Abstract
Background
Acute appendicitis in a neonate and premature baby is still considered a rare entity as diagnosis is always made after surgical exploration for acute abdominal findings mimicking necrotizing enterocolitis.
Our reported case is a premature baby who had a perforated appendix with no evidence of peritonitis.
Case presentation
We describe the case of a premature Bahraini girl born at 29 weeks of gestation by spontaneous vaginal delivery to a 39-year-old G6P5 mother. She was kept on a ventilator for the first 6 days of life, and had an uneventful Neonatal Intensive care stay until her 47th day of life when she developed sepsis that required ventilator support for 3 days. At day 51 she developed abdominal distension and was referred to a pediatric surgeon by day 54 with pneumoperitoneum. Her abdomen was soft with minimal tenderness and no evidence of erythema or edema. In view of pneumoperitoneum and previously reported sepsis, she was taken for exploratory laparotomy. The findings were consistent with a perforated appendix with no evidence of peritonitis or necrotizing enterocolitis. An appendectomy was performed. She had a smooth postoperative recovery.
Conclusions
Neonatal appendicitis continues to be a diagnostic challenge. Only with a high index of clinical suspicion and teamwork can these cases be managed successfully and mortality and morbidity rates may reduce.
Similar content being viewed by others
Background
Although no age is free from the risk of appendicitis, it is extremely uncommon in newborns [1].
The rarity of neonatal appendicitis (NA) together with lack of specific signs and low index of suspicion has led to delay in diagnosis and surgical intervention [2]. Most of the time the diagnosis is delayed and is made after perforation has occurred.
It was proposed that NA is actually a limited form of necrotizing enterocolitis (NEC) [3]. The observation that more than 50% of babies with appendicitis are preterm [4] adds strength to the theory because 90% of NEC is also found in premature babies [1].
Although it has been reported for over 100 years, the total collective cases reported are around 100 of which most presented with peritonitis [4].
Case presentation
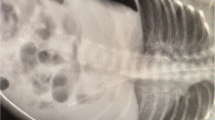
We describe the case of a premature Bahraini girl born at 29 weeks of gestation by spontaneous vaginal delivery, to a 39-year-old gravida 6 para 5 mother. She was born “flat” with an APGAR score of 4 and 9 at 1 and 5 minutes respectively and a birth weight of 910 g. Ventilatory support was required during her first 6 days of life, with a dose of surfactant. She had an uneventful Neonatal Intensive care stay, tolerating breast milk and was gaining weight at a steady pace. On her 47th day of life she developed sepsis and required repeated ventilator support for 3 days. At day 51 she weighed 1400 g, but developed abdominal distension and feed intolerance. She was referred to the pediatric surgeon on day 54 when pneumoperitoneum was detected by a shoot-through lateral plain abdominal film (Fig. 1). Our examination showed her abdomen to be distended but soft with mild diffuse tenderness and no signs of peritonitis. There was no abdominal wall erythema or visible bowel loops. We did not find any hernias or abdominal masses. Her C-reactive protein (CRP) was 37 mg/L which is 12 times higher than the normal range. In view of pneumoperitoneum, she was taken for exploratory laparotomy. A classic right transverse upper abdominal incision was used to open her abdomen as the diagnosis was NEC. Her entire small and large bowel was healthy and normal in appearance (Fig. 2). Her appendix measured approximately 2 cm in length and was acutely inflamed with a perforation at the tip. Except for the site of perforation, there was no other evidence of gangrene (Fig. 3). The findings were consistent with a perforated appendix with no evidence of peritonitis or NEC. An appendectomy was performed. She had a smooth postoperative recovery where she was started on breast milk on the second postoperative day and her CRP was normal on the eighth postoperative day. Histology demonstrated mucosal ulceration of her appendiceal wall, marked acute transmural inflammation, and necrotic wall at the perforated end (Fig. 4) but the rest had intact mucosal lining (Fig. 5). A neuron-specific enolase (NSE) immunohistochemical stain showed positive staining for nerve fibers (Fig. 6) which excluded Hirschsprung’s disease. She was discharged home at day 120 of life and was thriving at 2-year follow-up.
