlusion of flow distal to the aneurysm. The cause of the patient’s CAA is uncertain. He denied any history of hospital admissions as a child that could suggest Kawasaki disease.
Furthermore, his coronary angiography did not show arteriosclerosis. The patient developed an acute STEMI due to thrombotic occlusion of his right coronary artery. Increased venous and arterial thrombotic complications have been reported in patients with COVID-19 disease [6]. In addition, COVID-19 patients with acute STEMI have an increased thrombus load and higher rates of stent occlusion [7, 8]. It is uncertain how COVID-19 disease contributed to the development of thrombosis in our patient.
Management of CAA is on an individual basis due to a lack of consensus on the best treatment strategy. Small aneurysms (< 10 mm) are treated medically with dual antiplatelet and anticoagulation, while large aneurysms are managed with covered stents [5]. Giant aneurysms require surgical management [9]. Our patient was initially treated medically to expedite his transfer to the COVID-19 hospital. Based on the size of his aneurysm, he was a potential candidate for other interventions, such as covered stent and surgery. However, these options were not fully explored with him as he was lost to cardiology follow-up.
This case illustrates a particular challenge posed by the COVID-19 pandemic. Many emergency services have experienced reduced attendance during the pandemic [10]. A common reason for these is the fear of contracting COVID-19 in the hospital. A similar scenario may play out in high-risk patients who require follow-up. Moreira et al. recently reported a 13% reduction in the follow-up of patients with high-risk cardiovascular conditions [11]. The impact of this observation on patient’ outcomes is unknown, and further studies are required. Our region adopted a system similar to that used in China and Italy, which centralized the care of COVID-19 patients in COVID hospitals, while keeping other hospitals free from the disease [12, 13]. A potential downside is that care of non-COVID-19 diseases may become compromised when such patients are managed in a COVID-19 facility.
Conclusions
Acute myocardial infarction can be precipitated directly and indirectly by COVID-19. Those with underlying cardiovascular conditions are at high risk. Additional efforts must be made to mitigate the reasons for the nonattendance of high-risk patients. Health care reorganization in the face of the COVID-19 pandemic may negatively impact the clinical outcome and patient satisfaction.
Availability of data and materials
Not applicable.
Abbreviations
- CAA:
-
Coronary artery aneurysm
- COVID-19:
-
Coronavirus disease 2019
- MI:
-
Myocardial infarction
- PCR:
-
Polymerase chain reaction
- TIMI:
-
Thrombolysis in myocardial infarction
- STEMI:
-
ST-elevation myocardial infarction
References
Chen R, Liang W, Jiang M, Guan W, Zhan C, Wang T, Tang C, Sang L, Liu J, Ni Z, Hu Y, Liu L, Shan H, Lei C, Peng Y, Wei L, Liu Y, Hu Y, Peng P, Wang J, Liu J, Chen Z, Li G, Zheng Z, Qiu S, Luo J, Ye C, Zhu S, Liu X, Cheng L, Ye F, Zheng J, Zhang N, Li Y, He J, Li S, Zhong N, Medical Treatment Expert Group for COVID-19. Risk factors of fatal outcome in hospitalized subjects with coronavirus disease 2019 from a nationwide analysis in China. Chest. 2020;158(1):97–105. https://doi.org/10.1016/j.chest.2020.04.010 (Epub 2020 Apr 15).
Pessoa-Amorim G, Camm CF, Gajendragadkar P, De Maria GL, Arsac C, Laroche C, Zamorano JL, Weidinger F, Achenbach S, Maggioni AP, Gale CP, Poppas A, Casadei B. Admission of patients with STEMI since the outbreak of the COVID-19 pandemic: a survey by the European Society of Cardiology. Eur Heart J Qual Care Clin Outcomes. 2020;6(3):210–6. https://doi.org/10.1093/ehjqcco/qcaa046.
Guzik TJ, Mohiddin SA, Dimarco A, Patel V, Savvatis K, Marelli-Berg FM, Madhur MS, Tomaszewski M, Maffia P, D’Acquisto F, Nicklin SA, Marian AJ, Nosalski R, Murray EC, Guzik B, Berry C, Touyz RM, Kreutz R, Wang DW, Bhella D, Sagliocco O, Crea F, Thomson EC, McInnes IB. COVID-19 and the cardiovascular system: implications for risk assessment, diagnosis, and treatment options. Cardiovasc Res. 2020;116(10):1666–87. https://doi.org/10.1093/cvr/cvaa106.
