Abstract
Background
Unstable hemoglobinopathies are rare inherited disorders of hemoglobin causing a reduction of hemoglobin molecule solubility. This results in an unstable hemoglobin tetramer/globin polypeptide, which precipitates within the red blood cell. Affected red blood cells have a reduced lifespan due to oxidative stress and cellular rigidity, and tend to be phagocytized by spleen macrophages more rapidly. Unstable hemoglobin is frequently under- or misdiagnosed, because its clinical presentation varies broadly. Therefore, testing for unstable hemoglobinopathies is indicated in cases of unexplained hemolytic anemia. However, this approach is not systematically followed in clinical practice.
Case report
A 25-year-old Caucasian man with a recent history of a presumed viral upper respiratory infection was referred to the hematology outpatient clinic because of hemolytic anemia. The patient had scleral icterus, moderate splenomegaly, and mild macrocytic anemia with high reticulocyte count. Unconjugated bilirubin and lactate dehydrogenase were elevated. Haptoglobin was undetectable. Direct antiglobulin test was negative. Blood smear examination revealed anisopoikilocytosis, polychromasia, bite cells, and basophilic stippling, but no Heinz bodies. High-performance liquid chromatography and capillary electrophoresis showed slightly increased hemoglobin A2, normal fetal hemoglobin, and a variant hemoglobin. Deoxyribonucleic Acid sequencing revealed the heterozygous mutation c430delC in the beta-globin gene hallmark of hemoglobin Montreal II and the heterozygous mutation c287C>T in the alpha-globin gene corresponding to hemoglobin G-Georgia, indicative of the not yet described combination of double-heterozygous hemoglobin Montreal II and hemoglobin G-Georgia variants. Hemoglobinopathy Montreal II was here not associated with β-thalassemia syndrome, and carriers did not show ineffective erythropoiesis. In addition to the case report, we provide information about the largest pedigree with hemoglobinopathy Montreal II identified to date.
Conclusion
We emphasize that a transitory acute condition may uncover an underlying inherited red blood cell disorder. In this regard, awareness should be raised among hematologists caring for adult patients that unstable hemoglobinopathies should be considered in the differential diagnosis of unexplained hemolytic anemias.
Similar content being viewed by others
Introduction
Unstable hemoglobinopathies are rare inherited disorders of hemoglobin (Hb) [1]. More than 200 unstable Hb variants have been reported [2]. They cause a reduction of Hb molecule solubility, resulting in an unstable Hb tetramer/globin polypeptide, which precipitates within the red blood cell (RBC). Affected RBCs have a reduced lifespan due to oxidative stress and cellular rigidity, and tend to be phagocytized by spleen macrophages more rapidly [3].
Unstable Hb is frequently under- or misdiagnosed, because its clinical presentation varies broadly. Therefore, testing for unstable hemoglobinopathies is indicated in cases of unexplained hemolytic anemia.
Here, we report a case of unstable hemoglobinopathy in a young adult with unexplained hemolytic anemia, which manifested first during a presumed viral infection, and show his pedigree (Fig. 1). We display the diagnostic steps highlighting the importance of blood smear examination in patients with negative direct anti-globulin (DAT) hemolytic anemia.
Case presentation
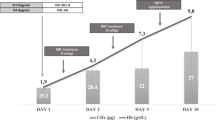
The index case, a 25-year-old Caucasian man (pedigree III.3, Fig. 1) who consulted the otolaryngology outpatient clinic for a presumed viral upper respiratory tract infection, was referred 2 days later to the hematology outpatient clinic because of the suspicion of an hemolytic anemia with an hemoglobin level of 129 g/L. Other than atopic rhinitis, the patient had an uneventful medical history. He started xylometazoline nose drops and saline nasal irrigation 2 days before the hematology consultation in the context of the presumed viral upper respiratory tract infection. In addition, his medication comprised mometasone nasal spray for the atopic rhinitis. The patient had no oral medication, did not smoke, and consumed alcohol occasionally and only moderately. He is a student, living with his parents in Switzerland. Clinical and laboratory characteristics at the time of the hematology consultation are reported in Table 1. Notably, the patient had scleral icterus and moderate splenomegaly. The rest of the physical examination was normal. Laboratory analyses revealed mild macrocytic anemia with high reticulocyte count. Unconjugated bilirubin and lactate dehydrogenase (LDH) were elevated. Haptoglobin was undetectable. DAT test was negative. Blood smear examination revealed anisopoikilocytosis, polychromasia, bite cells, and basophilic stippling (Fig. 2A). However, no Heinz bodies were detected. Although basophilic stippling is not a feature of glucose-6-phosphate dehydrogenase deficiency (G6PD), this diagnostic possibility was investigated and excluded [4], leading us to suspect an unstable hemoglobinopathy. Hb analysis was initiated by cellulose acetate electrophoresis (Helena) and high-performance liquid chromatography (HPLC) (VARIANT II, Bio-Rad Laboratories, Hercules), and confirmed by automated capillary electrophoresis (CapillaryS2 Flex Piercing, Sebia). Sanger sequencing (Applied Biosystems ABI 3500, Thermo Fisher Scientific) was performed using exon-specific primers. HPLC and capillary electrophoresis showed slightly increased HbA2, normal fetal Hb (HbF), and a variant hemoglobin (Fig. 2B, C). DNA sequencing revealed a heterozygous mutation c430delC in the beta-globin gene hallmark of Hb Montreal II [5] and a heterozygous mutation c287C>T in the alpha-globin gene corresponding to Hb G-Georgia [6,7,8,9,10,11], indicative of the not yet described combination of double-heterozygous Hb Montreal II and Hb G-Georgia variants. Owing to the likelihood that drugs with oxidative effects may aggravate hemolysis in our patient, we recommended him to avoid drugs contraindicated in G6PD deficiency (www.g6pd.org).
