Abstract
Background
Extramedullary plasmacytoma is a plasma cell neoplasm that presents as a solitary lesion in soft tissue. Most extramedullary plasmacytomas involve the nasopharynx or upper respiratory tract. Primary plasmacytoma of the stomach is extremely rare.
Case presentation
A 78-year-old Korean woman presented with epigastric pain for 3 months. She had a history of an intractable gastric ulcer despite repeated endoscopic biopsies and appropriate medical therapy for the ulcer. She underwent another endoscopy and a biopsy was performed for multiple large and deep specimens. Ultimately, primary gastric plasmacytoma was confirmed. However, she and her attendant refused standard local radiotherapy or surgical resection. She came to our emergency room 3 months later with hematemesis due to a large gastric ulcer, despite management with medication for over 3 months at a local clinic. We again recommended local radiation or surgical resection. However, as she was willing to undergo only medical therapy, she was prescribed high-dose dexamethasone. Surprisingly, her ulcer completely regressed and remission was maintained for over 1 year.
Conclusions
We report successful treatment of a rare primary gastric plasmacytoma mimicking intractable ulcer by using high-dose dexamethasone. To the best of our knowledge, this is the first reported case successfully treated with only high-dose dexamethasone.
Similar content being viewed by others
Background
Plasma cell neoplasms are commonly divided into four groups: multiple myeloma (MM), plasma cell leukemia, solitary plasmacytoma of the bone (SPB), and extramedullary plasmacytoma (EMP) [1]. Most EMPs involve the upper respiratory tract, including the sinuses, nasal cavity, and nasopharynx; isolated primary plasmacytoma of the stomach is extremely rare [2].
Case presentation
A 78-year-old Korean woman presented with a complaint of epigastric pain for 3 months. She was diagnosed with atrial fibrillation and ejection fraction-preserved heart failure 5 years earlier. She received regular follow-up observations and took aspirin.
She initially underwent an endoscopy at our clinic and was found to have extensive mucosal erythema with an ulcer crater at the antrum. Pathologic findings revealed chronic gastritis without Helicobacter pylori colonization. She underwent gastric ulcer therapy including a proton pump inhibitor (PPI). After 1 month, a follow-up endoscopy showed an unchanged ulcer. A repeat biopsy examination revealed chronic inflammation without H. pylori colonization. She was prescribed another PPI with a regimen for H. pylori eradication (metronidazole, clarithromycin, PPI). However, her epigastric symptoms continued and she left our hospital.
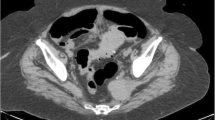
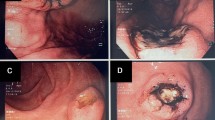
A follow-up endoscopy performed 2 months later, despite appropriate and sufficient medical therapy in our clinic for over 3 months, showed no interval change (Fig. 1a).
Endoscopic finding. a Extensive mucosal erythema with an ulcer crater at the antrum was seen. b A large gastric ulcer with a bleeding spot at the antrum was seen 3 months later. c After 2 weeks of high-dose dexamethasone, the ulcer lesion showed marked healing. d After four cycles of high-dose dexamethasone, a healed ulcer scar replaced the ulcer lesion
An endoscopic biopsy was performed to produce multiple large and deep specimens to differentiate other diseases. Pathologic findings showed dense plasmacytic proliferation of small mature lymphocytic cells; these proliferative cells stained immunohistochemically positive for lambda light chains and negative for kappa chains, suggesting plasmacytoma (Fig. 2). Therefore, we evaluated the patient for MM with a bone marrow biopsy and considered serum monoclonal gammopathy. However, she had no evidence of bone marrow involvement with plasmacytoma or any monoclonal gammopathy through electrophoresis and immunofixation.
We concluded that she had primary gastric plasmacytoma; we recommended local radiotherapy or surgical resection. However, she and her attendant refused further treatment due to old age and limited finances.
She came to our emergency room 3 months later because of hematemesis due to a large gastric ulcer, despite PPI treatment for over 3 months at a local clinic (Fig. 1b). We performed endoscopic hemocoagulation with high-dose PPI and tranexamic acid. We again recommended local radiation or surgical resection, but she still declined extensive treatment. Therefore, we recommended high-dose dexamethasone (40 mg daily for 4 days every 3 weeks) to be administered intravenously to control the plasmacytoma, and she accepted.
After 2 weeks of high-dose dexamethasone, an endoscopy revealed marked healing of her ulcer (Fig. 1c). After a total of four cycles of high-dose dexamethasone, the ulcer was not apparent on endoscopy (Fig. 1d). The patient underwent a total of six cycles of high-dose dexamethasone. One year later, no ulcer was observed on endoscopy.
Discussion
EMP is a mass of neoplastic monoclonal plasma cells that presents as a solitary lesion in a soft tissue other than the bone. It is uncommon and accounts for approximately 3 % of all plasma cell neoplasms [2].
On endoscopy, gastric plasmacytoma usually appears either as an ulcerated mass or as a discrete ulcer with thickened gastric folds. Thus, it must be differentiated from gastric ulcer, gastric adenocarcinoma, or lymphoma, in particular from mucosa-associated lymphoid tissue (MALT) lymphoma [3, 4]. This case initially revealed extensive mucosal erythema with an ulcer crater and then changed into a large bleeding ulcer.
On pathological examination, a gastric plasmacytoma shows the typical morphologic finding of plasma cell proliferation with immunohistochemistry demonstration of monoclonal light (kappa or lambda) or heavy chains (immunoglobulin G, A, or M). The final diagnosis of primary gastric plasmacytoma is made by histologic confirmation of a single lesion in the stomach without bone lesions, no evidence of plasma malignancy in the bone marrow, and no monoclonal gammopathy [5, 6].
