Abstract
Objectives
This systematic review and meta-analysis aimed to assess the stroke detection performance of artificial intelligence (AI) in magnetic resonance imaging (MRI), and additionally to identify reporting insufficiencies.
Methods
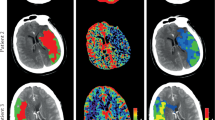
PRISMA guidelines were followed. MEDLINE, Embase, Cochrane Central, and IEEE Xplore were searched for studies utilising MRI and AI for stroke detection. The protocol was prospectively registered with PROSPERO (CRD42021289748). Sensitivity, specificity, accuracy, and area under the receiver operating characteristic (ROC) curve were the primary outcomes. Only studies using MRI in adults were included. The intervention was AI for stroke detection with ischaemic and haemorrhagic stroke in separate categories. Any manual labelling was used as a comparator. A modified QUADAS-2 tool was used for bias assessment. The minimum information about clinical artificial intelligence modelling (MI-CLAIM) checklist was used to assess reporting insufficiencies. Meta-analyses were performed for sensitivity, specificity, and hierarchical summary ROC (HSROC) on low risk of bias studies.
Results
Thirty-three studies were eligible for inclusion. Fifteen studies had a low risk of bias. Low-risk studies were better for reporting MI-CLAIM items. Only one study examined a CE-approved AI algorithm. Forest plots revealed detection sensitivity and specificity of 93% and 93% with identical performance in the HSROC analysis and positive and negative likelihood ratios of 12.6 and 0.079.
Conclusion
Current AI technology can detect ischaemic stroke in MRI. There is a need for further validation of haemorrhagic detection. The clinical usability of AI stroke detection in MRI is yet to be investigated.
Critical relevance statement
This first meta-analysis concludes that AI, utilising diffusion-weighted MRI sequences, can accurately aid the detection of ischaemic brain lesions and its clinical utility is ready to be uncovered in clinical trials.
Key Points
-
There is a growing interest in AI solutions for detection aid.
-
The performance is unknown for MRI stroke assessment.
-
AI detection sensitivity and specificity were 93% and 93% for ischaemic lesions.
-
There is limited evidence for the detection of patients with haemorrhagic lesions.
-
AI can accurately detect patients with ischaemic stroke in MRI.
Graphical Abstract

Similar content being viewed by others
Introduction
Stroke is an acute onset of focal neurologic symptoms due to of vascular origin from the central nervous system. It is a clinical diagnosis and brain imaging is needed to differentiate between ischaemic and haemorrhagic aetiology. Computed tomography (CT) has for years been the de facto standard imaging modality due to its availability and speed with current guidelines recommending intravenous thrombolysis for ischaemic stroke within 4.5 h of known onset [1, 2]. Presently, many advanced institutions are shifting towards magnetic resonance imaging (MRI) even in the acute diagnosis of stroke. MRI has superior sensitivity and can identify acute ischaemia with unknown stroke onset that is potentially reversible with revascularisation, e.g. by demonstrating a mismatch between diffusion-weighted imaging (DWI) and fluid-attenuated inversion recovery (FLAIR) negative sequences [1,2,3,4]. MRI is also highly useful in cases of uncertainty as to a stroke diagnosis. Moreover, MRI optimisation has enabled patient treatment flows similar to those achieved using brain CT regarding, e.g. door-to-needle time [5]. There is increased use of medical imaging including MRI in the healthcare system [6, 7], a trend that is expected to continue in the future [8]. The increasing burden on radiological departments is not predicted to be backed with an equivalent increase in radiologists and it is therefore highly likely that increased MRI use will lead to longer response times or increased error rates [9, 10]. To counterbalance this for stroke diagnosis, artificial intelligence (AI) has been proposed as a technology to enhance the radiology workflow [11,12,13].
The detection properties of AI can be used in a multitude of workflows including triaging, detection aid, MRI protocol selection, and contrast agent admission decisions. Several studies have reviewed AI for stroke imaging, but these are either applied to CT, are unsystematic, or with a scope too wide to properly elucidate stroke detection in MRI [11,12,13,14,15,16,17,18,19,20].
This systematic review aims to assess the performance of AI for automated stroke detection in brain MRI. The objectives of the review are to: (1) estimate the current detection performance for clinically representative studies, (2) characterise the studies, their respective AI algorithms, and whether they have received the European Conformity mark (CE) or received the US Food and Drug Administration (FDA) approval, and (3) utilise the minimum information about clinical artificial intelligence modelling (MI-CLAIM) checklist to characterise reporting trends [21]. For this study, only lesions confirmable in images and compatible with stroke lesions are examined and will onward be mentioned as either ischaemic stroke type or haemorrhagic stroke type depending on their radiological appearance.
Materials and methods
The review was performed according to the Preferred Reporting of Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [22]. The protocol was prospectively registered with the International Prospective Register of Systematic Reviews (PROSPERO) on 16th November 2021 (CRD42021289748) [23]. Eligibility criteria for inclusion were formed using the participants-intervention-comparator-outcome-study (PICOS) design [24].
Eligibility criteria
Studies with MRI and AI for stroke assessment, encompassing retrospective, prospective, and diagnostic test studies were included. Participant recruitment strategies were classified as outlined in the Cochrane Handbook [25, 26].
