Abstract
Background
Paragangliomas are rare vascular neuroendocrine tumors that develop in the extra-adrenal paraganglion tissue. They occur most commonly at the carotid bifurcation, where they are known as carotid body tumors. Most paragangliomas are benign, locally aggressive, infiltrative tumors. Approximately 10% of patients with paragangliomas develop distant metastases, 10% present with multiple or bilateral tumors (mostly carotid body tumors), and 10% have a family history of paragangliomas. The malignant transformation of carotid body tumors has been reported in 6% of cases.
Case presentation
We present the case of a 64 year-old Caucasian woman with a gigantic glomic tumor mass in the neck. Twenty years before the consultation, the patient had undergone an unsuccessful attempt to remove the mass. Over the last 3 years, the patient had felt enlargement of the mass at an increased rate, almost doubling the prior size. Angio magnetic resonance imaging showed a 9 cm paratracheal mass on the left cervical side that laterally displaced the sternocleidomastoid muscle and 2 c m of the trachea. Due to the change in the tumor behavior, the maxillofacial team at Ruber International Hospital decided to remove the tumor surgically after embolization. During the surgery the tumor was gently dissected from the carotid an removed from the carotid bifurcation uneventfully. Two small nodes adhering tightly to the internal carotid adventitia and the posterior torn hole were left in place to avoid any potentially life-threatening complications. The final biopsy confirmed the initial diagnosis of carotid body paraganglioma and showed a Ki-67 expression of 19%. Due to the aggressive growth behavior and high Ki-67 expression of the tumor, the patient was referred to the CyberKnife Unit of Ruber International Hospital for treatment of the remaining nodes.
Conclusions
The management of cervical paragangliomas is difficult and remains a challenge. Although the likelihood of tumor control is high with surgical or radiotherapeutic treatments, we currently lack consensus regarding the best treatment option. Nevertheless, in selected complex cases, such as the case we present, the combination of surgery and radiosurgery may allow complete local tumor control with minimal morbidity.
Similar content being viewed by others
Background
Paragangliomas are rare vascular neuroendocrine tumors that develop in the extra-adrenal paraganglion tissue. They represent less than 0.5% of all head and neck tumors. In the head and neck, paragangliomas are named after their site of origin. They occur most commonly at the carotid bifurcation, where they are known as carotid body tumors. Additional sites of origin include the jugular bulb (jugular paraganglioma), the vagus nerve (vagal paraganglioma), and within the middle ear mucosa (tympanic paraganglioma) [1].
These tumors grow slowly, and they are reported to have a median doubling time of 4.2 years. Without therapy, they may grow to a considerable size and become life threatening.
Most paragangliomas are benign, locally aggressive, infiltrative tumors. Approximately 10% of patients with paragangliomas develop distant metastases, 10% present with multiple or bilateral tumors (mostly carotid body tumors), and 10% have a family history of paragangliomas. The malignant transformation of carotid body tumors has been reported in 6% of cases [1,2,3,4,5,6].
The clinical signs and symptoms of benign and malignant paragangliomas overlap significantly. Most lesions produce local compressive symptoms including hearing loss, otalgia, tinnitus, neck mass, or cranial neuropathy. Cranial neuropathy can lead to dysphagia, facial weakness, and vocal fold paresis. A small proportion of head and neck paragangliomas may also show biochemical activity similar to that of pheochromocytomas, possibly inducing symptoms of diarrhea, hypertension, and flushing [4].
The diagnosis of paragangliomas is generally based on radiological appearance because biopsy is challenging due to the anatomical location and vascularity. The literature contains little information about the specific clinical behavior of malignant paragangliomas that would help to distinguish them from benign lesions prior to therapy. Furthermore, the diagnosis of malignant paraganglioma is problematic and often relies on final pathological results [7,8,9,10].
Several of these tumors are inherited through mutations of the genes that encode for the succinate dehydrogenase enzymes SDHD and SDHB. Although the inheritance of both genes is autosomal dominant, the SDHD gene is subject to maternal imprinting, and the SDHB gene has incomplete penetrance. Patients with the inherited gene almost invariably have multiple tumors [11, 12].
Three treatment options are currently recognized: surgical resection, radiation therapy, and a wait-and-scan policy. Of these, surgery is the only curative treatment. However, because surgery may be complicated by significant morbidity, especially in larger tumors, it is considered by some authors to be controversial.
