Abstract
Background
Post-Covid-19 syndrome is defined as non-self-sustaining signs and/or symptoms lasting more than 12 weeks, occurring during or after a Covid-19 infection. The primary outcome was the analysis of the respiratory muscle training (RMT) result in respiratory muscle strength, (maximum inspiratory pressure (MIP) e maximum expiratory pressure (MEP)); and the secondary results were the analysis of lung function, dyspnea, quality of life (QoL), fatigue and functional performance. Methods: The PICO description for this research was: P: patients diagnosed with post-Covid-19; I: RMT; C: Sham or simulated inspiratory or expiratory muscle training and usual care; O: MIP, MEP, Lung Function, level of dyspnea, QoL and functional performance. On January 15, 2024, the following databases were consulted: PubMed, Lilacs, Cochrane Library, PEDro and EMBASE. Randomized clinical trials were included without restrictions on year of publication or language. The data selection and extraction steps were carried out by two independent reviewers. Results: The search in the databases resulted in a total of 14,216 studies, and after the eligibility process, 7 studies were included with a sample of 527 patients. The MIP results suffered a statistically significant increase, that is, the RMT was favorable to improve the MIP (MD = 29.55cmH2O IC 95%: 7.56cmH2O to 51.54cmH2O, p = 0,00001). For the MEP outcome, the results were statistically significant in favor of RMT (MD = 10.93cmH2O CI 95%: 3.65cmH2O to 18.21cmH2O, p = 0.00001). We also noticed a significant improvement for the group that received the RMT in the distance covered in the 6-Minute Walk Test (6MWT) MD = 40.70 m CI 95%: 18.23 m to 65.17 m%, p = 0.01). Conclusion: We noticed that RMT is being used in patients with respiratory diseases, including post-Covid-19. Our systematic review observed that this training provides an increase in inspiratory and expiratory muscle strength, a reduction in dyspnea levels, and an increase in the distance covered in the 6MWT and improved QoL in post-covid patients after intervention.
Similar content being viewed by others
Introduction
In the month of April 2021, more than 127 million cases of coronavirus infection (COVID-19) were reported worldwide [1]. The pandemic was caused by the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), responsible for a new type of acute respiratory infection and atypical pneumonia with the potential to evolve into a severe acute respiratory syndrome (SARS), described for the first time in Wuhan Province, China [2].
The National Health Service (NHS - London) defines post-Covid-19 syndrome as non-self-sustaining signs and/or symptoms lasting longer than 12 weeks, occurring during or following a COVID-19 infection [3]. Additionally, the term COVID-19 has long been frequently used to describe signs and symptoms that continue or develop after acute Covid-19 [4,5,6].
For post-Covid hospitalized patients, there is an urgent need to develop new education and training programs focusing on interdisciplinary rehabilitation [7]. Previous studies confirm that physiotherapeutic interventions are especially relevant to combat respiratory and neuromuscular dysfunctions in these patients [7, 8].
The popularity of physical training in post-Covid-19 patients has increased significantly [9]. As the number of people recovering from the infection grows, physical rehabilitation has proven essential for restoring quality of life (QoL) and promoting overall health. Physical training is recognized for helping to improve cardiorespiratory capacity, muscle strength, and endurance, factors often compromised after coronavirus infection. This increase in popularity is due to the need to mitigate the residual effects of the disease, such as chronic fatigue, shortness of breath, and muscle weakness, which are common in many COVID-19 survivors [7,8,9].
The physiological adaptations to physical training in post-Covid-19 patients include a series of significant improvements in the cardiovascular, respiratory, and muscular systems [9]. Regular physical exercise can increase the efficiency of the heart and lungs, improving oxygenation and blood circulation [8, 9]. Additionally, resistance and strength training can contribute to the recovery of lost muscle mass and the improvement of muscle function, essential for performing daily activities [8, 9]. These adaptations are crucial to help patients resume their normal routines and reduce the incidence of long-term complications associated with Covid-19 [9].
Among the practices addressed in the rehabilitation of these patients is respiratory muscle training (RMT). Existing evidence supports the use of this practice within pulmonary rehabilitation programs, as this therapy has been shown to improve functional capacity, lung function and respiratory muscle strength in post-Covid-19 patients, hopefully to improve their QoL [10, 11]. However, it is still necessary to systematize the results of this treatment modality to guarantee and support its use.
Therefore, the aim of this study was to elucidate the effectiveness of controlled muscle training in post-Covid-19 patients. The primary outcome was the analysis of the RMT result in respiratory muscle strength (maximum inspiratory pressure (MIP) e maximum expiratory pressure (MEP)); and the secondary objectives were intervention responses on lung function, dyspnea, QoL, fatigue and functional performance.