Diagnostic process. A Blood smear of the index patient showing bite cells (black arrow head) and basophilic stippling (blank arrow head). B High-performance liquid chromatography (HPLC) of the index patient showing the values for HbA2, HbF, and variant hemoglobin (red arrow), with the same retention time as for HbA1c (0.693 minutes) in HPLC. C Capillary electrophoresis of the index patient showing two peaks for HbF and an abnormal peak for HbA (adult hemoglobin). These findings are consistent with a high suspicion of a variant hemoglobin
The patient had a control at the hematology outpatient clinic 3 weeks later showing a hemoglobin level of 135 g/L and a reticulocyte count of 662 G/L. LDH level was 1843 U/L, indicating the persistence of the hemolytic process. No further follow-up was performed in hematology. Six months ago, a cell blood count obtained at the occasion of a consultation at the allergology outpatient clinic showed a hemoglobin level of 140 g/L. We considered that this was probably the baseline hemoglobin level of our patient.
The grandfather (pedigree I.1, Fig. 1), of Italian origin, had anemia without more specification.
The mother (pedigree II.1, Fig. 1), 66 years old, carries heterozygous Montreal II. She has no anemia, but has signs of chronic hemolysis, had gallstones, and recently underwent cholecystectomy for cholecystitis.
The father (pedigree II.2, Fig. 1), 68 years old, carries heterozygous G-Georgia. His Hb level is normal, and he has no hemolysis.
The brother (pedigree III.2, Fig. 1), 33 years old, carries the combination of double-heterozygous Hb Montreal II and Hb G-Georgia variants. He suffers from moderate anemia and chronic hemolysis, and had splenectomy when he was 23 years old. During the same period, he received a kidney transplant for terminal renal failure because of a rapidly progressive glomerulonephritis.
The nephew (pedigree IV.1, Fig. 1), 3 years old, has mild anemia with basophilic stippling. No further investigation was undertaken.
There is no relevant additional family history to report.
Discussion and conclusion
Here we report a case of unstable hemoglobinopathy in a young adult with unexplained hemolytic anemia, which manifested first during a presumed viral infection, and show the largest pedigree reported to date of hemoglobinopathy Montreal II. Our case highlights the importance of considering unstable hemoglobinopathy as a differential diagnosis in any adult patient presenting with hemolysis. Notably, what distinguishes our case report from the initial case report of Montreal II hemoglobinopathy report [5] is the circumstance of the diagnosis of the index patient: a presumed viral upper respiratory tract infection that aggravated the hemolysis, drawing the attention of the otorhinolaryngologist consulted to the presumed upper respiratory tract infection and motivating the referral of the patient to hematology consultation. In addition, to our knowledge, the index patient and his brother are the first reported carriers of the combination of double-heterozygous Hb Montreal II and Hb G-Georgia variants.
