Abstract
Background
Cutaneous tuberculosis represents only 1–2% of extrapulmonary forms of tuberculosis. Scrofuloderma is an endogenous form of cutaneous tuberculosis and can present as isolated or coexist with pulmonary and disseminated forms of tuberculosis. Pathologically confirmed scrofuloderma coexisting with disseminated tuberculosis with a good treatment response is presented and discussed.
Case presentation
A 12-year-old African Ethiopian girl presented with bilateral neck swelling with purulent discharge and skin ulceration of 3 months’ duration. Dry cough, low-grade fever, decreased appetite, drenching night sweats, global throbbing headache, and a significant amount of weight loss were also reported. Biopsy of the skin identified scrofuloderma, and Mycobacterium tuberculosis was also identified by Xpert MTB/RIF assay. Cerebrospinal fluid analysis and brain computed tomographic scans showed tuberculous meningitis and tuberculoma. Antituberculosis therapy with rifampicin, isoniazid, pyrazinamide, and ethambutol; prednisolone; pyridoxine; and wound care were provided. The patient was discharged for outpatient directly observed antituberculosis therapy in a nearby health center after acute complications were treated and once the skin lesion had started to dry or heal.
Conclusions
Cutaneous tuberculosis should be considered in a child presenting with a skin lesion or discharge. Cutaneous tuberculosis cases should be investigated for coexisting pulmonary and extrapulmonary forms of tuberculosis. Histopathologic diagnosis should be considered to rule out other skin pathologies and also to prevent delay in treatment. Better tuberculosis prevention strategies, including vaccination scale-up, are warranted.
Similar content being viewed by others
Introduction
Tuberculosis (TB) has remained a global public health problem and has diverse pulmonary and extrapulmonary presentations [1]. Cutaneous tuberculosis (CTB) represents only 1–2% of extrapulmonary forms of TB [2]. CTB is classified into several variants, and scrofuloderma is a form of endogenous CTB [2, 3]. Scrofula, tuberculous lymphadenitis of the neck, is named for the likeness of the cluster of nodes to piglets feeding from a sow [4].
Scrofuloderma affects people of all ages. However, children, teenagers, and elders are highly affected, owing to immunologic failure to contain mycobacterial infection [5]. Scrofuloderma can present in an isolated form or coexist with pulmonary and disseminated forms of TB [2]. It presents as erythematous nodules that fistulize and discharge caseous and purulent material [6]. Pathologic examinations reveal abscesses, necrosis, and tuberculoid granulomas [7, 8]. In this report, pathologically confirmed scrofuloderma coexisting with disseminated TB in an unvaccinated teenager with good clinical response is presented and discussed. CTB is a rarely reported form of TB, and this case report highlights the need for CTB consideration and a confirmatory pathologic test in childhood skin lesions. This case emphasizes the need for workup to detect coexisting extrapulmonary TB.
Case presentation
A 12-year-old African Ethiopian girl presented with bilateral neck swelling with purulent discharge and skin ulceration of 3 months’ duration. She had dry cough, low-grade fever, decreased appetite, and drenching night sweats, and she had lost a significant amount of weight. She had a global throbbing type of headache with occasional projectile vomiting of ingested matter starting 6 days before her visit. She had never been vaccinated and had no known contact with any person diagnosed with TB or with any chronic cougher. She had not received any treatment for the complaints prior to her current visit. She had no known medical problem, and her family and psychosocial history were unremarkable.
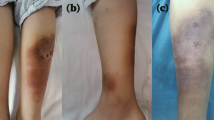
Her physical examination revealed a conscious, emaciated, and wasted child. Her admission vital signs were pulse rate 80 beats/min, respiratory rate 20 breaths/min, blood pressure 90/60 mmHg, and axillary temperature 37.3 °C. Matted bilateral anterior cervical and postauricular lymphadenopathy with pus-draining sinus was noted. Crepitation over the anterior and posterior lower right chest, multiple skin ulcers with purulent drainage over the left lateral neck, anterior left chest, and left axilla were documented (see Figs. 1 and 2). Nuchal rigidity was positive, but no neurologic deficit was present.
The results of complete blood count, urinalysis, and biochemical analysis were normal, except for mild anemia (see Table 1). The result of an antibody test for human immunodeficiency virus was negative. The patient’s erythrocyte sedimentation rate was 65 mm/hr in the first hour. Cerebrospinal fluid analysis showed 105 cells with 65 lymphocytes, and no organism was detected on Gram stain and acid-fast bacilli stain. Right upper and middle lobe ill-defined air space opacity was noted on a chest x-ray (see Fig. 3). Discharge analysis from the skin revealed gram-positive diplococci in chain, and Mycobacterium tuberculosis was detected using the Xpert MTB/RIF assay (Cepheid, Sunnyvale, CA, USA). Fine-needle aspiration cytology showed only caseous necrosis and no granuloma, and smears from ulcerated lesions showed mixed inflammatory cells, predominantly polymorphs. Tuberculous scrofuloderma was diagnosed on the basis of skin biopsy with a section showing mature squamous cell-lined skin tissue composed of epithelioid cell granuloma, multinucleated giant cells, caseous necrosis, and mixed inflammatory cells (see Figs. 4 and 5). Brain computed tomographic scans showed multiple precontrast hyperdense randomly distributed supra- and infratentorial lesions with mild perilesional edema. Rim enhancement on postcontrast images (caseating granulomas) on some lesions and a solid pattern of enhancement (noncaseating granulomas) were evident on other lesions. Dense basal cistern exudate seen on precontrast images with avid postcontrast basal leptomeningeal enhancement was observed. Severe bilateral lateral third- and fourth-ventricle dilation was noted (see Figs. 6, 7 and 8, Table 1). A tuberculin skin test (TST) could not be done, owing to unavailability of the service.
