Abstract
Traumatic bone marrow lesions (TBMLs) are considered to represent a range of concealed bone injuries, including haemorrhage, infarction, and localised oedema caused by trabecular microfracture occurring in the cancellous bone. If TBMLs are not managed timeously, they potentially cause a series of complications that can lead to irreversible morbidity and prolonged recovery time. This article reviews interesting image findings of bone marrow lesions in dual-energy computed tomography (DECT). In addition to combining the benefits of traditional CT imaging, DECT also reveals and identifies various structures using diverse attenuation characteristics of different radiographic spectra. Therefore, DECT has the capacity to detect TBMLs, which have traditionally been diagnosed using MRI. Through evaluating DECT virtual non-calcium maps, the detection of TBMLs is rendered easier and more efficient in some acute accidents.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Key Points
-
1.
Traumatic bone marrow lesions represent a range of concealed bone injuries.
-
2.
Dual-energy computed tomography and virtual non-calcium imaging have excellent diagnostic ability and proven utility for traumatic bone marrow lesion.
-
3.
Radiologists can benefit from integrating dual-energy computed tomography and virtual non-calcium imaging into workflow.
Introduction
Trauma induces a disruption of marrow trabeculae with leakage of interstitial fluid and haemorrhage to marrow spaces in Traumatic bone marrow lesion (TBML). TBML potentially causes various, severe clinical symptoms, leading to acute pain and joint-function loss, with or without other substantial soft-tissue injuries [1]. Without timely management, it may cause several complications, including dislocation, proteoglycan loss, chondrocyte degeneration, subchondral bone necrosis, and osteoarthritis, which potentially result in prolonged recovery time and irreversible morbidity [2]. In addition, after trauma, these reflect that the presence of TBML should lead to careful inspection and physical examination for other injuries changes to increase the diagnostic accuracy. Therefore, to prevent adverse patient outcomes, accurate and early diagnosis is prerequisite to optimal therapy.
MRI is the preferred imaging modality for diagnosing TBMLs. However, MRI has certain limitations in clinical practice, including pacemakers, claustrophobia, cochlear implants, and patient inability to remain stationary during image acquisition [3]. Conventional CT can detect fractures; however, TBMLs cannot be visualised due to the overlying trabecular bone [1]. By exploiting the photoelectric effect’s energy dependence in different radiographic spectra, dual-energy CT (DECT) facilitates the discrimination of different materials, decomposition of the three materials, and calculation of colour-coded virtual non-calcium (VNCa) images [4]. Therefore, dual-energy CT has enabled the detection of BMLs involving the absence of cortical disruption or with fractures [3,4,5,6,7,8,9].
In this review, we explore DECT’s emerging role in TBML imaging, with special focus on its diagnostic utility in delineating TBMLs [10].
Definition of bone marrow lesion
BML is a common finding on MRI, describing a change in bone marrow signal strength on MRI, with or without low T1-weighted and enhanced signal intensity on fluid-sensitive sequences (T2/proton density with fat suppression and STIR) [11]. Notably, BML is not limited to bone injuries and can occur in infection, ischaemia, migrating osteoporosis, and early osteonecrosis and as a reaction to a tumour or as an idiopathic condition [11]. TBML is a post-traumatic bone marrow lesion, combined with bone marrow oedema, bleeding, cancellous bone trabecular microfracture, interstitial fluid exudation, and extracellular space bleeding, due to acute direct or indirect trauma (e.g. bone contusion), or by overload-induced subacute injury (e.g. stress fracture) [12]. Although TBMLs are often considered benign and self-limiting, they have recently been identified as a useful clinical phenomenon that may inform disease management [1], such as providing a potential target in TBML treatment that may precipitate osteoarthritis [10].
Classification of bone marrow lesions
In 1988, Yao and Lee initially described irregular lesions on MRI in eight patients with acute knee injuries who had normal radiographs [13]. Berger et al. [14] described a series of 14 patients with radiographic occult fractures on MRI in the same year; nevertheless, these lesions were not classified. Bone bruising and occult fractures were separated a few years later [15]. Occult fractures are either radiographically undetectable or present minor abnormalities that are initially overlooked [16]. However, they exhibit MR characteristics remarkably similar to those of bone bruises, with the exception of an adjacent-cortex disturbance [15], whereas bone bruises or TBMLs exclusively involve the bone marrow [16].
