Abstract
Background
Giant parathyroid adenoma is a type of parathyroid adenoma weighing > 3.5 g and having a size of more than 2 cm.
Case presentation
This report describes giant primary parathyroid adenoma with reference to the literature. We report the case of a 48-year-old Persian man referred to the clinic with knee and lower back pain. He had a history of mitral valve replacement and several episodes of bilateral nephrolithiasis. After a thorough assessment, a neck mass with a possible thyroid origin was detected, but further assessment showed it was of parathyroid origin. The resected mass was 9 × 6× 4 cm and weighed 122 g, and histopathology showed a giant parathyroid adenoma.
Conclusion
Giant parathyroid adenomas that weigh more than 110 g and are larger than 8 cm can lead to significant hypercalcemia. Despite giant parathyroid adenomas and high parathyroid hormone levels, a calcium crisis may not always occur in these patients, and the masses may be initially misdiagnosed as a thyroid mass.
Similar content being viewed by others
Background
Primary hyperparathyroidism (PHPT) is the most common disease of parathyroid glands and the third most common endocrine disease [1, 2]. The prevalence of PHPT in the general population is 22 per 100,000. In postmenopausal women, the prevalence reaches up to 1 per 500. Parathyroid adenoma is the cause of 80–90% of PHPT. The remaining 10–20% of PHPT cases are due to parathyroid hyperplasia, and < 1% are due to parathyroid carcinoma 4. Giant parathyroid adenoma (GPA) is an adenoma with a weight > 3.5 g and diameter > 2 cm. The average weight of the parathyroid gland is about 70 mg to 1 g [1, 3]. The mainstay of the pathophysiology of hyperparathyroidism is hypersecretion of parathyroid hormone (PTH), which leads to the release of calcium from bone cells by inhibiting osteoblasts and stimulating osteoclast activity. PTH stimulates calcium reabsorption and inhibits phosphate reabsorption in kidneys. Additionally, PTH stimulates calcium absorption from the gut [3] by stimulating the conversion of 25-hydroxyvitamin D to 1,25-hydroxyvitamin D.
Clinical manifestations of PHPT include nephrolithiasis, osteoporosis–osteopenia, pancreatitis, depression, cognitive disorders, and others. The severity of symptoms correlates with the adenoma’s weight and PTH level [1, 3]. Patients with hypercalcemia may experience a life-threatening hypercalcemic crisis due to the high level of PTH secondary to a parathyroid carcinoma or a giant parathyroid adenoma [4, 5]. Since the most common cause of PHPT is adenoma and most adenomas are asymptomatic, PHPT cases are mostly diagnosed during screening tests with elevated calcium and parathormone levels [2, 3].
Previously, the largest reported GPA was 8 × 5 × 3.5 cm with a weight of 110 g [6] and was associated with hypercalcemia (3.21 mmol/L or 12.84 mg/dL).
Case presentation
A 48-year-old Persian man from Urmia, Iran, presented to Imam Hospital with knee pain, lower back pain, fatigue, and dizziness for the last 2 months. The patient had a history of mitral valve replacement 30 years earlier, several bilateral nephrolithotripsies, and diabetes mellitus under control with oral medication. His vital signs were typical. There was a palpable large and soft nodule in the left lobe of his thyroid, which moved with swallowing. A scar of previous cardiac surgery was visible on the chest. The rest of the examination was normal.
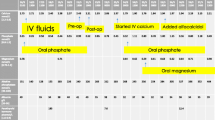
Color Doppler ultrasonography of the thyroid and parathyroid indicated a single isoechoic nodule in the right lobe (12 × 9.5 mm) and two cystic nodules in the left lobe (40 × 23 mm and 30 × 16 mm) of his thyroid. A cystic mass in the region of the left lobe of the thyroid was visible on computed tomography (CT), in contrast to the patient’s biochemistry, indicative of parathyroid carcinoma (Fig. 1). The mentioned findings were approved using 99mTc-MIBI scintigraphy. His complete blood count (CBC) was normal, and the results of the biochemical tests are presented in Table 1. Calcium and PTH serum levels were 14.6 mg/dL and 2702 pg/mL, respectively. Moreover, urine analysis revealed trace proteinuria, with two to three red blood cells (RBCs) per high-power field (HPF).
Based on the patient’s lab and imaging findings, the probability of a parathyroid carcinoma was high enough to send the patient to surgery for tumor resection.
