Abstract
Close contacts of individuals with pulmonary tuberculosis are at risk for tuberculosis infection and the development of active tuberculosis. In current contact investigations, immunologic tests (the tuberculin skin test and interferon-gamma release assay) and chest X-ray examinations are used to dichotomize contacts with Mycobacterium tuberculosis infections into those with active (X-ray abnormalities) versus latent tuberculosis (normal radiographs). This article is a critical review of computed tomographic (CT) and 18-fluorodeoxyglucose positron emission tomographic (PET) findings of incipient tuberculosis without X-ray abnormalities based on a systematic literature review of twenty-five publications. The CT and 18-fluorodeoxyglucose PET studies revealed minimal pauci-nodular infiltrations in the lung parenchyma and mediastinal lymph nodes abnormalities with metabolic uptake in approximately one-third of asymptomatic close contacts with negative chest radiographic and bacteriological/molecular results for active tuberculosis. Tuberculosis with minimal changes challenge the validity of simply dichotomizing cases of recent M. tuberculosis infections in contacts depending on the presence of X-ray abnormalities as the recent infections may spontaneously regress, remain stagnant, or progress to active tuberculosis in human and nonhuman primate studies. Whether contacts with tuberculosis with minimal changes are interpreted as having active tuberculosis or latent tuberculosis has clinical implications in terms of specific benefits and harms under the current contact management. Advanced imaging tools may help further stratify contacts intensely exposed to M. tuberculosis on a continuous spectrum from latent tuberculosis to incipient, subclinical and active tuberculosis. Identifying incipient tuberculosis would provide an opportunity for earlier and tailored treatment before active tuberculosis is established.
Similar content being viewed by others
Key points
-
Tuberculosis with minimal CT/PET changes challenges conventional radiographic dichotomization of active versus latent tuberculosis.
-
Pauci-nodular lesions and LN abnormalities are CT and PET findings of incipient tuberculosis.
-
CT and PET abnormalities in incipient tuberculosis may regress, stabilize, or progress.
-
Identifying incipient tuberculosis may provide earlier and tailored treatment before active tuberculosis.
Background
Tuberculosis (TB) is a major global public health problem. According to a 2016 study, latent infections with Mycobacterium tuberculosis (latent tuberculosis infections; LTBIs) affect approximately a quarter of the global population (1.7 billion people) [1]. In 2019, 10 million people developed active TB and 1.2 million died from the disease [2]; these numbers have declined slowly in recent years, but the coronavirus disease 2019 pandemic reversed this trend in 2020: Although new TB case reporting declined by 18%, TB-related deaths increased by one million [3]. In Europe, TB cases continued to decline between 2002 and 2019, but TB incidence varied considerably, from low rates in Western Europe to high rates in Eastern Europe [4]. Most active TB cases develop within 2 years of M. tuberculosis (Mtb) infection, with a small proportion of patients developing active TB later as a result of reactivation of LTBI [5]; This indicates that global TB cases are predominantly caused by recently transmitted Mtb infections [5].
Individuals in close physical contact with pulmonary TB patients are at risk for Mtb infection; thus, an investigation of close contacts is crucial for identifying cases of active TB early and preventing LBTI from progressing to active disease [6]. Indeed, contact investigations are effective for TB control and reducing TB-related mortality in both low-burden and high-burden settings [7, 8]. Contacts with active TB often present clinical symptoms and radiologic abnormalities and are diagnosed based on bacteriological (sputum smear or culture) or molecular (polymerase chain reaction assay) tests. In contrast, LTBI is diagnosed based on a positive tuberculin skin test (TST) or a T-cell-based (interferon-gamma release assay; IGRA) test but with no symptoms and radiologic abnormalities of active TB and negative bacteriological/molecular tests.
Radiologic abnormalities in LTBI are typically assessed using chest X-ray [6], which has limitations in visualizing small or subtle pulmonary lesions. Chest computed tomography (CT) scans can show the fine parenchymal lesions in active and healed TB [9, 10], and 18-fluorodeoxyglucose (18F-FDG) positron emission tomography (PET) scans can provide metabolic information beyond anatomic abnormalities [11, 12], contributing to an improved understanding of TB pathophysiology and manifestations. Healed TB refers to a remote Mtb infection, and the characteristic lung parenchymal CT findings of healed TB are well-established, including calcified or noncalcified granulomas, thin-wall cavities, cicatricial bronchiectasis, and end-stage lung destruction [10]. Healed TB typically has the maximum standardized uptake value below 1.5 on an 18F-FDG PET scan but may have a higher uptake in a minor portion, potentially raising a concern of TB reactivation [12]. In contrast, the CT and 18F-FDG PET findings of recent Mtb infections before the establishment of active disease have been sparsely reported. In this paper, we review the literature on the CT and 18F-FDG PET findings of recent Mtb infections before the establishment of active disease in humans with a representative case presentation, compare those findings with results from nonhuman primate models of Mtb infection, and discuss the implications and potential role of CT and 18F-FDG PET scans in a TB contact investigation.
Main text
Search strategy and study selection
One author (S.H.Y.; 7 years in experience of systematic reviews and meta-analyses, with more than 10 publications) conducted a systematic literature review of the OVID-MEDLINE and EMBASE databases to identify relevant articles. The author used a combination of keywords related to tuberculosis, CT, PET, and contact/outbreak/tracing/screening/latent up to October 25, 2021. This search was limited to literature with English titles and abstracts and was supplemented by screening the bibliographies of the retrieved articles and review articles.
We applied the following criteria for study selection: (a) prospective or retrospective human studies reporting adult or child contacts who were recently exposed to patients with pulmonary TB; (b) no symptoms, signs, or radiographic abnormalities suspicious for active TB; (c) a chest CT or 18F-FDG PET scan was performed in contact investigations. We excluded studies that used CT or PET scans (a) to evaluate contacts clinically or radiographically suspected of active TB in contact investigations, (b) to evaluate extrapulmonary TB in patients with active TB, (c) to identify remote TB infections (e.g., healed TB) in patients who were planned to receive immunosuppressive agents (e.g., for rheumatic diseases or transplantation), and (d) to screen for incidental TB (e.g., pre-employment or health worker screening) regardless of recent TB exposure.
