Abstract
Background
To assess the feasibility, acceptability, safety, and short-term benefits of a tailored cardiac rehabilitation program for children and adolescents with long QT syndrome (LQTS).
Methods
Eight participants, aged between 6 and 18, with a positive LQTS genotype and impaired cardiorespiratory fitness, were enrolled in a 12-week centre-based cardiac rehabilitation program. The program included supervised exercise training group sessions (aerobic, resistance, and outdoor activities) and patient education workshops. Feasibility, acceptability, and safety of the program were prospectively monitored. Feedback from the parents, children, and professionals involved was collected from qualitative interviews. Short-term effects on cardiorespiratory fitness, muscle fitness, physical activity, and health-related quality of life (HRQoL) were measured between baseline and the end of the program.
Results
Retention (88% with one participant dropping out) and adherence (79%) rates were good, and no cardiac events occurred during the 12-week intervention period. Participants, parents, and healthcare professionals expressed a high level of satisfaction with the program. A significant increase between the beginning and the end of the program was observed for ventilatory anaerobic threshold (21.7±5.2 vs. 28.7±5.1 mL/kg/min, P=0.01, effect size=0.89), grip strength, (18±5.3 Kg vs. 20±4.7 Kg, P=0.02, effect size=0.90), lower limb explosive strength (142±36.5 cm vs. 148±24 cm, P=0.02, effect size=0.90), and parent-reported physical health dimension of HRQoL (65.6±9.75 vs. 84.4±20.35, P=0.03, effect size=0.87).
Conclusions
A 12-week tailored centre-based cardiac rehabilitation program was feasible, acceptable, and safe for children with LQTS. Cardiac rehabilitation for children with LQTS presents a new approach aligned with secondary prevention in youth with cardiac diseases.
Trial registration
The trial was registered at Clinicaltrials.gov (NCT05964322, registration date: 27/07/2023).
Similar content being viewed by others
Background
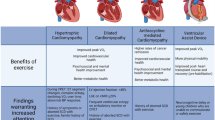
Children and adolescents who engage in physical activity experience many health benefits, including reduced cardiometabolic risk [1] and depression, [2] as well as improved cardiorespiratory fitness, better quality of life, [3] and a lower risk of chronic disease [4]. A large proportion of the pediatric population with or without chronic conditions fail to meet the recommended guidelines of 60 min per day of moderate-to-vigorous physical activity [5]. In children with chronic conditions, physical inactivity is associated with lower cardiorespiratory fitness, [6] i.e., an independent marker of all-cause mortality in the adult population [7]. Conversely, children with chronic conditions who have been physically active since childhood are less likely to become sedentary adults, [8] which, can ultimately reduce the risk for all-cause mortality by a third [9].
In children with inherited cardiac disease, promoting physical activity remains challenging because of the risk of sudden death during exercise. This is particularly true for children with long QT syndrome (LQTS), the most common inherited cardiac arrhythmia, which has long been restricted in permissible physical activities. Despite any strong evidence justifying this precautionary approach. Limiting physical activities and sports in youth with LQTS has potentially harmful psychological and physical effects, and may expose them to increased cardiovascular risk in adulthood [10, 11]. The latest sports guidelines for heart disease patients have introduced the notion of shared decision-making, [12] nevertheless, these recommendations have not been routinely transposed to children with LQTS. These young patients remain prone to an early onset of cardiorespiratory and muscle fitness impairment, [13] which, cumulated to the level of anxiety commonly reported in this population, may result in poor quality of life and mental health [14,15,16].
Cardiac rehabilitation programs have emerged in children with congenital heart disease, reporting excellent safety and efficacy on quality of life, physical fitness, and physical activity [17, 18]. Cardiac rehabilitation is defined by the World Health Organization as “the coordinated sum of activity and interventions required to ensure the best possible physical, mental, and social conditions so that patients may, by their own efforts, preserve or resume their proper place in society and lead an active life”. To the best of our knowledge, cardiac rehabilitation has not been evaluated in youth with LQTS. Yet, modern holistic models of preventive care developed in youth with congenital heart disease [17] could be of interest to children with LQTS, considering their potential need for supervised aerobic and resistance training, therapeutic education, and psychological support [13, 14].