Methods
Study registration
This systematic review of randomized controlled trials (RCT) is reported in line with the preferred reporting items for systematic review/meta-analysis (PRISMA) check list [12] and according to the Cochrane Handbook for Systematic Reviews methodology [13]. The protocol of this review is registered in the Open Science Framework (https://osf.io/h8gjm/and/or DOI https://doi.org/10.17605/OSF.IO/H8GJM) (Appendix I).
Eligibility criteria
PICOS for this study was defined as: P: Studies with patients who did or did not present symptoms after a previous infection with Covid-19, and currently classified with a diagnosis of post-Covid-19, Long Covid or Post-Covid Syndrome, of both sexes, regardless of age; and who did not have post-covid stroke, renal failure and/or myocardial infarction were included; I: RMT was considered any type of exercise to gain and/or maximize resistance and/or strength of the respiratory muscles. Equipment with progressive linear loads was considered, such as Threshold®, POWERbreathe® or any other equipment developed to make this training modality viable, regardless of being used in conjunction with other therapies; C: Sham or simulated inspiratory muscle training (IMT), expiratory muscle training (EMT), usual care (medication and/or education) were all used as comparators; S: RCT.
Search strategy and selection of articles
Searches were performed from baseline to January 15, 2024 (Appendix II), without date limits or language restrictions, in the following databases: Medline via PubMed (www.pubmed.gov), Lilacs via Virtual Health Library (www.bvsalud.org), CENTRAL through the Cochrane Library (www.cochranelibrary.com), Physiotherapy Evidence Database (PEDro) (https://www.pedro.org.au/) and EMBASE (https://www.embase.com/). ClinicalTrials.gov was evaluated to identify potential ongoing studies. In addition, the initial search was complemented by a manual search of the reference lists of retrieved articles. The terms used were related to “respiratory muscle training”, “Pos - covid” and “randomized controlled trials”. To avoid publication bias, gray literature (Google Scholar) was also consulted.
Electronic searches were performed by two independent authors (DMX and RALA). The articles found in the databases were exported to Rayyan (http://rayyan.qcri.org) [14]. After, duplicates were removed. First, manuscripts were selected by titles and abstracts based on eligibility criteria. Then, the selected studies were read in full to confirm their eligibility. Disagreements about the inclusion process were resolved by a third reviewer (MGNJ).
Data extraction
Data were extracted by two independent reviewers (DMX and RALA). The authors of the articles were contacted to request missing or additional data when necessary.
The following information was extracted: author, year and country of studies, time of intervention, inclusion and exclusion criteria; characteristics of the population (age, gender and sports practice); intervention used (equipment used and characteristics of the intervention and comparator groups); lung function: respiratory muscle strength (MIP) e (MEP), Forced Expiratory Volume in 1 s (FEV1), Forced Vital Capacity (FVC), Tiffenau Index (FEV1/FVC); results of indexes evaluating the level of dyspnea, QoL and fatigue; and performance/physical test results.
We extracted post-intervention means, standard deviations (SD) and sample sizes for each of our interest groups. In the study, short-term effects were considered as follow-up up to three months after the beginning of the study; medium-term effects were considered follow-up after three months but less than twelve months, and long-term effects were considered follow-up of at least twelve months after baseline.
In cases where there was more than one follow-up point available in the same period, the point closest to the end of the intervention was chosen. The study was excluded from the quantitative analysis when the authors did not respond [12, 15].
Risk of bias in individual studies
Two independent reviewers (DMX and RALA) assessed the risk of bias of the included studies using the PEDro scale from 0 to 10. The third reviewer was asked to resolve existing discrepancies (MGDJ). Where available, we use existing scores from the PEDro database (https://pedro.org.au/).
Summary measures and summary of results
When possible, a meta-analysis was performed using Review Manager software version 5.4. Meta-analysis was produced when at least two studies reported sufficient data for the same outcome in the RMT and GC groups. Data regarding the mean difference and SD from baseline to post-intervention follow-up were collected. Effect sizes were expressed as final (or standardized) weighted mean differences post-intervention (for continuous data) and their 95% confidence intervals. Heterogeneity was assessed in a statistically randomized fashion using I2 test, considering random-effects model if I2 ≥ 30% and fixed effects models if I2 < 30%. Subgroup analyzes were performed when sufficient data were available to investigate the impact between the types of programs used [16, 17].
Reliability of cumulative evidence
Two independent reviewers assessed the quality of the current evidence using the Grading of Recommendations Assessment (GRADE) approach [18, 19].
