Abstract
Background
Blood-based neurofilament light chain (NfL) is a promising biomarker of neurodegeneration across multiple neurodegenerative diseases. However, blood-based NfL is highly associated with renal function in older adults, which leads to the concern that blood-based NfL levels may be influenced by renal function, rather than neurodegeneration alone. Despite growing interest in using blood-based NfL as a biomarker of neurodegeneration in research and clinical practices, whether renal function should always be accounted for in these settings remains unclear. Moreover, the mechanisms underlying this association between blood-based measures of NfL and renal function remain elusive. In this study, we first evaluated the effect of renal function on the associations of plasma NfL with other measures of neurodegeneration. We then examined the extent of genetic and environmental contributions to the association between plasma NfL and renal function.
Methods
In a sample of 393 adults (mean age=75.22 years, range=54–90), we examined the associations of plasma NfL with cerebrospinal fluid (CSF) NfL and brain volumetric measures before and after adjusting for levels of serum creatinine (an index of renal function). In an independent sample of 969 men (mean age=67.57 years, range=61–73) that include monozygotic and dizygotic twin pairs, we replicated the same analyses and leveraged biometrical twin modeling to examine the genetic and environmental influences on the plasma NfL and creatinine association.
Results
Plasma NfL’s associations with cerebrospinal fluid NfL and brain volumetric measures did not meaningfully change after adjusting for creatinine levels. Both plasma NfL and creatinine were significantly heritable (h2=0.54 and 0.60, respectively). Their phenotypic correlation (r=0.38) was moderately explained by shared genetic influences (genetic correlation=0.46) and unique environmental influences (unique environmental correlation=0.27).
Conclusions
Adjusting for renal function is unnecessary when assessing associations between plasma NfL and other measures of neurodegeneration but is necessary if plasma NfL is compared to a cutoff for classifying neurodegeneration-positive versus neurodegeneration-negative individuals. Blood-based measures of NfL and renal function are heritable and share common genetic influences.
Similar content being viewed by others
Background
Blood-based biomarkers have garnered increasing attention from clinical and research communities for their low invasiveness and utility in the detection and monitoring of neurodegenerative pathophysiology [1]. As a biomarker of neurodegeneration, the neuron-specific heteropolymer neurofilament light chain (NfL) is an axoskeletal protein that maintains large-caliber myelinated axons and is released into the extracellular space following neuroaxonal damage [2, 3]. Elevated NfL concentrations are detected in both cerebrospinal fluid (CSF) and blood in mild cognitive impairment (MCI), Alzheimer’s disease (AD), frontotemporal dementias, traumatic brain injury, and other neurological conditions [1, 3].
Despite the diagnostic and prognostic potential of blood-based NfL (measured in either plasma or serum) across multiple neurological disorders [2,3,4,5,6], there have been growing calls for caution in interpreting elevated blood-based NfL levels as an indicator of neurodegeneration in older populations without considering common underlying comorbidities that also influence its concentration [5, 7,8,9,10,11,12]. Specific comorbidities associated with higher blood-based NfL levels include chronic kidney disease, neurological conditions (e.g., stroke), and cardiovascular diseases [10, 11]. Notably, declining renal function, but not increasing number of comorbidities in older adults, has been associated with elevated blood-based NfL levels [13]. Indeed, levels of blood-based NfL are correlated with multiple blood-based measures of renal function (r=±0.49–0.56), including serum creatinine, cystatin C, and estimated glomerular filtration rate, in both healthy older adults and those with diabetes [5, 7,8,9,10, 13]. Even after controlling for known confounding factors of blood-based NfL such as age and body mass index [7,8,9, 13], these associations remain. Thus, diminished renal function in older adults appears to be one of the strongest comorbidities contributing to elevated blood-based NfL levels.
Given the growing interest in using blood-based NfL in research and clinical practices [5, 12, 14], as well as the emerging emphasis on considering the impact of comorbidities on blood-based biomarkers of neurodegenerative disorders to avoid potential misdiagnosis [10,11,12, 15], there is a critical need to evaluate the impact of renal function on blood-based NfL levels with respect to the associations of blood-based NfL with other measures of neurodegeneration unrelated to renal function [1] and investigate the mechanisms underlying this blood-based NfL and renal function association [2]. Addressing these questions would inform best practices in research and clinical settings that use blood-based NfL to index neurodegeneration and enable a better understanding of the nature of these associations.
Because CSF NfL may be a more direct measure of neurodegeneration less influenced by peripheral clearance than blood-based NfL measured in either plasma or serum [16], we first examined whether the association between plasma NfL and CSF NfL changes after controlling for serum creatinine levels (i.e., an index of renal function) in 396 older adults (mean age=75.17 years) (study 1). We also ascertained whether associations between brain volumetric measures, which are alternate indices of neurodegeneration, and plasma NfL are affected by creatinine levels. Any substantial changes in these associations would indicate that renal function is a major factor influencing the accuracy of plasma NfL as a biomarker of neurodegeneration. Next, in a slightly younger sample of 969 community-dwelling twin men (mean age=67.57 years), we replicated the same analyses examining the effect of renal function on plasma NfL’s associations with other measures of neurodegeneration. Finally, we leveraged biometrical twin modeling to determine the extent to which the association between plasma NfL and renal function (i.e., serum creatinine) is explained by shared genetic and environmental influences (study 2).