Included studies
Of 1638 publications identified in the initial database search, 25 articles studies have applied chest CT, 18F-FDG PET/CT, or magnetic resonance imaging (MRI) to evaluate asymptomatic close contacts with pulmonary TB patients and normal radiographs (Table 1) (Additional file 1: Fig. 1): 21 CT studies [13,14,15,16,17,18,19,20,21,22,23,24,25,26,27,28,29,30,31,32,33], two 18F-FDG PET/CT studies [34, 35], and two PET/MR studies [36, 37]. Seventeen of the 25 studies were conducted in Asia, followed by Europe. The median number of contacts undergoing advanced imaging was relatively small, at 32. Twelve studies examined children to adolescents [13,14,15,16, 18, 21, 23,24,25, 27, 28, 30], while the other studies included adults. One study was conducted on contacts infected with HIV [35], while the other 24 studies were conducted in immunocompetent contacts. Four studies partly [25, 29] or entirely [23, 26] included close contacts with drug-resistant TB. Bacterial and molecular testing with sputum or other specimens (e.g., gastric aspirates) generally yielded a low positivity rate in contacts with minimal CT or PET abnormalities, reflecting a low bacillary burden (Table 1).
The median prevalence of minimal CT and/or PET abnormalities was 33.0%, but the range varied substantially from 3 to 100%. The wide range of prevalence may have resulted from differences in study populations, (including how to define close contacts having a risk for recent TB infections), the exposure intensity and infectivity of the index pulmonary TB case (more intensive exposures can lead to a higher prevalence), imaging modalities (lung parenchymal abnormalities on non-enhanced chest CT versus lung parenchymal and mediastinal and/or extrapulmonary abnormalities on contrast-enhanced chest CT or 18F-FDG PET-CT or MR), and definitional criteria for interpreting radiologic or metabolic abnormalities on imaging modalities.
CT and PET findings of recent TB infections in humans
Delacourt et al. [13] first used chest CT scans to evaluate children suspected of having been recently infected with TB without clinical and radiographic abnormalities. Among 15 children, nine (60%) had enlarged right paratracheal and hilar lymph nodes (LNs) without lung parenchymal lesions. Similarly, Durán et al. [14] reported enlarged mediastinal LNs (14 of 22 children) and peripheral lung infiltrations (4 of 22 children) in asymptomatic children with TB infections and normal radiographs, but there were no detailed descriptions of the parenchymal infiltrations. Katakura et al. [15] and Yoshiyama et al. [17] elaborated on morphologic findings of lung parenchymal abnormalities on CT images. Most CT abnormalities were a few small nodules smaller than 1 cm or micronodular infiltrations in a limited number of peripheral secondary pulmonary lobules, preferentially in the upper lobes (Fig. 1a, b). Similar morphologic descriptions of CT or MRI findings could be found in some other studies that provided sufficient information on morphologic characteristics [20, 21, 26, 29, 31].
Representative CT images showing dynamics of recent tuberculosis infection in a 33-year-old male contact of a patient with infectious multi-drug resistant tuberculosis. a, b Baseline CT images show a nodular consolidation (black arrow) and micronodules (black arrowhead) in two secondary pulmonary lobules in the apicoposterior segment of the left upper lobe (a). Another minimal pauci-nodular infiltration is noted in the adjacent subsegmental lobules (black arrowhead) (b). Bacteriologic/molecular tests of bronchoscopic alveolar lavage fluid were negative. The patient was observed without treatment. c, d Decreases in the previous pauci-nodular infiltrations are shown on follow-up CT images 14 months after the baseline CT examination. Sputum smear and culture were negative. e, f Eighteen-month follow-up CT images show new nodular consolidation and adjacent pauci-nodular infiltrations (white arrowheads) from one of the shrunken nodules (e, f), while another nodule remains stable (black arrow) (e; variable changes among lesions within a host). The close contact denied any symptoms and signs. Bacteriologic/molecular tests of bronchoscopic alveolar lavage fluid were negative. However, radiologic progression was regarded as indicating active tuberculosis, leading to the subsequent initiation of anti-multidrug resistant tuberculosis treatment. g, h Follow-up CT images 5 months after treatment show decreases in the previous nodular lesions with a few residual small nodules (black arrow and white arrowhead)
PET imaging visualized increased metabolic uptake in the lung parenchyma with or without identifiable lesions, and those findings were frequently accompanied by increased metabolic uptake in LNs confined to the hilum and mediastinum [34,35,36,37]. Interestingly, the involved mediastinal LNs tended not to be sufficiently enlarged to be detected on CT in adults, while children frequently had enlarged mediastinal LNs with or without necrosis [13,14,15, 21, 23, 28].
Follow-up of CT and PET findings of recent TB infections in humans
When CT or PET abnormalities were identified, most of the studies initiated full regimens of anti-TB medication solely based on radiologic or metabolic abnormalities without bacteriological/molecular test positivity for active TB. Contacts with minimal CT or PET abnormalities were treated successfully, including a treatment success rate (successful treatment completion with or without bacteriological evidence of success [38]) of 100% in twenty-two contacts younger than 18 years exposed to multi- or extensively drug-resistant TB [25]. There were two similarly treated contacts exposed to multi-drug resistant TB in the literature [23, 26].
It is rarely possible to prospectively monitor how untreated active pulmonary TB first manifests after infection and changes at an incipient stage in humans. Observing patients newly infected with Mtb without providing treatment may be controversial, as LTBI treatment effectively prevents progression to active disease in drug-sensitive or multidrug-resistant TB [39], although close regular monitoring can allow early detection of progressing active disease without LTBI treatment. Likewise, it would be unethical to acquire lung tissues for investigational purposes in these infected but asymptomatic patients. Eight studies reported follow-up data of minimal radiologic and metabolic abnormalities without anti-TB treatment [26, 31, 34, 35]: six studies applied LTBI treatment to in part or entire study populations [18, 30, 33,34,35,36], while two studies reported findings in patients who did not receive any treatment [26, 31].
