Abstract
Background
Aggressive angiomyxoma (AAM) is a locally infiltrative mesenchymal tumour that most commonly affects the pelvis and/or perineum in adult women. AAM is very rare in males, especially in infancy.
Case presentation
A 10-month-old fulani (African) male infant was referred to our department for a large painless mass in the right testicule. The mass was detected during the neonatal period and gradually increased in size. Ultrasound examination revealed a large heterogeneous lesion; computed tomography results led to the conclusion that the mass was a mesenteric hernia. An inguinal and scrotal surgical approach was adopted. Exploratory surgery found a normal right testicle displaced upwardly and a large scrotal mass. Radical excision of the mass and orchidopexy were performed. Subsequent histology and immunohistochemstry studies indicated that the mass was a scrotal angiomyxoma. The postoperative course was uneventful. No recurrence occurred during the 6-month follow-up.
Conclusion
To the best of our knowledge, this is the youngest patient with AAM reported to date. Angiomyxoma should be included in the differential diagnosis of scrotal masses, for which radical excision is justifiable to prevent recurrence.
Similar content being viewed by others
Introduction
Aggressive angiomyxoma (AAM) is a rare benign myxoid mesenchymal tumour. It is a non-metastasizing soft tissue tumour of the pelvis and perineum and occurs almost exclusively in adult females [1, 2], with only rare reports of AAM in males or involving the scrotum. Scrotal AAM mimics common paediatric pathologies, including hernia or hydrocele [2]. The recommended treatment for symptomatic patients is wide excision with tumour-free margins and close postoperative monitoring [3, 4]. Here, we report a case of AAM in a 10-month-old male who presented with voluminous slow-growing scrotal swelling.
Case report
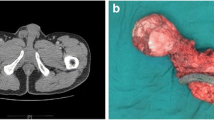
A 10-month-old fulani (African) male infant was referred to our paediatric surgery department for a scrotal mass. The mass was first detected during the neonatal period and gradually increased in size. The infant had no known medical, surgical or family history. Clinical examination revealed an infant in good general condition, good nutritional status and an afebrile state with a voluminous right scrotal mass that was painless, spherical, soft, regular in shape and 10 cm in diameter, with some collateral venous circulation. A mass effect on the penis and perineum could be observed (Fig. 1). There was no transillumination. The right testicle was not found, and the left testicle was in the testicular bursa and appeared to be healthy. The clinical impression was initially oriented towards a testicular tumour diagnosis. Ultrasound examination revealed a large structural mass, with the heterogeneous echo measuring 10 × 7 × 6 cm. The two testes were upwardly displaced by the mass. Abdominopelvic computed tomography (CT) demonstrated a large intrascrotal tissue mass communicating with the abdomen with no visible air component, leading to the decision that the mass was probably an inguinal mesenteric hernia.
Serum tumour biomarkers, including α-fetoprotein and β-human chorionic gonadotropin levels, were all within normal limits. Surgery for the testicular tumour was proposed. Two combined surgical incision approaches were adopted, in which the right inguinal approach made it possible to locate the healthy right testicle in the inguino-scrotal region. The scrotal route was chosen for wide excision. During surgery, a vascular mass that displaced the testis upwards was found between the spermatic fascia and the skin (Fig. 2). The boundary of the tumour was not well circumscribed, and the originating organ of the tumour could not be determined. Scrotoplasty and right orchidopexy were performed. The dimensions of the lump were 11 × 9.5 × 8.5 cm and it weighed 400 g. The lump had two different appearances: one portion had the appearance of a typical solid tumour and the other showed mixed tumour growth. Microscopy examination revealed that the tumour had the histological appearance of a benign fibroblastic tumour, which was initially suggestive of angiomyxoma (Fig. 3a, b); the absence of malignancy suggested the need for an immunohistochemistry study to support this diagnosis.
Immunohistochemical staining for CD34, smooth muscle actin, desmin, myogenin and protein S was performed, with positive staining found only for CD34 in the tumor (Fig. 4a). Actin staining was seen in the walls of the vessels and bundles of smooth muscle cells encompassing the tumour (Fig. 4b); desmin staining was observed in the bundles of smooth muscle cells (Fig. 4c). Staining for the other markers was negative. This study confirmed the diagnosis of benign scrotal angiomyxoma and ruled out cell-based fusiform rhabdomyosarcoma. There were no postoperative surgical complications. No further recurrence was identified in the 6 months following surgery (Fig. 5).
Histological features of angiomyxoma. a Microscopic image showing diffuse paucicellular proliferation with prominent vessels on a myxoid background (haematoxylin and eosin staining, magnification: ×50), b higher magnification showing spindle cells with oval nuclei without atypia (haematoxylin & eosin staining, magnification: ×400)
Discussion
Aggressive angiomyxoma is a rare tumour that is locally infiltrative but non-metastasizing. It occurs nearly exclusively in adult women of childbearing age and almost always arises in the perineum and pelvic area [5], occurring only rarely in other sites, such as the vagina, urinary bladder, various cutaneous locations, soft tissue of the perineum and perianal region, or in the uterine cavity as a polyp [1, 5, 6]. In males, AAM involves analogous sites, usually the scrotum[7, 8]. In our case, the tumour was located in the right scrotum. AAM is extremely rare in childhood [9]. To the best of our knowledge, the present case is the eighth to be reported in children, and it describes the youngest patient reported with AAM. Patients usually present with a long history of disease due to the slow growth of the tumour, without a history of pain, injury, fever or urinary tract symptoms. In general, AAM does not lead to distal metastases, and malignant transformation has not been observed [10]. During physical examination, AAM can mimic other common conditions causing scrotal enlargement; the tumour may present as a scrotal mass, which is often mistaken for a hernia or hydrocele [2, 4]. In our case, based on the results of the CT examination, we concluded that the mass was a mesenteric hernia.