Discussion
NA is an extremely rare condition, with fewer than 50 cases reported in the last 30 years and just more than 100 over the last century [5]. The incidence of NA has been reported as 0.04 to 0.2% [6]. NA occurs in males approximately 75% of the time and 25 to 50% of all reported cases involve premature babies [1, 4]. As the survival of young babies improves with better perinatal care, one would expect the frequency of appendicitis to rise along with the incidence of NEC in this population [3].
The rarity of appendicitis in the neonatal period (0.04% reported incidence) is classically attributed to the broad orifice of the appendix (“conical,” “funnel,” or “fetal” anatomy), liquid diet, near-constant supine positioning, the lack of fecaliths in neonates, and the presumed relative infrequency of lymphatic hyperplasia in the periappendiceal region caused by lack of infectious stimuli [7]. The infrequency of this disease and resultant delay in diagnosis are largely responsible for the higher reported associated morbidity and mortality in perinatal and other age groups [4].
Generalized peritonitis and intestinal congestion of perforated appendicitis is difficult to distinguish from that of NEC [1]. Existing reports suggest that even when a misdiagnosis occurs, if that diagnosis nevertheless leads to surgical exploration, then the outcome is likely to be better than if laparotomy is delayed [7].
The most common presenting clinical feature in the literature was abdominal distension, which was present in 89% of patients [1] and it was the presenting feature in our patient. The presence of free air on plain abdominal radiograph may confer a more favorable prognosis by leading to early surgical intervention [5].
Pneumoperitoneum is the single most useful sign which was seen in 23 of the 44 (52%) patients with perforation. Even in the absence of correct clinical diagnosis, perforation – as indicated by pneumoperitoneum – appears to have prompted surgical exploration; this was the reason for the referral of our patient. NA does not appear to have any causal relationship with Hirschsprung’s disease [1] and our reported case has normal ganglia. The association between NA and NEC deserves further investigation because both share the same spectrum of risk factors [1].
Although rare, NA can be expected to occur with increasing frequency as perinatal conditions associated with appendicitis, such as prematurity and survival after severe hypoxia or ischemia, are much more common in this era of improved neonatal care [7].
Conclusions
NA continues to be a diagnostic challenge. Only with a high index of clinical suspicion and teamwork can these cases be managed successfully and the mortality rate may reduce.
References
Raveenthiran V. Neonatal appendicitis (part 1): A Review of 52 cases with abdominal manifestation. J Neonatal Surg. 2015;4:4.
El-Gohary MA, Al JS. Neonatal appendicitis with perforation: A case report. J Ped Surg Case Reports. 2014;2:353–4.
Bax NM, Pearse RG, Dommering N, Molenaar JC. Perforation of the appendix in the neonatal period. J Pediatr Surg. 1980;15:200–2.
Karaman A, Cavuşoğlu YH, Karaman I, Cakmak O. Seven cases of neonatal appendicitis with a review of the English language literature of the last century. Pediatr Surg Int. 2003;19:707–9.
Schwartz KL, Gilad E, Sigalet D, Yu W, Wong AL. Neonatal acute appendicitis: a proposed algorithm for timely diagnosis. J Pediatr Surg. 2011;46:2060–4.
Stifle D, Stallmach T, Sachet P. Acute appendicitis in neonates: complication or morgues sui generis? Pediatr Surg Int. 1998;14:122–3.
Jancelewicz T, Kim G, Miniati D. Neonatal appendicitis: a new look at an old zebra. J Pediatr Surg. 2008;43:e1–5.
Acknowledgements
Not applicable.
Funding
Not applicable.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed during the current study.
Authors’ contributions
FH wrote the article, reviewed the literature, and provided the operative images. BA is part of the surgical team who reviewed the case and the manuscript. MK reviewed the manuscript with valuable comments. MJ managed the neonate in the Unit, reviewed the manuscript, and added some valuable information. SS provided the histological images, the comments and captions, and reviewed the manuscript. All authors read and approved the final manuscript.
Competing interests
The authors declare that they have no competing interests.
Consent for publication
Written informed consent was obtained from the patient’s parents for publication of this case report and any accompanying images. A copy of the written consent will be available for review by the Editor-in-Chief of this journal on request.
Ethics approval and consent to participate
Not applicable.
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Haider, F., Ayoub, B., Al Kooheji, M. et al. Perforated acute appendicitis with no peritonitis in a premature baby: a case report. J Med Case Reports 11, 125 (2017). https://doi.org/10.1186/s13256-017-1289-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-017-1289-0