The RYTHMO’FIT pilot study investigated the feasibility, acceptability, safety, and short-term efficacy of a structured cardiac rehabilitation program dedicated to children and adolescents with LQTS.
Methods
Study design and population
The prospective RYTHMO’FIT pilot study was performed from May 2022 to March 2023 in a pediatric cardiac rehabilitation centre experienced in clinical trials involving preventive cardiology (Saint-Pierre Institute, Palavas-Les-Flots, France). The study was reported following CONSORT guidelines for pilot studies, providing a checklist [19] [Additional file 1].
Children aged 6 to 18 years with an LQTS, characterized by a QT prolongation in repeated 12-lead electrocardiogram (ECG), and/or an LQTS-causative genetic mutation identified after familial screening, were screened from our recently reported cohort on cardiorespiratory fitness in children with LQTS [13]. Children with impaired cardiorespiratory fitness, assessed by a standardized pediatric cardiopulmonary exercise test (CPET), and defined by a peak oxygen uptake (VO2 peak) <80% of predicted values and/or a ventilatory anaerobic threshold (VAT) <55% of predicted values, were eligible for the study [17].
The RYTHMO’FIT cardiac rehabilitation program
Core program
The RYTHMO’FIT program was built using the major components of cardiac rehabilitation, such as exercise training, patient education, psychosocial support, and was adapted to the population of children and adolescents with LQTS. The program was an addition to current practice and did not replace any existing treatment. The intervention was described following the template for intervention description and replication checklist (TIDier) [20] [Additional file 2] .
A multidisciplinary group of healthcare professionals specialising in pediatric cardiac rehabilitation was established, including a pediatric cardiologist, an advanced practice nurse, an exercise physiologist, a dietitian, and a psychologist. Based on previous research on congenital heart disease [17] and in the absence of prior safety data on cardiac rehabilitation in the LQTS population, the group drafted a 12-week centre-based program. The content of each component (e.g. exercise training, patient education, and psychosocial support) was discussed using a decision-making approach. All professionals involved in the program were informed of the various stages of program development and invited to give their opinions where appropriate. The final version of the RYTHMO’FIT program included two periods (weeks 1 to 6 and weeks 6 to 12) and three different cohorts of 2 to 3 participants by age group (two for 6-12 years and one for 13-18 years old). The initial visit involved pediatric cardiology consultation, an interview with the exercise physiologist and advanced practice nurse, and the assessment of baseline outcomes (for example, ECG, echocardiography, and CPET). Each session incorporated a consultation with a pediatric cardiologist, completion of a questionnaire on exercise intensity and adaptations, and healthcare visits. The final visit was similar to the initial visit.
Exercise training
The 12-week exercise training component of the program was built around achievable goals, adapted exercises, and an emphasis on positive reinforcement. Exercise training sessions were supervised by an exercise physiologist, and took place in an equipped gymnasium and on an outside field. After each exercise session, the exercise physiologist collected patient feedback on any difficulties encountered during the sessions, their levels of satisfaction, and ideas for potential improvement.
Participants’ heart rates were continuously monitored by exercise physiologists using wireless ECG sensors (Auxil ECG; Auxil Science GmbH, Germany) attached to their chests. A pulse oximeter and external defibrillator were available during each exercise session. The pediatric cardiologist was always present in the rehabilitation centre during the exercise sessions. From weeks 1 to 6, two exercise sessions of 60 minutes each per week were held, including one aerobic session and one resistance training session. From weeks 7 to 12, one exercise session of 60 minutes per week was held, which combined aerobic and resistance training. Each session included a 5-minute warm-up, 30 min of individualised aerobic/resistance training, 25 min of group activities (e.g. basketball, football, squash), and cooldown and feedback with the exercise physiologist.
