Abstract
Background
Isolated renal hydatid cysts of the kidney are a rare occurrence that account for about 2–3% of all hydatidoses. They can stay asymptomatic for years and could have a variable presentation on imaging techniques, which results in a challenging diagnostic process.
Case presentation
We report a 22-year-old Caucasian male with a large cyst on the upper pole of the left kidney that had no septations nor membrane calcifications on computed tomography, which led to mistakenly considering it a simple renal cyst. The true diagnosis was identified intraoperatively and proven postoperatively by pathology.
Conclusions
This case highlights the importance of keeping echinococcosis in mind when treating suspected renal cysts and tumors to avoid incorrect treatment and possible content spillage, anaphylaxis, and peritoneal dissemination.
Similar content being viewed by others
Background
Cystic echinococcosis (hydatidosis), a parasitic disease caused by the larval form of Echinococcus granulosus, is a common endemic disease in sheep-breeding countries worldwide, where sheep, dogs, and humans live in close contact [1]. In this cycle, humans are an accidental intermediate host through ingestion of Echinococcus eggs shed in feces. The liver is the most involved organ, followed by the lungs, which together account for 90% of cases, while renal echinococcosis is an unusual location in only 2–3% of infections [2]. Although a concurrent localization of renal cysts along with hepatic and/or pulmonary cysts is probable and facilitates the diagnosis, an isolated presentation is hard to differentiate from other renal lesions, as they could cover up to 32% of inspected renal masses [3]. Furthermore, renal hydatid cysts typically remain asymptomatic for years, and therefore grow enormously before being detected after presentation with a constellation of possible symptoms including flank pain, hematuria, pyuria, or intermittent fever [4].
An additional challenge posed by the ambiguity of this presentation is rupture of the iatrogenic cyst, and the consecutive acute abdomen with a 6% mortality rate [5]. This case has been reported in line with the CARE guidelines [6]. Renal hydatid cysts may present with various clinical findings, ranging from asymptomatic clinical course to total loss of renal function. It is beneficial to consider a renal hydatid cyst in patients when treating suspected renal cysts and tumors, especially in societies where hydatid cyst (HC) disease is endemic, even with negative immunological results.
Case presentation
A 22-year-old Caucasian male farmer presented to our surgery clinic with hypogastric discomfort that started 1 month earlier and was not accompanied by severe pain, radiation of pain, nausea, vomiting, burning micturition, flank pain, pyuria, hematuria, or fever. Similarly, he had an insignificant surgical and medical history. His physical examination was normal except for mild tenderness in the left hypochondrium. There were no abnormal pulmonary signs and no peripheral lymphadenopathy.
Complete blood count, renal function tests, and liver function tests were normal with no eosinophilia. Immunological examination revealed negative Echinococcus immunoglobulin (Ig)G antibody titers (reference: negative ≤ 1:160). Urine tests did not reveal any signs of hydatiduria, and chest X-ray was also normal.
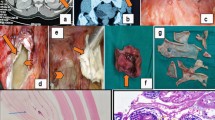
Ultrasonography of the abdomen and pelvis revealed a well-defined lesion in the mid and upper pole of the left kidney, measuring 14 cm in the largest dimension. Contrast-enhanced computed tomography (CECT) of the abdomen and pelvis confirmed these findings, and showed a compression of the kidney downwards, anteriorly, and medially, as well as an upwards pushed spleen. The cyst appeared to have a thickened, nonenhancing, noncalcified regular wall surrounding a homogeneous fluid. No similar lesion in the contralateral kidney, liver, nor lungs could be detected (Fig. 1).
With these findings, a clinical diagnosis of a simple renal cyst was made, with a suspicion of renal hydatid disease. A transabdominal retroperitoneal approach through a subcostal incision was planned, with the aim of organ preservation. During the exploration, a large cystic structure was found to arise from the middle and the upper pole of the left kidney. After sucking the inner cyst fluid, we strongly suspected a hydatid disease; therefore, the operation field was protected with swabs soaked in 20% hypertonic saline. The cyst was opened and contents were evacuated, and 20% hypertonic saline was instilled as a scolicidal agent owing to the high probability of an uncontrolled spillage of content. Finally, the cyst was excised with a rim of normal parenchyma, and the specimen was sent for pathological examination (Fig. 2).
Histopathologic examination confirmed the hydatidosis with the presence of a laminated acellular and eosinophilic membrane along with many scolices in the cystic lumen (Fig. 3).
The patient was discharged on the third postoperative day with oral albendazole 400 mg for 3 months. No recurrence was detected in the postoperative 3- and 6-month follow-up ultrasound (USG) and 6-month follow-up computed tomography (CT) scan, and the patient remained in good health with normal renal function.