Studies were included if participants were aged 18 years or older, the target condition was stroke or any of its subcategories, and non-stroke patients were used as comparators. At least one of the following had to be reported: (1) sensitivity and specificity, (2) accuracy, or (3) area under the ROC (AUROC) curve.
Search strategy and information sources
A systematic search was conducted in MEDLINE (Ovid), Embase (Ovid), Cochrane Central, and IEEE Xplore. The search strategy was defined in close cooperation with an information specialist at the local institutional research library. No limitations were made for publication date or language. Subject headings and free text terms relating to the categories MRI, stroke and AI were used. Search blocks were identified for both MRI [27] and stroke [28] through reviews in the Cochrane Library. The reviews from the Cochrane Library were also translated to cover all databases but IEEE Xplore. Due to the restrictions of the IEEE Xplore search machine, the search string was translated to only cover free text terms for this database. Complete search strings for all databases are provided in the online supplementary Table S1. Conference posters and abstracts identified in the search were also eligible. Conference and poster abstracts that were not excluded in the initial screening were followed up by an email enquiry to the corresponding authors for a full record. A reminder e-mail was sent one week after the first if no response was obtained. If no response was obtained after one additional week, they were assessed solely on the information contained in the conference poster or abstract and included based on this if deemed eligible. The systematic searches were updated on 1st November 2023.
Selection and extraction
All studies were uploaded to EndNote 20 (Clarivate, Philadelphia, PA, USA) and managed with Covidence systematic review software (Veritas Health Innovation, Melbourne, Australia). Duplicates were removed automatically after importation to Covidence. Eligibility was based on the PICOS model as seen in Table 1. Two independent reviewers (J.A.B. and M.T.E.) completed title-abstract and full-text screening and performed bias assessment and data extraction. Any disagreement was resolved through discussion along with arbitration by a third reader (B.S.B.R.). Full-text exclusions were done with reason in categorical order as illustrated in the PRISMA flow chart (Fig. 1). Descriptive data, risk of bias, and results were extracted and handled in consensus between the two primary readers. Risk of bias assessments were performed prior to the assessment of the results to reduce bias in the review. The results collected were sensitivity, specificity, accuracy, and AUROC. Descriptive data collected included Study ID, Study design, Number of participants, Index test, Use of neural network, and FDA approval and CE marking. FDA approval and CE marking status were in addition cross-checked using the Radiology Health AI Register list [29]. Two reviewers (J.A.B. and M.T.E.) independently extracted all data.
Risk of bias analysis
For risk of bias analysis, a modified version of the quality assessment for diagnostic accuracy studies 2 (QUADAS-2) tool was used [30]. Modification was done to the index test domain to better accommodate AI. The modified QUADAS-2 tool along with the changes made are illustrated in the online supplementary Table S2.
Data analysis
Descriptive analysis was done on all included reports. Synthesis of detection results was only performed on reports with an overall low risk of bias. Data on AI performance was abstracted from included studies, or, if not reported, corresponding data were calculated based on available information. A meta-analysis of proportions on true positives (sensitivity) and true negatives (specificity) was performed. A bivariate random effects model with restricted maximum likelihood was used to account for relative heterogeneity. To estimate the general state of AI for detection, a hierarchical summary ROC (HSROC) model was made using the STATA metandi module [31]. The MI-CLAIM checklists [21] were quantitatively synthesised for each study to identify trends in insufficiency in reporting. Trends were analysed overall and for each part, i.e. study design, data and optimisation, model performance, model examination, and reproducibility. Analyses were done using STATA 18 (StataCorp, College Station, TX, USA).
Results
After duplicate removal, 1738 records were screened by their title and abstract of which 152 were eligible for full-text reading. The total number of included reports was 33 [32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64]. The complete flow of records including reasons for exclusion is illustrated in the PRISMA flow chart (Fig. 1). Full-text reports excluded with reasons for exclusion are listed in Table S3.
Study characteristics
Twenty-six of the reports were published in 2020 or later. Five reports collected more than one dataset for analysis. Eighteen reports used a case-control design, 12 a cohort design, one collected two datasets of which one set was a cohort and the other a case-control [39], and two reports did not describe their design. No reports used a randomised controlled trial design. Twenty-six studies collected data retrospectively, one study prospectively, and five did not report the method of data collection. One study collected two datasets; one set was retrospective, and no information was provided for the other [37]. For stroke type, 24 reports studied ischaemic stroke, one studied haemorrhagic stroke [63], two had a dataset for both ischaemic and haemorrhagic stroke [40, 49], one studied cerebral venous sinus thrombosis [63], and five reports did not elaborate on stroke type. Four studies performed multicentre data collection [36, 37, 39, 40], but none of them had an external multicentre test set. Descriptive study characteristics for each study are found in Table 2.