Methods
Participants
Study 1
To examine the associations among serum creatinine, CSF NfL, and plasma NfL, we obtained publicly available biomarker data from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). The ADNI was launched in 2003 as a public-private partnership, led by principal investigator Michael W. Weiner, MD. The primary goal of ADNI has been to test whether serial magnetic resonance imaging, positron emission tomography, other biological markers, and clinical and neuropsychological assessment can be combined to measure the progression of MCI and early AD. In the current study, we used the ADNI1 dataset. Hereafter, we referred to the dataset as ADNI. Of the 572 participants with usable data for at least two biomarkers, we excluded 176 participants who had a clinical diagnosis of AD and 3 participants with stage 4 chronic kidney disease, resulting in a total of 396 ADNI participants who fell within stage 1 (normal) to stage 3 (moderate) chronic kidney disease (estimated glomerular filtration rate (eGFR) ≥ 30 ml/min/1.73 m2) (mean age=75.22 years, SD=6.35; range=54–90) (Table 1). The small set of stage 4 chronic kidney disease participants (N=3) was excluded because of their extreme outlying data points.
Study 2
To replicate the analyses from study 1 in an independent sample, as well as examine the genetic and environmental contributions to the NfL-renal function association, we examined 974 community-dwelling male-male twins from wave 3 of the Vietnam Era Twin Study of Aging (VETSA) with available biomarker data. VETSA is a multisite national longitudinal study of aging and risk for AD beginning in middle age [17]. All participants served in the US military some time between 1965 and 1975. Approximately 80% report no combat exposure. Moreover, they are similar to American men in their age range with respect to health, education, and lifestyle characteristics [18]. All traveled to the University of California San Diego or Boston University for the VETSA project. Informed consent was obtained from all participants and institutional review boards at both sites approved all protocols.
Of the 974 participants with usable data, 5 who met the criteria for stage 4 (severe) or stage 5 (end stage) chronic kidney disease (eGFR < 30 ml/min/1.73 m2) were excluded, resulting in a total of 969 participants who fell within stage 1 (normal) to stage 3 (moderate) chronic kidney disease (mean age=67.57 years, SD=2.52; range=61–73). The small set of stage 4 and 5 chronic kidney disease participants (N=5) were excluded because of their extreme outlying data points. There were 218 monozygotic (MZ) pairs, 151 dizygotic (DZ) pairs, and 231 unpaired individuals (i.e., participants whose co-twin had no available data) (Table 2).
Blood collection and processing
For ADNI participants, plasma and serum samples were collected under fasting conditions. NfL was measured from plasma samples, and creatinine was measured from serum samples. Fasting began overnight (approximately 8 h) before collection in the morning. All plasma samples were processed per ADNI laboratory standard operating procedures (http://adni.loni.ucla.edu). Plasma NfL was measured with an ultrasensitive single-molecule array (Simoa) platform using a home brew kit (Simoa Homebrew Assay Development Kit; Quanterix Corporation), as described previously [19]. The assay uses a combination of monoclonal antibodies and purified bovine NfL as a calibrator. The standard exclusion criteria included hemolysis and a coefficient of variation in plasma concentrations >.25. For serum samples, they were processed by Covance Laboratory kits using isotope dilution mass spectrometry as part of the clinical lab data generated for ADNI.
For VETSA participants, plasma and serum samples were collected under fasting conditions. NfL was measured from plasma samples, and creatinine was measured from serum samples. Fasting began by 9:00 PM the night before testing, and samples were acquired the following morning between 8:00 AM and 8:15 AM. For plasma samples, NfL was assayed on a single-plex plate using the ultra-sensitive Simoa technology platform HD-1 (Simoa NFL Advantage Kit; Quanterix Corporation) by the USC Alzheimer’s Therapeutic Research Institute Biomarker Core (PI: Dr. Robert Rissman) [20], and all assays were performed according to the manufacturer’s instructions. The standard exclusion criteria included hemolysis and a coefficient of variation in plasma concentrations >.20. For serum samples, they were processed by the Quest Diagnostic using spectrophotometry as part of the blood chemistry data generated for VETSA.
Cerebrospinal fluid collection and processing
For ADNI participants, cerebrospinal fluid (CSF) was sampled by lumbar puncture per ADNI laboratory standard operating procedures (http://adni.loni.ucla.edu) on the same day of the blood draw for plasma NfL. The CSF NfL concentration was measured using a commercially available enzyme-linked immunosorbent assay (ELISA) following the protocol provided by the manufacturer (NF-light; Uman Diagnostics) as described previously [21]. Intra-assay coefficients of variation were <10%. Additional procedures for CSF collection, processing, and storage procedures have been described previously [22].
MRI acquisition and processing
For ADNI, acquisition parameters have been described in detail previously [23]. Briefly, T1-weighted images for ADNI were collected from 3.0-T scanners, using protocols optimized for each scanner system. Detailed acquisition parameters can be found at https://adni.loni.usc.edu/methods/documents/mri-protocols/. Total cortical, medial temporal lobe, and hippocampal volume measures (UCSFFSX51_ADNI1_3T_02_01_16.csv) were derived using the FreeSurfer 5.1 (surfer.nmr.mgh.harvard.edu) software package. For more detailed information on preprocessing and quality control, please see the full UCSF FreeSurfer Overview and QC Guide and UCSF FreeSurfer Methods in the ADNI database.
For VETSA, acquisition parameters have been described in detail previously [24, 25]. Briefly, T1-weighted images (sagittal 3D fast spoiled gradient echo (FSPGR), TE = 3.164 ms, TR = 8.084 ms) were acquired on two General Electric (GE) Discovery MR750 3.0T scanners (GE Healthcare, Waukesha, WI, USA) at UCSD with an eight-channel phased array head coil. The structural MR images were processed as described previously [24,25,26]. Total cortical, medial temporal lobe, and hippocampal volume measures were derived using the FreeSurfer 6.0 (surfer.nmr.mgh.harvard.edu) software package. Preprocessing included correction of distortion due to gradient nonlinearity, image intensity normalization, and rigid registration into standard orientation with 1 mm isotropic voxel size. All images required some form of manual intervention to ensure the correct classification of the white matter and pial surfaces, either with normalization control points or manual editing of white matter or brain masks. Problematic cortical reconstructions were reviewed by consensus with 3 neuroimaging analysts.