The first follow-up observations of minimal abnormalities were made using 18F-FDG PET scans in 35 HIV-infected contacts who received LTBI treatment using isoniazid monotherapy [35]. Among them, 10 contacts had normal scans and 25 had baseline CT abnormalities, including 9 with infiltrates and/or fibrotic scars, 1 with hematogenous TB spread, and 15 with nonspecific discrete nodules. The authors regarded the 10 contacts with pulmonary infiltrates or hematogenous TB spread in the lung parenchyma as having minimal abnormalities. Hypermetabolism in mediastinal LNs was noted in 10 contacts with minimal abnormalities and 6 of 25 contacts without abnormalities. During a 6-month follow-up, 4 of these 10 contacts progressed to have culture-proven (n = 2) or clinically deteriorated (n = 2) TB, whereas TB did not develop in the remaining 25 contacts. With the exception of 4 patients who developed TB disease, 6-month follow-up PET/CT scans revealed that isoniazid monotherapy decreased pre-existing CT abnormalities in all six contacts with minimal abnormalities and metabolic LN uptake in 1 contact without parenchymal abnormalities [35]. Similarly, asymptomatic hypermetabolism of mediastinal LNs based on 18F-PET/CT findings [34] or pauci-nodular lesions [30, 33] decreased with LTBI treatment.
Another follow-up study performed submillisievert CT scans in 6 immunocompetent close contacts with multidrug-resistant TB [26] when standardized LTBI treatment was not well established. All the contacts were asymptomatic with normal radiographs, and half of the contacts were positive for both TST and IGRA. CT scans showed a minimal extent of small noncalcified nodular infiltrations in two contacts, but they had contradictory courses: one contact developed active multidrug-resistant TB shortly thereafter, while the lesion in the other contact regressed spontaneously. A few similar cases with minimal abnormalities progressing into active TB were reported in contacts who denied LTBI treatment [30, 33]. In the contrary, spontaneous regression of noncalcified nodules on CT scans was also noted in one prospective investigation of seventeen close contacts without LTBI under close regular monitoring [31].
As an example of the dynamic changes in minimal radiologic abnormalities, we present the case of a 33-year-old male close contact (Fig. 1), The contact had worked in the same office with a patient with multi-drug resistant TB for 1 year and had smoked cigarettes for 10 years without any comorbidities. He denied any symptoms and signs of active TB. In a contact investigation, TST and IGRA were positive, and sputum smear and culture were negative. Chest CT was conducted to evaluate an equivocal small nodular opacity on a chest radiograph. Baseline CT images (Fig. 1a, b) showed a nodular consolidation and a few micronodules in the apicoposterior segment of the left upper lobe. Bronchoscopy was performed, and bacteriologic/molecular tests of bronchoscopic alveolar lavage fluid were negative. The patient was observed without treatment. On the first follow-up CT scan (Fig. 1c, d; 14 months after baseline), the previous pauci-nodular infiltrations decreased, but a residual nodule was present. He visited our hospital for a second opinion, and the second set of follow-up CT images (Fig. 1e, f; 18 months after baseline) showed new nodular consolidation and adjacent pauci-nodular infiltrations from one of the shrunken nodules, while another nodule remained stable, indicating that lesions within a single host may show variable changes. He still denied any symptoms and signs. Bacteriologic/molecular tests of the sputum and bronchoscopic alveolar lavage fluid were negative. However, radiologic progression was regarded as indicating active TB, leading to the subsequent initiation of anti-multidrug resistant TB treatment. The third set of follow-up CT images (Fig. 1g, h; 5 months after treatment and 23 months after baseline) showed reductions in the previous nodular lesions with a few residual small nodules, radiologically similar to healed TB with negligible sequelae. Two additional cases (Figs. 2 and 3) also illustrate that active TB developed without apparent signs or symptoms or positive microbiologic tests, but CT detected the changes of incipient TB, indicating progression to active disease.
Representative CT images showing incipient TB progressing into active tuberculosis disease in a 52-year-old healthy male. a A screening CT image shows a small single incidental nodule in the right upper lobe (black arrow). b A follow-up CT image 20 months later reveals a few additional micronodules (black arrowheads) in a secondary pulmonary lobule around the small pre-existing nodule (black arrow). The patient denied any symptoms and signs and had negative sputum smear and culture tests. c The next follow-up CT image 24 months later shows the increasing size and number of the nodule (black arrow) and micronodules (black arrowheads) in the right upper lobe. The patient still denied any symptoms and signs. The sputum smear was negative, and Mycobacterium tuberculosis was confirmed on sputum culture. The patient had a 6-month standard anti-tuberculosis medication and healed without sequelae
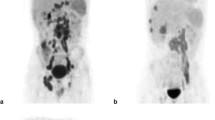
Representative CT and 18-fluorodeoxyglucose PET images showing incipient TB progressing into active tuberculosis disease in a 60-year-old female with malignancy. a, b CT and PET images for metastasis work-up shows a small single incidental nodule with subtle hypermetabolism in the left lobe lobe (black arrow). There was no metabolic uptake in mediastinal lymph nodes. (c) A follow-up CT image 6 months later reveals the increasing size of the nodule with micronodular infiltration (black arrow). The patient still denied any symptoms and signs. The sputum smear and culture was negative for Mycobacterium tuberculosis. The specimen of percutaneous transthoracic lung biopsy turned to be chronic granulomatous inflammation with necrosis, consistent with active tuberculosis disease
In summary, CT and PET scans showed incipient minimal pauci-nodular infiltration in the lung parenchyma with metabolic uptake in the infiltrate and mediastinal LNs in approximately one-third of asymptomatic close contacts with negative chest radiographic and bacteriological/molecular results for active TB. Despite limited observations, these contacts may show various changes during follow-up without treatment. However, the considerable limitations in comprehensively elucidating the natural course of untreated minimal radiologic or metabolic abnormalities make it necessary to refer to the natural course of Mtb infections in nonhuman primates.