Setting characteristics
Ten studies had a timeframe setting for stroke onset of 24 h or “acute” with no further specification. Liu et al [39] had longitudinal scan data with patients scanned within both 3 h of symptom onset and again 24 h after symptom onset. None of the other studies utilised a timeframe within 4.5 h, “hyper-acute”, or “FLAIR negative” corresponding to current time or tissue criteria for treatment with thrombolysis. Fourteen studies did not report any definition or specification of the timeframe from onset until the scan. The most used MRI-sequence was FLAIR, T2, T1, and DWI. Two studies utilised functional MRI (fMRI) sequences for assessment [42, 51] and one used time-of-flight [34]. The comparators used in the studies were heterogeneous. Overall, eight studies compared with known normal scans, and three compared with known other pathology. The remaining studies were compared with a mix of patient MRI scans including no pathology, degenerative disorders, and inflammatory disorders. Eighty-five per cent of included studies used a neural network AI with a range of different network architecture backbones. For ten studies, data origin was available in online databases. Of all the studies, only one AI algorithm had received CE marking and none had received FDA approval. The setting characteristics are presented in the online supplementary Table S4.
Bias assessment
The risk of bias assessment resulted in 15 reports with an overall low risk of bias, out of the 33 included reports. The patient selection domain and the index test domain were responsible for the largest introduction of bias. Seven reports did not describe their reference standard. Although heterogeneous, all studies that reported their reference standard were considered reliable reference standards. Table 3 presents the risk of bias assessment and Table S5 further specifies category bias for each study.
MI-CLAIM assessment
None of the included studies reported to follow the MI-CLAIM checklist, although 17 studies were published in the years after the release of the MI-CLAIM paper from 2020 [21]. Only two studies [32, 34] claimed to follow a reporting standard which was the Standards for Reporting of Diagnostic Accuracy Studies (STARD) guideline [65] and one of those studies [32] additionally followed the Checklist for Artificial Intelligence in Medical Imaging (CLAIM) [66]. The total percentage of reported items was 72%. This was found to be higher in the low risk of bias studies (84% vs 63%). Low-risk and high-risk categories varied significantly in the study design part and in the data and optimisation part with the overall completion rates 100% vs 72% (Chi-squared 13.75; p = 0.008) and 93% vs 78% (Chi-squared 7.61; p = 0.02), respectively. Only five studies reported all items (except the sharing of code part) [39, 40, 42,43,44]. The model performance and model examination parts had generally lower rates in reported items with an overall of 64% and 66%, respectively. Five studies, hereof four with a low risk of bias, reported sharing of their code for reproducibility, while the remaining studies did not offer any option to reproduce their results. MI-CLAIM assessment results are presented in the online supplementary Table S6.
Detection results
The most frequently reported measurements were sensitivity and specificity. Nine of the 33 studies reported AUROC of which four were low risk of bias. Missing values (e.g. accuracy) could be calculated based on other reported values for most studies. Performance ranged from, 51 to 100% for sensitivity, 57 to 100% for specificity, 68 to 99% for accuracy, and 0.83 to 0.98 for AUROC. Liu et al [39] had lower detection rates in the 3-h scans with 96% as compared to 99% in the 24-h scans. Dørum et al [42] utilising fMRI reached random chance detection performance. The single AI examining haemorrhagic stroke from Nael et al [40] performed generally worse than those examining ischaemic stroke. Results for all studies are reported in Table 4. Further notes and clarifications for the results are found in the online supplementary Table S7.
Meta-analysis
To reduce heterogeneity among the low-risk-bias studies, Yang et al [34], Dørum et al [42], and Uchiyama et al [46] were excluded from the meta-analyses since these studies did not use DWI sequence to detect acute ischaemic stroke lesions. Wu et al [35] were excluded due to insufficient reporting. Forest plot meta-analyses of studies (Fig. 2) revealed an ischaemic stroke detection sensitivity of 93% (CI 86–96%) and specificity of 93% (CI 84–96%). in the HSROC meta-analysis (Fig. 3), the summary point had identical sensitivity and specificity values to corresponding measures in the forest plots. The positive and negative likelihood ratios were 12.6 (CI 5.7–27.7) and 0.079 (CI 0.039–0.159), respectively. The STATA data output from both analyses is presented in Table S8. The literature was not extensive enough to support the conduct of meta-analyses on haemorrhagic stroke.
Discussion
This systematic review found 33 studies in total assessing AI detection for stroke in MRI. The studies were found to have heterogeneity in the data collection and study design. Most studies examined ischaemic stroke with only a few examining the utility of AI in haemorrhagic stroke. Only one AI algorithm among the included studies had obtained CE marking. The MI-CLAIM assessment revealed insufficiencies in current reporting practice. Based on the nine studies included in the meta-analysis, both ischaemic sensitivity and specificity were 93% with strong likelihood ratios in detecting DWI-positive stroke.
The detection sensitivity in two studies [33, 41] was significantly lower compared to the remaining studies in the meta-analysis. One of them [41] only examined subcortical infarcts which are small vessel based and hence also smaller in lesion volume, which could be the cause, whereas the other [33] separated their stroke scans in single images, which has likely led to some image slices with only a few voxels of actual stroke.
One study [43] achieved significantly lower detection specificity than the remaining studies in the meta-analysis. In this study, the best specificity was obtained by creating synthetic images for training and their algorithm trained without use of the synthetic image was lower at 48%. This could indicate that they had an insufficient amount of available data to train the algorithm to obtain optimum detection performance. The lower detection specificity in another study [39] could likely be due to the set threshold, as they also present a significantly higher detection sensitivity.