Here, we present the case of a giant paraganglioma body tumor treated with a combined surgical and radiotherapeutic (CyberKnife) protocol. This case report review has been approved by the Ethics Committee at the Ruber International Hospital.
Case presentation
A 64-year-old Caucasian woman was referred to our office for the assessment of a gigantic left neck mass (Fig. 1). The patient reported that she had started to feel a paratracheal node 34 years previously, and that it had grown progressively during the subsequent three decades. She had undergone an operation in the area 24 years previously, although the surgery had to be terminated due to massive bleeding from the mass. During surgery, the mass was diagnosed as most likely a glomus tumor. No further surgeries to remove the mass were attempted, and it had been allowed to grow steadily.
In May 2013, the patient was referred elsewhere for further study of the mass. Magnetic resonance imaging (MRI) revealed a hypervascularized mass with a maximum diameter of 4 cm located at the bifurcation of the left carotid artery and causing the forward displacement of the external carotid artery and the backward displacement of the internal carotid artery. The patient refused surgery at that time and remained asymptomatic for almost 3 years. She then decided to consult a physician again due to the enlargement of the mass, which caused discomfort and mild compression symptoms when swallowing.
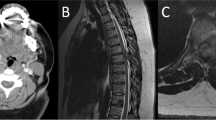
In 2016, angio MRI (Fig. 2) showed a 9 cm paratracheal mass on the left cervical side that laterally displaced the sternocleidomastoid muscle and 2 cm of the trachea. The mass was pulsatile and slightly painful. No Horner syndrome or Hering–Breuer reflex was noted. A carotid occlusion test and a complete angiography were also performed, and these confirmed the permeability of the Willis polygon and the diagnosis of the mass.
Due to the change in the behavior of the tumor, which had doubled in size within 3 years after remaining relatively stable for almost three decades, the size of the tumor, which had started causing compression symptoms, and the Shamblin grade II classification, the maxillofacial team at Ruber International Hospital decided to remove the tumor surgically after embolization.
The surgery was performed in February 2016. The tumor was approached through a wide cervical exposure after identifying the primitive carotid artery (Fig. 3).
The tumor was gently dissected from the carotid bifurcation in a subadventitial plane (Fig. 4), with great emphasis placed on maintaining hemostasis.
The surgeons would like to note that a partially blunt Freer periostotome is the best tool to use in high-risk areas. The vagal nerve was readily identified and separated from the mass. The hypoglossal nerve and major neck vessels were also preserved (Fig. 5A, B). The mass was then removed from the bifurcation uneventfully. Two small nodes adhering tightly to the internal carotid adventitia and the posterior torn hole were left in place to avoid any potentially life-threatening complication.
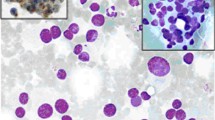
The postoperative phase was uneventful, and the patient was discharged 6 days after the surgery with moderate hoarseness, which was resolved within 1 month. The final biopsy confirmed the initial diagnosis of carotid body paraganglioma and showed a Ki-67 expression of 19%.
Due to the aggressive growth behavior and high Ki-67 expression of the tumor, the patient was referred to the CyberKnife Unit of Ruber International Hospital for treatment of the remaining nodes. A thermoplastic mask was made to ensure that the patient remained immobilized during the treatment. A T2 MRI and computed tomography (CT) with intravenous contrast were performed to locate the above-mentioned remaining nodes of the paraganglioma. The treatment was performed separately in each affected area on two consecutive days. A coverage dose of 14 Gy and an isodose of 83% were administered using 5- and 7.5-mm collimators. The maximum dose used was 16.87 Gy. The medullary canal received a dose of less than 4 Gy, and the left VII and VIII nerves received a dose of less than 5 Gy (Fig. 6). The treatment course was uneventful, and no complication occurred during or after treatment.
After a 48-month follow-up period, no lesion recurrence or surgery-related complications have occurred. Some minor scar revision due to the tracheostomy was performed under local anesthesia. The patient is otherwise completely symptom free (Fig. 7).
Discussion and conclusions
The carotid body tumor is the most common type of paraganglioma in the head and neck, and is the only pathology to affect the carotid body [1,2,3]. Carotid body tumors may be sporadic or familial; the sporadic form is slightly more common in women [3, 10, 11]. These tumors often present as slow-growing, non-tender neck masses located just anterior to the sternocleidomastoid muscle at the level of the thyroid [4].