Routine care and medical treatment was provided as per World Health Organization (WHO) guidelines for severe acute malnutrition. Antituberculosis therapy with rifampicin, isoniazid, pyrazinamide, and ethambutol as per weight (four tabs per day), prednisolone 2 mg/kg/day, and pyridoxine 25 mg/day was started. Wound care was also given. After a 1-month hospital stay, the patient was discharged for outpatient directly observed antituberculosis therapy in a nearby health center after acute complications were treated and once the skin lesion had started to dry or heal. She received antituberculosis therapy for 12 months. No drug-related side effects were seen or reported during admission or follow-up. Follow-up visits (including 6 months after completion of therapy) demonstrated a patient who had recovered well with no major neurologic problems and with healed skin lesions.
Discussion
This case report presents a rare form of TB, CTB. Our patient was an unvaccinated 12-year-old African Ethiopian girl who presented with purulent discharge and skin ulceration of 3 months’ duration. She had dry cough, low-grade fever, decreased appetite, drenching night sweats, and global throbbing headache, and she had lost a significant amount of weight. Pathologic tests confirmed scrofuloderma coexisting with disseminated TB. She was managed, and she responded well to the treatment. This case report uniquely presents CTB coexisting with extrapulmonary TB and calls for better clinical assessments and workup for coexisting forms of TB. It also stresses the need for a confirmatory pathologic skin test to avoid a delay in treatment initiation.
CTB is a rare form of TB [2], and Ethiopia has one of the highest TB burdens worldwide [1]. An Ethiopian study of adult patients documented CTB to be the second most common histopathologically diagnosed skin disorder [9]. Scrofuloderma is the commonest form of CTB in children and almost always is of the endogenous type [10, 11]. Children with CTB tend to have a disseminated form of TB, as in our patient [12].
CTB diagnosis is a challenge, owing to difficulty in recovering the bacilli. Generally, diagnostic methods have a low sensitivity and specificity for CTB compared with the pulmonary form of TB. For suspected CTB, it is advised to do a TST, obtain a chest x-ray, and perform histopathologic examination and culture for acid-fast bacilli as well as PCR of skin sample and blood [13].
The TST result tends to be positive in CTB (33–96% of cases), creating difficulty in differentiating whether positivity is for true mycobacterial infection or nontuberculous mycobacterial infection and/or related to bacille Calmette-Guérin vaccination. This is a common problem in endemic TB settings such as Ethiopia. Even then, it is not a routine practice in Ethiopian settings to do a TST for TB screening, and hence it was not done in our patient [14, 15]. Extrapulmonary TB diagnosis, including CTB, using the Xpert MTB/RIF assay is recommended by the WHO [14]. The Xpert MTB/RIF test of skin discharge revealed M. tuberculosis in our patient.
Histologic diagnosis of CTB is based on pathologic findings of lymphocytes, epithelioid histiocytes, giant cells, necrosis, and granuloma. Histology assists in differentiating other skin pathologies that mimic TB [13, 15, 16]. Our patient’s skin histologic examination results are depicted in the figures and support the diagnosis of scrofuloderma.
Treatment of CTB is similar to pulmonary TB and will be prolonged for coexisting extrapulmonary forms of TB. Recommended treatment includes a 2-month four-drug regimen (isoniazid, rifampicin, pyrazinamide, and ethambutol), followed by two-drug therapy (isoniazid and rifampicin). The duration of the two-drug regimen is decided on the basis of the patient’s clinical condition. Pyridoxine is recommended for malnourished children to alleviate the neurologic side effects of isoniazid [1, 17, 18]. Our patient had a central nervous system and pulmonary form of TB coexisting with CTB. Recommended treatment with four antituberculosis drugs, pyridoxine, and a steroid (prednisolone) was initiated. Severe acute malnutrition was managed as per WHO guidelines [19].
Early detection of TB through patient-initiated and screening pathways needs to be reinforced. Early detection or diagnosis, especially among high-risk groups such as children will help to alleviate death and disability related to TB [20]. Our patient had symptoms of TB for months, and early TB detection programs or systems could have prevented the severe and disfiguring form of TB in our patient.
