Abstract
Background
Accessory mitral valve tissue is a rare congenital anomaly that is commonly diagnosed in early childhood and rarely in adulthood. It is usually asymptomatic. However, it may cause left ventricular outflow tract obstruction in a way that mimics various other causes of obstruction.
Case summary
A 72-year-old Caucasian man complained of chest discomfort and exertional dyspnea for 3 months. There were no specific findings from a physical examination except systolic murmur. Transthoracic echocardiography demonstrated a mass on the mitral valve extending to the intraventricular septal, raising the pressure gradient flow across the aortic valve. Transesophageal echocardiography showed parachute-like tissue connected to the anterior leaflet of the mitral valve causing left ventricular outflow tract obstruction. During the surgery preparation period, he underwent coronary angiography and computed tomography to study the anatomy surrounding the mass. After surgery, biopsy showed non-specific findings.
Conclusion
When facing a case of aortic valve stenosis, accessory mitral valve tissue should be kept in mind as one of the possible underlying causes despite its rarity. Although it is simple and noninvasive, echocardiography remains the best diagnostic procedure to make the correct decision about management and to define the golden time for surgical intervention.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Background
Accessory mitral valve tissue (AMVT) is a rare congenital cardiac malformation that sometimes causes left ventricular outflow tract (LVOT) obstruction and is commonly associated with other congenital cardiac anomalies [1]. It is usually present in childhood causing LVOT obstruction. Such an obstruction leads to chest pain, effort syncope, or recurrent transient ischemic attack/stroke. The number of adults affected by such a disease is one per 26,000 echocardiograms [2].
The first case of this rare condition was described in the literature in 1842 [3], whereas the first surgical treatment was described in 1963 [4]. The majority of patients who were reported to have varying degrees of LVOT obstruction were diagnosed with AMTV during the first 10 years of their life. However, LVOT was rarely detected in adulthood [5].
Here is a case report of an adult patient with AMVT, whose disease developed a severe obstruction of LVOT.
Case presentation
A 72-year-old Caucasian man, suffering chest pain, visited our emergency department after being diagnosed as having dyspnea. The dyspnea started 3 months ago and deteriorated the week before visiting our emergency department. His dyspnea occurred with moderate exertion without any associated symptoms. His chest pain was atypical with some parietal characteristics. He was a heavy tobacco smoker with no medical history and with no chronic medications prescribed. However, hypertension seemed to have run in his family.
A physical examination revealed severe systolic murmur in the aortic area radiating toward the left parasternal space, becoming fainter at the apex. Blood pressure was symmetric, measuring 155/75 mmHg, pulse rate was 95 beats per minute (bpm). Lungs were clear on auscultation without crackles or abnormal sounds. A chest X-ray showed normal cardiac silhouette and aortic arch, and both lungs were clear and expanded with no infiltrates or pleural effusions. An electrocardiogram showed non-specific changes with T wave inversion on lateral leads and horizontal ST segment depression on V4–6.
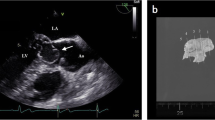
He was admitted to the coronary care unit to follow up on the process of examining his body functions. Transthoracic echocardiography (TTE) revealed an oval-like tissue with clean margins attached to the proximal portion of the anterior leaflet of the mitral valve causing LVOT occlusion during systole. The gradient pressure through LVOT measured 55 mmHg, without organic lesion in the aortic cusps. The left ventricle wall motion was normal. Dimensions at systolic and diastolic phases were normal. Pulmonary pressure was 18 mmHg. No other cardiac anomalies were present (Fig. 1b, c, Additional file 1: Video S1).
a Transesophageal echocardiography demonstrated tissue dimensions and location. b Transthoracic echocardiography pressure peak gradient measured by continuous wave Doppler across left ventricular outflow tract. c Transthoracic echocardiography apical four-chamber view showed the relation between the accessory mitral valve tissue and the anterior leaflet of the mitral valve
To obtain more detailed information, transesophageal echocardiography (TEE) was performed. This revealed a parachute-like structure (measuring 13 × 14 mm) attached to the proximal portion of the anterior leaflet of the mitral valve causing LVOT obstruction (Fig. 1a, Additional file 2: Video S2).