Various classification systems have been used in different studies (Table 1). Lynch subsequently developed a three-type classification [17], based on morphology. Type I is described as diffuse inhomogeneous loss of reticular signal intensity on T1-weighted images within the medullary space of the cancellous bone and enhanced signal on sequences T2-weighted; type II lesions are identical to type I lesions; however, they have an interruption in the form of a smooth, black cortical line; type III lesions suggested as a considerable reduction of signal intensity, which was primarily limited to the immediate subcortical region on short TE images. However, intact or disrupted cartilage was not included in this classification. Bohndorf categorised the BMLs with intact (A) and disrupted (B) cartilage by integrating various findings at direct inspection (arthroscopy/arthrotomy) and the MR appearance of acute articular surface lesions, based on radiological and clinical findings [18]. Nevertheless, this classification combined clinical findings using arthroscopy/arthrotomy, which is an invasive event. Costa-Paz analysed BMLs using a three-level grading system, combined with both the appearance and location of BMLs [19]. Type 1: diffuse signal intensity, with change of medullar component; often reticular and distant from articular surface; type 2: localised signal intensity, with contiguity to articular surface; usually crescent in shape; type 3: disruption or depression of articular surface; often associated with type 2 lesions.
Although several authors have attempted to improve these classification systems, Costa-Paz’s classification not only combined the appearance and location of BMLs but also evaluated both bone and cartilage non-invasively. The current studies focus on diagnostic performance of DECT for TBML. There are no studies about DECT for the TBML classification; however, its imaging appearance is similar with MR imaging finding. It is promising for classification of TBML in DECT. Therefore, the classification systems of TBML in MR are helpful to the understanding and diagnosis for DECT classification in TBML.
Radiography
Most fractures can be diagnosed radiographically [20,21,22]. Computer X-ray and digital X-ray photography have improved the imaging quality significantly [23]. However, due to the projection-principle limitation, radiography has low-density resolution and cannot clearly reveal the overlapping and complex bone parts. Therefore, radiography often cannot diagnose TBMLs [24].
Magnetic resonance imaging
TBMLs have widely been reported in the knee [10, 13, 15, 18, 25]. Yao and Lee describe these acute knee injuries as irregular signal on MRI, an unobvious or easily neglected phenomenon on plain radiographs [13]. MRI reveals BMLs as focal-signal abnormalities in the subchondral bone and bone marrow. A typical BML appears as a signal-loss area on T1 images and high signal intensity on T2 images owing to the wounded area’s increased fluid content. The optimal MRIs are produced from STIR sequences, where the signal from normal medullary fat is suppressed, thus highlighting BMLs with increased intensity. Although TBMLs have generally been diagnosed using MRI, which can identify characteristic findings, it necessitates prolonged acquisition times, and patients experiencing pain cannot remain in a fixed position, thus limiting MRI use in trauma settings.
Positron emission tomography (PET)
In a prospective study, Marks et al. [26] suggested that bone scintigraphy can reveal bone injuries, which MRI confirmed as subchondral bone damage in 13 patients. Another study demonstrated that PET revealed several areas with increased tracer uptake that were colocalised by either bone or cartilage damage, thus providing additional information regarding bone marrow injuries [27]. Furthermore, additional morphologic imaging is recommended using 18F-Fluoride PET/MR because it can present BMLs more precisely and provide further diagnostic information at a higher diagnostic certainty [28]. Researchers have concluded that PET is a highly sensitive but moderately specific tool for detecting BMLs, with the drawback of low specificity. Therefore, PET is seldomly used for TBMLs.
Ultrasonography (US)
US can sketch the cortical bone outline and adjacent soft-tissue changes at a fractured site using the high reflectivity at the cortical bone/peri-osseous soft-tissue interface [29]. Ultrasound is useful in bone and cartilage contour examinations when soft tissue surrounding the bone injury is painful and inflamed [30]. Moreover, when trauma history is obscure or a fracture is not suspected clinically, ultrasound can help diagnose occult fractures [31]. Additionally, US is a widely available, dynamic diagnostic imaging technology that is rapidly gaining traction as a cartilage evaluation tool [32]; however, most tibial- and patellar-cartilage parts in the knee joint are imperceptible [33]. Nevertheless, it is not the preferred TBML detection method [30].
Single-energy computed tomography (SECT)
Standard SECT can accurately depict bone and even small fractures. SECT for occult fractures has highly sensitive and negative predictive values [34]. SECT of 0.625 mm axial-slice thickness, it is easy to assess patients with small or occult fractures with clinical suspicion of fracture and negative plain films, improving the time to diagnosis [35]. In particular, MDCT is a safe and appropriate first-line assessment tool for occult or small fractures [35]. Additionally, SECT yields substantial CT information and high resolution. It can perform three-dimensional reconstruction using surface shade display, volume rendering, maximum intensity projection, and other technologies [36]. Moreover, it reveals the fracture by any-plane reconstruction and is unaffected by overlapping shadows. It can clearly display fracture details and internal structure, which is an important means of diagnosing occult fracture. Therefore, SECT is an important and appropriate first-line investigation for early diagnosis of fracture, especially in occult or small fractures. However, SECT does not allow to evaluate bone marrow changes [6], it cannot facilitate TBML evaluation.