Aerobic sessions relied on indoor cycling interval training (2 to 3 repetitions of 10 min bouts with 3 to 5 min of active recovery) at the VAT’s heart rate and workload, determined by baseline CPET assessment. During the program, the workload, duration, and frequency of working bouts progress according to the patient's perceived level of exhaustion. Resistance training sessions were held at the local gymnasium using various materials (e.g. hoops, elastic bands, play mats, and kettlebells) and included two different circuit training workouts (upper and lower limbs) of four exercises each (e.g. push-ups, squats, bear walking). Initially, the children learned the movement with no additional weight. Set and progressive loads were recorded over the weeks and adjusted according to patient characteristics, perceived exhaustion, and movement execution. When the participant was unable to perform the required execution movement properly, personalized support from an exercise physiologist was provided. After completing either aerobic or resistance training, participants engaged in a variety of physical activities adapted. Intensity was monitored using ECG sensors and perceived exhaustion. Activities were diversified and adapted to patients’ spontaneous desires to enhance their engagement and interest. Before each session, the participants voted and decided collectively on the activities proposed by the exercise physiologist. Team games, small competitions, and music were integrated into each session to stimulate enthusiasm and motivation which were evaluated through a short questionnaire and oral feedback at the end of each session. After the last session in week 12, a celebratory snack was organised to end the program on a positive and supportive note. The exercise program is described in detail in Additional file 3 [Additional file 3].
Patient education program
During the program construction phase, educational topics relevant to the population of children with LQTS were identified, educational tools (e.g. game-based learning platforms) were selected, and interactive child-friendly presentation slides were designed to promote self-management and problem-solving techniques. An advanced practice nurse in pediatric cardiology holding board certification in patient education supervised the educational program. The educational sessions were delivered to the child and his or her family by a multidisciplinary team (advanced practice nurse, pediatric cardiologist, exercise physiologist, dietician, social worker, and psychologist).
The educational component of the cardiac rehabilitation program was divided into three parts: (1) The first one-hour individual educational session was delivered by the advanced practice nurse during the initial visit (first day of week 1) and aimed to assess participants' needs, objectives, basic knowledge of the disease, and expectations of the education program.
(2) A total of 18 half-hour educational group sessions (2 per week from week 1 to week 6, and one per week from week 7 to week 12) were delivered by the multidisciplinary team, addressing four topics: “my heart”, “my treatment”, “my daily life”, and “support”. Participants were warmly encouraged to participate, engage in discussions, and ask questions related to their lives with the LQTS. A specific group session for parents was set up and led by a pediatric cardiologist and an advanced practice nurse.
(3) The final one-hour individual session at the end of the program (the last day of week 12) was designed to gather feedback from the patient and family and to establish a personalised educational report.
The contents of the different educational workshops are further detailed in the additional file 4 [Additional file 4].
Outcomes
Feasibility, acceptability, and safety
The feasibility of the intervention was determined by (1) recruitment rate (number of participants at baseline vs. number of eligible patients), (2) retention rate (number of participants who completed the 12-week program vs. number of participants who dropped out), (3) adherence rate (number of sessions completed vs. number of sessions offered), and (4) a final self-reported questionnaire which provided patient feedback on the program (scored on a scale of 0 to 5, with comments allowed) and their overall satisfaction (scoring from 0 to 10 by patients and families).
Acceptability was determined from the qualitative data collected during all phases of the program (preparation, initiation, core program, and final assessment). Logistics issues and reasons for not attending the sessions were prospectively recorded. All comments from the participants and healthcare professionals throughout the program were aggregated to refine the assessment of the acceptability of the intervention. At the end of the program, the exercise physiologist and advanced practice nurse provided feedback through brief interviews.