Metoprolol tartrate 50 mg twice daily was prescribed for our patient until the scheduled surgery. During hospitalization, multi-slice computed tomography (MS-CT) scan was performed. It emphasized the presence of the abnormal mass and its dimensions and location (Fig. 2).
He underwent coronary catheterization before the surgery. The angiography showed ostial lesion and severe stenosis in the mid left anterior descending (LAD) in addition to 80% stenosis in circumflex (CX), and the right coronary artery (RCA) had multi-sequential lesions beginning from the first segment (Fig. 3).
The surgery was delayed for a month due to a huge workload in the surgical department at that time. Since the case was rare and not fully understood by surgeons, it was classified as “cold case” in comparison to other on-list cases. Later on, our patient underwent coronary artery bypass graft (CABG) surgery and the abnormal tissue was surgically removed. The biopsy was sent to the pathology laboratory for further investigation (Fig. 4). The pathology report indicated a pure fibrous tissue with non-differentiated cells. Two weeks later, another TEE was done to assess the flow across the LVOT and the pressure gradient (PG) was normal. No residue of the abnormal tissue was seen. A timeline is shown in Table 1.
Discussion
AMVT in adults is very rare and can mimic various causes of LVOT obstruction. While most cases are diagnosed in childhood, rarely do these cases happen in adulthood. Less than 30% of these anomalies occur in adults, two thirds of the patients were associated with other cardiac anomalies, and symptoms of LVOT obstruction developed early in the neonatal or childhood periods [1]. Although the underlying cause is still uncertain, it is suggested that AMVT results from an incomplete separation of the mitral valve from the endocardial cushion during cardiac development during embryogenesis [6]. Patients with AMVT anomaly may be asymptomatic but more frequently experience palpitations and fatigue [7].
Patients with AMVT become symptomatic when the mean gradient across the LVOT is more than 50 mmHg [2]. Severe obstruction is defined when LVOT gradient is over 50 mmHg, while the obstruction is defined as mild when the gradient is less than 31 mmHg [1]. AMVT has been variably described as sail-shaped, sac-like, balloon-like, parachute-like, and leaflet-like, or as a sheet, membrane, or pedunculated mass [8].
Despite the rarity of AMVT in adults, it should be kept in mind as part of the differential diagnosis of LVOT obstruction. Other LVOT masses that might cause obstruction include: myxoma, papillary fibroelastoma, and thrombus or vegetations, which can produce similar echocardiographic appearances. However, a detailed TTE and TEE can be used to differentiate them from AMVT [9]. Both TTE and TEE may help in the diagnosis, revealing possible associated lesions and complications [10]. Regarding treatment of this anomaly, cardiac surgery is indicated only in patients with significant LVOT gradients and those undergoing correction of other congenital cardiac defects in childhood or acquired disease if an adult. Surgery includes accessory tissue removal and, sometimes, artificial chordae implantation and annuloplasty, depending on the severity of the disease [11,12,13].
Conclusion
Echocardiography is considered to be the cornerstone investigation tool when assessing an aortic valve stenosis regardless of the cause. Significant LVOT obstruction happens when the PG exceeds 50 mmHg through LVOT flow and surgery is the only treatment in this severe status. However, conservative therapy is indicated for PG less than 50 mmHg except when the lesion is associated with other congenital defects. Finally, when facing such a case in the future, it is recommended to make a more rapid surgical response.
Abbreviations
- AMVT:
-
Accessory mitral valve tissue
- bpm:
-
Beats per minute
- CABG:
-
Coronary artery bypass graft
- CX:
-
Circumflex
- LAD:
-
Left anterior descending
- LVOT:
-
Left ventricular outflow tract
- MS-CT:
-
Multi-slice computed tomography
- PG:
-
Pressure gradient
- RCA:
-
Right coronary artery
- TEE:
-
Transesophageal echocardiography
- TTE:
-
Transthoracic echocardiography
References
Prifti E, Bonacchi M, Bartolozzi F, Frati G, Leacche M, Vanini V. Postoperative outcome in patients with accessory mitral valve tissue. Med Sci Monit. 2003;9:126–33.