The operation was performed under general anesthesia. After creating a large collar incision (12 cm length) two-finger width above the suprasternal notch, subplatysmal flaps were created as a routine thyroidectomy procedure. The raphe between strap muscles was opened, and the muscles were incised on the left near the upper pole of the thyroid.
On initial evaluation after the thyroid was exposed, it appeared as a thyroid mass displacing the carotid sheath laterally and extending into the mediastinum as a retrosternal goiter. However, further evaluation showed a central posterior neck mass with extension to mediastinum that displaced carotid sheath laterally and the left lobe of the thyroid superior and medially. The inferior thyroidal artery crossed the mass toward the carotid sheath. These findings favored a parathyroid origin, most likely from the superior parathyroid glands. The inferior thyroid artery was ligated as laterally as possible, and then the lateral side of the tumor was dissected out with sharp and blunt dissection, and the tumor was pulled out of the mediastinum to the neck (Fig. 2). The recurrent laryngeal nerve was explored between the trachea and medial side of the tumor, that is, the mass was located dorsal to the recurrent laryngeal nerve (further evidence of superior parathyroid origin of the tumor).
Owing to the PTH value, size of the tumor, and adhesion to adjacent tissues, the patient was diagnosed with parathyroid carcinoma, and the tumor, right lobe of the thyroid, and adjacent lymph nodes were resected. After inserting a Hemovac drain, the neck wound was closed. The resected mass had a size of 9 × 6 × 4 cm and weighed 122 g. Since the mass was descended to the retro-esophageal space and was located posterior to the recurrent laryngeal nerve, we believe it originated from the superior parathyroid gland.
The postoperative period was eventless. In the first 24 hours, an intravenous infusion (drip) of calcium gluconate was given to prevent bone hunger syndrome. Liquid diet was started in the second 24 hours, and the patient was discharged on the third postoperative day with oral CaCO3 and calcitriol pearls gradually tapered until discontinued after 2 weeks.
Histopathological assessment of the resected mass revealed a parathyroid adenoma and multinodular goiter of the resected thyroid lobe (Fig. 3). No lymph node or local invasion, vascular invasion, or perineural invasion was reported on histopathological assessment, and there was no significant invasion of adjacent structures or organs. Finally, the patient was followed up for 12 months without any problems.
Discussion
Primary hyperparathyroidism (PHP) is the third most common endocrine disorder and is usually due to parathyroid adenoma. Parathyroid carcinoma is the least common cause of PHP but should be considered in the differential diagnosis of PHP when the serum calcium (mg/dL) level is above 14 or PHP is associated with a palpable neck mass [7,8,9]. The symptoms result from high levels of PTH and higher reabsorption of Ca from bones, renal tubules, and the gut, causing hypercalcemia [1, 2, 10, 11]. However, giant parathyroid adenoma can cause anatomical symptoms due to the large tumor size, including dysphagia, odynophagia, and dyspnea [12, 13]. Clinical studies show that hypercalcemia is very common in cases presenting with parathyroid mass. Owing to the increase in PTH levels and parathyroid function, ultrasonography and 99mTc-MIBI scintigraphy facilitate the diagnosis of giant parathyroid adenoma [14].
The patient had been suffering from recurrent bilateral nephrolithiasis. Considering his back and bone pain, the adenoma might have been chronically functional, so the patient had not experienced calcium crisis symptoms. Diagnosis of a parathyroid mass was made on the basis of lab findings, including high calcium and PTH levels. While the CBC was as expected, the level of PTH was almost 50 times its expected value. Previous studies have shown that parathyroid carcinoma occurs with equal frequency in both sexes and usually increases serum PTH to five- to tenfold of the normal upper limit [8, 9, 11]. Furthermore, some criteria increase parathyroid carcinoma likelihood, including “local invasion of contiguous structures” or “lymph node or distant metastases.”
However, the calcium level was not as high as the PTH level, which could be due to chronic elevation of PTH or genetic resistance to PTH [15].
At that point, we had no evidence to prove either option. After tumor resection and putting the patient on calcium and calcitriol for several months, then tapering them, the patient no longer had symptoms of hypo- or hyperparathyroidism, which ruled out any genetic disorder of Ca metabolism.
In summary, hyperparathyroidism should be considered in the differential diagnosis of any neck and cervical mass, even though it is a sporadic tumor.
Conclusion
This case report describes the largest giant parathyroid adenoma that has ever been diagnosed, although the size of the mass, location, and imaging might be misleading. It should be noted that very high levels of parathormone may not always lead to calcium crisis signs and symptoms.