Statistical analyses
Statistical analyses were performed using R version 4.1.2. Correlational analyses for study 1 and twin analyses for study 2 were performed using the raw data application of the maximum likelihood-based structural equation modeling software OpenMx version 2.19.8 [27]. For ADNI participants, serum creatinine, plasma NfL, and CSF NfL were adjusted for (1) age, (2) race/ethnicity (White/non-Hispanic or others), and (3) body mass index, using the umx_residualize() function [24]. Information on the storage time of blood samples was not available for ADNI data. The testing site was not adjusted given the blood collection protocols were standardized across sites. For VETSA participants, measures of serum creatinine and plasma NfL were residualized using the umx_residualize() function [28] to account for (1) age, (2) race/ethnicity (White/non-Hispanic or others), (3) body mass index, and (4) whether or not twin pairs were assessed on the same day. Plasma NfL was additionally adjusted for testing site and sample storage time. Residualized scores of all measures from both datasets were then log-transformed to improve their distribution properties. For each measure, data points that were more than three times the interquartile range above the third quartile were excluded from further analyses. For the ADNI sample, 2 plasma NfL data points, 2 CSF NfL data points, and 1 serum creatinine data point were excluded. For the VETSA sample, 3 plasma NfL data points were excluded.
Brain volumetric measures in both samples were residualized to account for (1) age, (2) race/ethnicity (White/non-Hispanic or others), and (3) intracranial volume. Sex was adjusted for in the ADNI sample. Scanner differences were adjusted for the VETSA sample, but not the ADNI sample as the data were standardized across collection sites.
Biometrical twin analyses
To determine the relative contributions of genetic and environmental influences on the variance in creatinine and plasma NfL, we fitted univariate and bivariate biometrical models to the data. In univariate twin analysis, the variance in a phenotype (e.g., biomarker) is decomposed into additive genetic (A) influences, common or shared environmental (C) influences (i.e., environmental factors that make members of a twin pair similar to one another), and non-shared or unique environmental (E) influences (i.e., environmental factors that make members of a twin pair different from one another, including measurement error) (Fig. 1A) [29, 30]. This approach is also referred to as the biometrical “ACE” model.
Biometrical twin modeling. A Univariate biometrical ACE model. A = additive genetic influences, C = common/shared environmental influences, E = unique environmental influences, ramz = correlation within MZ twin pairs, radz = correlation within DZ twin pairs, rc = correlation within MZ and DZ twin pairs. B Bivariate correlated factor model with creatinine and plasma NfL. For simplicity, only one twin is shown for the bivariate model. Genetic (rg), common environmental (rc), and unique environmental (re) correlations between the two biomarkers were estimated
The decomposition is achieved by exploiting the expected genetic and environmental correlations between MZ and DZ twin pairs. MZ twin pairs are genetically identical, whereas DZ twin pairs share, on average, half of their genes. Therefore, the MZ and DZ twin pair correlations for the additive genetic effects are fixed to rA=1.0 and rA=0.5, respectively. The modeling assumes that the sharing of environmental effects (C) is equal in MZ and DZ twin pairs (rC=1.0), while non-shared environmental effects (E) are, by definition, uncorrelated within twin pairs and include measurement errors. The biometrical “ACE” model based on twins reared together also assumes no genotype by environmental interactions or correlations and non-random mating.
In bivariate twin analyses, the univariate model is extended to estimate the A, C, and E within each biomarker and the magnitude and significance of shared genetic and environmental influences between the two biomarkers. Specifically, we fitted a bivariate ACE “correlated factors” model [31] to the data (Fig. 1B) to estimate the genetic and environmental correlations that represent the degree to which genetic and environmental influences are shared between biomarkers.
For both univariate and bivariate analyses, we determined the most likely sources of variance by fitting a series of competing sub-models (AE, CE, and E) in which the (i) C, (ii) A, and (iii) C and A influences were dropped and fixed to 0. The sub-models were then compared to the full ACE model using the likelihood ratio chi-square tests. The best-fitting model was determined based on the optimal balance of complexity and explanatory power by using the Akaike Information Criterion (AIC) [32] and likelihood ratio chi-square tests.
Results
Associations of biomarkers with covariates
For ADNI participants, we found that age at assessment (β=0.99, t=4.88, p<0.001) and body mass index (β=− 0.95, t=− 2.96, p=0.003) were the two covariates showing significant associations with plasma NfL. For CSF NfL, age at assessment was a significant covariate (β=28.20, t=3.20, p=0.002). For serum creatinine, age at assessment (β=0.01, t=3.40, p<0.001) and body mass index (β=0.01, t=3.41, p<0.001) were significant covariates. Race/ethnicity was not associated with individual differences in any of the biomarkers.
For VETSA participants, we found that age at assessment (β=0.28, t=3.19, p=0.001) and body mass index (β=− 0.12, t=− 2.80, p=0.005) were the two covariates showing significant associations with plasma NfL. For serum creatinine, only body mass index was a significant covariate (β=0.003, t=2.36, p=0.018). Individuals in the White/non-Hispanic group had lower serum creatinine than those in the other group (β=− 0.07, t=− 3.11, p=0.002). Whether or not twins were assessed on the same day was not associated with individual differences in any of the biomarkers. Likewise, testing sites and sample storage time were not associated with plasma NfL.