One study [37] achieved significantly higher results both in terms of sensitivity and specificity. The most likely reason for this was their utilisation of multiple AI algorithms in a combined iterative majority voting. This practice may be better in terms of raw performance, however costly in terms of computational power requiring much more time to process and large expensive computer setups, which can be difficult to obtain in a clinical setup.
Reporting of AI studies
Sensitivity, specificity, and accuracy were the most reported outcomes. A measurement of AUROC was not available for most studies. Although FDA-approved and/or CE-marked solutions do exist [29], this systematic review only found one report of such a solution. Therefore, the performance of these commercial AI solutions in clinical practice cannot be extrapolated. The MI-CLAIM checklist was applied to collect the minimum information needed to compare the capabilities of AI and reproduce the results. However, several other relevant reporting guidelines exist, such as the CLAIM guideline, which is a more comprehensive checklist, and the specific AI version of the STARD guideline, which is in the works [65,66,67]. Given that only five of the 33 reports managed to inform on all MI-CLAIM fields, future studies should follow a relevant checklist for their studies to ensure good reporting practice in research.
Clinical relevance
Current stroke AI solutions are intended for decision support, as opposed to replacing medical staff [29, 68]. Another task of dismissing the AI false positive scans will be needed, which could prove time-consuming. Additionally, the impact of AI on the decisiveness of radiologists has been investigated in other fields of medical imaging. Mehrizi et al [69] piloted a study for AI support in mammography showing radiologists' evaluations were more prone to be erroneous when the AI made erroneous suggestions.
To assist the assessment before the implementation of an AI solution in a clinical setting, the recently developed model for assessing AI in medical imaging (MAS-AI) could be useful [70]. MAS-AI uses a holistic approach to match different AI algorithms and intended usage scenarios to help support decision-making. How AI affects patient prognosis and the diagnostic work-up routine of stroke patients has not been the scope of this review, but clinical trials examining such are needed prior to implementation.
Clinical stroke vs radiologically confirmed stroke
Stroke is a clinical diagnosis and occasionally the pathology of interest is invisible on MRI [71]. Furthermore, patients could be suffering from a transient ischaemic attack, where ischaemic lesions often are not visible. Considering the findings in this review, all the included studies utilised image evaluation by one or more medical doctors or the radiology report as their reference standard. It would be of interest to evaluate whether AI possesses the ability to detect strokes not apparent on MRI for the reporting radiologist.
Limitations
A large proportion of the included studies applied a case-control design, and none were randomised controlled trials. Furthermore, only a small proportion of the studies underwent analysis on external data, which introduces selection bias. We identified only five studies using external datasets for testing [32, 36, 37, 39, 40]. Systematic reviews for AI in other radiological fields have shown that AI performance decreases when tested on externally collected data [72, 73]. Therefore, it is preferable for future AI validation studies to incorporate externally collected, clinically representable datasets and this step is crucial for any AI prior to clinical use.
Limited data was available for evaluating the influence of time from stroke onset to scan on AI detection performance. However, data from the one study available suggests caution must be made for scans with a time of onset below 3 h, as it could negatively affect the AI detection performance.
This systematic review is possibly affected by reporting bias from selected outcome reporting and publication bias. Ideally, the QUADAS-AI tool would have been fitting in this context, but it is still under development [74]. Instead, we used the currently available QUADAS-2, which we modified in an effort to address established shortcomings of this tool in the context of evaluating AI [74, 75]. However, it is possible our modifications reduced the validity of QUADAS-2. Lastly, the topic of this systematic review is under rapid development, as illustrated by the fact that a large proportion of the studies included were published within the last three years. Major developments in the field in the near future are foreseeable which will necessitate updates of this meta-analysis.
Conclusion
The current AI detection performance of ischaemic stroke in MRI is usable as a diagnostic test. Further investigation is needed to elucidate AI detection of haemorrhagic stroke. Most AI technologies are based on neural networks. There are reporting gaps, mainly in the reporting of AI model performance and examination, and future AI studies should utilise a reporting guideline to improve validity. The clinical usability is yet to be investigated.
Data availability
Datasheets used for meta-analyses are available upon request from the corresponding author.