A Summary of Results (SoF) was created using GRADEPro GDT (McMaster University, ON, Canada) for each outcome that allowed meta-analyses. SoF tables were generated at the end of the analysis according to the certainty of evidence across studies and classified as high, moderate, low or very low certainty of evidence. When no reason was found to downgrade the evidence, it was classified as “no limitation”. When any reason was found to downgrade the evidence, it was classified as “serious”.
Results
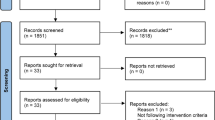
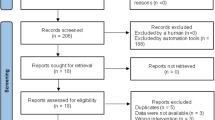
In total, 14,216 potentially relevant articles were found in electronic databases, manual searches and gray literature. Duplicates were then removed and two reviewers carried out the eligibility assessment according to titles and abstracts, leaving a total of 126 articles. Afterwards, these 126 articles were read in full; A total of 119 manuscripts were excluded for different reasons (not RCT: (n = 24), not population of interest: (n = 35), not intervention of interest: (n = 29), not comparison of interest: (n = 18) and not results of interest: (n: 13). This left a total of 7 studies [11, 20,21,22,23,24,25] were included in the qualitative study in which 527 post-Covid 19 patients participated. Only two studies [10, 22] were excluded from the quantitative analysis because they presented their data differently from the others. Figure 1 shows the flowchart of the study selection process.
Description of studies and assessment of risk of bias
The studies included in this review were published between 2021 and 2023. The duration of the RMT programs ranged from six weeks to a maximum of 12 weeks. The sample size of the included studies ranged from 26 to 160 participants and the mean age ranged from 44 (11.28) to 50.40 (12.12). Data on the gender of participating athletes were reported in 6 studies, involving a total of 156 men and 223 women [20,21,22,23,24,25].
The POWERbreathe® device was the most used among the studies. The load used to perform the RMT was most commonly performed between 25 and 80% of the MIP and/or MEP. Participants in the comparison group used sham RMT, usual care. Tables 1 and 2 show the main characteristics of the included studies, participants, interventions and clinical characteristics.
Five included studies were at low risk of bias; their PEDro scores were greater than 6. The main reasons for the reduction in risk of bias scores were: not blinding allocation (not blinding therapists and subjects (4 trials [100%])). Detailed characteristics of the risk of bias of included studies are presented in Appendix III.
Data extraction and meta-analysis
MIP
In a meta-analysis involving 4 studies [11, 21, 24, 25] the MIP results suffered a statistically significant increase in the medium term, that is, the RMT was favorable to improve the MIP (MD = 29.55cmH2O IC 95%: 7.56cmH2O to 51.54cmH2O, p = 0,00001). Data present in Fig. 2.
MEP
The produced meta-analysis showed statistically significant results in the medium term in favor of the RMT (MD = 10.93cmH2O IC 95%: 3.65cmH2O to 18.21cmH2O, p = 0,00001). Figure 3.
FEV1
The meta-analysis produced included a total of three articles [21, 23, 25] and indicated that there was no statistically significant difference, in the medium term, between the intervention and GC groups after the RMT intervention in FEV1 values (MD = 0.30 95% CI: -0.07 to 0.67%, p = 0.01). Figure 4.
FEV1/FVC
The meta-analysis produced included a total of two articles [21, 25] indicated that there was no statistically significant difference, in the medium term, between the intervention and GC groups after the RMT intervention in FEV1/FVC values (MD = -1.66 95% CI: -4.04 to 0.72%, p = 0.01). Appendix IV.
FVC
The meta-analysis involving 3 studies [21, 23, 25] showed that there was no statistically significant difference, in the short term and medium term, after the RMT when comparing the intervention and control groups (MD = 0.35 95% CI: -0.13 to 0.82%, p = 0.01). Appendix V.
Performance and/or physical test
1-min sit-to-stand (1-min STS)
The 1-min STS test was used by two studies [21, 24]. In the meta-analysis produced, we can see that there was no statistically significant difference, medium term, between the CG and the intervention group after RMT (MD = 1.79 95% CI: -0.99 to 4.57%, p = 0.01). Appendix VI.
Six-minute walk test (6MWT)
The 6MWT was carried out in a study [23] and we noticed that there was a statistically significant improvement, in the short term, in favor of the intervention group when compared to the CG, demonstrating an improvement in functional capacity (MD = 40.70 m 95% CI: 18.23 m to 65.17 m %, p = 0.01).
