Abstract
Background
The term rapidly progressive dementia (RPD) with Lewy bodies (rpDLB) is used for DLB patients who develop a rapidly progressive neurological syndrome and have reduced survival. Here, we characterise the clinical, neuropathological, and molecular characteristics of a large rpDLB neuropathological series.
Methods
We included all RPD patients with a disease duration < 4 years submitted to our prion disease referral centre between 2003 and 2022 who showed Lewy body pathology (LBP) in limbic or neocortical stages as primary neuropathological diagnosis, had no systemic condition justifying the rapid deterioration and were previously neurologically unimpaired. Clinical features were retrieved and compared with Creutzfeldt-Jakob disease (CJD) and rapidly progressive Alzheimer’s disease (rpAD) cohorts. Neuropathological and genetic (whole exome sequencing, APOE genotyping, and C9orf72 repeat expansion analysis) characteristics of rpDLB patients were systematically investigated. We scored semi-quantitatively the LBP load and performed a α-synuclein (αSyn) RT-QuIC seeding amplification assay (SAA) on cerebrospinal fluid (CSF) and tenfold serially diluted brain homogenates from different brain areas in rpDLB patients and typical long-lasting Lewy body disease (LBD) with dementia patients as control group.
Results
RpDLB patients were older (p = 0.047) and presented more cognitive fluctuations (p = 0.005), visual hallucinations (p = 0.020), neuropsychiatric symptoms (p = 0.006) and seizures (p = 0.032), and fewer cerebellar (p < 0.001) and visual (p = 0.004) signs than CJD ones. Delirium onset was more common than in both CJD (p < 0.001) and rpAD (p = 0.008). Atypical LBD signs (pyramidal, myoclonus, akinetic mutism) were common. All tested patients were positive by CSF αSyn SAA. Concomitant pathologies were common, with only four cases showing relatively “pure” LBP. LBP load and αSyn seeding activity measured through αSyn RT-QuIC SAA were not significantly different between rpDLB patients and typical LBD. We found a likely pathogenic variant in GBA in one patient.
Conclusions
Our results indicate that: 1) rpDLB exhibits a distinct clinical signature (2) CSF αSyn SAA is a reliable diagnostic test; 3) rpDLB is a heterogeneous neuropathological entity that can be underlain by both widespread pure LBP, or multiple copathologies 4) rpDLB is likely not sustained by distinct αSyn conformational strains; 5) genetic defects may, at least occasionally, contribute to the poor prognosis in these patients.
Similar content being viewed by others
Background
Lewy body disease (LBD), the second-most common neurodegenerative disorder after Alzheimer’s disease (AD), is characterized by misfolded alpha-synuclein (αSyn) aggregates in neuronal cell bodies (i.e., Lewy bodies [LBs]) and nerve terminals (i.e., Lewy neurites [LNs]). LB pathology (LBP) spread within the CNS can follow distinct pathways, most commonly exhibiting an ascending course, from the early brainstem involvement (brainstem stage, I), through the limbic areas (limbic stage, II) to the neocortex (neocortical stage, III) [1]. LBP is the hallmark of prevalent neurodegenerative diseases, e.g., Parkinson’s disease (PD), Parkinson’s disease dementia (PDD), and Dementia with Lewy bodies (DLB), commonly characterized by progressive motor, cognitive, dysautonomic, and sleep disturbances. These likely represent different subtypes within the same disease spectrum, for which the term neuronal synuclein disorder has been recently proposed, with at least some phenotypic heterogeneity depending on topography and severity of lesions and co-pathologies (primarily AD) [2, 3]. Despite the clinical variability, the disease is “slowly” progressive in most cases, with the shortest average survival in DLB, estimated to be around 7–8 years from onset [4, 5]. The term rapidly progressive DLB (rpDLB) is commonly used to refer to DLB patients who develop a rapidly progressive neurological syndrome and have reduced survival. Although these cases have long been described in the literature, there is no international consensus on the rpDLB definition. Furthermore, whether rpDLB represents a distinct clinicopathological entity in the LBD spectrum or the reduced survival is simply due to concomitant factors or pathologies is still debated. Finally, from a clinical perspective, the possibility of a rapidly progressive neurological syndrome being underlain by potentially treatable disorders and the prospective identification of targeted therapies for neurodegenerative diseases require high speed and accuracy in rpDLB diagnosis, which is often challenged by the high frequency of atypical signs for LBD (e.g., myoclonus, akinetic mutism, pyramidal and cerebellar signs) [6,7,8,9,10,11,12,13].
Here we describe the clinical, diagnostic, genetic, and neuropathologic features in the largest neuropathologic rpDLB cohort defined to date, taking advantage of our 20-year experience as a rapidly progressive dementia (RPD) reference centre in Italy. Furthermore, by performing αSyn Real-Time Quaking Induced Conversion (RT-QuIC) seeding amplification assay (SAA) on cerebrospinal fluid (CSF) and brain samples, we characterize for the first time the αSyn seeding properties in rpDLB.
Methods
Patient selection
A series of 826 consecutive brains were submitted to the Neuropathology Laboratory (NP-Lab) at the Istituto delle Scienze Neurologiche di Bologna, Italy (ISNB) between 2003 and 2022 for neuropathologic assessment of RPD. The cohort mainly included cases of Creutzfeldt-Jakob disease (CJD), rpAD, encephalitis, lymphoma, Wernicke’s encephalopathy, vascular dementia, and frontotemporal lobar degeneration (FTLD). Neuropathological diagnosis of neurodegenerative diseases was made according to established criteria [14,15,16,17]. All brains were screened for the presence of LBP. The rpDLB cohort was selected according to the following inclusion criteria: (1) the presence of LBP in the limbic or neocortical stage, (2) LBP as primary neuropathological diagnosis (e.g., CJD, inflammatory, toxic/metabolic, neoplasms cases showing LBP were excluded), (3) no clinical, biochemical or imaging findings suggestive of any primary systemic condition justifying the rapidly progressive disease course, (4) availability of adequate clinical documentation including the information that patients were neurologically unimpaired before the RPD onset, (5) disease duration (defined as timespan between onset and death) < 4 years, as previously reported [10]. Overall, 22 participants fulfilled our inclusion criteria for rpDLB. Of note, in 18 out of 22 rpDLB cases eventually included, disease duration was < 2 years (see Supplementary materials for further details concerning patient selection).
Clinical assessment
We retrieved clinical and diagnostic data of rpDLB patients. We also analyzed the medical records of two additional sub-cohorts of consecutive RPD patients, representative of the most common differential diagnoses of neurodegenerative RPD: CJD (N = 100) and rpAD (N = 31) (see Supplementary material for further details). Two independent evaluators (PP and GMB) identified each patient who fulfilled the current diagnostic criteria for DLB [18] and CJD [19].