Abbreviations
- AI:
-
Artificial intelligence
- AUROC:
-
Area under the receiver operating characteristics curve
- CE:
-
European conformity
- CLAIM:
-
Checklist for artificial intelligence in medical imaging
- CT:
-
Computed tomography
- DWI:
-
Diffusion-weighted imaging
- FDA:
-
Food and drug administration
- FLAIR:
-
Fluid-attenuated inversion recovery
- fMRI:
-
Functional magnetic resonance imaging
- HSROC:
-
Hierarchical summary receiver operating characteristics
- MAS-AI:
-
Model for assessing artificial intelligence in medical imaging
- MI-CLAIM:
-
Minimum information about clinical artificial intelligence modelling
- MRI:
-
Magnetic resonance imaging
- PICOS:
-
Participants-intervention-comparator-outcome-study
- PRISMA:
-
Preferred reporting of items for systematic reviews and meta-Analyses
- PROSPERO:
-
International prospective register of systematic reviews
- QUADAS-2:
-
Quality assessment for diagnostic accuracy studies 2
- ROC:
-
Receiver operating characteristics
- STARD:
-
Standards for reporting of diagnostic accuracy studies
References
Powers WJ, Rabinstein AA, Ackerson T et al (2019) Guidelines for the early management of patients with acute ischemic stroke: 2019 update to the 2018 guidelines for the early management of acute ischemic stroke: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke 50:e344–e418. https://doi.org/10.1161/STR.0000000000000211
Berge E, Whiteley W, Audebert H et al (2021) European Stroke Organisation (ESO) guidelines on intravenous thrombolysis for acute ischaemic stroke. Eur Stroke J 6:I–LXII. https://doi.org/10.1177/2396987321989865
Thomalla G, Simonsen CZ, Boutitie F et al (2018) MRI-Guided Thrombolysis for Stroke with Unknown Time of Onset. N Engl J Med 379:611–622. https://doi.org/10.1056/NEJMoa1804355
Campbell BCV, Ma H, Ringleb PA et al (2019) Extending thrombolysis to 4·5–9 h and wake-up stroke using perfusion imaging: a systematic review and meta-analysis of individual patient data. Lancet 394:139–147. https://doi.org/10.1016/s0140-6736(19)31053-0
Provost C, Soudant M, Legrand L et al (2019) Magnetic resonance imaging or computed tomography before treatment in acute ischemic stroke. Stroke 50:659–664. https://doi.org/10.1161/STROKEAHA.118.023882
Organisation for Economic Co-operation and Development (2022) OECD Stat Health, Paris. https://stats.oecd.org/Index.aspx?ThemeTreeId=9. Accessed 2 June 2022
OECD (2019) Health at a glance 2019. OECD indicators. OECD Publishing, Paris.
Kwee TC, Kwee RM (2021) Workload of diagnostic radiologists in the foreseeable future based on recent scientific advances: growth expectations and role of artificial intelligence. Insights Imaging 12:88. https://doi.org/10.1186/s13244-021-01031-4
Brady AP (2017) Error and discrepancy in radiology: Inevitable or avoidable? Insights Imaging 8:171–182. https://doi.org/10.1007/s13244-016-0534-1
Waite S, Scott J, Gale B, Fuchs T, Kolla S, Reede D (2017) Interpretive error in radiology. AJR Am J Roentgenol 208:739–749. https://doi.org/10.2214/ajr.16.16963
Gupta R, Krishnam SP, Schaefer PW, Lev MH, Gilberto Gonzalez R (2020) An east coast perspective on artificial intelligence and machine learning: part 1: hemorrhagic stroke imaging and triage. Neuroimaging Clin N Am 30:459–466. https://doi.org/10.1016/j.nic.2020.07.005
Gupta R, Krishnam SP, Schaefer PW, Lev MH, Gonzalez RG (2020) An east coast perspective on artificial intelligence and machine learning: part 2: ischemic stroke imaging and triage. Neuroimaging Clin N Am 30:467–478. https://doi.org/10.1016/j.nic.2020.08.002
Zhu G, Jiang B, Chen H et al (2020) Artificial intelligence and stroke imaging: a west coast perspective. Neuroimaging Clin N Am 30:479–492. https://doi.org/10.1016/j.nic.2020.07.001
Karthik R, Menaka R, Johnson A, Anand S (2020) Neuroimaging and deep learning for brain stroke detection—a review of recent advancements and future prospects. Comput Methods Programs Biomed 197:105728. https://doi.org/10.1016/j.cmpb.2020.105728
Jørgensen MD, Antulov R, Hess S, Lysdahlgaard S (2022) Convolutional neural network performance compared to radiologists in detecting intracranial hemorrhage from brain computed tomography: a systematic review and meta-analysis. Eur J Radiol 146:110073. https://doi.org/10.1016/j.ejrad.2021.110073
Murray NM, Unberath M, Hager GD, Hui FK (2020) Artificial intelligence to diagnose ischemic stroke and identify large vessel occlusions: a systematic review. J Neurointerv Surg 12:156–164. https://doi.org/10.1136/neurintsurg-2019-015135
Sheng K, Offersen CM, Middleton J et al (2022) Automated identification of multiple findings on brain MRI for improving scan acquisition and interpretation workflows: a systematic review. Diagnostics 12:1878
Amann J, Vayena E, Ormond KE, Frey D, Madai VI, Blasimme A (2023) Expectations and attitudes towards medical artificial intelligence: a qualitative study in the field of stroke. PLoS One 18:e0279088. https://doi.org/10.1371/journal.pone.0279088
