Abstract
Background
The spirometry test is a valuable test to evaluate the performance of the respiratory system. The interpretation of the results is highly dependent on the quality of its performance, while the inappropriate quality results in unwanted consequences for individuals and the healthcare system. This study investigated the quality of spirometry tests performed in occupational health.
Methods
In this cross-sectional study, the quality of 776 spirometry tests in different occupational centers by the specialists in Rasht, Iran, in 2020, based on the guidelines of the American Thoracic Society (ATS), was investigated. The quality and success rate of the test and the demographical characteristics of the operators and the participants were collected. All data was analyzed using SPSS software version 20.
Results
Out of 776 spirometry tests, about 69.7% were unacceptable. Among the unacceptable tests, a pause error between inhalation and exhalation was identified in 7.4% of tests. Additionally, 4.6% of the unacceptable tests exhibited a cough error within the first second, while an exhalation error of less than six was observed in 85%. Repeatability errors were found in 60.9% of the tests. Furthermore, among some errors, the communication error between the characteristics of the technicians and the test performance errors were evident.
Conclusion
According to the results, most of the performed tests were unacceptable with no repeatability, which indicated that the validity and quality of spirometry tests and their interpretation were inappropriate in the field of occupational health in Rasht, Iran.
Similar content being viewed by others
Introduction
The spirometry test is a valuable diagnostic tool used to assess the performance and functionality of the respiratory system. It is crucial in evaluating and monitoring various respiratory conditions, such as chronic obstructive pulmonary disease (COPD), asthma, and occupational lung diseases [1, 2]. The accurate interpretation of spirometry results depends on the test performance quality, as any inaccuracies or inconsistencies in the procedure may lead to misleading outcomes and undesirable consequences for both individuals and the economy [3, 4].
A spirometry test measures the volume of air an individual can inhale or exhale and the speed at which they can perform these respiratory maneuvers. It provides essential data on lung capacity, airflow limitation, and other parameters that help diagnose respiratory disorders, assess disease severity, and monitor treatment effectiveness [5, 6]. However, the reliability and validity of spirometry results heavily rely on adherence to standardized protocols, proper technique execution, and appropriate equipment calibration [7, 8]. In the field of occupational health, spirometry testing assumes particular significance. Occupational hazards, such as exposure to dust, chemicals, and other respiratory irritants, can impair lung function and occupational lung diseases [9, 10]. Regular spirometry testing is crucial in identifying early signs of respiratory dysfunction among workers exposed to these occupational hazards. It aids in implementing timely interventions, ensuring worker safety, and preventing further health deterioration [3, 11].
Despite the importance of spirometry testing, the quality of these tests in the field of occupational health remains a critical concern. Inadequate test performance, including errors in technique, equipment calibration, or data interpretation, can result in inaccuracies and misdiagnosis, leading to improper management strategies, unnecessary medical interventions, and potential economic burdens [12,13,14]. Therefore, this study aims to investigate the quality of spirometry tests performed on workers in different occupational areas.
Methods and patients
Study design
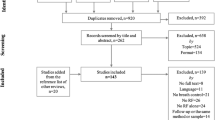
In this descriptive-cross-sectional study, the data of 776 performed spirometry tests in different occupational areas applied by the specialists in Rasht, Iran, in 2020 were collected. Also, the demographical data of participants and technicians, including age, gender, history of smoking, educational field, and years of occupational experiences, were recorded. All participants gave their consent to participate in the study. The study was confirmed by the ethical committee of the Guilan University of Medical Sciences, Rasht, Iran [REC.GUMS.REC.1399.403].