CSF biomarker analysis
CSF samples were obtained by lumbar puncture (LP) at the L3/L4 or L4/L5 level following a standard procedure, centrifuged in case of blood contamination, divided into aliquots, and stored in polypropylene tubes at − 80 °C until analysis. CSF total tau (t-tau), phospho-tau181 (p-tau181), Aβ42 and Aβ40 were measured by chemiluminescent enzyme immunoassays on the automated Lumipulse G600II platform (Fujirebio), as described [20]. We used ELISA kits to measure CSF 14–3–3 gamma isoform and neurofilament light chain (NfL), as described [21]. Also, the second-generation prion RT-QuIC was performed in all available CSF samples, as previously reported [22]. All analyses were performed at the NP-Lab by personnel blinded to neuropathological diagnosis.
Neuropathological studies
Neuropathological examination was performed at NP-Lab using standardized procedures as described [23]. Specifically, half of the brain was frozen and stored at -80 °C. The other half was fixed in 10% buffered formalin, processed by paraffin wax embedding, and sliced to obtain tissue blocks from 24 regions. Hematoxylin–eosin staining was applied to 7 μm thick sections from each block. An immunohistochemical panel with antibodies specific for αSyn (LB509, dilution 1:100, Thermo Fisher Scientific), phospho-tau (p-tau) (AT8, dilution 1:100, Innogenetics), Aβ (4G8, dilution 1:5000, Signet Labs), prion protein (3F4, dilution 1:400, Signet Labs), and TDP-43 (409/410, dilution 1:5000, Cosmo Bio) was applied to all cases using several brain regions, following established consensus criteria [14,15,16, 24]. An experienced neuropathologist (PP) formulated the final diagnosis and assigned the stage of LBP according to current consensus criteria [14, 25]. Moreover, the level of AD neuropathologic change (ABC score) [16], the presence of atherosclerosis, small vessel disease (SVD), vascular brain injury (VBI), cerebral amyloid angiopathy (CAA), hippocampal sclerosis (HS), and any other relevant pathology (e.g., primary age-related tauopathy [PART], and limbic-predominant age-related TDP-43 encephalopathy [LATE]) were also reported and classified according to consensus criteria [16, 24, 26, 27]. Considering these parameters, a composite neuropathology score (NP score) was calculated for each case (see Supplementary material for further details).
For the semiquantitative assessment of LBP, brains with LBs or LNs in at least one section were examined independently by two evaluators (PP and GMB), as previously reported [23]. Briefly, αSyn immunoreactivity was evaluated semi-quantitatively (0-no immunoreactivity; 1-mild; 2-moderate; 3-prominent immunoreactivity) in the following regions: medulla oblongata (vagus dorsomedial nucleus, intermediate reticular zone), pons (locus coeruleus, raphe), substantia nigra, hypothalamus, basal forebrain (Meynert’s basal nucleus and surrounding gray matter), amygdala, hippocampus (CA2–CA4 sectors), parahippocampal gyrus, cingulate gyrus, middle temporal gyrus, and middle frontal gyrus. We scored the neuronal LBs and LNs separately. Each case was given a combined “LB score” (range 0–66).
Evaluation of αSyn seeding activity in CSF and brain homogenates by RT-QuIC SAA
The αSyn RT-QuIC SAA was performed in CSF and brain homogenates as previously described [23]. Specifically, samples and controls were deemed positive after the first run when at least three out of four replicates reached a threshold arbitrarily set at 30% of the median of the maximum fluorescence intensity (Imax) reached by the positive control replicates. Tenfold serial dilutions were analyzed for the αSyn seeds quantification in brain homogenates. The dilution series was analyzed until the αSyn RT-QuIC SAA yielded ≤ 2 out of 4 positive replicates. Then, we used the Spearman–Kärber algorithm, which has been previously applied for the quantification of prion seeding activity [28,29,30], to estimate a seeding dose or dilution at which only 50% (e.g., 2 of 4) of replicates are positive (50% seeding doses or SD50). Next, to estimate the αSyn seed concentration in each brain area, an SD50 (expressed in logarithmic scale) per mg of tissue was calculated. Finally, we obtained a combined SD50 score for each brain by summing all brain areas’ SD50/mg values to compare the overall αSyn seeding activity between brains.
Genetic analysis
All rpDLB patients with an age at onset < 75 years and with DNA viable for analyses underwent whole exome sequencing (WES). WES was performed on DNA extracted from the peripheral blood cells of each patient. The sample library was prepared using xGen™ DNA EZ Library Prep Kit (IDT), enriched with xGen Exome Research Panel v2 (IDT) probes, and then sequenced with 2 × 100 bp paired-end reads on a NovaSeq 6000 instrument (Illumina). Sequencing was performed with an average coverage of 131.7X and the coverage 20x was over 99% of all samples. Bioinformatic analysis followed the GATK v.4.2.0.0 workflow for germline variant discovery, aligning to reference genome GRCh38/hg38. We prioritized rare variants compatible with autosomal inheritance in genes involved in PD, DLB, AD, and FTLD diseases. Variants of interest were classified according to the American College of Medical Genetics (ACMG) guidelines, and the evaluation of clinical consequences was based on ClinVar and Franklin Genoox databases [31, 32].
Genotyping of APOE was performed separately by restriction fragment length polymorphism according to Wenham et al. in all patients with DNA viable for analyses [33]. We also screened our cohort for the presence of C9orf72 repeat expansions using the 2-step strategy with southern blotting confirmation, as previously described [20].
Statistical analysis
Statistical analyses were performed using GraphPad Prism 9 (Graph-Pad Software) and Stata 18 SE (StataCorp). Data were expressed as mean ± standard deviation (SD) or median and interquartile range (IQR) based on the distribution of values. For αSyn RT-QuIC SAA experiments, the assay relative fluorescence response data (the Imax, the lag phase, and the area under curve (AUC) were extracted and analyzed [23]. The normality of the distribution of variables was assessed using the Kolmogorov–Smirnov test. For continuous variables, we variably applied the Mann–Whitney U test, t-test, Kruskal–Wallis test (followed by Dunn–Bonferroni post hoc test), or the one-way analysis of variance (followed by Tukey’s post hoc test), depending on the group number and data distribution. The Chi-square test or the Fisher’s exact test were adopted for categorical variables. Pearson’s correlation coefficient or Spearman’s rank correlation coefficient were variably computed to determine significant associations between variables, depending on values distribution. P values < 0.05 were considered statistically significant.