Dietz SM, van Stijn D, Burgner D, et al. Dissecting Kawasaki disease: a state-of-the-art review. Eur J Pediatr. 2017;176(8):995–1009. https://doi.org/10.1007/s00431-017-2937-5.
Abou Sherif S, Ozden Tok O, Taşköylü Ö, Goktekin O, Kilic ID. Coronary artery aneurysms: a review of the epidemiology, pathophysiology, diagnosis, and treatment. Front Cardiovasc Med. 2017;4:24. https://doi.org/10.3389/fcvm.2017.00024.
Klok FA, Kruip MJHA, van der Meer NJM, Arbous MS, Gommers DAMPJ, Kant KM, Kaptein FHJ, van Paassen J, Stals MAM, Huisman MV, Endeman H. Incidence of thrombotic complications in critically ill ICU patients with COVID-19. Thromb Res. 2020;191:145–7. https://doi.org/10.1016/j.thromres.2020.04.013 (Epub 2020 Apr 10).
Kelham M, Choudry FA, Hamshere S, Beirne AM, Rathod KS, Baumbach A, Ahluwalia A, Mathur A, Jones DA. Therapeutic implications of COVID-19 for the interventional cardiologist. J Cardiovasc Pharmacol Ther. 2021;26(3):203–16. https://doi.org/10.1177/1074248420982736 (Epub 2020 Dec 17).
Choudry FA, Hamshere SM, Rathod KS, Akhtar MM, Archbold RA, Guttmann OP, Woldman S, Jain AK, Knight CJ, Baumbach A, Mathur A, Jones DA. High thrombus burden in patients with COVID-19 presenting with ST-segment elevation myocardial infarction. J Am Coll Cardiol. 2020;76(10):1168–76. https://doi.org/10.1016/j.jacc.2020.07.022 (Epub 2020 Jul 14).
Potter EL, Meredith IT, Psaltis PJ. ST-elevation myocardial infarction in a young adult secondary to giant coronary aneurysm thrombosis: an important sequela of Kawasaki disease and a management challenge. BMJ Case Rep. 2016. https://doi.org/10.1136/bcr-23.
Mafham MM, Spata E, Goldacre R, Gair D, Curnow P, Bray M, Hollings S, Roebuck C, Gale CP, Mamas MA, Deanfield JE, de Belder MA, Luescher TF, Denwood T, Landray MJ, Emberson JR, Collins R, Morris EJA, Casadei B, Baigent C. COVID-19 pandemic and admission rates for and management of acute coronary syndromes in England. Lancet. 2020;396(10248):381–9. https://doi.org/10.1016/S0140-6736(20)31356-8 (Epub 2020 Jul 14).
Moreira HT, Volpe GJ, Rezek UC, et al. Telemedicine in cardiology for outpatient follow-up of patients at high cardiovascular risk in response to the COVID-19 pandemic. Arq Bras Cardiol. 2021;116(1):153–7. https://doi.org/10.36660/abc.20200715.
Han Y, Zeng H, Jiang H, et al. CSC expert consensus on principles of clinical management of patients with severe emergent cardiovascular diseases during the COVID-19 epidemic. Circulation. 2020;141(20):e810–6. https://doi.org/10.1161/circulationaha.120.047011.
Gamberini L, Coniglio C, Cilloni N, et al. Remodelling of a regional emergency hub in response to the COVID-19 outbreak in Emilia-Romagna. Emerg Med J. 2021. https://doi.org/10.1136/emermed-2020-209671.
Acknowledgements
None.
Funding
None.
Author information
Authors and Affiliations
Contributions
DA, AA, and JA were involved in managing the patient at the emergency department. DA wrote the first draft. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alao, D.O., Alabdouli, A. & Jalabi, A. Coronary artery aneurysm presenting as ST-elevation myocardial infarction in a man with coronavirus disease 2019: a case report. J Med Case Reports 16, 475 (2022). https://doi.org/10.1186/s13256-022-03693-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03693-0