Respiratory test
The quality of the performed spirometry tests was evaluated according to the American Thoracic Society (ATS) guidelines [6] designed by the American ATS/European Respiratory Society (ATS/ERS) to evaluate acceptable indicators and reproducibility of the spirometry maneuver. The spirometry test maneuver must have an appropriate beginning, continuation, and end. The spirometry test was considered acceptable if there was no artifact (cough in the first second of exhalation, glottis closure, leakage of the spirometer device and obstruction in the mouthpiece, etc.), no early end in the exhalation maneuver (exhalation maneuver less than six seconds or plateauing or the volume-time curve was less than one second), and the exhalation maneuver has a suitable start (extrapolated volume < 5% of forced vital capacity (FVC)). After achieving three acceptable maneuvers, at least two tests with repeatability (reproducibility with no difference of more than 150 ml in the amount of the two maximum indicators of FVC two maximum indicators of forced expiratory volume (FEV1) in the exhalation maneuver) were obtained. In this study, the seven operators conducted the spirometry tests (medical students, nurses, and healthcare staff). The pulmonologists evaluated all spirometry tests based on ATS/ERS, and interpersonal variability was assessed (kappa coefficient 95%).
Statistical analysis
Data was analyzed using SPSS software version 20. Qualitative variables were expressed as frequency (number and percentage), and quantitative variables were expressed as mean and standard error (SD). The significance level for this study was considered less than 0.05.
Results
Out of 776 spirometry tests, about 653 were male workers, and the study participants’ average age was 34.62 ± 8.14 years. About 97 of the participants were smokers. Through checking the quality of spirometry tests, only 235 tests were acceptable. Peak error in the first second, maneuver initiation error, pause error between inhalation and exhalation, cough error in the first second, errors of the continuation of the maneuver, maneuver termination error in the first second, exhalation error of less than six seconds, were present in 19, 8, 40, 25, 57, 37, and 460 of unacceptable tests, respectively. About 473 tests had reproducibility errors, and 38 tests had misinterpretations (Table 1).
The average age of the operators was 35.14 years (30–42 years). The average working experience of the operators was 7.57 years (1–12 years). In terms of the relationship between technicians’ gender and spirometry test errors, the frequency of the error of starting the maneuver with insufficient strength was significantly higher in male technicians than in females (P < 0.05). Also, the frequency of pause error between inhalation and exhalation, cough error in the first second, and peak error in the first second were significantly higher in male technicians compared to females (P < 0.001). However, the frequency of exhalation error of less than six seconds was significantly higher in female technicians (P < 0.05). Also, the frequency of errors of repeatability criteria in male technicians was significantly higher than in females (P < 0.05).
Regarding the relationship between technicians’ field of study and spirometry test errors, the frequency of pause error between inhalation and exhalation and peak error in the first second in medical student technicians was significantly higher than the technicians of the other two fields (P < 0.05). The frequency of maneuver termination error and exhalation error of less than six seconds in nursing technicians was significantly higher than in the technicians of the other two fields (P < 0.05). Also, the frequency of errors of reproducibility criteria in technicians in the health education field was significantly higher than in the other two fields (P < 0.001).
In terms of the relationship between technicians’ age and spirometry test errors, the frequency of pause errors between inhalation and exhalation, re-exhalation error, and peak error in the first second in technicians with age ≥ 33 years was significantly higher than in technicians with younger age (P < 0.05). The frequency of cough errors in the first second and exhalation errors less than six seconds in technicians aged < 33 years was significantly higher than in technicians aged ≥ 33 years (P < 0.05). Also, the frequency of errors of reproducibility criteria was significantly higher in technicians with age < 33 years than in technicians with age ≥ 33 years (P = 0.001).
In terms of the relationship between technicians’ work experience and spirometry test errors, frequency of pause error between inhalation and exhalation, peak error in the first second, maneuver termination error, and exhalation error of less than six seconds in technicians with experience years ≥ 7 was more than technicians with less experiences (P < 0.001). The frequency of maneuver continuation error and cough error in the first second and errors in repeatability criteria in technicians with experience years < 7 was significantly higher than in technicians with work experiences ≥ 7 years (P < 0.001) (Table 2).
Discussion
In work environments that contain harmful respiratory factors, periodic and regular spirometry tests are essential for the prevention and early diagnosis of respiratory system disorders. To achieve this, it is necessary to have qualified spirometry tests performed [15, 16]. In this study, we evaluated the quality of spirometry tests conducted on a sample of predominantly male workers, focusing on identifying errors and deficiencies. Our findings revealed that only 30% met the criteria for acceptability, indicating a substantial prevalence of errors within the tested population. One notable observation was the high frequency of exhalation error of fewer than six seconds, which was present in many unacceptable tests.