Results
Clinical features and diagnostic findings
Demographic and clinical features, diagnostic findings, and clinical diagnoses at the time of the first diagnostic assessment are reported in Tables 1 and 2. All 22 rpDLB cases presented with RPD as per inclusion criteria. The median age of onset was 73.0 (IQR 70.5–77.0) years, with a median disease duration of 7.5 (IQR 2.0–21.0) months. CJD was the most common diagnostic suspect, followed by rapidly progressive non-prion neurodegenerative disorders (i.e., AD and DLB). Retrospectively, 16/22 patients fulfilled the current diagnostic criteria for DLB (7 probable and 9 possible), while 2/22 and 7/22 could be classified as probable and possible sCJD, respectively. Core DLB clinical features were common within the cohort (36% of patients exhibited cognitive fluctuations and recurrent visual hallucinations, while 50% showed one or more spontaneous cardinal features of parkinsonism), except for REM sleep behavior disorder (RBD), which was anamnestically reported in only one patient (of note, polysomnographic recordings were not available in any patient). Psychiatric symptoms were relatively common, with 47% of cases showing a delirium onset RPD, 27% and 50% developing apathy, anxiety and/or depression, and systematized delusions, respectively, along the disease course. Atypical LBD signs were variably found in our cohort, with some patients showing myoclonus (41%), akinetic mutism (22%), and pyramidal signs (13%). Finally, 18% of cases developed seizures during the disease course.
Next, we checked whether rpDLB exhibited a peculiar clinical signature against the most common differential diagnoses (i.e., CJD and rpAD) by looking for differences in neurological signs frequencies at the time of the first clinical assessment between the three groups (Table 1). CJD patients were significantly younger than rpDLB (p = 0.047) and rpAD (p = 0.034) ones. They more often exhibited cerebellar signs than rpDLB and rpAD (both p < 0.001). Conversely, complex visual hallucinations and seizures were rarer in CJD compared to rpDLB (p = 0.020 and p = 0.032, respectively) and rpAD (p = 0.003 and p < 0.001, respectively). rpDLB patients showed more cognitive fluctuations and neuropsychiatric symptoms, and fewer visual disturbances than CJD ones (p = 0.005, p = 0.006, and p = 0.004, respectively). Eventually, a delirium onset RPD was the only clinical feature that could distinguish rpDLB patients from both CJD (p < 0.001) and rpAD (p = 0.008) ones.
Regarding diagnostic investigations performed for the differential diagnosis with CJD, 21% of rpDLB patients showed generalized periodic sharp/wave complexes (PSWCs) on electroencephalography (EEG), and none exhibited characteristic hyperintensities on magnetic resonance imaging (MRI) on fluid-attenuated inversion recovery (FLAIR) and diffusion-weighted (DWI) sequences. Surrogate neurodegeneration CSF biomarkers showed lower CSF levels in rpDLB patients than CJD ones (14-3-3: p < 0.001; t-tau: p < 0.001; NfL: p = 0.072) (Table 1). However, 14-3-3 and t-tau exceeded the cut-off levels supporting the diagnosis of probable CJD (when clinical criteria for possible CJD are fulfilled) in 8.3% and 33.3% of rpDLB patients, respectively. Retrospectively, the negative prion protein RT-QuIC SAA combined with a positive αSyn RT-QuIC SAA confirmed the diagnosis of LBD in all cases and excluded that of CJD.
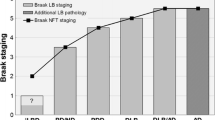
Neuropathological findings
All cases exhibited LBP in neocortical or limbic stages as per inclusion criteria. Concomitant AD neuropathological changes were reported in 73% and 14% of patients in intermediate/high and low degrees, respectively. Two of the remaining three patients (cases #8 and #18) showed PART. SVD was relevant in 23% of patients. VBI was insignificant in most patients, except for patient #7, who presented widespread cortical and subcortical microscopical infarctions. CAA type 1 was present in three patients in moderate/severe grade (#7, #13, and #19), while type 2 was reported in four cases (#12, #15, #16, and #17) in mild/moderate grade. Finally, two patients had hippocampal sclerosis (cases #7 and #15), and one had LATE (case #4). Neuropathological findings are reported in Table 2 and Fig. 1.
Main histopathological features of rpDLB cases. LPB showed typical morphology, with varying amounts of αSyn-immunoreactive LBs and LNs (a-d). Brainstem-type LBs and LNs in the medulla oblongata (a), substantia nigra (bi-bii), and basal forebrain (c) and cortical-type LBs and LNs in the amygdala (d) of case #22. High magnification image of an LB (c): αSyn immunoreactivity is prominent in the halo and peripheral portion of the core of brainstem-type LBs [1]. P-tau immunoreactive neuritic plaques in the frontal cortex of patient #21 (e), who presented high-grade AD neuropathological changes. Type 1 CAA copathology in the occipital cortex of patient #7 (f). Immunohistochemistry for αSyn (LB509) (a-d), p-tau (AT8) (e), and Aβ (4G8) (f). Abbreviations: αSyn, α-synuclein; AD, Alzheimer’s disease; CAA, cerebral amyloid angiopathy; LBP, Lewy body pathology; LN, Lewy neurites; p-tau, phosphorylated tau; Aβ, amyloid-beta
LBP semiquantitative assessment results
To investigate possible differences in LBP load between patients with rpDLB and typical DLB, we also scored semi-quantitatively the entity of LBP at immunohistochemistry in all rpDLB cases (see Table 2 and Supplementary Table 2 for details) and in eight subjects with typical long-standing LBD with dementia as controls (see Supplementary material). The average LB score was 48.5 ± 8.5 (ranging from 34 to 66) in rpDLB, while it was 49.1 ± 5.2 (ranging from 42 to 56) in the control group. There were no significant differences between the average LB scores of the two groups in any of the examined brain areas (Fig. 2A).
The LB score was not associated with clinical variables such as disease duration, age at onset, or age at death, while it significantly negatively correlated with the NP score (r=-0.42, p = 0.046) (Fig. 2B).
LB score in different brain areas and correlation with NP score. (a) Mean LB score of rpDLB patients and controls in different brain areas. Error bars represent standard deviation. (b) Correlation plot of the LB score and NP score (r=-0.42, p = 0.046). Linear regression line and relative confidence interval were applied to the plot. Abbreviations: AMG, amygdala; CIN, cingulate gyrus; CTRL, controls; EC, entorhinal cortex; FC, frontal cortex; HYP, hypothalamus; HIPP, hippocampus; LB, Lewy-body; MED, medulla oblongata; NP, neuropathology; PO, pons; SN, substantia nigra; TC, temporal cortex
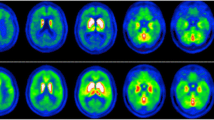
Brain homogenates αSyn RT-QuIC SAA results
To investigate the seeding properties of αSyn in rpDLB, we performed αSyn RT-QuIC SAA on brain homogenates from five rpDLB subjects (cases #10, #14, #17, #18, and #22) and five age-matched and sex-matched patients with a typical history of long-standing LBD with dementia (see Supplementary material). Tenfold serial dilutions of brain homogenates were obtained from the medulla oblongata, substantia nigra, amygdala, and frontal cortex. αSyn seeding activity was detected in all tested brain areas over a heterogeneous dilution range (from 10− 4 to 10− 21), depending on the brain area. The average brain SD50 score was 51.1 ± 16.2 SD50/mg (ranging from 38.5 to 73.9 SD50/mg) in rpDLB, while it was 46.7 ± 13.6 SD50/mg (ranging from 39.0 to 63.2) in typical DLB. We found no significant differences between the mean SD50 scores of the two groups in any of the four examined brain areas, apart from a slight tendency for rpDLB to have higher levels than typical DLB (especially in the amygdala and the substantia nigra) (see Fig. 3). Next, to further exclude that a different αSyn conformational strain is responsible for the rapidly progressive course in rpDLB patients, compared with typical DLB, we looked for differences in the seeding activity in different brain areas at dilution corresponding to SD50 (i.e., assuming that an equal seed dose is contained in each sample), as previously described [23]. This analysis showed no differences in the average αSyn RT-QuIC SAA kinetic parameters (Lag phase, Imax, and AUC) between rpDLB and the control group in any of the four investigated brain areas.