The differential diagnosis includes cervical lymphadenopathy, carotid artery aneurysm, brachial cleft cyst, laryngeal carcinoma, and metastatic tumor. Carotid body tumors are typically mobile in the lateral plane but have restricted mobility in the cephalocaudal direction (Fontaine sign). Occasionally, such tumors may transmit the carotid pulse or demonstrate a bruit or thrill. Due to the close proximity to the carotid vessels and cranial nerves X–XII, tumor enlargement may cause progressive neurological symptoms, such as dysphagia, odynophagia, or hoarseness [4,5,6].
Histologically, carotid body tumors resemble the normal architecture of the carotid body. The tumors are highly vascular and contain clusters of tumor cells between the capillaries, producing the pseudoalveolar pattern of Zellballen (cell balls) [1, 2, 7, 8]. These cells have fine-grained eosinophilic cytoplasm and small round or oval nuclei. The malignant potential of these tumors cannot be predicted by histological studies. The diagnosis of malignancy is based on the invasion of lymph nodes, vessels, nerves, the airway, or the base of the skull, rather than on tumor size or histological features [9]. Chapman et al. [4] recently suggested that pain, a rapidly enlarging neck mass, and younger age are predictive factors of underlying malignancy, which should prompt the consideration of an aggressive diagnostic and management approach.
Contrast CT and MRI [9] have evolved as effective noninvasive imaging modalities for the detection of carotid body tumors. They commonly demonstrate tumor blood supply and the widening of the carotid bifurcation by a well-defined tumor blush (Lyre sign), which is a classic pathognomonic contrast angiographic finding. Carotid angiography also plays an important role in the evaluation and management of these tumors. Angiography demonstrates the vascular extent of the tumor, carotid artery involvement, the size and location of tumor-feeding vessels (useful for evaluating the possibility of tumor embolization), and coexisting atherosclerotic disease of the carotid arteries.
The management of carotid body tumors has been controversial because of their low malignant potential and high rates of operative complications. Early experiences with carotid body tumor resections were associated with operative mortality rates ranging from 5% to 13%, postoperative cranial nerve palsy in 32–44% of patients, and other postoperative neurological complications in 8–20% of patients. However, most recent experiences have demonstrated the safety of the surgical approach, with mortality rates of 1–2% but a high (40%) morbidity rate due to cranial nerve injury and cerebral ischemic events [12]. Surgical treatment has been the standard approach to symptomatic carotid body tumors for many years and has shown high cure rates [12].
The size of a carotid body tumor is a very important consideration in the development of a treatment strategy. As in the case reported here, tumors larger than 4–5 cm tend to show partial or complete encirclement of the carotid arteries. Larger tumors have been associated with higher risks of bleeding and cranial nerve injury during surgery. Preoperative tumor embolization has been employed to reduce tumor size and thereby decrease the risk of complications. The Shamblin classification system (Table 1), which is based on tumor size, was proposed in 1971. According to this classification, group I tumors are relatively small and minimally attached to carotid vessels; the surgical excision of these tumors is not difficult. Group II tumors, including the case reported here, are large and show moderate attachment to the carotid vessels; these tumors are amenable to careful surgical excision. Group III tumors are very large and encase the carotid vessels; these tumors often require arterial resection and grafting [13].
As previously described, a thorough subadventitial dissection with proximal control of the primitive carotid artery and the early identification and dissection of the cranial nerves (mainly the vagal and hypoglossal nerves) help to prevent much of the morbidity related to the surgical excision.
Recent studies have reported on the use of radiotherapy as the first-choice treatment for paragangliomas [14]. The main arguments in favor of this treatment are that it is less invasive than surgery, has fewer complications, and achieves high rates of local control. Hinerman and colleagues [14] reported a 96–100% tumor control rate in cervical paragangliomas after radiation therapy using a dose of 45 Gy. However, the cure criterion for radiotherapy, which is growth cessation rather than disappearance, is difficult to evaluate [15]. Thus, in gigantic tumors such as the one presented here, radiotherapy may stop growth but will not reduce the tumor mass. In such cases, compression symptoms may not worsen but will not disappear.
Further complications of radiation therapy may include inflammation of the external auditory canal and middle ear, osteoradionecrosis, cranial nerve neuropathies, and direct injury to brain tissue. Furthermore, it must be remembered that surgery will be more difficult if radiation therapy fails [12].