Agarwal S, Wood D, Grzeda M et al (2023) Systematic review of artificial intelligence for abnormality detection in high-volume neuroimaging and subgroup meta-analysis for intracranial hemorrhage detection. Clin Neuroradiol 33:943–956. https://doi.org/10.1007/s00062-023-01291-1
Bivard A, Churilov L, Parsons M (2020) Artificial intelligence for decision support in acute stroke—current roles and potential. Nat Rev Neurol 16:575–585. https://doi.org/10.1038/s41582-020-0390-y
Norgeot B, Quer G, Beaulieu-Jones BK et al (2020) Minimum information about clinical artificial intelligence modeling: the MI-CLAIM checklist. Nat Med 26:1320–1324. https://doi.org/10.1038/s41591-020-1041-y
Page MJ, McKenzie JE, Bossuyt PM et al (2021) The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ 372:n71. https://doi.org/10.1136/bmj.n71
Booth A, Clarke M, Dooley G et al (2012) The nuts and bolts of PROSPERO: an international prospective register of systematic reviews. Syst Rev 1:2. https://doi.org/10.1186/2046-4053-1-2
Methley AM, Campbell S, Chew-Graham C, McNally R, Cheraghi-Sohi S (2014) PICO, PICOS and SPIDER: a comparison study of specificity and sensitivity in three search tools for qualitative systematic reviews. BMC Health Serv Res 14:579. https://doi.org/10.1186/s12913-014-0579-0
Bossuyt PM (2022) Chapter 4: understanding the design of test accuracy studies. Draft version. In: Deeks JJ, Bossuyt PMM, Leeflang MMG, Takwoingi Y, (eds) Cochrane handbook for systematic reviews of diagnostic test accuracy, 2nd edn. The Cochrane Collaboration, London
Deeks JJ, Wisniewski S, Davenport C (2013) Chapter 4: guide to the contents of a Cochrane Diagnostic Test Accuracy Protocol. In: Deeks JJ, Bossuyt PM, Gatsonis C (eds) Cochrane handbook for systematic reviews of diagnostic test accuracy, 1.0.0 edn. The Cochrane Collaboration, London
Mallee WH, Wang J, Poolman RW et al (2015) Computed tomography versus magnetic resonance imaging versus bone scintigraphy for clinically suspected scaphoid fractures in patients with negative plain radiographs Cochrane Database Syst Rev 2015:Cd010023. https://doi.org/10.1002/14651858.CD010023.pub2
Liu J, Zhang J, Wang LN (2018) Gamma aminobutyric acid (GABA) receptor agonists for acute stroke. Cochrane Database Syst Rev 10:Cd009622. https://doi.org/10.1002/14651858.CD009622.pub5
Romion Health (2024) Radiology health AI register 2024. Available via https://radiology.healthairegister.com. Archived URL https://web.archive.org/web/20240318055427/https://radiology.healthairegister.com/. Accessed 18 Mar 2024
Whiting PF, Rutjes AWS, Westwood ME et al (2011) QUADAS-2: a revised tool for the quality assessment of diagnostic accuracy studies. Ann Intern Med 155:529–536. https://doi.org/10.7326/0003-4819-155-8-201110180-00009
Harbord RM, Whiting P (2009) Metandi: meta-analysis of diagnostic accuracy using hierarchical logistic regression. Stata J 9:211–229. https://doi.org/10.1177/1536867x0900900203
Krag CH, Muller FC, Gandrup KL et al (2023) Diagnostic test accuracy study of a commercially available deep learning algorithm for ischemic lesion detection on brain MRIs in suspected stroke patients from a non-comprehensive stroke center. Eur J Radiol 168:111126. https://doi.org/10.1016/j.ejrad.2023.111126
Lee K-Y, Liu C-C, Chen DY-T, Weng C-L, Chiu H-W, Chiang C-H (2023) Automatic detection and vascular territory classification of hyperacute staged ischemic stroke on diffusion weighted image using convolutional neural networks. Sci Rep. 13:404. https://doi.org/10.1038/s41598-023-27621-4
Yang X, Yu P, Zhang H et al (2023) Deep learning algorithm enables cerebral venous thrombosis detection with routine brain magnetic resonance imaging. Stroke 54:1357–1366. https://doi.org/10.1161/STROKEAHA.122.041520
Wu Y, Sun R, Xie Y, Nie S (2023) Automatic alberta stroke program early computed tomographic scoring in patients with acute ischemic stroke using diffusion-weighted imaging. Med Biol Eng Comput 61:2149–2157. https://doi.org/10.1007/s11517-023-02867-2
Bridge CP, Bizzo BC, Hillis JM et al (2022) Development and clinical application of a deep learning model to identify acute infarct on magnetic resonance imaging. Sci Rep. 12:2154. https://doi.org/10.1038/s41598-022-06021-0
Tasci B, Tasci I (2022) Deep feature extraction based brain image classification model using preprocessed images: PDRNet. Biomed Signal Process Control 78:103948. https://doi.org/10.1016/j.bspc.2022.103948
Qiu J, Tan G, Lin Y et al (2022) Automated detection of intracranial artery stenosis and occlusion in magnetic resonance angiography: a preliminary study based on deep learning. Magn Res Imaging 94:105-111. https://doi.org/10.1016/j.mri.2022.09.006
Liu C-F, Hsu J, Xu X et al (2021) Deep learning-based detection and segmentation of diffusion abnormalities in acute ischemic stroke. Commun Med 1:61. https://doi.org/10.1038/s43856-021-00062-8
Nael K, Gibson E, Yang C et al (2021) Automated detection of critical findings in multi-parametric brain MRI using a system of 3D neural networks. Sci Rep. 11:6876. https://doi.org/10.1038/s41598-021-86022-7