Quantification of αSyn seeding activity in brain homogenates. Mean SD50 score of rpDLB patients and controls in different brain areas. Error bars represent standard deviation. Abbreviations: AMG, amygdala; CTRL, controls; FC, frontal cortex; MED, medulla oblongata; SD, seeding dose; SN, substantia nigra
Genetic findings
We identified rare variants in known neurodegenerative disease-associated genes in six (cases #3, #9, #10, #16, #19, and #22) out of eight patients who underwent WES (Table 2 and Supplementary Table 3). Of the identified genes, four (EIF4G1, VPS13C, SYNJ1, and GBA1) were associated with PD, one (GRN) with FTLD, one with idiopathic basal ganglia calcification (MYORG), and one (NOTCH3) with Cerebral arteriopathy with subcortical infarcts and leukoencephalopathy 1 (CADASIL1). All were classified as variants of uncertain significance (VUS) according to the Franklin ACMG Classification [32], apart from one (case #22 - GBA: p.Lys196Gln), which was considered likely pathogenic. In the ClinVar database [31], five (case #3 - EIF4G1: p.Ala13Pro + p.Ser15ProfsX39 + p.Gly17ThrfsX37 + p.Leu18Pro, and case #19 - MYORG: p.Leu544Gln) were not reported, two (case #9 - VPS13C: p.Pro933Leu, and case #10 - SYNJ1: p.Thr842Asn) were classified as VUS, while three (case #9 - GRN: p.Val90Met, case #16 - NOTCH3: p.Glu813Lys, and case #22 - GBA: p.Lys196Gln) had conflicting interpretations. The GBA variant of case #22 has been associated with Gaucher disease [34, 35]. Patients #3, #19, and #22 presented intermediate/high levels of AD neuropathological changes, while cases #9 and #10 exhibited no significant AD copathology. Cases #16 and #19 also had moderate grade type 2 and type 1 CAA, respectively (Table 2). No pathogenic C9orf72 repeat expansions were found. APOE genotyping was possible in sixteen patients. Seven of them carried an APOE ε4 allele, of whom five showed intermediate/high levels of AD neuropathological changes (cases #4, #12, #15, #16, and #19), three had type 2 CAA (cases #12, #15, and #16), and one had type 1 CAA (case #19) (Table 2).
Discussion
In CJD surveillance centers, rpDLB accounts for about 2–8% of RPD cases. However, only a few studies with small case series have addressed this patient subgroup’s clinical, diagnostic, neuropathological, and molecular features. At the same time, whether or not rpDLB represents a distinct clinicopathologic subtype is still debated [6,7,8,9,10,11, 36,37,38].
The small number of deeply phenotyped rpDLB cases described in the literature limits the definition of the rpDLB clinical phenotype. Consistent with our results, the mean age of onset ranges from 70 to 80 years [9, 11, 13] with no [9] or slight male predominance [7, 13], as reported in typical DLB [5]. In previous studies, disease duration varied between 9 and 45 months [9, 11, 13]. From a clinical perspective, rpDLB patients can present core DLB clinical features [18], including cognitive fluctuations (20–69%), visual hallucinations (60–100%), and parkinsonism (65–90%) [6, 7, 9, 11, 13]. RBD has also been reported in some patients [11], although confirmatory polysomnographic studies defining its true prevalence are lacking. High sensitivity to antipsychotic agents is also a common finding [9, 11, 13]. Consistent with our results, associated atypical signs are relatively frequent, including myoclonus (50–90%), pyramidal signs (38–90%), and akinetic mutism (19–50%). However, this may reflect a selection bias as most reports come from prion disease surveillance centers. Cerebellar signs are rare (0–25%) [6, 7, 9, 13]. Neuropsychiatric symptoms, e.g., apathy, anxiety, depression, and systematized delusions (20–56%), are highly prevalent, as in typical DLB [6, 7, 11, 13, 18]. Interestingly, almost half of our patients presented a delirium onset RPD, with an initial phase characterized by an acute confusional state, only sometimes in the presence of delirium-associated factors (hospitalization or intercurrent illness), then a possible period of improvement, followed by a rapidly dementing phase, as previously reported by Josephs et al. in three cases [10]. We also reported that 18% of our patients showed seizures at some point during the disease course in comparison to an estimated seizures/epilepsy prevalence of 3% in typical DLB [39]. Of note, 4 of 5 of our seizure-presenting patients showed only low AD pathological changes and no significant cerebrovascular disease, suggesting that other mechanisms, possibly involving alterations in neuronal excitability and connectivity due to αSyn deposition and rapid neurodegeneration, may contribute to epileptogenesis in rpDLB.
From a diagnostic perspective, our data indicate that, when compared to CJD, rpDLB patients are older, and present more cognitive fluctuations, visual hallucinations, neuropsychiatric symptoms and seizures, and fewer cerebellar and visual signs (apart from hallucinations). Interestingly, delirium onset was the only clinical variable that could distinguish rpDLB from both CJD and rpAD. Although the link between delirium and LBD is not well understood, delirium has been recognized as a possible onset presentation of DLB [40], and our data suggest that in the context of an RPD, an acute confusional state onset should raise the index of suspicion for underlying LBP.
Regarding the investigations performed for the differential diagnosis with prion disease, rpDLB patients may show PSWCs (0–60%) at EEG, confirming the known low specificity for differentiating CJD from other RPDs [6,7,8, 19]. Conversely, no patients displayed the typical hyperintensities at DWI or FLAIR MRI that are often seen in typical CJD, while most cases showed brain atrophy [9, 11, 13]. To date, conventional brain MRI appears to be of greatest benefit in ruling out other RPD causes with distinctive MRI patterns (e.g., CJD, Wernicke’s encephalopathy, or encephalitis) rather than diagnosing rpDLB specifically [41].