Availability of data and materials
Not applicable.
Abbreviations
- PHPT:
-
Primary hyperparathyroidism
- GPA:
-
Giant parathyroid adenoma
- PTH:
-
Parathyroid hormone
References
Spanheimer PM, Stoltze AJ, Howe JR, Sugg SL, Lal G, Weigel RJ. Do giant parathyroid adenomas represent a distinct clinical entity? Surgery. 2013;154:714–9.
Neagoe RM, Sala DT, Borda A, Mogoanta CA, Muhlfay G. Clinicopathologic and therapeutic aspects of giant parathyroid adenomas—three case reports and short review of the literature. Rom J Morphol Embryol. 2014;55:669–74.
Salehian MT, Namdari O, Mohammadi SS, Yousofabad HF. Primary hyperparathyroidism due to a giant parathyroid adenoma: a case report. Int J Endocrinol Metab. 2009;7(2):101–5.
Rutledge S, Harrison M, O’Connell M, O’Dwyer T, Byrne MM. Acute presentation of a giant intrathyroidal parathyroid adenoma: a case report. J Med Case Rep. 2016;10:1–6.
Asghar A, Ikram M, Islam N. A case report: giant cystic parathyroid adenoma presenting with parathyroid crisis after vitamin D replacement. BMC Endocr Disord. 2012;12:1–6.
Power C, Kavanagh D, Hill AD, O’Higgins N, McDermott E. Unusual presentation of a giant parathyroid adenoma: report of a case. Surg Today. 2005;35:235–7.
Wei CH, Harari A. Parathyroid carcinoma: update and guidelines for management. Curr Treat Options Oncol. 2012;13:11–23.
Ruda JM, Hollenbeak CS, Stack BC Jr. A systematic review of the diagnosis and treatment of primary hyperparathyroidism from 1995 to 2003. Otolaryngol Head Neck Surg. 2005;132:359–72.
Ozolins A, Narbuts Z, Vanags A, Simtniece Z, Visnevska Z, Akca A, Wirowski D, Gardovskis J, Strumfa I, Goretzki PE. Evaluation of malignant parathyroid tumours in two European cohorts of patients with sporadic primary hyperparathyroidism. Langenbecks Arch Surg. 2016;401:943–51.
Aoyagi T. Large parathyroid adenoma presented with prominent hypercalcemia. Jpn J Clin Urol. 2001;55:75–8.
Quinn CE, Healy J, Lebastchi AH, Brown TC, Stein JE, Prasad ML, Callender GG, Carling T, Udelsman R. Modern experience with aggressive parathyroid tumors in a high-volume New England referral center. J Am Coll Surg. 2015;220:1054–62.
Liu F, Dong M, Zhu Y, Zhang Y, Fan QH. Clinical features of parathyroid space-occupying lesions. Chin J Otorhinolaryngol Head Neck Surg. 2009;44:282–6.
Ziaeean B, Sohrabi-Nazari S. Huge parathyroid adenoma with dysphagia presentation; a case report from southern Iran. Iran J Med Sci. 2016;41:446.
Yang Z, Zhu L, Wang PZ. Diagnosis and surgical treatment of 48 cases of parathyroid adenoma and parathyroid carcinoma. Chin J Oncol. 2006;28:625–7.
Elli FM, Pereda A, Linglart A, de Nanclares GP, Mantovani G. Parathyroid hormone resistance syndromes—inactivating PTH/PTHrP signaling disorders (iPPSDs). Best Pract Res Clin Endocrinol Metab. 2018;32:941–54.
Acknowledgments
We wish to show our appreciation to the operating room personnel, department of surgery, and department of internal medicine of Imam Hospital for their help diagnosing and treating the patient.
Funding
This study has no funding body. There was no corporate or governmental funding.
Author information
Authors and Affiliations
Contributions
In this case report, RM was the chief surgeon and supervisor. AS and BN contributed to data collection and manuscript writing. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The patient’s identity was kept confidential in the article. The patient signed an informed consent form approved by the ethics committee of both Imam Hospital and Urmia University of Medical Sciences.
Consent for publication
Written informed consent was obtained from the patient to publish this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Mahmodlou, R., Sedokani, A., Pezeshk, A. et al. Giant parathyroid adenoma: a case report. J Med Case Reports 16, 150 (2022). https://doi.org/10.1186/s13256-022-03401-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03401-y