Usually, most EMPs present at an upper respiratory site and are hard to resect completely due to invasiveness; thus, surgery is not recommended for initial treatment. EMP is highly sensitive to radiotherapy; thus, local radiotherapy is the first choice for EMP due to its significant curative potential and lower relapse rate [1].
Currently, there are no general guidelines for the treatment of primary gastric plasmacytoma; however, local radiotherapy may be superior to surgery in plasmacytomas of the stomach due to organ preservation [7, 8].
If primary gastric plasmacytoma only involves the submucosa of the stomach, endoscopic submucosal resection can be another treatment option. If the result of a test for H. pylori is positive, then eradication may be an alternative treatment [9, 10]. Recently, bortezomib, which acts as an inhibitor of the ubiquitin–proteasome pathway, alone or in combination with dexamethasone proved effective in the management of extramedullary relapse of MM, and might be an alternative treatment [11].
EMP usually behaves like an indolent disease because of its tendency to localize and it shows a low rate of progression to MM. The prognosis of gastric plasmacytoma is not well understood. However, EMP has a favorable prognosis with a 70 % disease-free survival at 10 years; the 10-year rate of progression of EMP to MM ranges from 11 to 30 % [12, 13]. In this case, our patient and her attendant refused local radiotherapy and surgery due to old age and limited finances; however, she was refractory to ulcer medication and had a life-threatening condition. Therefore, we only used high-dose dexamethasone and the large refractory ulcer showed dramatic regression.
Conclusions
This is the report of a case of an intractable gastric ulcer, despite repeated endoscopic biopsies and sufficient gastric ulcer therapy, which was finally confirmed as a primary gastric plasmacytoma through deep multiple endoscopic biopsies. The patient only accepted high-dose dexamethasone despite the recommendation of standard local radiotherapy or surgical resection. The intractable and life-threatening ulcer completely regressed and remission was maintained for over 1 year. This case was rare and to the best of our knowledge it is the first report of successful treatment using only high-dose dexamethasone.
Consent
Written informed consent was obtained from the patient for publication of this case report and any accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Abbreviations
- EMP:
-
extramedullary plasmacytoma
- H. pylori :
-
Helicobacter pylori
- MALT:
-
mucosa-associated lymphoid tissue
- MM:
-
multiple myeloma
- PPI:
-
proton pump inhibitor
- SPB:
-
plasmacytoma of the bone
References
Alexiou C, Kau RJ, Dietzfelbinger H, Kremer M, Spiess JC, Schratezenstaller B, et al. Extramedullary plasmacytoma: Tumor occurrence and therapeutic concepts. Cancer. 1999;85:2305–14.
Nolan KD, Mone MC, Nelson EW. Plasma cell neoplasms. Review of disease progression and report of a new variant. Surg Oncol. 2005;14:85–90.
Gutnik SH, Bacon BR. Endoscopic appearance of gastric myeloma. Gastrointest Endosc. 1985;31:263–5.
Esfandyari T, Abraham SC, Arora AS. Gastrointestinal plasmacytoma that caused anemia in a patient with multiple myeloma. Nat Clin Pract Gastroenterol Hepatol. 2007;4:111–5.
Soutar R, Lucraft H, Jackson G, Reece A, Bird J, Low E, et al. Guidelines on the diagnosis and management of solitary plasmacytoma of bone and solitary extramedullary plasmacytoma. Br J Haematol. 2004;124:717–26.
Vincent RS. Multiple myeloma: 2014 update on diagnosis, risk-stratification, and management. Am J Hematol. 2014;89:999–1009.
Tan J, Lade S, Harrison S, Opat S, Mac Manus MP. Complete remission of localised gastric plasmacytomas following definitive radiotherapy. J Med Imaging Radiat Oncol. 2012;56(3):328–31.
Krishnamoorthy N, Bal MM, Ramadwar M, Deodhar K, Mohandas KM. A rare case of primary gastric plasmacytoma: an unforeseen surprise. J Cancer Res Ther. 2010;6:549–51.
Park CH, Lee SM, Kim TO, et al. Treatment of solitary extramedullary plasmacytoma of the stomach with endoscopic submucosal dissection. Gut Liver. 2009;3:334–7.
Wöhrer S, Isaacson PG, Raderer M. Complete regression of primary gastric plasmacytoma following Helicobacter pylori eradication. Ann Hematol. 2004;83(10):666.
Katodritou E, Kartsios C, Gastari V, Verrou E, Mihou D, Banti A, et al. Successful treatment of extramedullary gastric plasmacytoma with the combination of bortezomib and dexamethasone: first reported case. Leuk Res. 2008;32:339–41.
Kilciksiz S, Karakoyun-Celik O, Agaoglu FY, Haydaroglu A. A review for solitary plasmacytoma of bone and extramedullary plasmacytoma. Sci World J. 2012;2012:895765.
Galieni P, Cavo M, Pulsoni A, Avvisati G, Neri CB. Clinical outcome of extramedullary plasmacytoma. Haematologica. 2000;85:47–51.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
DYK was the major contributor in writing the manuscript. GBK, BSC, JWS, HJL, and RH were involved in drafting, writing and editing the manuscript. SGP was involved in drafting, writing and editing the manuscript, and reviewed the manuscript as Corresponding author. All authors read and approved the final manuscript.
Rights and permissions
Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (http://creativecommons.org/licenses/by/4.0/), which permits unrestricted use, distribution, and reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Kang, Dy., Kim, GB., Choi, BS. et al. Successful treatment of a primary gastric plasmacytoma mimicking intractable gastric ulcer by using high-dose dexamethasone therapy: a case report. J Med Case Reports 10, 79 (2016). https://doi.org/10.1186/s13256-016-0863-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13256-016-0863-1