Estimated VO2max
VO2max was measured in one study [11] (estimated by the Chester Step Test). After the intervention, we noticed a statistically significant improvement in the VO2max of the participants who were in the intervention group (MD = 5.2mL·kg− 1·min− 1 95% CI: 1.78mL·kg− 1·min− 1 to 8.62mL·kg− 1·min− 1%, p = 0.01).
Fatigue
Only one study [11] evaluated fatigue after intervention using the Fatigue Index Time (FIT). The results did not identify a statistically significant difference after the intervention between the CG and the RMT group (MD = 2.9 95% CI: -6.37 to 12.17%, p = 0.01).
QoL
The QoL was evaluated in four studies [11, 20, 22, 23] being quantified by 3 different instruments: Euro Quality 5Dimensions-3Levels (EQ-5D-3 L), The King’s Brief Interstitial Lung Disease (K-BILD) and 12- item Short Form Survey (SF-12). The study by McNarry et al. [11] and Abodonya et al. [23] demonstrated an improvement in the QoL for participants in the RMT intervention group when compared to the CG: (MD = 16.10 95% CI: 11.59 to 20.61%, p = 0.01) and (MD = 8.00 95% CI: 3.14 to 12.86%, p = 0.01), respectively. The SF-12 was used by one study [20] however, only two domains were reported in the study (Physical Activity and mental health) and found no significant difference between groups after the intervention. In addition, the study by Palau et al. [22] demonstrated that after the intervention there were significant improvements in the dimensions of usual activities and anxiety/depression in the group that received the RMT.
Dyspnea
Four studies evaluated dyspnea [11, 20, 23, 25]. However, it was not possible to carry out any meta-analysis due to differences in the scales used and the method of disseminating the results. The scales used to quantify the results were: Transition Dyspnea Index (TDI), dyspnea severity index (DSI) and modified Medical Research Council (mMRC). In the study by Jimeno-Almazán et al. [20] and McNarry et al. [11] an improvement in dyspnea was observed after the RMT intervention. We noticed a reduction in the mMRC scale score after the intervention (MD = -1.45 95% CI: -1.94 to -0.96%, p = 0.01) [25] and also in the DSI scale (MD = -2.90 95% CI: -5.44 to -0.36%, p = 0.01) [23] after RMT, which is indicative of improvement in dyspnea symptoms.
Reliability of cumulative evidence
The assessment of the quality of evidence using GRADE showed very low quality of evidence for the results obtained in MIP and FEV1/FVC; low certainty for FEV1 and FVC; and moderate certainty of evidence for MEP and 1-min STS. The main reasons for the decrease in the certainty of the evidence of the evaluated outcomes were the possibility of inconsistency and imprecision (Appendix VII).
Discussion
The Covid-19 pandemic has brought significant challenges to global health, with many patients experiencing persistent sequelae even after recovering from the acute infection [2, 3, 5]. Among these sequelae, respiratory muscle weakness has been a growing concern, as it directly impacts the QoL and functional capacity of patients [3, 5, 9]. RMT has emerged as a potentially beneficial intervention to mitigate these adverse effects [9,10,11].
Post-Covid syndrome (also known as Long-Covid), can be defined as a syndrome that encompasses a prolonged course of different physical and neuropsychiatric symptoms that persist for more than 12 weeks without an alternative explanation [26]. In this systematic review, 7 studies were included to evaluate an RMT program as a complementary treatment option for patients with post-Covid syndrome. The main findings of this systematic review and meta-analysis indicate that RMT results in significant improvements in respiratory function (MIP, MEP), exercise capacity (6MWT, VO2max) and QoL in post-Covid-19 patients. These results are consistent with previous studies demonstrating the effectiveness of RMT in populations with chronic respiratory diseases.
The number of weekly sessions in the studies ranged from 3 to 14 sessions, with a minimum duration of 2 weeks and a maximum of 12 weeks. The included studies only counted patients who were able to perform at least 70% of the RMT sessions.
RMT is already used in different types of health conditions that affect the respiratory system, such as chronic obstructive pulmonary disease (COPD) [27], cystic fibrosis [28] and asthma [29]. Our review observed that studies (RCTs) are being carried out from the year 2021 to the current year.
The most used device for RMT was the POWERbreathe®. This device is capable of adapting the inspiratory resistance to the pulmonary pressure curve, stabilizing the load during exercise, allowing training to be more comfortable; Furthermore, it is known that this equipment offers the possibility of introducing greater levels of load during exercise [30]. These facts could explain the choice of this device in most RCTs.