Concerning CSF testing, surrogate neurodegeneration biomarkers (most commonly t-tau, 14-3-3, and NfL) are still used in most centers as first-level investigations in RPD assessment (especially in the absence of CSF findings suggesting an inflammatory or neoplastic etiology). Unfortunately, only a few research papers analyzed rpDLB as a distinct group from other neurodegenerative RPDs, and, in most cases, the diagnosis was made solely on a clinical basis. With these limitations, in line with our results, available studies reported increased t-tau, 14-3-3, and NfL levels in rpDLB, with values tending to be higher than in typical LBD but lower than in CJD [21, 42, 43]. In particular, biomarkers specificity in distinguishing CJD from rpDLB was 88–98% for t-tau, 88–95% for 14-3-3 (western blot assay), and 79% for NfL [21, 42, 43]. High t-tau and 14-3-3 levels in our cohort falsely supported a CJD diagnosis in 33.3% and 8.3% of cases, respectively. We recently reported that synaptic neurodegeneration biomarkers (i.e., β-synuclein, α-synuclein, SNAP-25, and neurogranin) CSF levels increase in rpDLB cases and have high accuracy in the real-life clinical setting of RPD differential diagnosis [44, 45]. In typical LBD, the rise in CSF concentration of these markers seems mostly related to AD copathology, rather than underlying LBP [46]. Future studies are needed to validate this finding in “pure” rpDLB cases in the absence of concomitant AD pathological changes.
The introduction of SAAs (e.g., RT-QuIC), which detect misfolded prion protein and αSyn in the CSF with high accuracy in CJD and LBD, has dramatically increased the diagnostic potential within the spectrum of RPDs [47]. Indeed, within the limits of our small case series, all patients with available CSF tested negative for prion RT-QuIC and positive for αSyn RT-QuIC SAA. Besides SAAs, AD core biomarkers will also play an essential role in the first-line assessment of RPD. Given the routine use of LP in patients with RPDs, the availability of accurate pathology-specific biomarkers for LBD, AD, and CJD will help identify the underlying neurodegenerative pathological processes to carry out targeted therapies.
In this paper, we expand the small neuropathological series of patients with rpDLB described in the literature [7, 10, 11, 13, 48]. It is reported that most rpDLB cases are underlain by LBP in limbic or neocortical stages, and high LBP stages have been associated with shorter survival [7, 10,11,12,13, 48]. However, one rpDLB case with LBP limited to the brainstem has also been described [13]. The level of AD neuropathological changes is highly variable, ranging from none to high [10, 11, 13, 36]. Multiple pathologies are common, including CAA, SVD, VBI, TDP-43 inclusions, and argyrophilic grain disease [7, 10, 11, 13, 48]. In line with these reports, concomitant pathologies were common in our series, including AD, atherosclerosis, SVD, and CAA.
A few studies have investigated the neuropathological correlates of disease duration in DLB. AD copathology (both Aβ and tau) has been shown to act independently and synergistically with LBP, shortening LBD survival [49,50,51]. Non-AD pathologies, including cerebrovascular disease (atherosclerosis, SVD, VBI, CAA), HS, and concomitant proteinopathies (e.g., LATE or PART) are increasingly recognized as synergistic factors in conditioning cognitive decline speed and trajectories, and impacting disease duration [49,50,51,52]. Despite the acknowledged importance of multiple neuropathologies, our data teach that also relatively “pure” LBP cases may show a rapidly progressive disease course.
To further characterize the correlation between LBP and survival, we assessed and compared the LBP loads (expressed as LB score) in rpDLB patients with typical (i.e., long-duration) DLB controls in multiple brain areas. Specifically, we found no significant differences in LB scores between the two groups in any of the examined brain areas, indicating that LBP load is not the main factor responsible for the reduced disease duration in rpDLB patients. In line with this result, the LB score did not correlate with disease duration in rpDLB.
Regarding correlation to other neuropathological lesions, we found a negative correlation between the LB score and the NP score. This finding suggests that rpDLB is a heterogeneous neuropathological entity with some cases exclusively sustained by significant “pure” LBP burden, and others exhibiting LBP of lesser magnitude but with multiple concomitant pathologies, which likely act independently and synergistically to lower the threshold for the development of cognitive impairment and to reduce the overall disease duration.
To investigate the molecular characteristics of αSyn in rpDLB, we performed αSyn RT-QuIC SAA on tenfold serial dilutions of brain homogenates from five rpDLB subjects and five typical LBD patients as controls. We found no significant differences in SD50 scores (reflecting both the seed quantity and the seeding kinetics) between the two groups in any of the examined brain areas, apart from a slight trend towards higher values in the amygdala and substantia nigra of rpDLB patients, further confirming the evidence that LBP load is not the factor responsible for reduced disease duration in rpDLB patients. Moreover, we found no differences in αSyn seeding kinetic parameters at the dilution corresponding to the SD50 (i.e., assuming equal seed dose) in any of the brain areas. This result suggests that, within the limitations of our small case series and intrinsic to the assay’s ability to distinguish different αSyn conformers, the physiochemical properties of αSyn are not significantly different between rpDLB and typical DLB. It has been indeed hypothesized that RPDs are underlain by different conformational strains than typical long-lasting degenerative dementias, in analogy to CJD, where distinct clinical-pathological subtypes (also in terms of disease duration) are determined by distinct strains of the PrPSc protein [15]. While this theory has received some experimental support for rpAD [21], our data suggest that rpDLB is unrelated to peculiar αSyn conformational strains. Future studies, possibly employing advanced structural imaging techniques such as CryoEM, should confirm this finding.
To date, the genetic characteristics of rpDLB patients have been poorly investigated. Geut et al., have described one case with a combination of two genetic variants in GBA and two cases with variants in SORL1 [13]. We identified rare variants in genes associated with PD and/or DLB (EIF4G1, VPS13C, SYNJ1, and GBA). All variants were classified as VUS, apart from the one in GBA (p.Lys196Gln), which was considered pathogenic and associated with Gaucher disease [34, 35]. Carriers harboring GBA variants have an earlier age of onset, more severe cognitive impairment, and rapid symptom progression [53], and in our case, this may have contributed to the disease’s rapidly progressive course. The three patients carrying variants in genes not normally associated with α-synucleinopathy (GRN, MYORG, and NOTCH3) were also classified as VUS and did not show any related pathological phenotype (i.e., TDP-43 inclusions, basal ganglia calcifications, and cerebral arteriopathy with leukoencephalopathy, respectively). However, we cannot exclude that functional pathway alterations related to them may have contributed to the poor prognosis in these patients.
In addition to genetic defects, several mechanisms could contribute to rapid deterioration in rpDLB. Severe mitochondrial and purine metabolism dysfunction, altered neuroinflammation, abnormal expression of nucleolar and ribosomal proteins, and deregulation of brain olfactory and taste receptors signaling have been reported in the frontal cortex of rpDLB patients [54]. Multi-omics studies are needed to dissect further the pathophysiological processes and individual predisposing factors differentially involved in rpDLB.