Histopathologic, CT, and PET Findings of recent TB infections in nonhuman primates
One of the major areas of progress in TB animal models has been the establishment of LTBI in cynomolgus macaques [40]. Cynomolgus macaques are 40- to 50-cm primates that are relatively resistant to M. tuberculosis compared to other species used for TB research [41] in that these macaques develop the full range of human Mtb infection outcomes, from LTBI to severe active disease. A bronchoscopic instillation of low-dose (< 102 colony forming unit) virulent M. tuberculosis in cynomolgus macaques results in an approximately even distribution of active TB and LTBI [41]. Cynomolgus macaques with LTBI were found to have no clinical signs of disease for at least 6 months after infection, with normal chest radiographs. Necropsies of macaques classified as LTBI revealed a limited number of small granulomas in the lung parenchyma with corresponding mediastinal lymphadenopathy, including a granuloma in a mediastinal LN, in some of the animals [42]. The granulomas showed a histologic spectrum from caseous granulomas with mineralization and/or collagenous materials to non-necrotizing sclerotic granulomas and completely fibrotic granulomas with an admixture of amorphous calcification and fibrotic tissues. Although it is difficult to follow infected macaques for long periods of time due to space constraints in biosafety level3 facilities, macaques with LTBI can be stable up to 20 months after infection. However, some macaques with LBTI progressed to active TB during follow-up [43]. Longitudinal monitoring of LTBI progression using 18F-FDG PET/CT scans showed varying fates of granulomas when over the course of Mtb infection [44]. Each lung parenchymal granuloma in LTBIs was typically initiated by a single bacterium and could spontaneously regress, persist, progress, or newly appear in a single infected host. Thoracic LN involvement can also be tracked in macaques by PET/CT imaging [45]. One or more mediastinal LNs become apparent by PET/CT in macaques within 4 weeks of infection and granulomas are often found in LNs at necropsy at multiple time points. In fact, LNs are a site for bacterial persistence in macaques [46].
In cynomolgus macaque models, recent Mtb infection may cause a few subcentimeter granulomas beyond the radiographic resolution and involve thoracic LNs, and the granulomas show lesion-by-lesion patterns of dynamic change, including spontaneous resolution, stabilization, and progression to active disease.
Interpretation of minimal CT or PET abnormalities in current contact investigations
TB is a continuum encompassing LTBI, incipient, subclinical TB, and active TB [47, 48] (Fig. 4), and subclinical TB can have X-ray abnormalities or microbiological evidence of active, viable M. tuberculosis without symptoms suggestive of active TB disease [47]. Minimal CT or PET abnormalities in asymptomatic close contacts without X-ray abnormalities correspond to incipient TB, which slowly and intermittently replicates. In current contact investigations, the minimal CT or PET abnormalities can be interpreted as either foreshadowing active TB or undetermined latent TB. The former interpretation necessitates anti-TB medication, whereas the latter interpretation requires LTBI management. In the latter interpretation, clinical or radiologic changes during follow-up can differentiate progressing active TB from stagnant or regressing latent TB.
Both interpretations have specific benefits and harms (Table 2). Labeling patients as having active TB, followed by anti-TB treatment, can prevent early undetermined cases from progressing to active TB and curtail TB transmission. However, active TB could be over-diagnosed [49, 50], and LTBI patients may receive unnecessary anti-TB treatment, even though patients may have a chance of spontaneous resolution with LTBI treatment. On the contrary, labeling patients as having latent TB, followed by monitoring, may miss the chance for earlier treatment and blockage of subsequent TB transmission or place contacts at risk of acquiring resistance to LTBI drugs [51] (although the risk is very low), if cases progress to active TB. Classifying these cases as latent TB rather than active TB seems more conventional and consistent with the results of the current contact investigations using X-ray examinations. However, categorizing these cases as active disease may help control TB outbreaks in crowded places such as prisons, military barracks, or quarantine asylums where TB can be transmitted massively in a short period and should be controlled without delay.
Potential role of CT and PET imaging in TB contact investigations as continuum disease
A potential advantage of CT and 18F-FDG PET imaging in TB contact investigations is that these modalities may enable earlier detection of active TB (i.e., before it becomes full-blown) in patients with normal radiographs requiring anti-TB medication and further stratification of contacts with recent LTBI who are at the higher risk for developing active TB (minimal abnormalities) from those who are less likely to develop (no abnormalities) (Fig. 5).
The recommended US Centers for Disease Control and Prevention treatment regimens for drug-sensitive LTBIs include 3-month once-weekly isoniazid plus rifapentine, 4-month daily rifampin, and 3-month isoniazid plus rifampin with alternative options of daily isoniazid for 6 or 9 months [52]. All three regimens showed odd ratios of 0.25–0.36 against developing active TB compared to no treatment [52]. Multidrug-resistant LTBI treatment also provides a relative risk reduction against developing active TB by 90%, although the LTBI treatment regimen has not been standardized [53].
LTBI treatment is initiated for close contacts based on the result of TST and/or IGRA positivity. The positive predictive values of TST and IGRA for developing active TB are limited to an average of 2.7% and 1.5% over a 2-year period after TB infection, respectively [54], suggesting that narrower criteria are needed to identify contacts at high risk for developing TB. Recently introduced whole-blood transcriptional signatures are a promising tool to improve prediction, but their positive predictive values were 6.8–9.4% over 2 years and 11.2–14.4% over 3 months based on a pre-test probability of 2% [55]. The 2-year positive predictive values did not meet the World Health Organization (WHO) target for predicting progression from TB infection to active disease, although the 3-month result exceeded the minimum of the WHO target [56].
Currently, radiographically-negative asymptomatic cases with incipient TB receive LTBI treatment, as they are classified as having latent TB due to normal X-ray findings. In a small series of HIV-infected contacts, TB progression exclusively occurred in contacts with minimal CT or PET abnormalities [35]. Greater bacterial burdens place patients at a higher risk for progression, and the size and metabolic uptake of abnormalities can reflect the quantity of bacilli and associated inflammatory burden [57, 58]. Taken together, close contacts with minimal CT or PET abnormalities may have a higher risk for TB progression than those without such abnormalities.
Treatment initiation for incipient TB with a low bacillary burden may be a potential way to improve the treatment outcomes of TB [59, 60] and reduce the probability of acquiring drug resistance [61]. This may be particularly beneficial for close contacts with multi- or extensively drug-resistant TB that needs relatively long treatment but is less likely to respond to treatment when active TB is established [25, 62]. Since these minimal CT and PET abnormalities pathologically occupy a position between LTBI and active TB, treatment may also be tailored by introducing a shorter abbreviated regimen, as indicated by the recent results of the SHINE (Shorter Treatment for Minimal Tuberculosis in Children) trial reporting non-inferiority of 4 months of treatment to the standard 6-month treatment regimen for non-severe TB [63].
CT or PET imaging in TB contact investigations may further benefit immunocompromised contacts (i.e., those with HIV) or contacts suspected of having intense TB exposures [64] who are at higher risk for TB infection and active disease [65]. Immunocompromised hosts with active TB can have normal radiographs in up to 10–40% of cases, and often have mediastinal lymphadenopathy or extrapulmonary diseases that can only be evaluated to a limited degree using chest radiographs [66]. Furthermore, miliary TB relatively frequently develops in immunocompromised hosts, but 59 to 69% of miliary TB cases are detectable on chest radiographs [67]. If minimal CT or PET abnormalities are shown in immunocompromised contacts, labeling these cases as active disease may be more suitable for immunocompromised or immunosuppressed contacts, since that they have a higher chance of TB progression [6].