DECT
Principle of DECT
DECT’s ability to define and identify diverse body contents based on material degradation has recently increased due to technological advancements. DECT can distinguish different materials because high-density substances, such as iron, calcium, or iodine, exhibit variable attenuation at different X-ray spectrum energy levels at two separate energy levels, while conventional CT scan use a single polychromatic x-ray energy to acquire images with a single peak energy of around 100–120 kV [6, 37]. VNCa-image reconstruction can remove calcium from cancellous bone using a three-material decomposition model [4, 38]. The VNCa image, produced from the data of bone mineral composition removal (comprising calcium), can display the underlying bone marrow. VNCa-image colour coding allows qualitative assessment, while region-of-interest measurements provide quantitative assessment [39]. Consequently, DECT permits the characterisation and distinguishing of various body structures using varied attenuation at different X-ray spectra and allows increased visualisation of bone-marrow-oedema distribution for identifying BMLs. The specificity of DECT was highly dependent on reader experience and the acquisition technique. For reader experience, the specificity of DECT in the diagnosis of TBML was dependent on the experience of readers. Although inter-reader agreement was excellent for DECT-VNCa images, board-certified experienced readers had a higher specificity of 96% compared with trainees (residents or research students) [3]. A larger voltage difference (at least 60) can result in higher sensitivity between low and high kilovoltage for spectral separation [3]. In addition, single-source consecutive DECT showed lower specificity compared with the dual source CT; moreover, fast kilovoltage switching techniques showed similar estimates of diagnostic accuracy as a dual source technique compared with dual-layer DECT [3]. Different studies used different Rel.CM values for diagnosing TBMLs [5, 6, 8, 39, 40]; their results showed that the VNCa image with a Rel.CM value of 1.45 could be an optimal parameter. Therefore, for the evaluation of TBML on DECT in the clinical, we should try to read the images by certified experienced readers instead of trainees. For the sensitivity and specificity, we slightly recommend to use dual source and dual-layer DECT with a larger voltage difference (at least 60) and Rel.CM value of 1.45 can be an appropriate parameter for VNCa post-processing procedure.
Application of DECT
DECT successfully detects TBMLs after acute trauma of the spine, knee, wrist, hip, and ankle in patients with trauma events using the VNCa technique, according to numerous previously published studies [4, 6, 8, 41,42,43,44]. Li’s meta-analysis evaluated the accuracy of DECT-VNCa imaging in detecting TBMLs and revealed DECT’s high sensitivity and specificity for detecting TBMLs; DECT-VNCa imaging performs considerably well in diagnosing TBMLs [45]. DECT is a potentially important future diagnostic modality for evaluating TBMLs.
Vertebral TBMLs
DECT’s advancement has allowed it to directly assess BMLs present in acute fractures through VNCa-technique development, which is comparable to that of MRI [5, 38, 41, 43,44,45,46,47,48,49] (Fig. 1). This potentially enhances the diagnosis of patients with traumatic and osteoporotic fractures.
Yang et al. conducted a meta-analysis of seven studies involving 510 vertebrae, evaluated DECT’s accuracy in detecting TBMLs in patients suffering from vertebral-compression fractures used MRI as the reference standard, and found that the sensitivity, specificity, and AUC value of DECT for detecting TBML were 0.82, 0.98, and 0.965, respectively [41]. Ghazi analysed 17 studies involving 2468 vertebrae in 742 patients with BML on MRI and found DECT to have a high sensitivity, specificity, and AUC, pooled the sensitivity, specificity, and AUC of DECT for vertebral body TBML were 89%, 96%, and 96%, respectively [3]. These findings suggest that DECT offers impressive diagnostic accuracy for TBMLs in vertebrae, resulted a moderate sensitivity and a high specificity for TBML identification, and suggested that positive predictive value is higher than negative predictive value. In the diagnostic performance of quantitative assessment, some studies have some contradictions [38, 43, 44, 48]. Comparing with the qualitative evaluation, the quantitative evaluation has a lower specificity in DECT for TBMLs. Some studies supported that the quantitative evaluation is more dependent on the experience of the readers, complex post-processing technology, and individual patient differences [44, 50]. However, the high diagnostic performance of qualitative assessment is more important because it is more feasible to perform in in trauma settings, instead of quantitative measurement that requires additional time and effort. Since DECT’s high specificity and positive predictive value, the detection of TBML in DECT can help to increase radiologists’ confidence to diagnosis. It allows the detection of BMLs associated with vertebral fractures and may obviate emergency confirmatory MRI. Furthermore, DECT allows TBML detection, even in patients without evident fractures. Therefore, DECT is a promising diagnostic tool for detecting vertebral TBMLs.