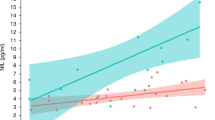
Study 1: Associations among plasma NfL, CSF NfL, and serum creatinine
Consistent with prior work [16], we detected a correlation between plasma NfL and CSF NfL with similar magnitudes in the ADNI dataset (full sample: r=0.53, 95% CI: 0.44–0.61, p<0.001; male: r=0.56, 95% CI: 0.45–0.66, p<0.001; female: r=0.54, 95% CI: 0.41–0.66, p<0.001). Likewise, plasma NfL and creatinine were significantly correlated (r=0.26, 95% CI: 0.17–0.35, p<0.001), but the correlations appeared to be numerically but not significantly stronger in males (r=0.39, 95% CI: 0.27–0.49, p<0.001) than in females (r=0.22, 95% CI: 0.06–0.37, p=0.006). Creatinine and CSF NfL were modestly correlated in the full sample (r=0.14, 95% CI: 0.03–0.24, p=0.013) but no longer correlated after controlling for sex (r=0.06, 95% CI: − 0.05–0.17, p>0.05) or separating the sample by sex (male: r=0.04, 95% CI: − 0.10–0.17, p>0.05; female: r=0.08, 95% CI: − 0.10–0.26, p>0.05) (Fig. 2).
Next, we examined whether statistically controlling for the effect of creatinine on plasma NfL alters its association with CSF NfL. If plasma NfL level is affected by renal function and does not solely reflect neurodegeneration, then adjusting plasma NfL for creatinine could significantly change its association with CSF NfL. After adjustment, there was a negligible change (±0.02) in the magnitude of correlations between plasma NfL and CSF NfL (full sample: r=0.51, 95% CI: 0.41–0.59, p<0.001; male: r=0.58, 95% CI: 0.47–0.67, p<0.001; female: r=0.56, 95% CI: 0.42–0.67, p<0.001). Analyses on brain volumetric measures revealed the same patterns, such that plasma NfL’s correlations with these measures differed little (±0.03) after adjusting for creatinine in the ADNI sample (Table 3 top panel).
Study 2: Replications and twin analyses
We replicated the same analyses examining the associations between plasma NfL and brain volumetric measures before and after adjusting for creatinine levels in the VETSA sample. Not surprisingly, these associations did not meaningfully change (±0.02) (Table 3 bottom panel). Similarly, consistent with prior findings [7, 8, 13] and results in the ADNI sample, the phenotypic correlation between creatinine and plasma NfL was significant (r=0.38, 95% CI: 0.32–0.43, p<0.001). The DZ twin pair correlations (creatinine: r=0.31, 95% CI: 0.15–0.46, p<0.001; plasma NfL: r=0.23, 95% CI: 0.06–0.38, p=0.008) were less than or equal to one-half the size of MZ twin pair correlations (creatinine: r=0.64, 95% CI: 0.56–0.71, p<0.001; plasma NfL: r=0.57, 95% CI: 0.48–0.65, p<0.001), which is consistent with additive genetic influences.
Tests of mean and variance homogeneity
Prior to the twin modeling, we tested the assumption of mean and variance homogeneity within and across the MZ and DZ twin groups for each biomarker using the residualized data. We compared the constrained models that equated mean and variance between and across zygosity to a fully saturated model that perfectly reproduced all mean and variance-covariance information for each biomarker.
We conducted the chi-square tests to compare the constrained models to the fully saturated model. A significant change in chi-square (p=0.05, Bonferroni corrected p=0.01) would suggest that there is a significant difference between the models (i.e., actual mean and variance vs. constrained mean and variance), indicating that the assumption of mean and variance homogeneity is violated. As shown in Table 4, constraining the means and variances to be equal within twin pairs and across zygosity resulted in a significant change in chi-square for creatinine (p<0.01), but not for NfL (p>0.01). This was likely attributable to the small numbers of complete and incomplete twin pairs within each zygosity group. Notwithstanding this limitation, all subsequent analyses proceeded under the assumption of mean variance homogeneity for each biomarker.
We also tested the assumption of mean and variance homogeneity by comparing the bivariate correlated factor model to a fully saturated model that reproduces perfectly all mean and variance-covariance information for the observed variables. Although the bivariate ACE model resulted in a significant difference in fit compared to the fully saturated model, all other fit indices (i.e., lower AIC, CFI>0.9, RMSEA<0.05) suggested that the bivariate model fits the data well.
Estimation of genetic and environmental influences
In both univariate and bivariate twin analyses, the AE models provided the best fitting to the data as judged by the lowest AIC values and non-significant changes in − 2 log-likelihood (-− 2LL) when compared to the ACE models (Table 5). Univariate and bivariate analyses yielded essentially identical estimates of A and E for both biomarkers.
Here, we report the bivariate results, as they provide more precise estimates than univariate analyses. Additive genetic influences accounted for 60% (95% CI: 52–67%) of the variance in creatinine and 54% (95% CI: 45–62%) of the variance in plasma NfL, and there was a significant genetic correlation between them (rg=0.46, 95% CI: 0.34–0.57, p<0.001). There was also a smaller but significant non-shared environmental correlation between the biomarkers (re=0.27, 95% CI: 0.15–0.38, p<0.001).
Discussion
Considering comorbidities in research and clinical practice using blood-based biomarkers of neurodegenerative disorders is critical for establishing generalizable cutoffs under different contexts of use and avoiding potential misdiagnosis in real-world settings [10, 11, 15]. In two different study samples, we examined how renal function impacts plasma NfL levels and their accuracy in reflecting neurodegeneration. We showed that adjusting for the effect of serum creatinine levels (i.e., renal function) on plasma NfL levels did not meaningfully change plasma NfL’s association with CSF NfL or brain volumetric measures that index neurodegeneration. To tease apart the underlying mechanisms of the NfL-renal function association, we leveraged twin modeling to show that not only were plasma NfL and creatinine both heritable (h2=0.54 and 0.60, respectively), but also their association was accounted for to a moderate degree by shared genetic factors, with the remaining variance accounted for by unique environmental factors.