In the study of Hnizdo et al. on 2500 spirometry tests of firefighters, based on ATS criteria, the rate of acceptable tests was reported to be 60% [17]. Kaur et al. illustrated that among the participants, 87.3% exhibited spirometry tests of acceptable quality. Multivariable analysis revealed that the age ≥ 70 was associated with poor-quality spirometry. They suggested that using a portable spirometer enabled the performance of spirometry tests with acceptable quality in community settings [18].
Another noteworthy finding was the relatively high frequency of errors related to the initiation and continuation of the maneuver, including peak error in the first second and maneuver termination error. These errors have been recognized as familiar sources of variability and inconsistency in spirometry results [19]. These studies emphasized the need for standardized training and higher adherence to best practices among technicians to minimize these errors. Regarding the influence of technician characteristics on spirometry test errors, our study revealed significant associations between gender, field of study, age, and work experience of the operators, and the frequency of errors encountered during testing. Licskai et al. reported that differences in patient population, training protocols, and testing environments can influence the quality and performance of spirometry tests [20].
Furthermore, our findings illustrated that male technicians exhibited a higher frequency of errors than females. The gender disparity may be attributed to differences in technique, experience, and confidence levels. Moreover, analysis of the technicians’ field of study highlighted variations in error frequencies across different professional backgrounds. Medical student technicians were more prone to errors related to pauses between inhalation and exhalation and peak error in the first second, suggesting a potential need for enhanced training in these specific areas. On the other hand, nursing technicians exhibited higher rates of maneuver termination and exhalation errors of less than six seconds, emphasizing the importance of ongoing education and skill refinement in spirometry testing for this group. These findings highlighted the importance of ongoing mentorship and quality control measures to improve the proficiency of less-experienced technicians.
A study by Seyedmehdi et al. on 1004 male workers evaluated the standardization of spirometry tests before and after training according to National Institute for Occupational Safety and Health (NIOSH) guidelines and reported a significant improvement in the quality of spirometry tests following the training intervention [3]. Another study by Saraei et al. indicated that the spirometry tests conducted during the periodic examinations of workers exhibited low quality. They suggested training spirometry operators and implementing more stringent monitoring measures to ensure the accuracy and reliability of spirometry tests in occupational examinations [4]. Most spirometer tests in a study by Hegewald et al. demonstrated inaccuracies, with the errors being substantial enough to lead to significant alterations in the classification of patients with obstruction. Furthermore, only 60% of patients underwent acceptable-quality tests [21]. These findings highlight apprehensions regarding the usefulness of spirometry conducted in primary care settings without adequate emphasis on quality assurance and comprehensive training.
Conclusion
The current study suggested the need for continued efforts to improve the quality of spirometry testing. By identifying common errors, understanding their associations with technician characteristics, and drawing comparisons to previous research, the study provided valuable insights for practitioners, educators, and policymakers to enhance the accuracy and reliability of spirometry measurements in the field of occupational health.
Data availability
The datasets used and/or analyzed in the current study are available from the corresponding author on reasonable request.
References
Haynes JM. Basic spirometry testing and interpretation for the primary care provider. Can J Respir Ther CJRT = Rev Can La Ther Respir RCTR. 2018;54.
Johns DP, Walters JAE, Walters EH. Diagnosis and early detection of COPD using spirometry. J Thorac Dis Vol 6, No 11 (November 18, 2014) J Thorac Dis (Chronic Obstr Pulm Dis. 2014.
Seyedmehdi SM, Attarchi M, Yazdanparast T, Lakeh MM. Quality of spirometry tests and pulmonary function changes among industrial company workers in Iran: a two-year before-and-after study following an intensive training intervention. Prim Care Respir J. 2013;22:86–91.
Saraei M, Heydarbeygi E, Mehrdad R. Quality of spirometry tests in periodic examination of workers. 2018;75–9.
Moore VC. Spirometry: step by step. Breathe. 2012;8:232LP–240.
Miller MR, Hankinson J, Brusasco V, Burgos F, Casaburi R, Coates A, et al. Standardisation of spirometry. Eur Respir J. 2005;26:319–38.