Conclusions
This report presents a case of a patient with a rare form of extrapulmonary TB. CTB should be considered in a child presenting with a skin lesion or discharge. CTB cases should be investigated for coexisting pulmonary and extrapulmonary forms of TB. A histopathologic diagnosis should be considered to rule out other skin pathologies and also to prevent delay in treatment. TB prevention strategies, including vaccination, need to be strengthened.
Abbreviations
- CTB:
-
Cutaneous tuberculosis
- TB:
-
Tuberculosis
- TST:
-
Tuberculin skin test
- WHO:
-
World Health Organization
- Xpert MTB/RIF:
-
Automated real-time nucleic acid amplification technology used for rapid and simultaneous detection of tuberculosis and rifampicin resistance
References
World Health Organization. Global tuberculosis report 2017. Geneva: World Health Organization; 2017.
Santos JB, Figueiredo AR, Ferraz CE, Oliveira MH, Silva PG, Medeiros VL. Cutaneous tuberculosis: epidemiologic, etiopathogenic and clinical aspects - part I. An Bras Dermatol. 2014;89(2):219–28.
Sehgal VN, Bhattacharya SN, Jain S, Logani K. Cutaneous tuberculosis: the evolving scenario. Int J Dermatol. 1994;33(2):97–104.
Grange JM. Mycobacterial diseases. London: Edward Arnold; 1980. p. 68–75.
Frankel A, Penrose C, Emer J. Cutaneous tuberculosis: a practical case report and review for the dermatologist. J Clin Aesthet Dermatol. 2009;2(10):19–27.
Lai-Cheong JE, Perez A, Tang V, Martinez A, Hill V, Menagé HP. Cutaneous manifestations of tuberculosis. Clin Exp Dermatol. 2007;32(4):461–6.
Bravo FG, Gotuzzo E. Cutaneous tuberculosis. Clin Dermatol. 2007;25(2):173–80.
Murugan S, Vetrichevvel T, Subramanyam S, Subramanian A. Childhood multicentric lupus vulgaris. Indian J Dermatol. 2011;56(3):343–4.
Bezabih M. Patterns of chronic dermatoses in an Ethiopian central teaching hospital: a histopathologic approach. Skinmed. 2002;1(2):101–6.
Terranova M, Padovese V, Fornari U, Morrone A. Clinical and epidemiological study of cutaneous tuberculosis in Northern Ethiopia. Dermatology. 2008;217(1):89–93.
Dias MF, Bernardes Filho F, Quaresma MV, Nascimento LV, Nery JA, Azulay DR. Update on cutaneous tuberculosis. An Bras Dermatol. 2014;89(6):925–38.
Kumar B, Rai R, Kaur I, Sahoo B, Muralidhar S, Radotra BD. Childhood cutaneous tuberculosis: a study over 25 years from northern India. Int J Dermatol. 2001;40(1):26–32.
Santos JB, Figueiredo AR, Ferraz CE, Oliveira MH, Silva PG, Medeiros VL. Cutaneous tuberculosis: diagnosis, histopathology and treatment - part II. An Bras Dermatol. 2014;89(4):545–55.
World Health Organization. Automated real-time nucleic acid amplification technology for rapid and simultaneous detection of tuberculosis and rifampicin resistance: Xpert MTB/RIF assay for the diagnosis of pulmonary and extra pulmonary TB in adults and children. Policy update. Geneva: World Health Organization; 2013.
De Maio F, Trecarichi EM, Visconti E, Sanguinetti M, Delogu G, Sali M. Understanding cutaneous tuberculosis: two clinical cases. JMM Case Rep. 2016;3(6):e005070.
Bhutto AM, Solangi A, Khaskhely NM, Arakaki H, Nonaka S. Clinical and epidemiological observations of cutaneous tuberculosis in Larkana, Pakistan. Int J Dermatol. 2002;41(3):159–65.
Dartois V. The path of anti-tuberculosis drugs: from blood to lesions to mycobacterial cells. Nat Rev Microbiol. 2014;12(3):159–67.
Van Zyl L, du Plessis J, Viljoen J. Cutaneous tuberculosis overview and current treatment regimens. Tuberculosis (Edinb). 2015;95(6):629–38.
World Health Organization. Guideline: Updates on the management of severe acute malnutrition in infants and children. Geneva: World Health Organization; 2013.
World Health Organization. Early detection of tuberculosis: an overview of approaches, guidelines and tools. Geneva: World Health Organization; 2011.
Acknowledgements
Not applicable.
Funding
No funding was received for this study.
Availability of data and materials
Data used in the creation of this case report can be made available depending on the effect on the patient’s confidentiality.
Author information
Authors and Affiliations
Contributions
HT has accepted the responsibility of this manuscript preparation. The author read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Written informed consent was obtained from the patient’s legal guardian(s) for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing interests
The author declares that he has no competing interests.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Tadele, H. Scrofuloderma with disseminated tuberculosis in an Ethiopian child: a case report. J Med Case Reports 12, 371 (2018). https://doi.org/10.1186/s13256-018-1927-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-018-1927-1