Discussion
In this study, we report a 22-year-old male with a large cyst on the upper pole of the left kidney that had no septations nor membrane calcifications on CT-scan, which led to mistakenly considering it a simple renal cyst. The true diagnosis was guessed intraoperatively and proven postoperatively by pathology. Renal hydatid cysts may present with various clinical findings, ranging from asymptomatic clinical course to total loss in renal function. It is beneficial to keep echinococcosis in mind when treating suspected renal cysts and tumors.
Echinococcosis is a common endemic disease that presents with cysts in different organs, predominantly the liver and the lungs, with a rare settlement elsewhere. It could be a problematic disease to cure when it disseminates [2]. In the seldom cases of renal localization, the cyst is often located in the upper pole (37% of reported cases) [4]. The ages of the affected patients ranged between 30 and 50 years [21], while, perhaps surprisingly, renal hydatid disease is extremely rare in the pediatric population, accounting for approximately 1.9% of all cases [19, 20]. However, a high suspicion of this disease should be considered in any cystic mass of the kidney in children, especially in endemic regions. Diagnostic and therapeutic methods conform with those applied to hepatic and pulmonary hydatidosis, including ultrasonography, serology, and CT, in addition to postoperative histopathology [3].
However, the isolated occurrence of renal hydatid cysts presents a diagnostic challenge, as the clinical and imaging findings could either be understated and the cyst considered a simple renal cyst, especially with the absence of internal septation and mural calcifications, or on the contrary, overstated and feared to be malignant when it has a lobulated appearance [7, 8]. Others also misinterpreted the findings for an abscess [9]. In this case, the patient presented with a cyst void of septations and membrane calcifications on CECT, and the absence of positive Echinococcus immunoglobulin (Ig)G antibody titers, as well as hydatiduria, led to a misdiagnosis of a simple renal cyst. Only after the pathology report were we able to establish a specific diagnosis.
Treatment is modulated based on different factors. Conservative treatment requires a confident diagnosis, which was unavailable. Percutaneous management (puncture, aspiration, injection of scolicidal agent, reaspiration) might be a safe option [10]. However,there are some disadvantages to this method, including dissemination of daughter cysts and fatal anaphylaxis [11, 12]. Surgical treatment is the other option and could take the form of complete excision of the cyst with pericystectomy, or partial/complete nephrectomy depending on the residual functional parenchyma. This requires extreme caution to avoid spillage, recurrence, or the development of severe anaphylactic shock [13].
Although laparoscopy, transperitoneal and retroperitoneal, has been reported in cases of hydatid renal cysts [14, 15], such procedures can only be performed at centers with vast experience in laparoscopic surgery. An open surgical approach is preferred at developing centers where laparoscopic expertise is not available, as in our case. Based on our findings, we went for a transabdominal retroperitoneal approach. Postoperatively, we gave the patient prophylactic albendazole as per international recommendations [16].
It is worth noting that during the last decade, the number of urological laparo-endoscopic single-site (LESS) procedures performed worldwide has increased. Symeonidis et al. reported that in the hands of experienced surgeons, LESS seems a feasible, efficient, and less invasive alternative to standard/conventional laparoscopy [17]. Moreover, Zouari et al. assessed the feasibility and outcomes of pediatric LESS, successfully treating one renal hydatid cyst (RHC) case [18]. There is no doubt that if this endoscopic technique is applied in the management of RHC in adults, it may have some advantages, although this depends on many factors and perhaps future studies can evaluate this.
Conclusions
Isolated hydatidosis of the kidney is a rare entity that could easily be confused with renal cysts, malignancies, and abscesses, thus it is important to keep in mind as a crucial differential diagnosis in such cases to avoid incorrect surgical intervention, and possible content spillage, anaphylaxis, and peritoneal dissemination.
References
Budke CM, Carabin H, Ndimubanzi PC, et al. A systematic review of the literature on cystic echinococcosis frequency worldwide and its associated clinical manifestations. Am J Trop Med Hyg. 2013;88(6):1011–27. https://doi.org/10.4269/ajtmh.12-0692.
McManus DP, Zhang W, Li J, Bartley PB. Echinococcosis. Lancet. 2003;362(9392):1295–304. https://doi.org/10.1016/S0140-6736(03)14573-4.
Horchani A, Nouira Y, Kbaier I, Attyaoui F, Zribi AS. Hydatid cyst of the kidney. A report of 147 controlled cases. Eur Urol. 2000;38(4):461–7. https://doi.org/10.1159/000020325.
Zmerli S, Ayed M, Horchani A, Chami I, El Ouakdi M, Ben Slama MR. Hydatid cyst of the kidney: diagnosis and treatment. World J Surg. 2001;25(1):68–74. https://doi.org/10.1007/s002680020009.