Practical considerations of CT and PET imaging in TB contact investigations
Chest CT and 18F-FDG PET scans are advanced imaging tools to evaluate recent TB infections, but before use, practitioners should rigorously assess whether the use of advanced imaging tools will add value to the contact investigation. The current contact investigation and LTBI treatment methods are effective for TB control, and advanced imaging tools will be worthless in most situations if the tools are used indiscriminately. There are two fundamental points to consider: (1) the risk of TB infection and developing active TB and (2) the probability of active TB manifesting as normal radiographs. If the risk is not sufficiently intense (e.g., in a mass screening context), most examinations will not additionally depict changes from incipient TB to active TB beyond what is portrayed by X-ray examinations, as TB disease infrequently occurs and progresses [29, 50, 68, 69]. TB more frequently manifests with normal radiographs in immunocompromised contacts or children. Esmail’s study on HIV contacts using 18F-FDG PET/CT is a representative example of how advanced imaging can add value to contact investigations [35].
Each modality has its own advantages and disadvantages (Table 3). Chest CT radiation is a matter of concern, but it can be minimized to be comparable to the doses of chest frontal and lateral radiographs for evaluating TB lesions [26, 31, 70]. As an alternative imaging modality, 18F-FDG PET may be considered, but it can deliver a greater radiation dose than chest CT, potentially raising the risk of cancer [71, 72]. Chest CT scans are much more broadly implemented, are less expensive, faster obtainable, and may be more cost-effective [73] than 18F-FDG PET scans. Chest CT scans can detect incipient pulmonary TB and intrathoracic extrapulmonary TB (TB pleurisy and enlarged TB lymphadenitis), but cannot cover extrathoracic TB diseases, which is evaluable by 18F-FDG PET scans [74]. Nevertheless, incipient TB primarily manifests in the thorax [75], and even in cases with extrapulmonary TB, TB pleurisy comprises more than half of extrapulmonary TB [76]. Therefore, chest CT scans are a more reasonable and practical modality in most contact investigations than 18F-FDG PET scans may be considered in contacts at risk for a higher chance of extrapulmonary TB, such as HIV-infected persons with low CD4 counts [77].
In most of the included studies, radiologists evaluated radiologic or metabolic abnormalities subjectively without pre-specified definition (Additional file 1: Table 1), demanding the necessity for standardized definitional criteria. CT size criteria for assessing enlarged mediastinal LNs in children varied in the relevant studies [78], and LNs with similar metabolic uptake on an 18F-FDG PET scan may be less specific in TB-endemic areas than in non-TB-endemic areas [79]. Furthermore, CT or PET findings of incipient TB are not specific for TB in 100%, demanding the exclusion of other alternative diagnoses [80, 81]. Lastly, it has not been established which findings should be called minimal CT or 18F-FDG PET parenchymal abnormalities with an undetermined fate and which findings are suggestive of irreversible progression to active TB. At a minimum, a thick-walled cavity is a hallmark of active TB [82], although a thin-walled cavity may present in both active and healed TB [10]. According to the modern understanding of TB pathology in humans [83], asymptomatic obstructive bronchioles and associated lobular pneumonia seem to be a key process in establishing active TB, but spontaneous resolution occurs in 95% of cases before caseation, while the remaining 5% of cases evolve into caseous pneumonia, the irreversible tipping point. Caseous obstruction of bronchioles manifests as the tree-in-bud sign [84, 85]; therefore, the overt tree-in-bud sign on CT images also may be regarded as indicating active TB.
We suggest that minimal parenchymal CT abnormalities can be morphologically defined as pauci-nodular lesions with five or fewer small nodules or micronodules confined to a limited number of subsegmental secondary pulmonary lobules without overt cavities or tree-in-bud manifestations. Our provisional definition needs validation but will help investigate incipient TB on chest CT scans with uniform criteria. The number of studies seems too limited to suggest any provisional criteria for LN or metabolic abnormalities of incipient TB so far.
Limitation of current understanding and future direction
A few limitations exist in the current radiologic and metabolic understanding of incipient TB. The sensitivity and specificity of chest CT and 18F-FDG PET scans for incipient TB. remain unclear yet. It is challenging to set a reference for assessing diagnostic accuracy: tools for confirming incipient TB are lacking, and minimal radiologic and metabolic abnormalities in TB contact investigations were typically regarded as active TB in the literature. Progression into active TB without treatment or regression by treatment may be indirect evidence for incipient TB, but few studies had an observation during follow-up. Furthermore, incipient TB. can naturally undergo a dynamic process without treatment, making the assessment of diagnostic accuracy more difficult.
The knowledge gap will be overcome by studies evaluating the diagnostic accuracy of advanced imaging modalities with predefined radiologic and metabolic criteria for incipient TB.. Prospective studies are also needed to examine the value of differing management based on a TB spectrum according to the presence of radiologic and metabolic abnormalities. More specifically, it is demanding to test whether adding to chest CT scans to the current contact investigation can help more effectively find active TB manifesting as normal radiographs in immunocompromised hosts and TB with minimal changes. Incipient TB. may have a higher chance for progression than latent TB but a higher chance for treatment success than active TB. In particular, it is crucial to systematically examine whether advanced imaging tools can prompt the treatment of drug-resistant TB at an earlier stage with a lower bacillary burden.
Conclusions
Chest CT and 18F-FDG PET examinations in TB contact investigations can depict minimal pauci-nodular infiltrations in the lung parenchyma and metabolic uptake in the opacity and mediastinal LNs, in patients without any symptoms, X-ray abnormalities, or bacteriological/molecular evidence of active TB. Despite the paucity of follow-up data, human and nonhuman primate studies have found that such abnormalities may spontaneously regress, remain stagnant, or progress to active TB, and contacts with such abnormalities have a higher risk for progression than those without any abnormalities. In a contact investigation where the risk for TB infection and developing active TB is intense and active TB is more likely to manifest with normal radiographs, chest CT and 18F-FDG PET examinations may help further stratify contacts recently infected with M. tuberculosis along a continuous spectrum from latent tuberculosis to incipient, subclinical and active TB. In most contact investigations, a chest CT scan is preferable over an 18F-FDG PET scan, considering the accessibility, cost, and radiation dose. Identifying incipient TB would provide an opportunity for earlier and tailored treatment before active TB is established.