Knee TBMLs
DECT exhibits similar diagnostic accuracy in depicting traumatic knee BMLs compared with vertebral TBMLs [8, 9, 39, 51,52,53,54,55] (Fig. 2). Previous TBML studies have concluded that DECT has high diagnostic accuracy, which is comparable to that of MRI.
According to a meta-analysis that used MRI as the reference standard, DECT demonstrates excellent specificity in evaluating TBMLs in patients with acute knee injuries [54]. However, DECT exhibits slightly lower sensitivity in detecting TBMLs than MRI, indicating that when DECT yields negative results in patients presenting symptoms, MRI may be required to further detect occult BMLs [54]. Moreover, several studies that have evaluated patients with acute knee injuries using DECT and MRI suggested that DECT is specific and accurate in detecting TBMLs in adult patients with acute knee injuries. DECT-VNCa reconstructions exhibit superb diagnostic performance in terms of sensitivity, specificity, and accuracy in depicting TBMLs compared with MRI [8, 39, 52, 53]. Furthermore, Booz’s study found DECT colour-coded map visualisation of TBMLs to have great diagnostic accuracy for TBML characterisation owing to its high-resolution and bone window compared with conventional CT images [39]. Moreover, in Foti’s study, DECT images improved the overall accuracy of TBML visualisation in chronic knee injuries [9]. These results confirmed DECT’s favourable diagnostic accuracy in depicting TBMLs around the knee joint both in acute and chronic traumatic situations compared with that of MRI. Ultimately, these results corroborate DECT’s excellent specificity and accuracy in detecting TBMLs in adult patients with suspected bone fractures or symptoms after acute knee injury, especially when MRI is contraindicated or unavailable.
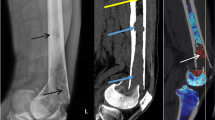
Appendicular-skeleton (excluding knees) TBMLs
Recent studies have primarily investigated the DECT-VNCa technique’s diagnostic ability in detecting TBMLs in the appendicular skeleton, such as in the ankles, wrists, calcaneus, and lower limbs, compared with that of MRI [6, 42, 46, 56,57,58] (Fig. 3). They evaluated DECT’s diagnostic accuracy in detecting TBMLs throughout the appendicular skeleton. In a meta-analysis by Wilson, TBML detection in the appendicular skeleton by DECT was found to have excellent sensitivity, specificity, and AUC values [59]. According to Guggenberger’s study, DECT-reconstructed non-calcium images can help diagnose separate ankle-joint TBMLs with great sensitivity and negative predictive value and intermediate specificity and low positive predictive value [6]. Two studies demonstrated DECT’s utility in reliably identifying BMLs in the trauma wrist [42, 57]. DECT coupled with the VNCa algorithm was used to detect BMLs in wrist fractures and demonstrated reliability and user friendliness, rendering the DECT-VNCa algorithm a promising BML-detection technique in acute carpal trauma, with potential to improve CT’s diagnostic value in this injury type [42, 57]. Another study demonstrated the clinical applicability and high diagnostic accuracy of colour-coded DECT-VNCa reconstructions in the visualisation of calcaneus TBMLs compared with that of MRI [46]. This study demonstrated colour-coded-VNCa reconstruction’s comparability with MRI regarding diagnostic confidence and image noise, revealing no significant difference [46]. Accordingly, DECT exhibited high diagnostic accuracy and confidence in detecting TBMLs in patients with acute trauma injury to the appendicular system. Where MRI is unavailable or contraindicated, DECT can be performed as a feasible alternative for patients with acute trauma and probable BMLs, potentially leading to more efficient patient care after appendicular-skeleton trauma.
Limitations and prospects of DECT for TBMLs
According to previous studies, there are certain limitations to DECT. First, DECT cannot provide enough information to assess soft-tissue injuries, such as those affecting periarticular ligaments, which are frequently injured in acute trauma accidents. Although DECT generally cannot assess soft-tissue injuries accurately, it is an alternative to MRI for patients with BMLs in appropriate circumstances and provides indirect signs that contribute to soft-tissue-injury assessment. Second, patients with negative DECT results and a high bone-abnormality suspicion may still require MRI to detect hidden bone marrow injuries. Third, DECT poses the risk of radiation exposure compared with MRI. Nevertheless, it is valuable in injury characterisation in acute trauma accidents; in addition to enabling the rapid delineation of fracture patterns, it can also detect BMLs without fractures and indirectly identify soft-tissue injuries.