A previous study showed that among all known factors associated with blood-based NfL, body mass index was the only significant factor associated with blood-based NfL levels in individuals less than 60 years old. In those who are greater than 60 years old, however, blood-based measures of renal function (i.e., creatinine, eGFR) became significantly correlated with blood-based NfL levels [8]. Indeed, studies that showed associations were all in samples above the age of 60 [7, 8, 13], during which diminished renal function becomes more common and/or may be more difficult to compensate for. Our observed phenotypic associations between creatinine and plasma NfL in the ADNI sample with a mean age of 75 years and in the VETSA sample with a mean age of 67 years are consistent with those findings. As such, one prominent hypothesis is that renal dysfunction in old age, albeit not reaching the end or severe stages of chronic kidney disease, may reduce the peripheral clearance of NfL in the blood [7, 10, 13]. In fact, it has been suggested that smaller fragments of NfL resulting from neurodegeneration or metabolism of NfL could be filtered at the glomerular level in the kidney [13]. Thus, renal dysfunction in old age may lead to the accumulation of these fragments, which may then be recognized by the NfL antibody in blood-based assays [13].
Using biometrical twin modeling, our results from the VETSA sample offered unique insights into the association between plasma NfL and serum creatinine by showing the extent of overlapping genetic influences. These findings may lay the groundwork for future genome-wide association studies (GWAS), which would be able to identify what the shared genes are and provide more information on potential cellular and molecular pathways involving both biomarkers. If peripheral clearance through the kidney [33,34,35] is indeed what contributes to the association between blood-based measures of renal function and NfL, then the detection of genes related to renal clearance in GWAS would provide concrete evidence in support of this hypothesis. Nonetheless, more large-scale studies are needed to validate our findings and empirically test the clearance hypothesis at molecular and cellular levels.
For researchers and clinicians, one major concern regarding the association between blood-based measures of renal function (in this case serum creatinine) and NfL is that reduced clearance of blood NfL fragments may increase the level of plasma NfL, thereby reflecting an inaccurate and potentially inflated estimate of neurodegeneration [7, 8, 13]. If poor renal function weakens the relationship between plasma NfL and other measures of neurodegeneration, then creatinine should always be controlled for when using plasma NfL as a biomarker of neurodegeneration. Alternatively, if poor renal function is associated with increased neurodegeneration, the association between plasma NfL and creatinine could be driven by a common process. In this case, creatinine should not be controlled for when measuring plasma NfL. The associations of plasma NfL with CSF NfL in the ADNI sample and with brain volumetric measures in both samples were unaffected by creatinine levels. Thus, we speculate that the portion of the variance in plasma NfL that is related to neurodegeneration is independent from the variance related to renal clearance (Fig. 3A). Consequently, covarying for creatinine levels in plasma NfL would not meaningfully alter the strength and direction of its associations with other markers of neurodegeneration. We thus recommend not adjusting for creatinine levels in such analyses.
Conceptual diagram of plasma NfL, CSF NfL, and serum creatinine. A Venn diagram of the associations among plasma NfL, CSF NfL, and serum creatinine. Shared variance between plasma NfL and serum creatinine is independent of the shared variance between plasma NfL and CSF NfL. B Conceptual plot of plasma NfL indexing the same degree of neurodegeneration in groups with good or poor renal function and in groups after controlling for renal function. Renal function affects the level of plasma NfL and therefore how it performs as a stand-alone measure (e.g., when compared to a threshold for abnormality as shown in the green line). However, adjusting for renal function does not alter the slope of association between plasma NfL and another measure of neurodegeneration
However, renal function and potentially other health conditions (see [5] for an example approach) should be accounted for when plasma NfL is compared to a cutoff to classify individuals as positive or negative for neurodegeneration [13, 14, 36]. This is because the level of plasma NfL is determined by the full variance of plasma NfL, including that shared with renal function (i.e., the entire plasma NfL circle in Fig. 3A). As shown in extant literature [10, 11], individuals or groups with poor renal function tend to have higher plasma NfL than those with good renal function. Thus, the 2 groups based on renal function may have different plasma NfL levels, but may not differ on neurodegeneration (Fig. 3B). Thus, for this purpose, adjusting for renal function may be necessary to ensure comparable estimates and categorization of neurodegeneration across groups or among individuals with varying levels of renal function. Relatedly, when comparing the associations of plasma NfL with other measures among the groups with a significant mean difference in renal function, investigators may run into Simpson’s paradox [37] (i.e., when an association in the full sample disappears or reverses when it is divided into subgroups) and would need to adjust for renal function to reveal the more accurate relationship.
Finally, our study has some limitations. First, the twin sample only has male participants. Thus, we cannot determine if there are sex differences in the genetic and environmental influences on these biomarkers. However, our results from the ADNI sample and prior reports all detected a phenotypic association between blood-based measures of NfL and renal function in both sexes with comparable magnitudes, suggesting no sex difference in the association [7,8,9, 13]. Second, because both samples are largely White, non-Hispanic, our results may not be generalizable to other racial/ethnic groups. Third, different collection and processing procedures of the biomarkers between the two studies may lead to potential differences in biomarker levels. For example, storage time differences between the two studies may lead to potential differences in biomarker levels. Serum creatinine was processed differently between the two datasets (spectrophotometry vs. isotope dilution mass spectrometry) at two different laboratories. Additionally, plasma NfL was processed using different kits (Simoa Homebrew Assay Development Kit vs. Simoa NFL Advantage Kit). Fourth, different ages and proportions of MCI cases (see Tables 1 and 2) between the two studies may lead to differences in mean biomarker levels. However, despite those differences, results from both studies on the association between plasma NfL and creatinine were consistent, strongly supporting the generalizability of our findings. Fifth, our samples focused on older adults with mean ages of 67 and 75, which may not generalize to younger age groups. For individuals that are less than 60–65 years of age, the diagnostic cutoffs for plasma NfL levels [14, 36] and the association between plasma NfL and creatinine [8] may be different from those in the older age groups. Sixth, our study only examined one measure of renal function (i.e., serum creatinine), but other indices of renal function such as cystatin C, which has been reported to have high sensitivity for detecting renal impairment [13], could also be examined in relation to plasma NfL. We expect similar genetic and environmental influences would be detected in other blood-based measures of renal function, as similar phenotypic associations have been observed across different measures of renal function [13].