Availability of data and materials
Data sharing is not applicable to this article as no datasets were generated or analyzed in the current review.
Abbreviations
- 18F-FDG:
-
18-Fluorodeoxyglucose
- CT:
-
Computed tomography
- IGRA:
-
Interferon-gamma release assay
- LN:
-
Lymph node
- LTBI:
-
Latent tuberculosis infections
- MRI:
-
Magnetic resonance imaging
- Mtb:
-
M. tuberculosis
- PET:
-
Positron emission tomography
- TB:
-
Tuberculosis
- TST:
-
Tuberculin skin test
References
Houben RM, Dodd PJ (2016) The global burden of latent tuberculosis infection: a re-estimation using mathematical modelling. PLoS Med 13:e1002152
Cilloni L, Fu H, Vesga JF et al (2020) The potential impact of the COVID-19 pandemic on the tuberculosis epidemic a modelling analysis. EClinicalMedicine 28:100603
Organization GWH (2021) Global tuberculosis report 2021
European Centre for Disease Prevention and Control WROfE (2021) Tuberculosis surveillance and monitoring in Europe 2021–2019 data. WHO Regional Office for Europe, Copenhagen. https://doi.org/10.2807/ese.19.11.20741-en
Behr MA, Edelstein PH, Ramakrishnan L (2018) Revisiting the timetable of tuberculosis. BMJ 362:k2738
National Tuberculosis Controllers A, Centers for Disease C, Prevention (2005) Guidelines for the investigation of contacts of persons with infectious tuberculosis. Recommendations from the National Tuberculosis Controllers Association and CDC. MMWR Recomm Rep 54:1–47
Velen K, Shingde RV, Ho J, Fox GJ (2021) The effectiveness of contact investigation among contacts of tuberculosis patients: a systematic review and meta-analysis. Eur Respir J. https://doi.org/10.1183/13993003.00266-2021
Fox GJ, Barry SE, Britton WJ, Marks GB (2013) Contact investigation for tuberculosis: a systematic review and meta-analysis. Eur Respir J 41:140–156
Lee KS, Im JG (1995) CT in adults with tuberculosis of the chest: characteristic findings and role in management. Am J Roentgenol 164:1361–1367
Kim HY, Song KS, Goo JM, Lee JS, Lee KS, Lim TH (2001) Thoracic sequelae and complications of tuberculosis. Radiographics 21:839–858 (discussion 859-860)
Goo JM, Im JG, Do KH et al (2000) Pulmonary tuberculoma evaluated by means of FDG PET: findings in 10 cases. Radiology 216:117–121
Jeong YJ, Paeng JC, Nam HY et al (2014) (18)F-FDG positron-emission tomography/computed tomography findings of radiographic lesions suggesting old healed tuberculosis. J Korean Med Sci 29:386–391
Delacourt C, Mani TM, Bonnerot V et al (1993) Computed tomography with normal chest radiograph in tuberculous infection. Arch Dis Child 69:430–432
Gómez-Pastrana Durán D, Caro Mateo P, Torronteras Santiago R et al (1996) Computed tomography and polymerase chain reaction in tuberculosis infection in childhood. Arch Bronconeumol 32:500–504
Katakura S, Imagawa T, Ito S et al (1999) Computed tomography with normal chest radiography in childhood tuberculosis. Kansenshogaku Zasshi 73:130–137
Baghiei N, Khalilzadeh S, Arami S, Velayati AA, Bakhshayesh Karam M, Masjedi R (2005) Diagnostic value of lung CT-scan in childhood tuberculosis. Tanaffos 4:57–62
Takashi Yoshiyama HO (2008) CT screening before treatment of latent tuberculous infection for the diagnosis of clinical TB among contacts. Kekkaku 83:411–416
Lew WJ, Jung YJ, Song JW et al (2009) Combined use of QuantiFERON-TB Gold assay and chest computed tomography in a tuberculosis outbreak. Int J Tuberc Lung Dis 13:633–639
Lee SW, Jang YS, Park CM et al (2010) The role of chest CT scanning in TB outbreak investigation. Chest 137:1057–1064
Hirama T, Hagiwara K, Kanazawa M (2011) Tuberculosis screening programme using the QuantiFERON-TB Gold test and chest computed tomography for healthcare workers accidentally exposed to patients with tuberculosis. J Hosp Infect 77:257–262
Garrido JB, Alias Hernandez I, Bonillo Perales A et al (2012) Usefulness of thoracic CT to diagnose tuberculosis disease in patients younger than 4 years of age. Pediatr Pulmonol 47:895–902
Fujikawa A, Fujii T, Mimura S et al (2014) Tuberculosis contact investigation using interferon-gamma release assay with chest x-ray and computed tomography. PLoS One 9:e85612
Catho G, Senechal A, Ronnaux-Baron AS et al (2015) Children exposed to multidrug-resistant tuberculosis: How should we manage? Analysis of 46 child contacts and review of the literature. Rev Pneumol Clin 71:335–341
Lu X, Wang X, Li D, Wang X, Wu J (2016) Comparative study of DR and CT in the application of close contacts screening for tuberculosis outbreaks. Radiol Infect Dis 3:34–39
Ziemele B, Ranka R, Ozere I (2017) Pediatric and adolescent tuberculosis in Latvia, 2011–2014: case detection, diagnosis and treatment. Int J Tuberc Lung Dis 21:637–645
Lee SC, Yoon SH, Goo JM, Yim JJ, Kim CK (2017) Submillisievert computed tomography of the chest in contact investigation for drug-resistant tuberculosis. J Korean Med Sci 32:1779–1783
Shimizu H, Mori M (2017) Usefulness of the combination of tuberculin skin test and interferon-gamma release assay in diagnosing children with tuberculosis. Tohoku J Exp Med 243:205–210
Moreno-Ballester V, Aparici-Robles F, Marti-Bonmati L et al (2018) Findings and utility of chest computed tomography in pediatric tuberculosis. J Pediatr Infect Dis 13:25–31
Yoshiyama T, Kurosaki A, Ogata H, Sasaki Y, Okumura M (2019) Limited benefit of CT scans in tuberculosis contact tracing. J Infect Chemother 25:764–768
Zhou Y, Gu Y, Guo T, Zhang Y, Miao Z (2019) Outbreak of pulmonary tuberculosis in lodging high school, should X-ray be replaced by CT? Radiol Infect Dis 6:154–162
Yoon S, Mihn D-C, Song J-H, Kim SA, Yim J-J (2020) Evolution of interferon-gamma release assay results and submillisievert chest CT findings among close contacts of active pulmonary tuberculosis patients. Tuberc Respir Dis 83:283–288