Dziri C, Haouet K, Fingerhut A, Zaouche A. Management of cystic echinococcosis complications and dissemination: where is the evidence? World J Surg. 2009;33(6):1266–73. https://doi.org/10.1007/s00268-009-9982-9.
Gagnier JJ, Kienle G, Altman DG, et al. The CARE guidelines: consensus-based clinical case reporting guideline development. J Med Case Rep. 2013;7:223. https://doi.org/10.1186/1752-1947-7-223.
Singh V, Devana SK, Gorsi U, Bal A. Isolated renal hydatid cyst masquerading as cystic renal tumor. Urology. 2019;133:e11–2. https://doi.org/10.1016/j.urology.2019.07.014.
Kilciler M, Bedir S, Erdemir F, Coban H, Sahan B, Ozgok Y. Isolated unilocular renal hydatid cyst: a rare diagnostic difficulty with simple cyst. Urol Int. 2006;77(4):371–4. https://doi.org/10.1159/000096345.
Gupta R, Kapoor R, Mandhani A, Dubey D. Renal hydatid cyst presenting as perinephric and iliopsoas abscess. Urol Int. 2004;73(2):178–80. https://doi.org/10.1159/000079701.
Goel MC, Agarwal MR, Misra A. Percutaneous drainage of renal hydatid cyst: early results and follow-up. Br J Urol. 1995;75(6):724–8. https://doi.org/10.1111/j.1464-410x.1995.tb07379.x.
Buckley RJ, Smith S, Herschorn S, Comisarow RH, Barkin M. Echinococcal disease of the kidney presenting as a renal filling defect. J Urol. 1985;133(4):660–1. https://doi.org/10.1016/s0022-5347(17)49134-8.
Roylance J, Davies ER, Alexander WD. Translumbar puncture of a renal hydatid cyst. Br J Radiol. 1973;46(551):960–3. https://doi.org/10.1259/0007-1285-46-551-960.
Ameur A, Lezrek M, Boumdin H, Touiti D, Abbar M, Beddouch A. Le kyste hydatique du rein. Traitement à propos de 34 cas [Hydatid cyst of the kidney based on a series of 34 cases]. Prog Urol. 2002;12(3):409–14.
Ozden E, Bostanci Y, Mercimek MN, Yakupoglu YK, Yilmaz AF, Sarıkaya S. Renal hydatid cyst treatment: retroperitoneoscopic “closed cyst” pericystectomy. Int J Urol. 2011;18(3):237–9. https://doi.org/10.1111/j.1442-2042.2010.02703.x.
Shah KJ, Ganpule AP, Desai MR. Isolated renal hydatid cyst managed by laparoscopic transperitoneal nephrectomy. Indian J Urol. 2009;25(4):531–3. https://doi.org/10.4103/0970-1591.57925.
Velasco-Tirado V, Alonso-Sardón M, Lopez-Bernus A, et al. Medical treatment of cystic echinococcosis: systematic review and meta-analysis. BMC Infect Dis. 2018;18(1):306. https://doi.org/10.1186/s12879-018-3201-y.
Symeonidis EN, Nasioudis D, Economopoulos KP. Laparoendoscopic single-site surgery (LESS) for major urological procedures in the pediatric population: a systematic review. Int J Surg. 2016;29:53–61. https://doi.org/10.1016/j.ijsu.2016.03.040.
Zouari M, Ben Dhaou M, Ammar S, Jallouli M, Mhiri R. Laparoendoscopic single-site (LESS) surgery in pediatric urology: a 4-year experience. Curr Urol. 2019;12(3):153–7.
Sarmast AH, Sherwani AY, Dangroo SA, Wani MS, Hamid A, Showkat HI. An isolated renal hydatid cyst in a 6-year-old child: a rare case report. J Res Med Sci. 2014;19(3):279–81.
Demir M, Yağmur İ. Isolated renal hydatid cyst in a 6-year-old boy: a case report. Iran J Parasitol. 2021;16(4):692–6. https://doi.org/10.18502/ijpa.v16i4.7883.
Aragona F, Di Candio G, Serretta V, Fiorentini L. Renal hydatid disease: report of 9 cases and discussion of urologic diagnostic procedures. Urol Radiol. 1984;6(3–4):182–6. https://doi.org/10.1007/BF02923720.
Acknowledgments
Not applicable.
Funding
No funding was received for this publication.
Author information
Authors and Affiliations
Contributions
MH: Introduction, case presentation, discussion, and review of the manuscript. SA: Discussion and review of the manuscript. AA: supervisor and last author, review of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal
Competing interests
The authors declare that they have no competing interests.
Availability of data and materials
Not applicable.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hammade, M., Alhoulaiby, S. & Ahmed, A. Isolated giant renal hydatid cyst with a simple renal cyst appearance: a case report. J Med Case Reports 16, 386 (2022). https://doi.org/10.1186/s13256-022-03630-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03630-1