The clinical presentation of unstable Hb depends on the causative mutation. Hemolysis may be chronic or acute, induced by oxidative stress. Chronic hemolysis may be mild to severe, and is usually recognized early in life [12]. Icterus, splenomegaly, and gallstones may belong to the clinical picture. Transfusion might be required during acute hemolytic episodes or chronically in patients with severe hemolysis. Splenectomy is indicated in patients with severe hemolysis and may improve anemia. However, there is a risk of vasculopathy and stroke in the post-splenectomy stage. Guidelines may help with splenectomy decision and choice of splenectomy type [12, 13]. If a hemolytic anemia workup is performed, characteristic findings include decreased Hb and elevated reticulocytes, unconjugated bilirubin and LDH, and undetectable haptoglobin. Facing a patient with DAT-negative hemolysis, the first suspicion of an unstable hemoglobinopathy arises from blood smear examination since it may reveal anisopoikilocytosis, bite and/or blister cells, polychromasia, and basophilic stippling. Heinz bodies may be detected by RBC supravital staining. However, absence of Heinz bodies does not exclude unstable hemoglobinopathy, particularly in nonsplenectomized patients [12]. Indeed, the spleen removes just the RBC membrane parts with Heinz bodies, leaving bite cells. Moreover, Heinz bodies are not specific to unstable hemoglobinopathies and may be observed in other conditions such as G6PD deficiency. Hb stability test may be used as a screening test [1]. In the second diagnostic step, Hb electrophoresis or HPLC may reveal increased HbA2, HbF, and peaks corresponding to abnormal Hb. However, hyperunstable variants may undergo rapid denaturation and degradation, so that the remaining Hb may appear normal. Therefore, normal Hb electrophoresis/HPLC results do not exclude unstable hemoglobinopathy [12, 14]. Finally, diagnostic steps comprise globin gene sequencing, which is the only technique to detect some rare unstable Hb variants [12]. A flowsheet describing the diagnosis process is shown in Fig. 3.
Diagnosis flowsheet. In the context of a direct antiglobulin test (DAT)-negative hemolysis, a blood smear needs to be performed. If Heinz bodies and/or bite cells are present, consider the following differential diagnoses: glucose-6-phosphate dehydrogenase (G6PD) deficiency, unstable hemoglobinopathies, or hemoglobin H disease. Then, perform G6PD enzyme testing. If normal, consider isopropanol heat stability testing. This test is optional; be aware that false positive may occur if hemoglobin F is high or in case of methemoglobinemia [1]. The next step would be hemoglobin electrophoresis/high-performance liquid chromatography (HPLC). Independently of the result, genetic testing is recommended. Indeed, hyperunstable variants may undergo rapid denaturation and degradation, so that the remaining Hb may appear normal. Therefore, normal Hb electrophoresis/HPLC result does not exclude unstable hemoglobinopathy, and genetic testing needs to be conducted [12, 13].
Hb Montreal II is a rare unstable beta Hb variant caused by a single nucleotide deletion that shifts the gene stop codon from codon 147 to codon 157. Presently, only the case of a Canadian patient with compensated chronic hemolysis without thalassemia features has been published (Table 1) [5]. Here, we report a family comprising three heterozygous carriers (pedigrees II.2, III.1, and III.2; Fig. 1) and two possible additional carriers (pedigrees I.1 and IV.1; Fig. 1). Hb Montreal II was here not associated with β-thalassemia syndrome, and carriers did not display ineffective erythropoiesis. Other than pedigree III.2 and the index case at presentation when he had a viral infection, carriers showed compensated chronic hemolysis. Therefore, in absence of additional erythropoietic challenges, heterozygous carriers can compensate for hemolysis by increasing erythropoiesis. The clinical picture of our patient was very similar to that of patients with Hb Tak, Trento, or Saverne [5]. However, Hb Florida, also similar to Hb Montreal II, has been associated with anemia and thalassemia [5].
Hb G-Georgia is an alpha hemoglobin variant caused by a nucleotide mutation (T) at codon 95, causing the substitution of the amino acid proline with a leucine. Heterozygosity may be associated with mild anemia and is asymptomatic [8]. Homozygous individuals display microcytic, hypochromic anemia with mild splenomegaly. Hb G-Georgia was reported in three African-American patients [6,7,8] and in a Turkish family [10], and has been described in combination with alpha thalassemia [15], HbS heterozygosity [11], and HbC heterozygosity [8].
There are many similarities between our patient and the first reported Montreal II case [5]. Both cases had good health condition and presented with splenomegaly. The Swiss patient was diagnosed shortly after an infection, which could explain the occurrence of severe hemolysis.
There was no clinical and laboratory difference between carriers of heterozygous Montreal II and those of compound heterozygous Montreal II and G-Georgia, confirming that heterozygosity for G-Georgia Hb does not cause relevant RBC changes.
We emphasize the importance of blood smear examination during the diagnosis process of DAT-negative hemolytic anemia. In this regard, awareness should be raised among hematologists caring for adult patients, stressing that inherited RBC disorders remain part of the differential diagnosis in adults and that a transitory acute condition may uncover an inherited RBC disorder. Finally, we want to stress that screening individuals with a family history of unstable Hb is recommended [16].