Although MRI is a commonly used technique for BMLs, especially TBMLs, certain difficulties limit its usefulness for BML. MRI takes longer than CT; hence, patients who are in pain generally cannot maintain the same position for a long time. However, DECT has a short scanning time and no contraindications; moreover, it is applicable in emergency settings and involves individual clinical assistance. DECT enables perfect registration due to the almost simultaneous acquisition of different kVp data, which are not affected by breathing and movement artefacts [48]. Therefore, DECT is often the first option due to its increased availability, especially in emergency situations. DECT has shorter imaging duration and is helpful in patients who cannot assume a specific and rigid position. Additionally, TBMLs with small and subtle fractures cannot be discovered easily on MRI [60]. In addition to identifying fracture lines, DECT can also reveal TBMLs.
Consequently, DECT has developed the ability to visualise both BMLs and fracture lines, and it will serve as an alternative to MRI in future studies and applications, where MRI is unavailable or unfeasible. Despite certain limitations, when MRI is not available, DECT remains an excellent alternative to MRI, especially in acute trauma accidents. In TBML assessment, radiologists can benefit from integrating DECT and VNCa imaging into a radiology workflow for TBML portrayal and characterisation in trauma accidents and several acute trauma diagnostic challenges. Moreover, in acute trauma incidents, DECT is a potential ‘one-stop-shop’ evaluation tool, avoiding further patient repositioning and enhancing efficiency.
Conclusion
DECT is a promising clinical application with potential benefits. DECT-VNCa imaging has excellent diagnostic ability and proven utility in TBML detection, and radiologists can improve the detection of TBMLs and TBMLs with subtle and occult fractures. DECT integration into TBML-assessment workflows in acute trauma accidents is set to increase, and DECT is a promising alternative to MRI.
Availability of data and materials
Not applicable.
Abbreviations
- BML:
-
Bone marrow lesion
- DECT:
-
Dual-energy computed tomography
- DECT:
-
Dual-energy CT
- PET:
-
Positron emission tomography
- SECT:
-
Single-energy CT
- STIR:
-
Short-time inversion recovery
- TBML:
-
Traumatic bone marrow lesion
- US:
-
Ultrasonography
- VNCa:
-
Virtual non-calcium
References
Boks SS, Vroegindeweij D, Koes BW et al (2006) Follow-up of occult bone lesions detected at MR imaging: systematic review. Radiology 238(3):853–862. https://doi.org/10.1148/radiol.2382050062
Nakamae A, Engebretsen L, Bahr R et al (2006) Natural history of bone bruises after acute knee injury: clinical outcome and histopathological findings. Knee Surg Sports Traumatol Arthrosc 14(12):1252–1258. https://doi.org/10.1007/s00167-006-0087-9
Ghazi Sherbaf F, Sair HI, Shakoor D et al (2021) DECT in detection of vertebral fracture-associated bone marrow Edema: a systematic review and meta-analysis with emphasis on technical and imaging interpretation parameters. Radiology 300(1):110–119. https://doi.org/10.1148/radiol.2021203624
Pache G, Krauss B, Strohm P et al (2010) Dual-energy CT virtual noncalcium technique: detecting posttraumatic bone marrow lesions–feasibility study. Radiology 256(2):617–624. https://doi.org/10.1148/radiol.10091230
Wang Y, Chen Y, Zheng H et al (2020) Detection of different degree traumatic vertebral bone marrow oedema by virtual non-calcium technique of dual-source dual-energy CT. Clin Radiol 75(2):156 e11-156 e19. https://doi.org/10.1016/j.crad.2019.09.143
Guggenberger R, Gnannt R, Hodler J et al (2012) Diagnostic performance of dual-energy CT for the detection of traumatic bone marrow lesions in the ankle: comparison with MR imaging. Radiology 264(1):164–173. https://doi.org/10.1148/radiol.12112217
Narayanan A, Dettori N, Chalian M et al (2021) Dual-energy CT-generated bone marrow oedema maps improve timely visualisation and recognition of acute lower extremity fractures. Clin Radiol. https://doi.org/10.1016/j.crad.2021.05.004