Wang M, Huang C, Shen X et al (2020) The study of tuberculosis outbreak in a high school—Shanghai, China, 2017–2018. J Public Health. https://doi.org/10.1007/s10389-020-01380-2
Mok J, Yeom JA, Nam SW et al (2021) Role of digital tomosynthesis in the context of tuberculosis contact investigation: comparisons with digital radiography. Acta Radiol. https://doi.org/10.1177/02841851211022498
Ghesani N, Patrawalla A, Lardizabal A, Salgame P, Fennelly KP (2014) Increased cellular activity in thoracic lymph nodes in early human latent tuberculosis infection. Am J Respir Crit Care Med 189:748–750
Esmail H, Lai RP, Lesosky M et al (2016) Characterization of progressive HIV-associated tuberculosis using 2-deoxy-2-[(18)F]fluoro-D-glucose positron emission and computed tomography. Nat Med 22:1090–1093
Molton JS, Thomas BA, Pang Y et al (2019) Sub-clinical abnormalities detected by PET/MRI in household tuberculosis contacts. BMC Infect Dis 19:83
Naftalin CM, Leek F, Hallinan JTPD et al (2020) Comparison of 68Ga-DOTANOC with 18F-FDG using PET/MRI imaging in patients with pulmonary tuberculosis. Sci Rep 10:14236
Treatment success rate for patients treated for MDR-TB. WHO World Health Organization:https://www.who.int/data/gho/indicator-metadata-registry/imr-details/3432
Prophylaxis IUATCo (1982) Efficacy of various durations of isoniazid preventive therapy for tuberculosis: five years of follow-up in the IUAT trial. International Union Against Tuberculosis Committee on Prophylaxis. Bull World Health Organ 60:555–564
Walsh GP, Tan EV, dela Cruz EC et al (1996) The Philippine cynomolgus monkey (Macaca fasicularis) provides a new nonhuman primate model of tuberculosis that resembles human disease. Nat Med 2:430–436
Scanga CA, Flynn JL (2014) Modeling tuberculosis in nonhuman primates. Cold Spring Harb Perspect Med 4:a018564
Capuano SV 3rd, Croix DA, Pawar S et al (2003) Experimental Mycobacterium tuberculosis infection of cynomolgus macaques closely resembles the various manifestations of human M. tuberculosis infection. Infect Immun 71:5831–5844
Lin PL, Rodgers M, Smith L et al (2009) Quantitative comparison of active and latent tuberculosis in the cynomolgus macaque model. Infect Immun 77:4631–4642
Lin PL, Ford CB, Coleman MT et al (2014) Sterilization of granulomas is common in active and latent tuberculosis despite within-host variability in bacterial killing. Nat Med 20:75–79
Ganchua SKC, White AG, Klein EC, Flynn JL (2020) Lymph nodes-The neglected battlefield in tuberculosis. PLoS Pathog 16:e1008632
Ganchua SKC, Cadena AM, Maiello P et al (2018) Lymph nodes are sites of prolonged bacterial persistence during Mycobacterium tuberculosis infection in macaques. PLoS Pathog 14:e1007337
Drain PK, Bajema KL, Dowdy D et al (2018) Incipient and subclinical tuberculosis: a clinical review of early stages and progression of infection. Clin Microbiol Rev 31:18
Migliori GB, Ong CWM, Petrone L, Ambrosio L, Centis R, Goletti D (2021) The definition of tuberculosis infection based on the spectrum of tuberculosis disease. Breathe 17:210079
Bhuniya S, De P (2010) Questions in the role of chest CT scanning in TB outbreak investigation. Chest 138:1522–1523
Schluger NW (2010) CT scanning for evaluating contacts of TB patients: ready for prime time? Chest 137:1011–1013
Gillini L, Centis R, D’Ambrosio L et al (2015) Is Europe ready to reach tuberculosis elimination? An outbreak report from Southern Italy. Eur Respir J 46:274–277
Sterling TR, Njie G, Zenner D et al (2020) Guidelines for the treatment of latent tuberculosis infection: recommendations from the National Tuberculosis Controllers Association and CDC, 2020. MMWR Recomm Rep 69:1–11
Nahid P, Mase SR, Migliori GB et al (2019) Treatment of drug-resistant tuberculosis. An Official ATS/CDC/ERS/IDSA Clinical Practice Guideline. Am J Respir Crit Care Med 200:e93–e142
Diel R, Loddenkemper R, Nienhaus A (2012) Predictive value of interferon-gamma release assays and tuberculin skin testing for progression from latent TB infection to disease state: a meta-analysis. Chest 142:63–75
Gupta RK, Turner CT, Venturini C et al (2020) Concise whole blood transcriptional signatures for incipient tuberculosis: a systematic review and patient-level pooled meta-analysis. Lancet Respir Med 8:395–406
World Health O (2017) Consensus meeting report: development of a target product profile (TPP) and a framework for evaluation for a test for predicting progression from tuberculosis infection to active disease. World Health Organization, Geneva
Lin PL, Coleman T, Carney JP et al (2013) Radiologic responses in cynomolgus macaques for assessing tuberculosis chemotherapy regimens. Antimicrob Agents Chemother 57:4237–4244
Lin PL, Maiello P, Gideon HP et al (2016) PET CT identifies reactivation risk in cynomolgus macaques with latent M. tuberculosis. PLoS Pathog 12:e1005739
Perrin FM, Woodward N, Phillips PP et al (2010) Radiological cavitation, sputum mycobacterial load and treatment response in pulmonary tuberculosis. Int J Tuberc Lung Dis 14:1596–1602
Singla R, Singla N, Sarin R, Arora VK (2005) Influence of pre-treatment bacillary load on treatment outcome of pulmonary tuberculosis patients receiving DOTS under revised national tuberculosis control programme. Indian J Chest Dis Allied Sci 47:19–23
Ford CB, Shah RR, Maeda MK et al (2013) Mycobacterium tuberculosis mutation rate estimates from different lineages predict substantial differences in the emergence of drug-resistant tuberculosis. Nat Genet 45:784–790
Bastos ML, Lan Z, Menzies D (2017) An updated systematic review and meta-analysis for treatment of multidrug-resistant tuberculosis. Eur Respir J 49:1600803