Duan Y, Liu L, Wu Z et al (2020) Primary categorizing and masking cerebral small vessel disease based on “deep learning system. Front Neuroinformatics 14:17. https://doi.org/10.3389/fninf.2020.00017
Dorum ES, Kaufmann T, Alnaes D et al (2020) Functional brain network modeling in sub-acute stroke patients and healthy controls during rest and continuous attentive tracking. Heliyon 6:e04854. https://doi.org/10.1016/j.heliyon.2020.e04854
Federau C, Christensen S, Scherrer N et al (2020) Improved segmentation and detection sensitivity of diffusion-weighted stroke lesions with synthetically enhanced deep learning. Radiol Artif Intell 2:1–8. https://doi.org/10.1148/ryai.2020190217
Herzog L, Murina E, Durr O, Wegener S, Sick B (2020) Integrating uncertainty in deep neural networks for MRI based stroke analysis. Med Image Anal 65:101790. https://doi.org/10.1016/j.media.2020.101790
Bizzo B, Bridge C, Gauriau R et al (2019) Deep learning for acute ischemic stroke on diffusion mri: performance analysis in a consecutive cohort. Stroke. https://doi.org/10.1161/str.50.suppl_1.WP78
Uchiyama Y, Yokoyama R, Ando H et al (2007) Improvement of automated detection method of lacunar infarcts in brain MR images. In: conference proceedings: annual international conference of the IEEE Engineering in Medicine and Biology Society, IEEE Engineering in Medicine and Biology Society Conference, Piscataway, pp 1599–1602
Yaman S, Isilay Unlu E, Guler H, Sengur A, Rajendra Acharya U (2023) Application of novel DIRF feature selection algorithm for automated brain disease detection. Biomed Signal Process Control 85:105006. https://doi.org/10.1016/j.bspc.2023.105006
Arnold TC, Baldassano SN, Litt B, Stein JM (2022) Simulated diagnostic performance of low-field MRI: harnessing open-access datasets to evaluate novel devices. Magn Reson Imaging 87:67–76. https://doi.org/10.1016/j.mri.2021.12.007
Eshmawi AA, Khayyat M, Algarni AD, Hilali-Jaghdam I (2022) An ensemble of deep learning enabled brain stroke classification model in magnetic resonance images. J Healthc Eng 2022:7815434. https://doi.org/10.1155/2022/7815434
Guo Y, Yang Y, Cao F et al (2022) A focus on the role of DSC-PWI dynamic radiomics features in diagnosis and outcome prediction of ischemic stroke. J Clin Med 11:5364. https://doi.org/10.3390/jcm11185364
Li J, Cheng L, Chen S et al (2022) Functional connectivity changes in multiple-frequency bands in acute basal ganglia ischemic stroke patients: a machine learning approach. Neural Plast 2022:1560748. https://doi.org/10.1155/2022/1560748
Cetinoglu YK, Koska IO, Uluc ME, Gelal MF (2021) Detection and vascular territorial classification of stroke on diffusion-weighted MRI by deep learning. Eur J Radiol 145:110050. https://doi.org/10.1016/j.ejrad.2021.110050
Cui L, Han S, Qi S, Duan Y, Kang Y, Luo Y (2021) Deep symmetric three-dimensional convolutional neural networks for identifying acute ischemic stroke via diffusion-weighted images. J Xray Sci Technol 29:551–566. https://doi.org/10.3233/XST-210861
Hossain MS, Saha S, Paul LC, Azim R, Suman AA (eds) (2021) Ischemic brain stroke detection from MRI image using logistic regression classifier. In: 2nd international conference on robotics, electrical and signal processing techniques. ICREST, Dhaka
Kadry S, Nam Y, Rauf HT, Rajinikanth V, Lawal IA (eds) (2021) Automated detection of brain abnormality using deep-learning-scheme: a study. 2021 Seventh International Conference on Bio Signals, Images, and Instrumentation (ICBSII). https://doi.org/10.1109/ICBSII51839.2021.9445122
Liu S, Kong K, Yang B, Zhang L (2020) Clinical value of texture analysis for the assistant diagnosis of acute cerebral infarction based on MRI. Basic Clin Pharmacol Toxicol 126:45–46
Nayak DR, Dash R, Majhi B, Pachori RB, Zhang Y (2020) A deep stacked random vector functional link network autoencoder for diagnosis of brain abnormalities and breast cancer. Biomed Signal Process Control 58:101860. https://doi.org/10.1016/j.bspc.2020.101860
Nayak DR, Dash R, Chang X, Majhi B, Bakshi S (2020) Automated diagnosis of pathological brain using fast curvelet entropy features. IEEE Trans Sustain Comput 5:416–427. https://doi.org/10.1109/TSUSC.2018.2883822
Nazari-Farsani S, Karjalainen T, Isojarvi J, Nyman M, Bucci M, Nummenmaa L (2020) Automated segmentation of acute stroke lesions using a data-driven anomaly detection on diffusion weighted MRI. J Neurosci Methods 333:108575. https://doi.org/10.1016/j.jneumeth.2019.108575
Gaidhani BR, Rajamenakshi RR, Sonavane S (eds) (2019) Brain stroke detection using convolutional neural network and deep learning models. In: 2nd International Conference on Intelligent Communication and Computational Techniques. ICCT, Jaipur, pp 242–249
Nayak DR, Dash R, Majhi B, Acharya UR (2019) Application of fast curvelet Tsallis entropy and kernel random vector functional link network for automated detection of multiclass brain abnormalities. Comput Med Imaging Graph 77:101656. https://doi.org/10.1016/j.compmedimag.2019.101656