Respiratory muscle strength is a critical component of lung function and overall ventilatory capacity [8, 9]. In post-Covid-19 patients, respiratory muscle weakness has been identified as a significant sequela, contributing to persistent symptoms such as dyspnea and fatigue [7,8,9]. Our results showed an improvement in both inspiratory and expiratory muscle strength following TMR. This finding corroborates results from previous studies that have employed this type of training [29, 31]. These improvements can be explained by the principle that respiratory muscle groups, like other skeletal muscles, respond to training stimuli through adaptations when their fibers are stimulated to generate a state of overload [32, 33].
Moreover, previous studies involving participants with pulmonary diseases who underwent IMT also demonstrated an increase in MIP results, similar to what was observed in our review [34, 35]. The minimal clinically important difference for MIP in post-Covid-19 individuals has recently been established at 18cmH2O [36]. Our results may be clinically significant, as we found values exceeding the established threshold following the intervention (MD = 29.55cmH2O, 95% CI: 7.56 cmH2O to 51.54cmH2O, p = 0.00001).
The MEP is a crucial indicator of the strength and function of the muscles responsible for expiration [37]. Our study revealed that RMT, including EMT, has a substantial positive impact on MEP, highlighting the effectiveness of this approach in respiratory recovery. The observed increase in MEP across the included studies suggests that EMT can lead to significant gains in respiratory muscle strength and expiratory capacity, which are essential for the restoration of pulmonary function [10, 21]. These benefits are particularly relevant for patients who may have experienced a reduction in expiratory strength due to the prolonged impact of Covid-19, contributing to improved respiratory efficiency and greater comfort during daily activities [37].
We noticed that there were no statistically significant results between CG and intervention for FEV1/FVC values. This difficulty in obtaining a significant improvement in this outcome can be explained by the pulmonary consequences that may occur due to Covid-19 [38, 39]. It has already been reported that Covid-19 can develop abnormalities in the bronchi, such as necrotizing bronchiolitis [38] bronchial or focal bronchiolar inflammation [40].
The QoL has been increasingly reported in studies involving patients with diseases involving the respiratory system. Studies have found that respiratory rehabilitation can improve the QoL of patients with COPD [40], cystic fibrosis [41], asthma [28]. These results corroborate the findings of this study since the scores of the questionnaires used after the intervention were favorable to the improvement of QoL. Several studies included in the analysis reported improvements in patients’ QoL, measured by standardized questionnaires. These improvements were attributed to reduced dyspnea and increased ability to perform daily activities without excessive fatigue [11, 20, 23]. However, this outcome should be further explored; the standardization of instruments and their application may be important for future research to better describe the results of this intervention in these patients.
The 6MWT, a common measure of functional capacity, also showed significant improvements in the intervention groups [23]. The greater distance covered by patients who participated in RMT indicates an increase in endurance and aerobic capacity. Dyspnea is a common and debilitating symptom in post-Covid-19 patients. The increase in distance covered on the 6MWT after RMT suggests a reduction in dyspnea, allowing patients to maintain a higher level of activity without excessive respiratory distress. This fact corroborates the results presented by the study Abodonya et al. [23], since after intervention we observed a reduction in dyspnea and an increase in the distance covered.
Therefore, the results indicate that RMT can be an effective intervention to mitigate the prolonged respiratory effects of COVID-19, promoting the recovery of lung function and improving exercise capacity and QoL. The improvement in respiratory muscle strength likely contributes to a reduction in respiratory effort and greater respiratory efficiency, which may explain the improvements observed in the functional and subjective evaluations of the patients.
Study limitations
Several concerns should be considered as limitations of this study. Although the included studies had similar primary objectives, they exhibited substantial heterogeneity in terms of methodology, follow-up periods, and outcome assessments. Consequently, only a few studies were included in our meta-analyses. Additionally, despite our conclusions being based on the analysis of experimental studies, the very small number of patients included in these analyses precludes the generalization of the results to the entire population with post-Covid syndrome. Furthermore, we were unable to assess publication bias due to the limited number of studies included.
However, despite these limitations, we believe that the scarcity of data underscores the need for future and additional investigations. This could serve as a positive impetus to enhance our understanding of the use of RMT in post-Covid syndrome.
Conclusion
There are a limited number of studies comparing post-covid patients undergoing RMT versus standard treatment. However, in our systematic review we found an increase in inspiratory and expiratory muscle strength in post-covid patients after intervention. The descriptive analysis suggests a reduction in dyspnea levels, an increase in the distance covered in the 6MWT, and an improvement in QoL. However, the conclusions remain uncertain as these results are based on very low to low quality evidence.
Data availability
Data is provided within the manuscript or supplementary information files.