Limitations
This study comes with several limitations. First, its retrospective and unicentric design and the small sample size could limit the generalizability of the results. We cannot exclude that some of the included patients had a systemic condition justifying the rapidly progressive course as no whole-body autopsy was performed, however, we are confident that through the thorough examination of medical records, we have minimized this risk. Concerning the clinical section, the heterogeneity of the clinical assessment, the absence of repeated clinical evaluations, the lack of a “typical DLB” control group, and the limited availability of CSF in most cases are potential limitations. In addition, our evaluation of the αSyn pathological and molecular characteristics is limited by the fact that the LBP assessment was conducted with a single antibody (i.e., LB509), thus limiting the ability to distinguish the heterogeneous post-translational changes in different brain areas that might impact the disease course in these patients. However, the lack of differences in αSyn seeding activity reasonably ruled out (within the specificity limitations of the assay) the existence of significantly distinct αSyn conformers between the two groups. We are also aware that the absence of examination of spinal cord sections limits the clinicopathological correlation results, and, to some extent, even some of the conclusions of the study (especially related to the LBP semiquantitative assessment), however spinal cord examination is not included in the RPD autoptic protocol at our center. Finally, regarding the genetic section, the results are severely limited by the impossibility of performing segregation analyses in families of VUS carriers, by the limited availability of DNA suitable for analysis for all patients, and by the lack of a wide control group of typical DLB to explore the genetic determinants of rapid disease progression. Moreover, we did not perform WES of frozen brain tissue of rpDLB cases to investigate the potential role of somatic variants as determinants of disease duration. Future studies should address this issue. As main strengths, we compared rpDLB clinical characteristics with two large cohorts reflecting the main differential diagnoses (CJD and rpAD). Moreover, for the first time, we compared the LBP load assessed by immunohistochemistry and αSyn seeding properties estimated with SAA between rpDLB and typical LBD.
Conclusions
In conclusion, we demonstrated that: (1) rpDLB may exhibit a distinct clinical signature with atypical signs for LBD (e.g., myoclonus, pyramidal signs, akinetic mutism, and seizures), (2) some clinical variables (i.e., cognitive fluctuations, visual hallucinations, neuropsychiatric symptoms, seizures, cerebellar and visual signs, delirium onset) may aid in the differential diagnosis with CJD and rpAD; (3) neuropathological biomarkers (e.g., prion, and αSyn SAAs) are the most reliable tests for an accurate diagnostic assessment; (4) rpDLB is a heterogeneous neuropathological entity which can be underlain by both significant but isolated LBP, or low-magnitude LBD with multiple concomitant pathologies 4) rpDLB is likely not sustained by distinct αSyn conformational strains than typical LBD; (5) genetic defects may contribute to the poor prognosis in these patients. Future studies, possibly involving multi-omics techniques, should help identify the individual factors contributing to rapid clinical deterioration to carry out patient-tailored approaches.
Data availability
Anonymized data not published within this article will be made available by request from any qualified investigator.
Abbreviations
- Aβ:
-
beta amyloid
- AD:
-
Alzheimer’s Disease
- αSyn:
-
α-Synuclein
- AUC:
-
Area Under the Curve
- CAA:
-
Cerebral Amyloid Angiopathy
- CADASIL:
-
Cerebral Arteriopathy with Subcortical Infarcts and Leukoencephalopathy
- CJD:
-
Creutzfeldt-Jakob disease
- CSF:
-
Cerebrospinal Fluid
- DLB:
-
Dementia with Lewy Bodies
- DWI:
-
Diffusion Weighted Imaging
- EEG:
-
Electroencephalography
- FLAIR:
-
Fluid-Attenuated Inversion Recovery
- FTLD:
-
Frontotemporal Lobar Degeneration
- HS:
-
Hippocampal Sclerosis
- IQR:
-
Interquartile Range
- LATE:
-
Limbic-Predominant Age-Related TDP-43 Encephalopathy
- LB:
-
Lewy Body
- LBD:
-
Lewy Body Disease
- LBP:
-
Lewy Body Pathology
- LN:
-
Lewy Neurite
- MRI:
-
Magnetic Resonance Imaging
- NfL:
-
Neurofilament Light Chain
- NP:
-
Neuropathology
- PART:
-
Primary Age-Related Tauopathy
- PD:
-
Parkinson’s Disease
- PDD:
-
Parkinson’s Disease Dementia
- p-tau181:
-
phospho-tau181
- PSWCs:
-
Periodic Sharp/Wave Complexes
- rp:
-
Rapidly Progressive
- RBD:
-
REM Sleep Behaviour Disorder
- RPD:
-
Rapidly Progressive Dementia
- RT-QuIC:
-
Real-Time Quaking-Induced Conversion
- SAA:
-
Seeding Amplification Assay
- SD:
-
Standard Deviation
- SD50 :
-
50% Seeding Dose
- SVD:
-
Small Vessel Disease
- t-tau:
-
Total Tau
- VBI:
-
Vascular Brain Injury
- VUS:
-
Variant of Uncertain Significance
- WES:
-
Whole Exome Sequencing
References
Koga S, Sekiya H. Kondru N, Ross OA, Dickson DW. Neuropathology and molecular diagnosis of synucleinopathies. Mol Neurodegener. 2021;16:83.
Jellinger KA. Neuropathology and pathogenesis of extrapyramidal movement disorders: a critical update—I. Hypokinetic-rigid movement disorders. J Neural Transm. 2019;126:933–95.
Simuni T, Chahine LM, Poston K, Brumm M, Buracchio T, Campbell M et al. A biological definition of neuronal α-synuclein disease: towards an integrated staging system for research. Lancet Neurol. 2024;23:178–90.
Williams MM, Xiong C, Morris JC, Galvin JE. Survival and mortality differences between dementia with Lewy bodies vs Alzheimer disease. Neurology. 2006;67:1935–41.
Savica R, Grossardt BR, Bower JH, Ahlskog JE, Boeve BF, Graff-Radford J, et al. Survival and causes of death among people with clinically diagnosed synucleinopathies with parkinsonism. JAMA Neurol. 2017;74:839–46.
Haïk S, Brandel JP, Sazdovitch V, Delasnerie-Lauprêtre N, Peoc’h K, Laplanche JL, et al. Dementia with Lewy bodies in a neuropathologic series of suspected Creutzfeldt-Jakob disease. Neurology. 2000;55:1401–4.
Tschampa HJ, Neumann M, Zerr I, Henkel K, Schröter A, Schulz-Schaeffer WJ, et al. Patients with Alzheimer’s disease and dementia with Lewy bodies mistaken for Creutzfeldt-Jakob disease. J Neurol Neurosurg Psychiatry. 2001;71:33–9.
Van Everbroeck B, Dobbeleir I, De Waele M, De Deyn P, Martin J-J, Cras P. Differential diagnosis of 201 possible creutzfeldt-jakob disease patients. J Neurol. 2004;251:298–304.