Rovner A, Thanigaraj S, Perez JE. Accessory mitral valve in an adult population: the role of echocardiography in diagnosis and management. J Am Soc Echocardiography. 2005;18:494–8.
Chevers N. Observations on diseases of the orifice and valves of the aorta. Guy’s Hospital Reports. 1842;7:387–452.
MacLean LD. Subaortic stenosis due to accessory tissue on the mitral valve. J Thorac Cardiovasc Surg. 1963;45:382–7.
Yuan S, Shinfeld A, Mishaly D, Haizler R, Ghosh P, Raanani. E. Accessory mitral valve tissue: a case report and an updated review of literature. J Card Surg. 2008;(23):769–72.
Uslu N, Gorgulu S, Yildirim A, Eren M. Accessory mitral valve tissue: report of two asymptomatic cases. Cardiology. 2006;(105):155–7.
Prifti E, Frati G, Bonacchi M, Vanini V, Chauvaud S. Accessory mitral valve tissue causing left ventricular outflow tract obstruction: case reports and literature review. J Heart Valve Dis. 2001;10:774–8.
Rozo JC, Medina D, Guerrero C, Calderon AM, Mesa A. Accessory mitral valve without left ventricular outflow tract obstruction in an adult. Tex Heart Inst J. 2008;35:324–6.
W W LX, Wang L, Sun X, Jiang Y, Huo S, et al. The accuracy of echocardiography versus surgical and pathological classification of patients with ruptured mitral chordae tendinae: a large study in a Chinese cardiovascular center. Cardiothorac Surg. 2011;6:94.
Sharma R, Smith J, Elliott PM, Mckenna WJ, Pellerin D. Left ventricular outflow tract obstruction caused by accessory mitral valve tissue. J Am Soc Echocardiography. 2006;19:354.
Panduranga P, Eapen T, Al-Maskari S, Al-Farqani A. Accessory mitral valve tissue causing severe left ventricular outflow tract obstruction in a post-Senning patient with transposition of the great arteries. Heart Int. 2011;6:6.
D'Aloia A, Vizzardi E, Chiari E, Fracassi F, Zanini G, Faggiano P, et al. Dynamic mild subaortic left ventricular obstruction caused by an accessory mitral valve attached to the anterior mitral valve in a young pregnant woman. Eur J Echocardiography. 2008;9:160–1.
Manganaro R, Zito C, Khandheria BK, Cusmà-Piccione M, Todaro MC, Oreto G, et al. Accessory mitral valve tissue: an updated review of the literature. EHJ Cardiovascular Imaging. 2014;15:489–97.
Acknowledgements
The authors are grateful to Dr Antoine Nasimian, MD (Radiologist of Aleppo University Hospital, Aleppo, Syria) for his assistance to our study.
Funding
N/A.
Availability of data and materials
All data generated or analyzed during this study are included in this published article and its supplementary information files.
Author information
Authors and Affiliations
Contributions
MM was responsible for critical revision of the manuscript for content and supervision. AS was responsible for conception, design, acquisition, and interpretation of data. HA was responsible for surgical treatment. AB was responsible for doing echocardiography and follow up. All authors reviewed and contributed to the final version of this case report. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
No ethical approval was required in our institution for a case report involving a single patient.
Consent for publication
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The authors declare that they have no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Additional files
Additional file 1:
Video S1. Transthoracic echocardiography demonstrated left ventricle output obstruction caused by a mobile mass. (MP4 421 kb)
Additional file 2:
Video S2. Transesophageal echocardiography showed the anatomical relation of the accessory tissue and the anterior leaflet of the mitral valve. (MP4 3570 kb)
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Mardenli, M., Samman, A., Alkanj, H. et al. Obstructive accessory mitral valve tissue in an adult patient: a case report. J Med Case Reports 13, 184 (2019). https://doi.org/10.1186/s13256-019-2110-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-019-2110-z