Cao JX, Wang YM, Kong XQ et al (2015) Good interrater reliability of a new grading system in detecting traumatic bone marrow lesions in the knee by dual energy CT virtual non-calcium images. Eur J Radiol 84(6):1109–1115. https://doi.org/10.1016/j.ejrad.2015.03.003
Foti G, Mantovani W, Faccioli N et al (2020) Identification of bone marrow edema of the knee: diagnostic accuracy of dual-energy CT in comparison with MRI. Radiol Med. https://doi.org/10.1007/s11547-020-01267-y
Punwar S, Hall-Craggs M, Haddad FS (2007) Bone bruises: definition, classification and significance. Br J Hosp Med (London) 68(3):148–151. https://doi.org/10.12968/hmed.2007.68.3.22852
Jelic D, Masulovic D (2011) Bone bruise of the knee associated with the lesions of anterior cruciate ligament and menisci on magnetic resonance imaging. Vojnosanit Pregl 68(9):762–766. https://doi.org/10.2298/vsp1109762j
Marcacci M, Andriolo L, Kon E et al (2016) Aetiology and pathogenesis of bone marrow lesions and osteonecrosis of the knee. EFORT Open Rev 1(5):219–224. https://doi.org/10.1302/2058-5241.1.000044
Yao L, Lee JK (1988) Occult intraosseous fracture: detection with MR imaging. Radiology 167(3):749–751. https://doi.org/10.1148/radiology.167.3.3363134
Berger PE, Ofstein RA, Jackson DW et al (1989) MRI demonstration of radiographically occult fractures: What have we been missing? Radiographics 9(3):407–436. https://doi.org/10.1148/radiographics.9.3.2727354
Vellet AD, Marks PH, Fowler PJ et al (1991) Occult posttraumatic osteochondral lesions of the knee: prevalence, classification, and short-term sequelae evaluated with MR imaging. Radiology 178(1):271–276. https://doi.org/10.1148/radiology.178.1.1984319
Ahn JM, El-Khoury GY (2007) Occult fractures of extremities. Radiol Clin North Am 45(3):561–579. https://doi.org/10.1016/j.rcl.2007.04.008
Lynch TC, Crues JV 3rd, Morgan FW et al (1989) Bone abnormalities of the knee: prevalence and significance at MR imaging. Radiology 171(3):761–766. https://doi.org/10.1148/radiology.171.3.2717748
Roemer FW, Bohndorf K (2002) Long-term osseous sequelae after acute trauma of the knee joint evaluated by MRI. Skeletal Radiol 31(11):615–623. https://doi.org/10.1007/s00256-002-0575-z
Costa-Paz M, Muscolo DL, Ayerza M et al (2001) Magnetic resonance imaging follow-up study of bone bruises associated with anterior cruciate ligament ruptures. Arthroscopy 17(5):445–449. https://doi.org/10.1053/jars.2001.23581
Smith M, Bain GI, Turner PC, Watts AC (2010) Review of imaging of scaphoid fractures. ANZ J Surg 80(1–2):82–90. https://doi.org/10.1111/j.1445-2197.2009.05204.x
Cannon J, Silvestri S, Munro M (2009) Imaging choices in occult hip fracture. J Emerg Med 37(2):144–152. https://doi.org/10.1016/j.jemermed.2007.12.039
Kani KK (2020) Clavicle fractures: review and update for radiologists. Curr Probl Diagn Radiol 49(3):199–204. https://doi.org/10.1067/j.cpradiol.2019.02.010
Hiscox C, LaMothe J, White N, Bromley M, Oddone Paolucci E, Hildebrand K (2015) Diagnosis of occult scaphoid fractures: a randomized, controlled trial comparing bone scans to radiographs for diagnosis. CJEM 16(04):296–303. https://doi.org/10.2310/8000.2013.131074
Najaf-Zadeh A, Nectoux E, Dubos F et al (2014) Prevalence and clinical significance of occult fractures in children with radiograph-negative acute ankle injury. A meta-analysis. Acta Orthop 85(5):518–524. https://doi.org/10.3109/17453674.2014.925353
Rangger C, Kathrein A, Freund MC et al (1998) Bone bruise of the knee: histology and cryosections in 5 cases. Acta Orthop Scand 69(3):291–294. https://doi.org/10.3109/17453679809000933
Marks PH, Goldenberg JA, Vezina WC et al (1992) Subchondral bone infractions in acute ligamentous knee injuries demonstrated on bone scintigraphy and magnetic resonance imaging. J Nucl Med 33(4):516–520
Draper CE, Quon A, Fredericson M et al (2012) Comparison of MRI and (1)(8)F-NaF PET/CT in patients with patellofemoral pain. J Magn Reson Imaging 36(4):928–932. https://doi.org/10.1002/jmri.23682
Rauscher I, Beer AJ, Schaeffeler C et al (2015) Evaluation of 18F-fluoride PET/MR and PET/CT in patients with foot pain of unclear cause. J Nucl Med 56(3):430–435. https://doi.org/10.2967/jnumed.114.150532