References
European Center For Disease Prevention and Control (ECDC). COVID-19 Situation Dashboard. https://qap.ecdc.europa.eu/public/extensions/COVID-19/COVID-19.html#global-overview-tab. Accessed 31 January 2021.
Greenhalgh T, Knight M, A’Court C, Buxton M, Husain L. Management of post-acute covid-19 in primary care. BMJ. 2020;370. https://doi.org/10.1136/bmj.m3026.
Royal College of General Practitioners. COVID-19 Guideline Scope: management of the Long-Term effects of COVID-19. London: NICE; 2020. pp. 1–7.
UK Office for National Statistics. Prevalence of ongoing symptoms following coronavirus (COVID-19) infection in the UK: 1 April 2021. London: ONS; 2021.
Mahase E. Long covid could be four different syndromes, review suggests. BMJ. 2020;371. https://doi.org/10.1136/bmj.m3981.
Callard F, Perego E. How and why patients made Long Covid. Soc Sci Med. 2021;268:113426. https://doi.org/10.1016/j.socscimed.2020.113426.
Scheiber B, Spiegl C, Wiederin C, Schifferegger E, Schiefermeier-Mach N, Post. -COVID-19 Rehabilitation: perception and experience of Austrian physiotherapists and physiotherapy students. Int J Environ Res Public Health. 2021;18(16):8730. https://doi.org/10.3390/ijerph18168730.
Yong SJ. Long COVID or post-COVID-19 syndrome: putative pathophysiology, risk factors, and treatments. Infect Dis (Lond). 2021;53(10):737–54. https://doi.org/10.1080/23744235.2021.1924397.
Al-Mhanna SB, Batrakoulis A, Hofmeister M, Drenowatz C, Ghazali WSW, Badicu G, Afolabi HA, Gülü M, Wada Y, Aldhahi MI, Nikolaidis PT. Psychophysiological adaptations to Exercise Training in COVID-19 patients: a systematic review. Biomed Res Int. 2024;2024:3325321. https://doi.org/10.1155/2024/3325321.
Hockele LF, Sachet Affonso JV, Rossi D, Eibel B. Pulmonary and Functional Rehabilitation improves functional capacity, pulmonary function and respiratory muscle strength in Post COVID-19 patients: Pilot Clinical Trial. Int J Environ Res Public Health. 2022;19(22):14899. https://doi.org/10.3390/ijerph192214899.
McNarry MA, Berg RMG, Shelley J, Hudson J, Saynor ZL, Duckers J, Lewis K, Davies GA, Mackintosh KA. Inspiratory muscle training enhances recovery post-COVID-19: a randomised controlled trial. Eur Respir J. 2022;60(4):2103101. https://doi.org/10.1183/13993003.03101-2021.
Higgins JP, Thomas J, Chandler J, Cumpston M, Li T, Page MJ et al. Cochrane handbook for systematic reviews of interventions. https://training.cochrane.org/cochrane-handbook-systematic-reviews-interventions. Accessed 7 December 2020.
Moher D, Liberati A, Tetzlaff J, Altman DG, PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 2009;6(7). https://doi.org/10.1371/journal.pmed.1000097.
Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan—a web and mobile app for systematic reviews. Syst Rev. 2016;5:210. https://doi.org/10.1186/s13643-016-0384-4.
Wan X, Wang W, Liu J, Tong T. Estimating the sample mean and standard deviation from the sample size, median, range and/or interquartile range. BMC Med Res Methodol. 2014;14:135. https://doi.org/10.1186/1471-2288-14-135.
Guyatt GH, Oxman AD, Vist GE, et al. GRADE: an emerging consensus on rating quality of evidence and strength of recommendations. BMJ. 2008;336(7650):924–6. https://doi.org/10.1136/bmj.39489.470347.AD.
Ioannidis JP, Trikalinos TA. The appropriateness of asymmetry tests for publication bias in meta-analyses: a large survey. CMAJ. 2007;176(8):1091–6. https://doi.org/10.1503/cmaj.060410.
Atkins D, Eccles M, Flottorp S, Guyatt GH, Henry D, Hill S, et al. Systems for grading the quality of evidence and the strength of recommendations I: critical appraisal of existing approaches. BMC Health Serv Res. 2004;4:38. https://doi.org/10.1186/1472-6963-4-38.
Balshem H, Helfand M, Schünemann HJ, et al. GRADE guidelines: 3. Rating the quality of evidence. J Clin Epidemiol. 2011;64(4):401–6. https://doi.org/10.1016/j.jclinepi.2010.07.015.