Lemstra AW, Schoenmaker N, Rozemuller-Kwakkel A J M, Van Gool W et al. The association of neuroleptic sensitivity in Lewy body disease with a false positive clinical diagnosis of Creutzfeldt-Jakob disease. Int J Geriatr Psychiatry. 2006;21:1031–5.
Josephs KA, Ahlskog JE, Parisi JE, Boeve BF, Crum BA, Giannini C et al. Rapidly progressive neurodegenerative dementias. Arch Neurol. 2009;66:201–7.
Gaig C, Valldeoriola F, Gelpi E, Ezquerra M, Llufriu S, Buongiorno M, et al. Rapidly progressive diffuse Lewy body disease. Mov Disord. 2011;26:1316–23.
Graff-Radford J, Aakre J, Savica R, Boeve B, Kremers WK, Ferman TJ, et al. Duration and pathologic correlates of Lewy body disease. JAMA Neurol. 2017;74:310.
Geut H, Vergouw LJM, Galis Y, Ingrassia A, de Jong FJ, Quadri M, et al. Neuropathological and genetic characteristics of a post-mortem series of cases with dementia with Lewy bodies clinically suspected of Creutzfeldt-Jakob’s disease. Parkinsonism Relat Disord. 2019;63:162–8.
Alafuzoff I, Ince PG, Arzberger T, Al-Sarraj S, Bell J, Bodi I, et al. Staging/typing of Lewy body related α-synuclein pathology: a study of the BrainNet Europe Consortium. Acta Neuropathol. 2009;117:635–52.
Parchi P, de Boni L, Saverioni D, Cohen ML, Ferrer I, Gambetti P et al. Consensus classification of human prion disease histotypes allows reliable identification of molecular subtypes: an inter-rater study among surveillance centres in Europe and USA. Acta Neuropathol. 2012;124:517–29.
Montine TJ, Phelps CH, Beach TG, Bigio EH, Cairns NJ, Dickson DW, et al. National institute on Aging–Alzheimer’s association guidelines for the neuropathologic assessment of Alzheimer’s disease: a practical approach. Acta Neuropathol. 2012;123:1–11.
Dickson DW. Parkinson’s disease and parkinsonism: Neuropathology. Cold Spring Harb Perspect Med. 2012;2:a009258–009258.
McKeith IG, Boeve BF, Dickson DW, Halliday G, Taylor J-P, Weintraub D, et al. Diagnosis and management of dementia with Lewy bodies: fourth consensus report of the DLB consortium. Neurology. 2017;89:88–100.
Hermann P, Appleby B, Brandel J-P, Caughey B, Collins S, Geschwind MD, et al. Biomarkers and diagnostic guidelines for sporadic creutzfeldt-jakob disease. Lancet Neurol. 2021;20:235–46.
Baiardi S, Quadalti C, Mammana A, Dellavalle S, Zenesini C, Sambati L, et al. Diagnostic value of plasma p-tau181, NfL, and GFAP in a clinical setting cohort of prevalent neurodegenerative dementias. Alzheimers Res Ther. 2022;14:153.
Abu-Rumeileh S, Capellari S, Stanzani-Maserati M, Polischi B, Martinelli P, Caroppo P, et al. The CSF neurofilament light signature in rapidly progressive neurodegenerative dementias. Alzheimers Res Ther. 2018;10:3.
Franceschini A, Baiardi S, Hughson AG, McKenzie N, Moda F, Rossi F et al. High diagnostic value of second generation CSF RT-QuIC across the wide spectrum of CJD prions. Sci Rep. 2017;7:10655.
Bentivenga GM, Mammana A, Baiardi S, Rossi M, Ticca A, Magliocchetti F, et al. Performance of a seed amplification assay for misfolded alpha-synuclein in cerebrospinal fluid and brain tissue in relation to Lewy body disease stage and pathology burden. Acta Neuropathol. 2024;147:18.
Nelson PT, Dickson DW, Trojanowski JQ, Jack CR, Boyle PA, Arfanakis K, et al. Limbic-predominant age-related TDP-43 encephalopathy (LATE): consensus working group report. Brain. 2019;142:1503–27.
Attems J, Toledo JB, Walker L, Gelpi E, Gentleman S, Halliday G, et al. Neuropathological consensus criteria for the evaluation of Lewy pathology in post-mortem brains: a multi-centre study. Acta Neuropathol. 2021;141:159–72.
Thal DR, Griffin WST, De Vos RAI, Ghebremedhin E. Cerebral amyloid angiopathy and its relationship to Alzheimer’s disease. Acta Neuropathol. 2008;115:599–609.
Crary JF, Trojanowski JQ, Schneider JA, Abisambra JF, Abner EL, Alafuzoff I, et al. Primary age-related tauopathy (PART): a common pathology associated with human aging. Acta Neuropathol. 2014;128:755–66.
Dougherty T. Animal virus titration techniques. In: Harris RJC, editor. Techniques in experimental virology. New York Academic; 1964.
Wilham JM, Orrú CD, Bessen RA, Atarashi R, Sano R, Race K, et al. Rapid end-point quantitation of prion seeding activity with sensitivity comparable to bioassays. PLoS Pathog. 2010;6:e1001217.
Henderson DM, Davenport KA, Haley NJ, Denkers ND, Mathiason CK, Hoover EA. Quantitative assessment of prion infectivity in tissues and body fluids by real-time quaking-induced conversion. J Gen Virol. 2015;96:210–9.
Landrum MJ, Lee JM, Benson M, Brown GR, Chao C, Chitipiralla S, et al. ClinVar: improving access to variant interpretations and supporting evidence. Nucleic Acids Res. 2018;46:D1062–7.
Genoox. Franklin by Genoox. Available online: https://franklin.genoox.com. Accessed on 20 April 2024.
Wenham PR, Price WH, Blandell G. Apolipoprotein E genotyping by one-stage PCR. Lancet. 1991;337:1158–9.
Eyal N, Firon N, Wilder S, Kolodny EH, Horowitz M. Three unique base pair changes in a family with Gaucher disease. Hum Genet. 1991;87:328–32.
Manickam M, Ravanan P, Singh P, Talwar P. In silico identification of genetic variants in glucocerebrosidase (GBA) gene involved in Gaucher’s disease using multiple software tools. Front Genet. 2014;5:148.
Grau-Rivera O, Gelpi E, Nos C, Gaig C, Ferrer I, Saiz A, et al. Clinicopathological correlations and concomitant pathologies in rapidly progressive dementia: a brain bank series. Neurodegener Dis. 2015;15:350–60.
Chitravas N, Jung RS, Kofskey DM, Blevins JE, Gambetti P, Leigh RJ, et al. Treatable neurological disorders misdiagnosed as Creutzfeldt-Jakob disease. Ann Neurol. 2011;70:437–44.