Ortiz-Ramon R, Moratal D, Makin S et al (2019) Identification of the presence of ischaemic stroke lesions by means of texture analysis on brain magnetic resonance images. Comput Med Imaging Graph 74:12–24. https://doi.org/10.1016/j.compmedimag.2019.02.006
Phan A, Nguyen T, Phan T (eds) (2019) Detection and classification of brain hemorrhage based on hounsfield values and convolution neural network technique. In: IEEE-RIVF International Conference on Computing and Communication Technologies. RIVF, Vietnam, pp 1–7
Saritha M, Paul Joseph K, Mathew AT (2013) Classification of MRI brain images using combined wavelet entropy based spider web plots and probabilistic neural network. Pattern Recognit Lett 34:2151–2156. https://doi.org/10.1016/j.patrec.2013.08.017
Bossuyt PM, Reitsma JB, Bruns DE et al (2015) STARD 2015: an updated list of essential items for reporting diagnostic accuracy studies. BMJ 351:h5527. https://doi.org/10.1136/bmj.h5527
Mongan J, Moy L, Kahn Jr CE (2020) Checklist for artificial intelligence in medical imaging (CLAIM): a guide for authors and reviewers. Radio Artif Intell 2:e200029. https://doi.org/10.1148/ryai.2020200029
Sounderajah V, Ashrafian H, Golub RM et al (2021) Developing a reporting guideline for artificial intelligence-centred diagnostic test accuracy studies: the STARD-AI protocol. BMJ Open 11:e047709. https://doi.org/10.1136/bmjopen-2020-047709
Olthof AW, van Ooijen PMA, Rezazade Mehrizi MH (2020) Promises of artificial intelligence in neuroradiology: a systematic technographic review. Neuroradiology 62:1265–1278. https://doi.org/10.1007/s00234-020-02424-w
Rezazade Mehrizi MH, Mol F, Peter M et al (2023) The impact of AI suggestions on radiologists’ decisions: a pilot study of explainability and attitudinal priming interventions in mammography examination. Sci Rep. 13:9230. https://doi.org/10.1038/s41598-023-36435-3
Fasterholdt I, Kjølhede T, Naghavi-Behzad M et al (2022) Model for assessing the value of artificial intelligence in medical imaging (MAS-AI). Int J Technol Assess Health Care 38:e74. https://doi.org/10.1017/S0266462322000551
Makin SD, Doubal FN, Dennis MS, Wardlaw JM (2015) Clinically confirmed stroke with negative diffusion-weighted imaging magnetic resonance imaging: longitudinal study of clinical outcomes, stroke recurrence, and systematic review. Stroke 46:3142–3148. https://doi.org/10.1161/strokeaha.115.010665
Yu AC, Mohajer B, Eng J (2022) External validation of deep learning algorithms for radiologic diagnosis: a systematic review. Radiol Artif Intell 4:e210064. https://doi.org/10.1148/ryai.210064
Kim DW, Jang HY, Kim KW, Shin Y, Park SH (2019) Design characteristics of studies reporting the performance of artificial intelligence algorithms for diagnostic analysis of medical images: results from recently published papers. Korean J Radiol 20:405–410. https://doi.org/10.3348/kjr.2019.0025
Sounderajah V, Ashrafian H, Rose S et al (2021) A quality assessment tool for artificial intelligence-centered diagnostic test accuracy studies: QUADAS-AI. Nat Med 27:1663–1665. https://doi.org/10.1038/s41591-021-01517-0
Jayakumar S, Sounderajah V, Normahani P et al (2022) Quality assessment standards in artificial intelligence diagnostic accuracy systematic reviews: a meta-research study. NPJ Digit Med 5:11. https://doi.org/10.1038/s41746-021-00544-y
Acknowledgements
We acknowledge Cochrane Denmark & Centre of Evidence-based Medicine Odense (CEBMO) for counselling.
Funding
This study was financed with a grant from Innovation Fund Denmark, which was not involved in the study design, data collection, interpretation of data, or writing of the article. Open access funding provided by University of Southern Denmark.
Author information
Authors and Affiliations
Contributions
All authors provided substantial contributions to the design of the work. JAB, MTE, and BSBR contributed to the data acquisition. JAB performed the analyses and draughting of the manuscript. All authors critically reviewed and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
DG received speaker honoraria from Pfizer and Bristol Myers Squibb outside the submitted work and participated in research outside the submitted work funded by Bayer with funds paid to the institution where he is employed. MN hold shares in Cerebriu. CHK received consulting fees from Cerebriu. CK is the local principal investigator in clinical trials initiated by Bayer. The authors JAB, MTE, OG, FSGH, MVS, MPB, and BSBR declare that they have no competing interests.
Additional information
Publisher’s Note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Authors’ information (optional) Not applicable.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Bojsen, J.A., Elhakim, M.T., Graumann, O. et al. Artificial intelligence for MRI stroke detection: a systematic review and meta-analysis. Insights Imaging 15, 160 (2024). https://doi.org/10.1186/s13244-024-01723-7
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-024-01723-7