Conclusions
Taken together, the present study is the first to investigate whether adjusting for renal function alters plasma NfL’s accuracy in indexing neurodegeneration and examine the genetic and environmental determinants of the associations between blood-based measures of NfL and renal function. In two different study samples, we showed that adjusting for creatine levels is unlikely to affect correlations between plasma NfL and other measures of neurodegeneration, but it is likely to be important if plasma NfL is compared to a cutoff for classifying neurodegeneration-positive versus neurodegeneration-negative individuals. Future work would benefit from comparing the associations of NfL obtained from the blood and CSF with different biomarkers of renal function in both younger and older age groups to better understand the nature of their relationships.
Availability of data and materials
The Alzheimer’s Disease Neuroimaging Initiative (ADNI) dataset is publicly available on its database (http://adni.loni.usc.edu). The Vietnam Era Twin Study of Aging dataset is publicly available to qualified researchers, with restrictions. Information regarding data access can be found at http://www.vetsatwins.org/for-researchers/.
Abbreviations
- AD:
-
Alzheimer’s disease
- AIC:
-
Akaike Information Criterion
- CFI:
-
Comparative fit index
- CSF:
-
Cerebrospinal fluid
- DZ:
-
Dizygotic
- eGFR:
-
Estimated glomerular filtration rate
- GWAS:
-
Genome-wide association studies
- MCI:
-
Mild cognitive impairment
- MZ:
-
Monozygotic
- NfL:
-
Neurofilament light chain
- RMSEA:
-
Root mean square error of approximation
References
Ashton NJ, Hye A, Rajkumar AP, Leuzy A, Snowden S, Suarez-Calvet M, et al. An update on blood-based biomarkers for non-Alzheimer neurodegenerative disorders. Nat Rev Neurol. 2020;16(5):265–84.
Khalil M, Teunissen CE, Otto M, Piehl F, Sormani MP, Gattringer T, et al. Neurofilaments as biomarkers in neurological disorders. Nature Reviews Neurology. 2018;14(10):577–89.
Gaetani L, Blennow K, Calabresi P, Di Filippo M, Parnetti L, Zetterberg H. Neurofilament light chain as a biomarker in neurological disorders. J Neurol Neurosurg Psychiatry. 2019;90(8):870–81.
Mielke MM, Syrjanen JA, Blennow K, Zetterberg H, Vemuri P, Skoog I, et al. Plasma and CSF neurofilament light: relation to longitudinal neuroimaging and cognitive measures. Neurology. 2019;93(3):e252–60.
Fitzgerald KC, Sotirchos ES, Smith MD, Lord HN, DuVal A, Mowry EM, et al. Contributors to serum NfL levels in people without neurologic disease. Ann Neurol. 2022;92(4):688–98.
Teunissen CE, Verberk IMW, Thijssen EH, Vermunt L, Hansson O, Zetterberg H, et al. Blood-based biomarkers for Alzheimer’s disease: towards clinical implementation. Lancet Neurol. 2022;21(1):66–77.
Akamine S, Marutani N, Kanayama D, Gotoh S, Maruyama R, Yanagida K, et al. Renal function is associated with blood neurofilament light chain level in older adults. Scientific Reports. 2020;10(1):20350.
Koini M, Pirpamer L, Hofer E, Buchmann A, Pinter D, Ropele S, et al. Factors influencing serum neurofilament light chain levels in normal aging. Aging (Albany NY). 2021;13(24):25729–38.
Korley FK, Goldstick J, Mastali M, Van Eyk JE, Barsan W, Meurer WJ, et al. Serum NfL (neurofilament light chain) levels and incident stroke in adults with diabetes mellitus. Stroke. 2019;50(7):1669–75.
Syrjanen JA, Campbell MR, Algeciras-Schimnich A, Vemuri P, Graff-Radford J, Machulda MM, et al. Associations of amyloid and neurodegeneration plasma biomarkers with comorbidities. Alzheimers Dement. 2022;18(6):1128–40.
O’Bryant SE, Petersen M, Hall J, Johnson LA, Team H-HS. Medical comorbidities and ethnicity impact plasma Alzheimer’s disease biomarkers: important considerations for clinical trials and practice. Alzheimers Dement. 2022.
Hansson O, Edelmayer RM, Boxer AL, Carrillo MC, Mielke MM, Rabinovici GD, et al. The Alzheimer’s Association appropriate use recommendations for blood biomarkers in Alzheimer’s disease. Alzheimers Dement. 2022;n/a(n/a).
Ladang A, Kovacs S, Lengele L, Locquet M, Reginster JY, Bruyere O, et al. Neurofilament light chain concentration in an aging population. Aging Clin Exp Res. 2022;34(2):331–9.
Ashton NJ, Janelidze S, Al Khleifat A, Leuzy A, van der Ende EL, Karikari TK, et al. A multicentre validation study of the diagnostic value of plasma neurofilament light. Nat Commun. 2021;12(1):3400.