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- RBC:
-
Red blood cell
- DAT:
-
Direct anti-globulin
- LDH:
-
Lactate dehydrogenase
- G6PD:
-
Glucose-6-phosphate dehydrogenase deficiency
- HPLC:
-
High-performance liquid chromatography
- Hb:
-
Hemoglobin
References
Gallagher PG. Diagnosis and management of rare congenital nonimmune hemolytic disease. Hematol Am Soc Hematol Educ Program. 2015;2015:392–9.
Giardine B, Borg J, Viennas E, Pavlidis C, Moradkhani K, Joly P, et al. Updates of the HbVar database of human hemoglobin variants and thalassemia mutations. Nucleic Acids Res. 2014;42(1):D1063-9.
Matsumoto N, Ishihara T, Adachi H, Takahashi M, Miwa S. An ultrastructural study of the red pulp of the spleen and the liver in unstable hemoglobin hemolytic anemia. Virchows Arch A Pathol Anat Histol. 1977;374(4):339–51.
Cappellini MD, Fiorelli G. Glucose-6-phosphate dehydrogenase deficiency. Lancet. 2008;371(9606):64–74.
Chagnon P, Mollica L, Belisle C, Deveaux C, Angelo GD, Roy DC, et al. Hb Montreal II: a novel elongated beta-globin variant caused by a frameshift mutation [beta142 (-C)]. Hemoglobin. 2008;32(4):351–9.
Huisman TH, Adams HR, Wilson JB, Efremov GD, Reynolds CA, Wrightstone RN. Hemoglobin G Georgia or alpha 2–95 Leu (G-2) beta-2. Biochim Biophys Acta. 1970;200(3):578–80.
North ML, Garel MC, Thillet J, Oberling F, Lang JM, Mayer S, et al. A new case of hemoglobin G Georgia (author’s transl). Nouv Rev Fr Hematol. 1975;15(4):460–7.
Reynolds S, Miller C, King R, Lazarchick J. Hemoglobin C-G-Georgia double heterozygosity: a case report. Ann Clin Lab Sci. 1992;22(6):414–6.
Smith LL, Plese CF, Barton BP, Charache S, Wilson JB, Huisman TH. Subunit dissociation of the abnormal hemoglobins G Georgia (2 95Leu (G2) 2) and Rampa (2 95Ser (G2) 2). J Biol Chem. 1972;247(5):1433–9.
van Houte DP, van den Ende A, Statius van Eps LW, Giordano PC, Bernini LF. [Hemoglobin G Georgia in a Turkish family in the Netherlands]. Ned Tijdschr Geneeskd. 1986;130(8):360-3.
Wrightstone RN, Hubbard M, Huisman TH. Hemoglobin S-Ga Georgia disease: a case report. Acta Haematol. 1974;51(5):315–20.
Risinger M, Emberesh M, Kalfa TA. Rare hereditary hemolytic anemias: diagnostic approach and considerations in management. Hematol Oncol Clin North Am. 2019;33(3):373–92.
Iolascon A, Andolfo I, Barcellini W, Corcione F, Garcon L, De Franceschi L, et al. Recommendations regarding splenectomy in hereditary hemolytic anemias. Haematologica. 2017;102(8):1304–13.
Yates AM, Mortier NA, Hyde KS, Hankins JS, Ware RE. The diagnostic dilemma of congenital unstable hemoglobinopathies. Pediatr Blood Cancer. 2010;55(7):1393–5.
Srivorakun H, Singha K, Fucharoen G, Fucharoen S. Novel interactions of two alpha-Hb variants with SEA deletion alpha(0)-thalassemia: hematological and molecular analyses. Hematology. 2018;23(3):187–91.
Ryan K, Bain BJ, Worthington D, James J, Plews D, Mason A, et al. Significant haemoglobinopathies: guidelines for screening and diagnosis. Br J Haematol. 2010;149(1):35–49.
Acknowledgements
Not applicable.
Funding
The authors have no funding to declare.
Author information
Authors and Affiliations
Contributions
CM and AAS collected the data and wrote the manuscript. AH and AM performed the hemoglobin analyses. CM, AR, and AAS prepared the figures. AR, AH, and AM reviewed and approved the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
This study was conducted in accordance with the fundamental principles of the Declaration of Helsinki.
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Medri, C., Méndez, A., Hammerer-Lercher, A. et al. Unstable hemoglobin Montreal II uncovered in an adult with unexplained hemolysis exacerbated by a presumed viral infection: a case report. J Med Case Reports 16, 145 (2022). https://doi.org/10.1186/s13256-022-03374-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-022-03374-y