Joshi N, Lira A, Mehta N et al (2013) Diagnostic accuracy of history, physical examination, and bedside ultrasound for diagnosis of extremity fractures in the emergency department: a systematic review. Acad Emerg Med 20(1):1–15. https://doi.org/10.1111/acem.12058
Bianchi S (2020) Ultrasound and bone: a pictorial review. J Ultrasound 23(3):227–257. https://doi.org/10.1007/s40477-020-00477-4
Cho KH, Lee SM, Lee YH et al (2010) Ultrasound diagnosis of either an occult or missed fracture of an extremity in pediatric-aged children. Korean J Radiol 11(1):84–94. https://doi.org/10.3348/kjr.2010.11.1.84
Bedewi MA, Elsifey AA, Naguib MF et al (2020) Sonographic assessment of femoral cartilage thickness in healthy adults. J Int Med Res 48(8):300060520948754. https://doi.org/10.1177/0300060520948754
Okano T, Mamoto K, Di Carlo M et al (2019) Clinical utility and potential of ultrasound in osteoarthritis. Radiol Med 124(11):1101–1111. https://doi.org/10.1007/s11547-019-01013-z
Haims AH, Wang A, Yoo BJ et al (2020) Negative predictive value of CT for occult fractures of the hip and pelvis with imaging follow-up. Emerg Radiol. https://doi.org/10.1007/s10140-020-01834-w
Thomas RW, Williams HL, Carpenter EC et al (2016) The validity of investigating occult hip fractures using multidetector CT. Br J Radiol 89(1060):20150250. https://doi.org/10.1259/bjr.20150250
Rehman H, Clement RG, Perks F et al (2016) Imaging of occult hip fractures: CT or MRI? Injury 47(6):1297–1301. https://doi.org/10.1016/j.injury.2016.02.020
Johnson TR, Krauss B, Sedlmair M et al (2007) Material differentiation by dual energy CT: initial experience. Eur Radiol 17(6):1510–1517. https://doi.org/10.1007/s00330-006-0517-6
Foti G, Beltramello A, Catania M et al (2019) Diagnostic accuracy of dual-energy CT and virtual non-calcium techniques to evaluate bone marrow edema in vertebral compression fractures. Radiol Med 124(6):487–494. https://doi.org/10.1007/s11547-019-00998-x
Booz C, Noske J, Lenga L et al (2020) Color-coded virtual non-calcium dual-energy CT for the depiction of bone marrow edema in patients with acute knee trauma: a multireader diagnostic accuracy study. Eur Radiol 30(1):141–150. https://doi.org/10.1007/s00330-019-06304-7
Liang J, Fang Y, Jiang Y et al (2020) Diagnostic accuracy of dual-energy CT virtual non-calcium images with different related contrast material values for the detection of bone marrow edema in knee. Eur J Radiol. https://doi.org/10.1016/j.ejrad.2020.109385
Yang P, Wu G, Chang X (2018) Diagnostic accuracy of dual-energy computed tomography in bone marrow edema with vertebral compression fractures: a meta -analysis. Eur J Radiol 99:124–129. https://doi.org/10.1016/j.ejrad.2017.12.018
Dareez NM, Dahlslett KH, Engesland E et al (2017) Scaphoid fracture: bone marrow edema detected with dual-energy CT virtual non-calcium images and confirmed with MRI. Skeletal Radiol 46(12):1753–1756. https://doi.org/10.1007/s00256-017-2730-6
Petritsch B, Kosmala A, Weng AM et al (2017) Vertebral compression fractures: third-generation dual-energy CT for detection of bone marrow edema at visual and quantitative analyses. Radiology 284(1):161–168. https://doi.org/10.1148/radiol.2017162165
Bierry G, Venkatasamy A, Kremer S et al (2014) Dual-energy CT in vertebral compression fractures: performance of visual and quantitative analysis for bone marrow edema demonstration with comparison to MRI. Skeletal Radiol 43(4):485–492. https://doi.org/10.1007/s00256-013-1812-3
Li M, Qu Y, Song B (2017) Meta-analysis of dual-energy computed tomography virtual non-calcium imaging to detect bone marrow edema. Eur J Radiol 95:124–129. https://doi.org/10.1016/j.ejrad.2017.08.005
Booz C, Noske J, Albrecht MH et al (2019) Traumatic bone marrow edema of the calcaneus: evaluation of color-coded virtual non-calcium dual-energy CT in a multi-reader diagnostic accuracy study. Eur J Radiol 118:207–214. https://doi.org/10.1016/j.ejrad.2019.07.023
Suh CH, Yun SJ, Jin W et al (2018) Diagnostic performance of dual-energy CT for the detection of bone marrow oedema: a systematic review and meta-analysis. Eur Radiol 28(10):4182–4194. https://doi.org/10.1007/s00330-018-5411-5