Schindler SE, Karikari TK. Comorbidities confound Alzheimer’s blood tests. Nat Med. 2022;28(7):1349–51.
Alagaratnam J, von Widekind S, De Francesco D, Underwood J, Edison P, Winston A, et al. Correlation between CSF and blood neurofilament light chain protein: a systematic review and meta-analysis. BMJ Neurol Open. 2021;3(1): e000143.
Kremen WS, Franz CE, Lyons MJ. Current status of the Vietnam Era Twin Study of Aging (VETSA). Twin Res Hum Genet. 2019;22(6):783–7.
Schoenborn CA, Heyman KM. Health characteristics of adults aged 55 years and over: United States, 2004–2007. Natl Health Stat Report. 2009;16:1–31.
Mattsson N, Andreasson U, Zetterberg H, Blennow K. Alzheimer’s Disease Neuroimaging I. association of plasma neurofilament light with neurodegeneration in patients with Alzheimer disease. JAMA Neurol. 2017;74(5):557–66.
O’Bryant S, Petersen M, Hall J, Johnson L, Yaffe K, Braskie M, et al. Characterizing plasma NfL in a community-dwelling multi-ethnic cohort: results from the HABLE study. Alzheimers Dement. 2022;18(2):240–50.
Zetterberg H, Skillback T, Mattsson N, Trojanowski JQ, Portelius E, Shaw LM, et al. Association of cerebrospinal fluid neurofilament light concentration with Alzheimer disease progression. JAMA Neurol. 2016;73(1):60–7.
Shaw LM, Vanderstichele H, Knapik-Czajka M, Clark CM, Aisen PS, Petersen RC, et al. Cerebrospinal fluid biomarker signature in Alzheimer’s disease neuroimaging initiative subjects. Ann Neurol. 2009;65(4):403–13.
Jack CR Jr, Bernstein MA, Fox NC, Thompson P, Alexander G, Harvey D, et al. The Alzheimer’s Disease Neuroimaging Initiative (ADNI): MRI methods. J Magn Reson Imaging. 2008;27(4):685–91.
Hatton SN, Franz CE, Elman JA, Panizzon MS, Hagler DJ Jr, Fennema-Notestine C, et al. Negative fateful life events in midlife and advanced predicted brain aging. Neurobiol Aging. 2018;67:1–9.
Kremen WS, Beck A, Elman JA, Gustavson DE, Reynolds CA, Tu XM, et al. Influence of young adult cognitive ability and additional education on later-life cognition. Proc Natl Acad Sci U S A. 2019;116(6):2021–6.
Eyler LT, Chen CH, Panizzon MS, Fennema-Notestine C, Neale MC, Jak A, et al. A comparison of heritability maps of cortical surface area and thickness and the influence of adjustment for whole brain measures: a magnetic resonance imaging twin study. Twin Res Hum Genet. 2012;15(3):304–14.
Boker S, Neale MC, Maes H, Wilde M, Spiegel M, Brick T, et al. OpenMx: an open source extended structural equation modeling framework. Psychometrika. 2011;76:306–17.
Bates TC, Maes H, Neale MC. umx: twin and path-based structural equation modeling in R. Twin Res Hum Genet. 2019;22(1):27–41.
Eaves LJ, Last KA, Young PA, Martin NG. Model-fitting approaches to the analysis of human behavior. Heredity. 1978;41:249–320.
Neale MC, Cardon LR. Methodology for genetic studies of twins and families. Dordrecht, The Netherlands: Kluwer; 1992.
Verhulst B, Prom-Wormley E, Keller M, Medland S, Neale MC. Type I error rates and parameter bias in multivariate behavioral genetic models. Behav Genet. 2019;49(1):99–111.
Akaike H. A Bayesian extension of the minimum AIC procedure of autoregressive model fitting. Biometrika. 1979;66(2):237–42.
Cheng Y, Tian DY, Wang YJ. Peripheral clearance of brain-derived Aβ in Alzheimer’s disease: pathophysiology and therapeutic perspectives. Transl Neurodegener. 2020;9(1):16.
Xiang Y, Bu XL, Liu YH, Zhu C, Shen LL, Jiao SS, et al. Physiological amyloid-beta clearance in the periphery and its therapeutic potential for Alzheimer’s disease. Acta Neuropathol. 2015;130(4):487–99.
Liu Y-H, Xiang Y, Wang Y-R, Jiao S-S, Wang Q-H, Bu X-L, et al. Association between serum amyloid-beta and renal functions: implications for roles of kidney in amyloid-beta clearance. Mol Neurobiol. 2015;52(1):115–9.
Simren J, Andreasson U, Gobom J, Suarez Calvet M, Borroni B, Gillberg C, et al. Establishment of reference values for plasma neurofilament light based on healthy individuals aged 5–90 years. Brain Commun. 2022;4(4):fcac174.
Simpson EH. The interpretation of interaction in contingency tables. Journal of the Royal Statistical Society: series B (methodological). 1951;13(2):238–41.
Acknowledgements
For the VETSA dataset, the US Department of Veterans Affairs, Department of Defense; National Personnel Records Center, National Archives and Records Administration; National Opinion Research Center; National Research Council, National Academy of Sciences; and the Institute for Survey Research, Temple University provided invaluable assistance in the creation of the Vietnam Era Twin Registry (VETR). The Cooperative Studies Program of the US Department of Veterans Affairs provided financial support for the development and maintenance of the VETR. We would also like to acknowledge the continued cooperation and participation of the members of the VETR and their families. The content is the sole responsibility of the authors and does not necessarily represent the official views of the NIA, NIH, or VA.