Histological examination has shown that the chief cells are minimally affected by radiation; rather, the distinctive vascular structure of the tumor is replaced by fibrous connective tissue [15, 16]. This development is of concern in potentially malignant tumors, which have been reported in 3–5% of cases. In our case, we used the predictive factors of Chapman et al. [4] to consider the possibility of malignant transformation of the chemodectoma. Given the wide experience of the surgical team with this type of tumor, surgical excision was selected as the primary treatment option.
Radiosurgery has arisen as a promising approach to the management of paragangliomas, especially glomus jugular tumors. Radiosurgery provides a high degree of accuracy, exquisite precision, and rapid radiation-dose falloff at the peripheries of the target lesions, allowing the clinician to deliver a high radiation dose to neoplastic tissue while sparing healthy brain tissue. This treatment is also relatively noninvasive and can be performed as an outpatient procedure [17,18,19,20,21].
In the case reported here, a preoperative goal of zero morbidity was defined according to the patient’s desires. Therefore, although the tumor resection was practically completed, we did not attempt to remove the nodes adhering most strongly to the skull base and internal carotid artery to avoid taking any further risks. Thus, gamma-knife radiosurgery was crucial to ensure effective local disease control with minimal morbidity.
In summary, the management of cervical paragangliomas is difficult and remains a challenge. Treatment must be individualized, taking into account the patient’s age, tumor site and size, multicentricity, and preexisting cranial nerve deficits. Although the likelihood of tumor control is high with surgical or radiotherapeutic treatments, we currently lack consensus regarding the best treatment option. Nevertheless, in selected complex cases, the combination of surgery and radiosurgery may allow complete local tumor control with minimal morbidity.
References
Hoang VT, Trinh CT, Lai TAK, Doan DT, Tran TT. Carotid body tumor: a case report and literature review. J Radiol Case repo. 2019;31(8):19–30. https://doi.org/10.3941/jrcr.v13i8.3681.
Sevilla GMA, Llorente PJL, Rodrigo TJP, Garcia RG, Suarez FV, Coca PA, et al. Head and neck paragangliomas: revision of 89 cases in 73 patients. Acta Otorrinolaringol Esp. 2007;58(3):94–100.
Dixon JL, Atkins MD, Bohannon WT, Buckley CJ, Lairmore TC. Surgical management of carotid body tumors: a 15-year single institution experience employing an interdisciplinary approach. Proc (Baylor Univ Med Cent). 2016;29(1):16–20.
Chapman DB, Lippert D, Geer C, Edwards HD, Russell G, Rees CJ. Clinical, histopathologic and radiographic indicators of malignancy in head an neck paragangliomas. Otol Head Neck Surg. 2010;143:531–7. https://doi.org/10.1016/j.otohns.2010.05.031.
Lee JH, Barich F, Karnell LH. National Cancer Data Base report on malignant paragangliomas of the head and neck. Cancer. 2002;294:730–7. https://doi.org/10.1002/cncr.10252.
Barnes L, Everson JW, Reichart P, et al editors. World health organization classification of tumours. Pathology and genetics of head and neck tumours. Lyon: IARC Press; 2005.
Krijger R, van Nederveen FH, Korpershoek E. New developments in the detection of the clinical behavior of pheochromocytomas and paragangliomas. Endocr Pathol. 2006;17:137–41. https://doi.org/10.1385/ep:17:2:137.
Barnes L, Taylor S. Carotid body paragangliomas, a clinicopathologic and DNA analysis of 13 tumors. Arch Otolaryngol Head Neck Surg Arch Otolaryngol Head Neck Surg. 1990;116:447–53. https://doi.org/10.1001/archotol.1990.01870040069016.
Som PS, Curtin HD. Parapharyngeal and masticator space lesions. In: Som PS, Guss Curtin HD, editors. Head and neck imaging. 4th ed. St. Louis: Mosby; 2004. p. 1969–78.
Baysa BE, Willett-Brozick JE, Lawrence EC, Drovldlic CM, Savul SA, McLeod DR, Yee HA, Brackmann DE, Slattery WH, Myers EN, Ferrerl RE, Rubistein WS. Prevalence of SDHB, SDHC, and SDHD germline mutations in clinic patients with head and neck paragangliomas. J Med Genet. 2002;39:178–83. https://doi.org/10.1136/jmg.39.3.178.