Jimeno-Almazán A, Buendía-Romero Á, Martínez-Cava A, Franco-López F, Sánchez-Alcaraz BJ, Courel-Ibáñez J, Pallarés JG. Effects of a concurrent training, respiratory muscle exercise, and self-management recommendations on recovery from post-COVID-19 conditions: the RECOVE trial. J Appl Physiol (1985). 2023;134(1):95–104. https://doi.org/10.1152/japplphysiol.00489.2022.
Del Corral T, Fabero-Garrido R, Plaza-Manzano G, Fernández-de-Las-Peñas C, Navarro-Santana M, López-de-Uralde-Villanueva I. Home-based respiratory muscle training on quality of life and exercise tolerance in long-term post-COVID-19: Randomized controlled trial. Ann Phys Rehabil Med. 2023;66(1):101709. https://doi.org/10.1016/j.rehab.2022.101709.
Palau P, Domínguez E, Gonzalez C, Bondía E, Albiach C, Sastre C, Martínez ML, Núñez J, López L. Effect of a home-based inspiratory muscle training programme on functional capacity in postdischarged patients with long COVID: the InsCOVID trial. BMJ Open Respir Res. 2022;9(1). https://doi.org/10.1136/bmjresp-2022-001439.
Abodonya AM, Abdelbasset WK, Awad EA, Elalfy IE, Salem HA, Elsayed SH. Inspiratory muscle training for recovered COVID-19 patients after weaning from mechanical ventilation: a pilot control clinical study. Med (Baltim). 2021;100(13). https://doi.org/10.1097/MD.0000000000025339.
Gracelli MB. Efeitos do treinamento muscular inspiratório sobre a força muscular inspiratória, a endurance muscular inspiratória e a capacidade funcional de pacientes com síndrome pós-covid-19. 2023. https://repositorio.uvv.br/handle/123456789/993
Karina VC. Eficácia de um protocolo de reabilitação cardiopulmonar na função pulmonar e muscular respiratória de pacientes com síndrome pós COVID-19: um ensaio clínico randomizado. Universidade Federal da Paraíba, Centro de Ciências da Saúde Programa de Pós Graduação em Fisioterapia - PPGFIS; 2022. https://repositorio.ufpb.br/jspui/handle/123456789/25502?locale=pt_BR
Mahase E. Covid-19: what do we know about long covid? BMJ. 2020;370. https://doi.org/10.1136/bmj.m2815.
Vázquez-Gandullo E, Hidalgo-Molina A, Montoro-Ballesteros F, Morales-González M, Muñoz-Ramírez I, Arnedillo-Muñoz A. Inspiratory Muscle Training in patients with chronic obstructive Pulmonary Disease (COPD) as part of a respiratory Rehabilitation Program implementation of mechanical devices: a systematic review. Int J Environ Res Public Health. 2022;19(9):5564. https://doi.org/10.3390/ijerph19095564.
Stanford G, Ryan H, Solis-Moya A. Respiratory muscle training for cystic fibrosis. Cochrane Database Syst Rev. 2020;12(12). https://doi.org/10.1002/14651858.CD006112.pub5.
Chung Y, Huang TY, Liao YH, Kuo YC. 12-Week Inspiratory muscle training improves respiratory muscle strength in adult patients with stable asthma: a Randomized Controlled Trial. Int J Environ Res Public Health. 2021;18(6):3267. https://doi.org/10.3390/ijerph18063267.
McConnell AK, Sharpe GR. The effect of inspiratory muscle training upon maximum lactate steady-state and blood lactate concentration. Eur J Appl Physiol. 2005;94(3):277–84. https://doi.org/10.1007/s00421-004-1282-3.
Boswell-Ruys CL, Lewis CRH, Wijeysuriya NS, McBain RA, Lee BB, McKenzie DK, Gandevia SC, Butler JE. Impact of respiratory muscle training on respiratory muscle strength, respiratory function and quality of life in individuals with tetraplegia: a randomised clinical trial. Thorax. 2020;75(3):279–88. https://doi.org/10.1136/thoraxjnl-2019-213917.
Mcconnell K. Respiratory muscle training as an ergogenic aid. J Exerc Sci Fit. 2008;7:18–27. https://doi.org/10.1016/S1728-869X(09)60019-8.
Illi SK, Held U, Frank I, Spengler CM. Effect of respiratory muscle training on exercise performance in healthy individuals: a systematic review and meta-analysis. Sports Med. 2012;42(8):707–24. https://doi.org/10.1007/BF03262290.