For the ADNI dataset, data collection and sharing for this project was funded by the Alzheimer’s Disease Neuroimaging Initiative (ADNI) (National Institutes of Health Grant U01 AG024904) and DOD ADNI (Department of Defense award number W81XWH-12-2-0012). ADNI is funded by the National Institute on Aging and the National Institute of Biomedical Imaging and Bioengineering and through generous contributions from the following: AbbVie; Alzheimer’s Association; Alzheimer’s Drug Discovery Foundation; Araclon Biotech; BioClinica, Inc.; Biogen; Bristol-Myers Squibb Company; CereSpir, Inc.; Cogstate; Eisai Inc.; Elan Pharmaceuticals, Inc.; Eli Lilly and Company; EuroImmun; F. Hoffmann-La Roche Ltd. and its affiliated company Genentech, Inc.; Fujirebio; GE Healthcare; IXICO Ltd.; Janssen Alzheimer Immunotherapy Research & Development, LLC.; Johnson & Johnson Pharmaceutical Research & Development LLC.; Lumosity; Lundbeck; Merck & Co., Inc.; Meso Scale Diagnostics, LLC.; NeuroRx Research; Neurotrack Technologies; Novartis Pharmaceuticals Corporation; Pfizer Inc.; Piramal Imaging; Servier; Takeda Pharmaceutical Company; and Transition Therapeutics. The Canadian Institutes of Health Research is providing funds to support ADNI clinical sites in Canada. Private sector contributions are facilitated by the Foundation for the National Institutes of Health (www.fnih.org). The grantee organization is the Northern California Institute for Research and Education, and the study is coordinated by the Alzheimer’s Therapeutic Research Institute at the University of Southern California. ADNI data are disseminated by the Laboratory for Neuro Imaging at the University of Southern California.
Data used in the preparation of this article were obtained from the Alzheimer’s Disease Neuroimaging Initiative (ADNI) database (adni.loni.usc.edu). As such, the investigators within the ADNI contributed to the design and implementation of ADNI and/or provided data but did not participate in the analysis or writing of this report. A complete listing of ADNI investigators can be found at http://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf.
Funding
This work was supported by the National Institute on Aging at the National Institutes of Health grant numbers R01s AG050595 to WSK, CEF, and MJL; AG022381, AG076838, and AG064955 to WSK; P01 AG055367 and R01 AG037985 to CEF; and R01s AG058252, AG073979, and AG051848 to RAR and biomarker core funds to RAR from AG057437 (USC ACTC), AG010483 (UCSD ADCS), AG062429 (UCSD ADRC), and K01 AG063805 to JAE.
Author information
Authors and Affiliations
Consortia
Contributions
R.T., M.S.P., J.A.E., C.E.F., and W.S.K. contributed to the conception and design of the study. R.T., M.S.P., J.A.E., N.A.G., R.L.H., R.A.R., M.L.J., M.C.N., C.A.R., C.E.F., and W.S.K. contributed to the acquisition and analysis of the data. R.T., M.S.P., J.A.E., N.A.G., R.L.H., R.A.R., M.L.J., M.C.N., C.A.R., C.E.F., and W.S.K. contributed to the drafting of the manuscript or preparing of the figures. All authors reviewed the manuscript. The authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
For both VETSA and ADNI datasets, full written informed consents were obtained from all participants or their authorized representatives, and both studies were conducted in accordance with the ethical standards of the Declaration of Helsinki and with the institutional and/or national research committees.
For the VETSA dataset, institutional review boards at the University of California San Diego and Boston University approved all study protocols.
For the ADNI dataset, study protocols were approved by the institutional review boards of all participating centers (https://adni.loni.usc.edu/wp-content/uploads/how_to_apply/ADNI_Acknowledgement_List.pdf): Oregon Health and Science University; University of Southern California; University of California San Diego; University of Michigan; Mayo Clinic, Rochester; Baylor College of Medicine; Columbia University Medical Center; Washington University, St. Louis; University of Alabama at Birmingham; Mount Sinai School of Medicine; Rush University Medical Center; Wien Center; Johns Hopkins University; New York University; Duke University Medical Center; University of Pennsylvania; University of Kentucky; University of Pittsburgh; University of Rochester Medical Center; University of California, Irvine; University of Texas Southwestern Medical School; Emory University; University of Kansas, Medical Center; University of California, Los Angeles; Mayo Clinic, Jacksonville; Indiana University; Yale University School of Medicine; McGill University, Montreal-Jewish General Hospital; Sunnybrook Health Sciences, Ontario; U.B.C. Clinic for AD & Related Disorders; Cognitive Neurology St. Joseph’s, Ontario; Cleveland Clinic Lou Ruvo Center for Brain Health; Northwestern University; Premiere Research Inst (Palm Beach Neurology); Georgetown University Medical Center; Brigham and Women’s Hospital; Stanford University; Banner Sun Health Research Institute; Boston University; Howard University; Case Western Reserve University; University of California, Davis; Neurological Care of CNY; Parkwood Hospital; University of Wisconsin; University of California, Irvine—BIC; Banner Alzheimer’s Institute; Dent Neurologic Institute; Ohio State University; Albany Medical College; Hartford Hospital, Olin Neuropsychiatry Research Center; Dartmouth-Hitchcock Medical Center; Wake Forest University Health Sciences; Rhode Island Hospital; Butler Hospital; UC San Francisco; Medical University South Carolina; St. Joseph’s Health Care Nathan Kline Institute; University of Iowa College of Medicine; Cornell University and University of South Florida: USF Health Byrd Alzheimer’s Institute.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Tang, R., Panizzon, M.S., Elman, J.A. et al. Association of neurofilament light chain with renal function: mechanisms and clinical implications. Alz Res Therapy 14, 189 (2022). https://doi.org/10.1186/s13195-022-01134-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13195-022-01134-0