Wang CK, Tsai JM, Chuang MT et al (2013) Bone marrow edema in vertebral compression fractures: detection with dual-energy CT. Radiology 269(2):525–533. https://doi.org/10.1148/radiol.1312257710.1148/radiology.13122577
Cavallaro M, D’Angelo T, Albrecht MH et al (2022) Comprehensive comparison of dual-energy computed tomography and magnetic resonance imaging for the assessment of bone marrow edema and fracture lines in acute vertebral fractures. Eur Radiol 32(1):561–571. https://doi.org/10.1007/s00330-021-08081-8
Kaup M, Wichmann JL, Scholtz JE et al (2016) Dual-energy CT-based display of bone marrow edema in osteoporotic vertebral compression fractures: impact on diagnostic accuracy of radiologists with varying levels of experience in correlation to MR imaging. Radiology 280(2):510–519. https://doi.org/10.1148/radiol.2016150472
Seo SH, Sohn YJ, Lee CH et al (2013) Dual-energy CT for detection of traumatic bone bruises in the knee joint. J Korean Soc Radiol 69(6):487. https://doi.org/10.3348/jksr.2013.69.6.487
Bjorkman AS, Koskinen SK, Lindblom M et al (2020) Diagnostic accuracy of dual-energy CT for detection of bone marrow lesions in the subacutely injured knee with MRI as reference method. Acta Radiol 61(6):749–759. https://doi.org/10.1177/0284185119877343
Ai S, Qu M, Glazebrook KN et al (2014) Use of dual-energy CT and virtual non-calcium techniques to evaluate post-traumatic bone bruises in knees in the subacute setting. Skeletal Radiol 43(9):1289–1295. https://doi.org/10.1007/s00256-014-1913-7
Wilson MP, Lui K, Nobbee D et al (2021) Diagnostic accuracy of dual-energy CT for detecting bone marrow edema in patients with acute knee injuries: a systematic review and meta-analysis. Skelet Radiol 50(5):871–879. https://doi.org/10.1007/s00256-020-03646-y
Wang M-Y, Zhang X-Y, Xu L, Feng Y, Xu Y-C, Qi L, Zou Y-F. Detection of bone marrow oedema in knee joints using a dual-energy CT virtual non-calcium technique. Clin Radiol. 2019;74(10):815.e1–.e7. https://doi.org/10.1016/j.crad.2019.06.020
Yadav H, Khanduri S, Yadav P et al (2020) Diagnostic accuracy of dual energy CT in the assessment of traumatic bone marrow edema of lower limb and its correlation with MRI. Indian J Radiol Imaging 30(1):59–63. https://doi.org/10.4103/ijri.IJRI_59_19
Ali IT, Wong WD, Liang T et al (2018) Clinical utility of dual-energy CT analysis of bone marrow edema in acute wrist fractures. AJR Am J Roentgenol 210(4):842–847. https://doi.org/10.2214/AJR.17.18673
Koch V, Christoph F, Kasper M (2021) Incremental diagnostic value of color-coded virtual non-calcium dual-energy CT for the assessment of traumatic bone marrow edema of the scaphoid. Eur Radiol 31(7):4428–4437. https://doi.org/10.1007/s00330-020-07541-x.
Wilson MP, Lui K, Nobbee D et al (2020) Diagnostic accuracy of dual-energy CT for the detection of bone marrow edema in the appendicular skeleton: a systematic review and meta-analysis. Eur Radiol. https://doi.org/10.1007/s00330-020-07236-3
Palmer WE, Levine SM, Dupuy DE (1997) Knee and shoulder fractures: association of fracture detection and marrow edema on MR images with mechanism of injury. Radiology 204(2):395–401. https://doi.org/10.1148/radiology.204.2.9240526
Funding
This work is supported by the National Natural Science Foundation of China (81871323, 81901709); the Natural Science Foundation of Guangdong Province of China (2018B030311024, 2019A1515011918); the Scientific Research Project of Hunan Provincial Health Commission (Grant No. 202109010099); the Natural Science Foundation of Hunan Province of China (2021JJ30621).
Author information
Authors and Affiliations
Contributions
QR collated and analysed the data and articles and wrote the original draft of the manuscript. All authors contributed to the editing. SZ and HZ contributed equally to review and edit the manuscript. All authors read and approved the final manuscript.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Consent to publish was obtained from all participates.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ren, Q., Tang, D., Xiong, Z. et al. Traumatic bone marrow lesions in dual-energy computed tomography. Insights Imaging 13, 174 (2022). https://doi.org/10.1186/s13244-022-01312-6
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-022-01312-6