Lista-Paz A, Bouza Cousillas L, Jácome C, Fregonezi G, Labata-Lezaun N, Llurda-Almuzara L, Pérez-Bellmunt A. Effect of respiratory muscle training in asthma: a systematic review and meta-analysis. Ann Phys Rehabil Med. 2023;66(3):101691. https://doi.org/10.1016/j.rehab.2022.101691.
Hilton N, Solis-Moya A. Respiratory muscle training for cystic fibrosis. Cochrane Database Syst Rev. 2018;5(5):CD006112. https://doi.org/10.1002/14651858.CD006112.pub4. Update in: Cochrane Database Syst Rev. 2020;12:CD006112. doi: 10.1002/14651858.CD006112.pub5.
Del Corral T, Fabero-Garrido R, Plaza-Manzano G, Fernández-de-Las-Peñas C, Navarro-Santana MJ, López-de-Uralde-Villanueva I. Minimal clinically important differences in inspiratory muscle function variables after a respiratory muscle training programme in individuals with long-term post-COVID-19 symptoms. J Clin Med. 2023;12(7):2720. https://doi.org/10.3390/jcm12072720.
Laciuga H, Rosenbek JC, Davenport PW, Sapienza CM. Functional outcomes associated with expiratory muscle strength training: narrative review. J Rehabil Res Dev. 2014;51(4):535–46. https://doi.org/10.1682/JRRD.2013.03.0076.
Yao XH, Li TY, He ZC, Ping YF, Liu HW, Yu SC, et al. [A pathological report of three COVID-19 cases by minimal invasive autopsies]. Zhonghua Bing Li Xue Za Zhi. 2020;49(5):411–7. https://doi.org/10.3760/cma.j.cn112151-20200312-00193. Chinese.
Bradley BT, Maioli H, Johnston R, Chaudhry I, Fink SL, Xu H, et al. Histopathology and ultrastructural findings of fatal COVID-19 infections in Washington State: a case series. Lancet. 2020;396(10247):320–32. https://doi.org/10.1016/S0140-6736(20)31305-2.
Mendes Xavier D, Lanza Galvão E, Aliane Fonseca A, de Souza GM, Pereira Lima V. Effects of Home-based Pulmonary Rehabilitation on Dyspnea, Exercise Capacity, Quality of Life and Impact of the Disease in COPD patients: a systematic review. COPD. 2022;19(1):18–46. https://doi.org/10.1080/15412555.2021.2020234.
Junior MGDN, Xavier DM, Abreu RAL, da Silva LF, de Miranda JP, Aquino MJDV, et al. Home Based Rehabilitation in Children and adolescents with cystic fibrosis: a systematic review with Meta-Analysis and Grade recommendations. Phys Occup Ther Pediatr. 2023;43(5):528–47. https://doi.org/10.1080/01942638.2023.2169093.
Acknowledgements
We would like to thank Conselho Nacional de Desenvolvimento Científico e Tecnológico (National Council for Scientific and Technological Development) (CNPq), Coordenação de Aperfeiçoamento de Pessoal de Nível Superior (Coordination for the Improvement of Higher Education Personnel) (CAPES), and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (Research Support Foundation for the State of Minas Gerais) (FAPEMIG) for support and grants.
Funding
This study was financed in part by the Coordenação de Aperfeiçoamento de Pessoal de Nível Superior - Brasil (CAPES) - Finance Code 001 and Fundação de Amparo à Pesquisa do Estado de Minas Gerais (FAPEMIG) - APQ-00062-18This work was supported by the Fundação de Amparo à Pesquisa de Minas Gerais (FAPEMIG).
Author information
Authors and Affiliations
Contributions
D.M.X.: Conceptualization, Methodology, Formal analysis, Investigation, Writing - Original Draft; R.A.L.A.: Conceptualization, Methodology, Formal analysis, Investigation, Writing - Original Draft; F.G.C.: Methodology, Writing - Review & Editing; W.T.S.:Formal analysis, Writing - Review & Editing, Supervision; S.N.S.: Writing - Review & Editing; E.L.G.: Writing - Review & Editing; M.Ga.N.J.: Writing - Review & Editing, Supervision.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution-NonCommercial-NoDerivatives 4.0 International License, which permits any non-commercial use, sharing, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if you modified the licensed material. You do not have permission under this licence to share adapted material derived from this article or parts of it. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by-nc-nd/4.0/.
About this article
Cite this article
Xavier, D.M., Abreu, R.A.L., Corrêa, F.G. et al. Effects of respiratory muscular training in post-covid-19 patients: a systematic review and meta-analysis of randomized controlled trials. BMC Sports Sci Med Rehabil 16, 181 (2024). https://doi.org/10.1186/s13102-024-00954-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-024-00954-x