Turkova A, Wills GH, Wobudeya E et al (2022) Shorter treatment for nonsevere tuberculosis in African and Indian Children. N Engl J Med 386:911–922
Prevention Committee of the Japanese Society for T, Treatment Committee of the Japanese Society for T (2014) Treatment guidelines for latent tuberculosis infection. Kekkaku 89:21–37
Migliori GB, Nardell E, Yedilbayev A et al (2019) Reducing tuberculosis transmission: a consensus document from the World Health Organization Regional Office for Europe. Eur Respir J 53:1900391
Nachiappan AC, Rahbar K, Shi X et al (2017) Pulmonary tuberculosis: role of radiology in diagnosis and management. Radiographics 37:52–72
Kwong JS, Carignan S, Kang EY, Muller NL, FitzGerald JM (1996) Miliary tuberculosis. Diagnostic accuracy of chest radiography. Chest 110:339–342
Dong-Hyun Joo HWL, Yoon S-Y, Park TY, Heo EY, Kim DK, Chung HS, Lee J-K (2021) Chest computed tomography scan as an initial diagnostic method for tuberculosis infection detected by mass screening. Korean J Intern Med 1:1
Starshinova A, Dovgaliuk I, Korneva N, Yakunova O, Yablonskiy P (2013) The diagnosis of latent tuberculosis infection in children with new immunologic tests. Eur Respir J 42:P2840
Yan C, Liang C, Xu J et al (2019) Ultralow-dose CT with knowledge-based iterative model reconstruction (IMR) in evaluation of pulmonary tuberculosis: comparison of radiation dose and image quality. Eur Radiol 29:5358–5366
Huang B, Law MW, Khong PL (2009) Whole-body PET/CT scanning: estimation of radiation dose and cancer risk. Radiology 251:166–174
Pearce MS, Salotti JA, Little MP et al (2012) Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet 380:499–505
Kowada A (2013) Cost effectiveness of high resolution computed tomography with interferon-gamma release assay for tuberculosis contact investigation. Eur J Radiol 82:1353–1358
Bomanji J, Sharma R, Mittal BR et al (2020) PET/CT features of extrapulmonary tuberculosis at first clinical presentation: a cross-sectional observational <sup>18</sup>F-FDG imaging study across six countries. Eur Respir J 55:1901959
Frascella B, Richards AS, Sossen B et al (2021) Subclinical tuberculosis disease—a review and analysis of prevalence surveys to inform definitions, burden, associations, and screening methodology. Clin Infect Dis 73:e830–e841
Kang W, Yu J, Du J et al (2020) The epidemiology of extrapulmonary tuberculosis in China: a large-scale multi-center observational study. PLoS One 15:e0237753
Naing C, Mak JW, Maung M, Wong SF, Kassim AIBM (2013) Meta-analysis: the association between HIV infection and extrapulmonary tuberculosis. Lung 191:27–34
Gomez-Pastrana D, Carceller-Blanchard A (2007) Should pulmonary computed tomography be performed in children with tuberculosis infection without apparent disease? An Pediatr (Barc) 67:585–593
Liao CY, Chen JH, Liang JA, Yeh JJ, Kao CH (2012) Meta-analysis study of lymph node staging by 18 F-FDG PET/CT scan in non-small cell lung cancer: comparison of TB and non-TB endemic regions. Eur J Radiol 81:3518–3523
Joekes E, Davies G, Mwandumba HC, Squire SB (2010) Insufficient evidence for chest CT scan in TB outbreak investigation. Chest 138:234–235
Okada F, Ando Y, Yoshitake S et al (2007) Clinical/pathologic correlations in 553 patients with primary centrilobular findings on high-resolution CT scan of the thorax. Chest 132:1939–1948
Ong CW, Elkington PT, Friedland JS (2014) Tuberculosis, pulmonary cavitation, and matrix metalloproteinases. Am J Respir Crit Care Med 190:9–18
Hunter RL (2016) Tuberculosis as a three-act play: a new paradigm for the pathogenesis of pulmonary tuberculosis. Tuberculosis (Edinb) 97:8–17
Im JG, Itoh H (2018) Tree-in-bud pattern of pulmonary tuberculosis on thin-section CT: pathological implications. Korean J Radiol 19:859–865
Wells G, Glasgow JN, Nargan K et al (2021) Micro-computed tomography analysis of the human tuberculous lung reveals remarkable heterogeneity in three-dimensional granuloma morphology. Am J Respir Crit Care Med 204:583–595
Acknowledgments
The authors greatly appreciate the review and helpful comments from Professor Alexander A. Bankier, MD, Ph.D. The authors would like to acknowledge Andrew Dombrowski, Ph.D. (Compecs, Inc.), for his assistance in improving the use of English in this manuscript.
Funding
The authors did not receive any funding for this review.
Author information
Authors and Affiliations
Contributions
SHY initiated this review, conducted a systematic literature search, and led manuscript drafting. JMG, YJJ, TY, and JP critically reviewed the initial draft, revised and supplemented the content. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The institutional review boards of Seoul National University Hospital approved a representative case illustration in this review (IRB No. 2110-186-1267).
Consent for publication
The institutional review boards waived informed consent for an anonymized retrospective case presentation.
Competing interests
Soon Ho Yoon works in the MEDICALIP as an unpaid chief medical officer outside this work and has a stock option in the firm. Other authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1.
Supplemental figure 1. Preferred Reporting Items for Systematic Reviews and Meta-analyses diagram of the study selection process. Supplemental Table 1. Summary of definition for parenchymal and LN abnormalities in the included studies.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Yoon, S.H., Goo, J.M., Yim, JJ. et al. CT and 18F-FDG PET abnormalities in contacts with recent tuberculosis infections but negative chest X-ray. Insights Imaging 13, 112 (2022). https://doi.org/10.1186/s13244-022-01255-y
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13244-022-01255-y