Graham BL, Steenbruggen I, Miller MR, Barjaktarevic IZ, Cooper BG, Hall GL, et al. Standardization of Spirometry 2019 Update. An official American Thoracic Society and European Respiratory Society Technical Statement. Am J Respir Crit Care Med. 2019;200:e70–88.
Wu Z, Peng Y, Lin K, Huang R, Zheng J, Gao Y. Quality inspection and result analysis of the spirometer calibration cylinder. BMC Pulm Med. 2022;22:218.
Murgia N, Gambelunghe A. Occupational COPD—The most under-recognized occupational lung Disease? Respirology. 2022;27:399–410.
Ahmad I, Balkhyour MA. Occupational exposure and respiratory health of workers at small scale industries. Saudi J Biol Sci. 2020;27:985–90.
Redlich CA, Tarlo SM, Hankinson JL, Townsend MC, Eschenbacher WL, Von Essen SG, et al. Official American thoracic society technical standards: spirometry in the occupational setting. Am J Respir Crit Care Med. 2014;189:984–94.
Minov J. Occupational chronic obstructive pulmonary disorder: prevalence and prevention. Expert Rev Respir Med. 2022;16:429–36.
De Matteis S, Heederik D, Burdorf A, Colosio C, Cullinan P, Henneberger PK et al. Current and new challenges in occupational lung Diseases. Eur Respir Rev. 2017;26.
Dehghan F, Mohammadi S, Sadeghi Z, Attarchi M. Respiratory complaints and spirometric parameters in tile and ceramic factory workers. TANAFFOS (Respiration). 2009;8(4):19–25.
Ghosh T, Gangopadhyay S, Das B. Prevalence of respiratory symptoms and disorders among rice mill workers in India. Environ Health Prev Med. 2014;19:226–33.
Schneider I, Rodwell L, Baum S, Borg BM, Del Colle EA, Ingram ER, et al. Assessing spirometry competence through certification in community-based healthcare settings in Australia and New Zealand: a position paper of the Australian and New Zealand Society of Respiratory Science. Respirology. 2021;26:147–52.
Hnizdo E, Hakobyan A, Fleming JL, Beeckman-Wagner L-A. Periodic spirometry in occupational setting: improving quality, accuracy, and precision. J Occup Environ Med. 2011;53:1205–9.
Kaur R, Kumar A, Hadda V, Kalaivani M, Nongkynrih B, Kant S, et al. Quality of spirometry testing in a community setting: a study among elderly persons in a rural area of Haryana. J Fam Med Prim care. 2019;8:3718–25.
Belzer RB, Lewis RJ. The practical significance of measurement error in pulmonary function testing conducted in Research Settings. Risk Anal. 2019;39:2316–28.
Licskai CJ, Sands TW, Paolatto L, Nicoletti I, Ferrone M. Spirometry in primary care: an analysis of spirometery test quality in a regional primary care Asthma program. Can Respir J. 2012;19:249–54.
Hegewald MJ, Gallo HM, Wilson EL. Accuracy and quality of spirometry in primary care offices. Ann Am Thorac Soc. 2016;13:2119–24.
Acknowledgements
Not applicable.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
All authors contributed to the study’s conception and design. Material preparation, data collection, and analysis were performed by [Amirala Alavi Foumani], [Seyyed Ali Alavi Foumani], [Mirsaeed Attarchi], and [Habib Eslami-Kenarsari]. The first draft of the manuscript was written by [Alireza Etemadi Deilami], [Behzad Majlesi], [ Shima Ildari], [Seyyed Ali Alavi Foumani], [Amirala Alavi Foumani], and [Mirsaeed Attarchi] and all authors commented on previous versions of the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the medical ethics committee of the Tabriz University of Medical Sciences, Rasht, Iran [REC.GUMS.REC.1399.403]. All subjects gave their informed consent to participate in the study. All methods were carried out in accordance with relevant guidelines and regulations that is Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Alavi Foumani, A., Alavi Foumani, S., Attarchi, M. et al. Quality of spirometry tests in the field of occupational health. BMC Res Notes 17, 11 (2024). https://doi.org/10.1186/s13104-023-06671-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13104-023-06671-x