Tumour markers (alpha-fetoprotein, beta-human chorionic gonadotropin) and hormone levels (testosterone) contribute to the differential diagnosis and management of testicular masses in boys [11]. A few reported cases have included preoperative diagnoses based on histology. However, in most of the cases described to date, the diagnosis was made postoperatively following histological examination of the mass [4]. The diagnosis and distinction of AAM from other benign and malignant myxoid soft tissue tumours is mainly based on morphology and the exclusion of mimicking lesions with the help of immunohistochemistry [10]. Immunohistochemically, the cells expressed vimentin and, especially in peri-genital tumours, were positive for smooth muscle actin; in 50% of the tumours, CD34 positivity and S-100 negativity were observed. Most tumours showed positive oestrogen and progesterone expression, which expands the therapeutic options [11]. Our immunohistochemistry results were generally compatible with those reported previously.
AAM must be differentiated from other benign myxoid neoplasms given its propensity for local recurrence, such as intramuscular myxoma, myxoid neurofibroma, neurothekeoma, spindle cell lipoma, superficial angiomyxoma, angiomyofibroblastoma, angiomyxolipoma and benign mixed mesenchymal tumours [12]. The more effective treatment for AAM is radical surgical excision that leads to free margins. Radiation therapy has been proposed to control multiple recurrences after surgical excision but has led to poor results; chemotherapy has also been shown to lead to poor results in AAM because of the slow progression of the disease. Incomplete excision almost always results in locoregional recurrence [4]. In the present case, no recurrence was found at the 6-month follow-up. Because late recurrence is possible, close follow-up remains necessary [4, 10].
Conclusion
Aggressive angiomyxoma is a very rare benign neoplasm that is predominantly found in adult women. The present case describes the youngest male patient with AAM to date. Clinical examination and histology and immunochemistry studies were the main bases for the diagnosis of scrotal AAM, for which wide excision is justifiable to prevent recurrence.
Availability of data and materials
All data generated or analysed during this study are included in this published article.
References
Chuang FP, Wu ST, Lee SS, et al. Aggressive angiomyxoma of the scrotum. Arch Androl janv. 2002;48(2):101–6.
Korecka KK, Hyla-Klekot LE, Kudela GP, Paleń PA, Kajor MW, Koszutski TK. Aggressive angiomyxoma in an 11-year-old boy—diagnostic and therapeutic dilemmas: an unusual case report and review of the literature. Urology. 2020;144:205–7.
Koito R, Kohda F, Dugu L, Suenaga A, Ichiki T, Furue M. Scrotal angiomyxoma. Australas J Dermatol. 2020;61(1):78–9.
Kirkilessis G, Kakavia K, Bougiouklis D, Papadopoulos A, Lampropoulos C, Kirkilessis I. Aggressive angiomyxoma to 57-year old man. J Surg Case Rep. 2020;2020(9):rjaa313. https://doi.org/10.1093/jscr/rjaa313.
Andres LA, Mishra MJ. Angiomyxoma diagnosed in a man presenting for abdominal lipectomy. Can J Plast Surg J Can Chir Plast. 2007;15(3):163–4.
Skálová A, Zámečník M, Michal M, Opatrny V. Aggressive angiomyxoma presenting as polyp of uterine cavity. Pathol Res Pract. 2000;196(10):719–25.
Aydin AM, Katipoglu K, Baydar DE, Bilen CY. Long-standing aggressive angiomyxoma as a paratesticular mass: a case report and review of literature. SAGE Open Med Case Rep. 2017;5:2050313X17712090. https://doi.org/10.1177/2050313X17712090.
Ismail MI, Wong YP, Tan GH, Fam XI. Paratesticular aggressive angiomyxoma: a rare case. Urol Ann. 2017;9(2):197–9.
Kawamura M, Matsumoto F, Matsui F, Yazawa K, Shimada K. Aggressive angiomyxoma of the vulva mimicking clitoromegaly in a young child. Urology. 2017;101:142–4.
Neyaz A, Husain N, Anand N, Srivastava P. Rare paratesticular aggressive angiomyxoma with negative oestrogen and progesterone receptors in a male patient. BMJ Case Rep. 2018;2018:bcr2017222164.
Draeger DL, Protzel C, Hakenberg OW. Aggressive angiomyxoma as a rare differential diagnosis of enlargement of the scrotum. Clin Genitourin Cancer. 2016;14(2):e237–9.
Kim H-S, Park S-H, Chi JG. Aggressive angiomyxoma of childhood: two unusual cases developed in the scrotum. Pediatr Dev Pathol. 2003;6(2):187-91.
Acknowledgements
Not applicable.
Funding
Not applicable.
Author information
Authors and Affiliations
Contributions
NL designed and drafted the study and wrote the manuscript. IS helped design and draft the study and collected the data. EB and IB performed the laboratory examinations and created the figures. ZA performed the immunochemistry study and created the figures.d KA performed the immunochemistry experiments and collected data. MH, MO and AH designed the study and critically revised the manuscript. The authors received no specific funding for this study. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian for publication of this case report and any accompanying images. A copy of the written consent will be available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Nyandwi, L., Idrissa, S., Moustapha, H. et al. Aggressive angiomyxoma as a rare cause of scrotum enlargement in a 10-month-old boy: a case report. J Med Case Reports 16, 293 (2022). https://doi.org/10.1186/s13256-022-03497-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03497-2