Schiavi F, Boedeker CC, Bausch B. Predictors and prevalence of paraganglioma syndrome associated with mutations of the SDHC gene. JAMA. 2005;294(16):2057–63. https://doi.org/10.1001/jama.294.16.2057.
Chretien PB, Engelman K, Hoye RC, Geelhoed GW. Surgical management of intravascular glomus jugulare tumor. Am J Surg. 1971;122:740–3. https://doi.org/10.1016/0002-9610(71)90437-5.
Shamblin WR, RemiNe WH, Sheps SG. Carotid body tumor (chemodectoma). Clinicopathologic analysis of ninety cases. Am J Surg. 1971;122:732–9. https://doi.org/10.1016/0002-9610(71)90436-3.
Hinerman RW, Amdur RJ, Morris CG, Kirwan J, Mendenhall WM. Definitive radiotherapy in the management of paragangliomas arising in the head and neck: a 35-year experience. Head Neck. 2008;30:1431.
Miller JP, Semaan M, Einstein D, Einstein D, Megerian CA, Maciunas RJ. Staged gamma knife radiosurgery after tailored surgical resection: a novel treatment paradigm for glomus jugulare tumors. Stereotact Funct Neurosurg. 2009;87:31–6. https://doi.org/10.1159/000195717.
Varma A, Nathoo N, Neyman G, Suh JH, Ross J, Park J, Barnett G. Gamma knife radiosurgery for glomus jugulare tumors: volumetric analysis in 17 patients. Neurosurgery. 2006;59:1030–6. https://doi.org/10.1227/01.NEU.0000245596.46581.B2.
Lighttowlers S, Benedict S, Jefferies SJ, Jena R, Harris F, Burton KE, et al. Excellent local control of paraganglioma in the head and neck with fractionated radiotherapy. Clin Oncol (R Coll Radiol). 2010;22:382–9.
Austin-Seymour M. Skull base tumours: chemodectomas—nonchromaffin paragangliomas. In: Leibel S, Phillips T, editors. Textbook of radiation oncology. Philadelphia: W.B. Saunders; 1998. p. 341–6.
Powell S, Peters N, Harmer C. Chemodectoma of the head and neck: results of treatment in 84 patients. Int J Radiat Oncol Biol Phys. 1992;22:919–24. https://doi.org/10.1016/0360-3016(92)90788-j.
Havekes B, van der Klaauw AA, Hoftijzer HC. Reduced quality of life in patients with head-and-neck paragangliomas. Eur J Endocrinol. 2008;158:247–53. https://doi.org/10.1530/EJE-07-0464.
Jansen JC, van den Berg R, Kuiper A, van der Mey AG, Zwinderman AH, Cornelisse CJ. Estimation of growth rate in patients with head and neck paragangliomas influences the treatment proposal. Cancer. 2000;88(12):2811–6.
Guss ZD, Batra S, Limb CJ, Li G, Sughrue ME, Redmond K, Rigamonti D, Parsa AT, Chang S, Kleinberg L, Lim M. Radiosurgery of glomus jugulare tumors: a meta-analysis. Int J Radiat Oncol Biol Phys. 2011;2011(15):497–502.
Acknowledgements
To the Craniofacial and Maxillofacial Unit, Ruber International Hospital, Madrid (Spain) for their support.
Funding
No funding was granted from this study. The authors declare no conflict of interest.
Availability of data and materials
The datasets used and/or analyzed during the current study belong to the Craniofacial and Maxillofacial Surgery Unit, Ruber International Hospital (Madrid, Spain). They are available from the corresponding author on reasonable request.
Author information
Authors and Affiliations
Contributions
Conceptualization and methodology, CC; investigation, JMLA; resources, RM; data writing—original draft preparation, JMLA/FM—review and editing, BRS; supervision, JMA. All authors have read and agreed to the published version of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The retrospective chart review study was approved by the Ethics Committee of the Ruber International Hospital (Madrid, Spain) in 2020.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
This research received no external funding. The authors declare that they have no competing interests
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
López-Arcas, J.M., Colmenero, C.M., Martínez, R. et al. Giant carotid chemodectoma treated with a combination of surgery and CyberKnife radiotherapy: a case report and review of the literature. J Med Case Reports 16, 92 (2022). https://doi.org/10.1186/s13256-021-03237-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-021-03237-y