Peckeu L, Delasnerie-Lauprètre N, Brandel J-P, Salomon D, Sazdovitch V, Laplanche J-L, et al. Accuracy of diagnosis criteria in patients with suspected diagnosis of sporadic Creutzfeldt-Jakob disease and detection of 14-3-3 protein. Euro Surveill. 2017;22:16–00715.
Chen L, Yang W, Yang F, Yu Y, Xu T, Wang D, et al. The crosstalk between epilepsy and dementia: a systematic review and meta-analysis. Epilepsy Behav. 2024;152:109640.
McKeith IG, Ferman TJ, Thomas AJ, Blanc F, Boeve BF, Fujishiro H, et al. Research criteria for the diagnosis of prodromal dementia with Lewy bodies. Neurology. 2020;94:743–55.
Degnan AJ, Levy LM. Neuroimaging of rapidly progressive dementias: part 1: neurodegenerative etiologies. AJNR Am J Neuroradiol. 2014;35:418–23.
Stoeck K, Sanchez-Juan P, Gawinecka J, Green A, Ladogana A, Pocchiari M, et al. Cerebrospinal fluid biomarker supported diagnosis of Creutzfeldt–Jakob disease and rapid dementias: a longitudinal multicentre study over 10 years. Brain. 2012;135:3051–61.
Lattanzio F, Abu-Rumeileh S, Franceschini A, Kai H, Amore G, Poggiolini I, et al. Prion-specific and surrogate CSF biomarkers in Creutzfeldt-Jakob disease: diagnostic accuracy in relation to molecular subtypes and analysis of neuropathological correlates of p-tau and Aβ42 levels. Acta Neuropathol. 2017;133:559–78.
Bentivenga GM, Baiardi S, Mastrangelo A, Zenesini C, Mammana A, Polischi B, et al. Diagnostic and prognostic value of cerebrospinal fluid SNAP-25 and neurogranin in Creutzfeldt-Jakob disease in a clinical setting cohort of rapidly progressive dementias. Alzheimers Res Ther. 2023;15:150.
Abu-Rumeileh S, Halbgebauer S, Bentivenga GM, Barba L, Baiardi S, Mastrangelo A, et al. High diagnostic performance of plasma and cerebrospinal fluid beta-synuclein for sporadic Creutzfeldt–Jakob disease. Ann Clin Transl Neurol. 2023;10:1904–9.
Barba L, Abu-Rumeileh S, Halbgebauer S, Bellomo G, Paolini Paoletti F, Gaetani L, et al. CSF synaptic biomarkers in AT(N)-Based subgroups of Lewy body disease. Neurology. 2023;101:e50–62.
Candelise N, Baiardi S, Franceschini A, Rossi M, Parchi P. Towards an improved early diagnosis of neurodegenerative diseases: the emerging role of in vitro conversion assays for protein amyloids. Acta Neuropathol Commun. 2020;8:117.
Saint-Aubert L, Pariente J, Dumas H, Payoux P, Brandel J-P, Puel M, et al. Case report of Lewy body disease mimicking Creutzfeldt-Jakob disease in a 44-year-old man. BMC Neurol. 2016;16:122.
Ferman TJ, Aoki N, Crook JE, Murray ME, Graff-Radford NR, van Gerpen JA, et al. The limbic and neocortical contribution of α-synuclein, tau, and amyloid β to disease duration in dementia with Lewy bodies. Alzheimers Dement. 2018;14:330–9.
Irwin DJ, Grossman M, Weintraub D, Hurtig HI, Duda JE, Xie SX, et al. Neuropathological and genetic correlates of survival and dementia onset in synucleinopathies: a retrospective analysis. Lancet Neurol. 2017;16:55–65.
Jellinger KA. Significance of cerebral amyloid angiopathy and other co-morbidities in Lewy body diseases. J Neural Transm. 2021;128:687–99.
Boyle PA, Yang J, Yu L, Leurgans SE, Capuano AW, Schneider JA, et al. Varied effects of age-related neuropathologies on the trajectory of late life cognitive decline. Brain. 2017;140:804–12.
Liu L, Li J, Quan W, Qin Y, Zhang Q, Pei X, et al. Effect of GBA gene variants on clinical characteristics of dementia with Lewy bodies: a review and meta-analyses. Neurol Sci. 2022;43:3541–50.
Garcia-Esparcia P, López-González I, Grau-Rivera O, García-Garrido MF, Konetti A, Llorens F, et al. Dementia with Lewy bodies: molecular pathology in the frontal cortex in typical and rapidly progressive forms. Front Neurol. 2017;8:89.
Acknowledgements
The authors wish to thank the patients and their caregivers for supporting the research in neurodegenerative diseases and the Italian neurologists who provided the clinical information. We thank Elisa Saltimbanco for her valuable technical assistance.
Funding
The study was supported by the Italian Ministry of Health (“Ricerca Corrente”) and the #NextGenerationEU (NGEU) funded by the Ministry of University and Research (MUR): National Recovery and Resilience Plan (NRRP): project MNESYS (PE0000006).
Author information
Authors and Affiliations
Contributions
Conceptualization and design of the study: GMB and PP. Drafting/revision of the manuscript for content, including medical writing for content: GMB and PP. Neuropathological analyses: GMB, SB, and PP. αSyn RT-QuIC SAA experiments: AM (Angela Mammana), AT, and MR. Genetic analyses: ER. Major role in the acquisition, analysis, or interpretation of data: SB, AM (Andrea Mastrangelo), ER, AM (Angela Mammana), AT, MR, SC, and PP. Statistical analysis: GMB and AT. Supervision: PP. Critical review of the manuscript and approval of the final version: all authors.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was conducted according to the revised Declaration of Helsinki and Good Clinical Practice guidelines and approved by the local ethics committee Area Vasta Emilia Centro (CE-AVEC) (approval number: 18025: 113/2018/OSS/AUSLBO). Written informed consent was given by study participants or the next of kin.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Additional file 1: Supplementary material. rpDLB patients selection
: inclusion criteria and selected rpDLB patients. CJD and rpAD cohorts selection: inclusion criteria and selected CJD and rpAD patients. Neuropathology score composition: factors included in NP score calculation. Patients and control cohorts in LBP assessment and αSyn RT-QuIC SAA experiments: demographic characteristics of LBD patients included in control cohorts. Supplementary Table 1: NP score composition. Supplementary Table 2: LB score distribution per brain area in rpDLB cases. Supplementary Table 3: variants in genes related to neurodegenerative conditions identified in rpDLB cases.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Bentivenga, G.M., Baiardi, S., Mastrangelo, A. et al. Clinical, neuropathological, and molecular characteristics of rapidly progressive dementia with Lewy bodies: a distinct clinicopathological entity?. Alz Res Therapy 16, 201 (2024). https://doi.org/10.1186/s13195-024-01565-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-024-01565-x