Safety outcomes were prospectively collected from patient enrolment to the final visit (12-week follow-up). Serious and non-serious adverse events were analysed by the data safety and monitoring board members, to determine their relation to the intervention, as previously reported.[17]
The feasibility, acceptability, and safety data were prospectively collected by a single investigator.
Secondary outcomes
The evaluation of secondary outcomes included the assessment of cardiac parameters, cardiorespiratory fitness, muscle fitness, physical activity, and patient-reported outcomes at baseline and at the end of the 12-week program.
The cardiac parameters included clinical, ECG, conventional, and 2D-strain echocardiography data. Cardiorespiratory fitness was assessed using a standardised pediatric incremental CPET protocol: 1-minute rest; 3-minute warm-up (10–20 watts) in increments of 10, 15, or 20 watts each minute for 8-12 min; 3-minute active recovery (20 watts); and 2-minute rest [17]. The exercise test was considered maximal when two of the following criteria were reached: respiratory exchange ratio (VCO2/VO2) ≥ 1, maximum heart rate>85% of maximal age-predicted heart rate, plateau of VO2 despite the increasing exercise intensity or the patient's inability to provide a minimum pedalling frequency of 60 revolutions per minute despite verbal encouragement. The following parameters were measured: peak oxygen uptake (VO2peak), ventilatory anaerobic threshold (VAT), ventilatory efficiency (VE/VCO2 slope), maximum heart rate (HR), oxygen pulse (VO2/HR), and maximal power. The same investigator manually calculated the VO2peak and the VAT using V-slope method. The QT interval was manually measured by a single pediatric cardiologist at peak exercise and every minute of the 5-minute recovery phase, under magnification adjacent to a scale with 20-ms segments by the tangent method [21]. For each measurement of exercise ECG, 3 consecutive QT intervals and their corresponding preceding RR intervals were measured. Raw QT measurements were corrected for heart rate using the Bazett Formula (QTc= QT/ √RR, where QT and RR intervals were measured in seconds).
Muscle fitness was determined by assessing the muscle architecture and strength. Muscle architecture was evaluated using a muscular ultrasound technique, on the patient in dorsal decubitus, as previously described [13]. Four parameters were measured: (1) the anatomical cross-sectional area, (2) the pennation angle of vastus lateralis, (3) the muscle thickness of vastus lateralis, and (4) the fascicle length of vastus lateralis, which was assessed from longitudinal analysis with linear extrapolation of the length of the part of the fascicle that was not visible on the image. Five measurements were performed by a single operator for each parameter. The minimal and maximal values were excluded, and the mean of the three remaining values was calculated. Measures were considered valid when the coefficient of variation was < 5%. ImageJ software was used for image analysis. The maximal isometric strength of the lower limb was assessed using a knee extension test with an Easy Force dynamometer (Meloq AB, Sweden). Easy Force is a belt-stabilised handheld dynamometer attached to a support and then linked to the participant's ankle, which continuously records the tension force. The strap was positioned perpendicular to the anterior or posterior aspect of the tibia 5 cm proximal to the medial malleolus. The participants were seated on the edge of the examination table with the knee bent at 60° to avoid knee pain. Participants performed one submaximal trial, followed by three maximal extensions with a one-minute rest period after each trial. The maximum isometric strength of the upper limb was assessed using a handgrip test [13]. The subjects were seated on a chair without an armrest, elbow flexed at 90°, and squeezed the handgrip with their right hand for four seconds, as hard as they could. The procedure was repeated three times, with one minute’s rest between each trial. The average of the three measurements for isometric strength of both the upper and lower limbs was calculated. In the event of a variation coefficient of >5%, the participants performed an additional maximal trial. Lower body explosive muscular strength was assessed using a long-standing broad jump. The participants stood behind the jump line, feet together, and vigorously pushed forward as far as possible. If they lost balance or touched an object, they were asked to repeat the jump. The distance from the jump line to the heel landing was measured. The longest jump distance between the two trials was selected.
The level of physical activity was evaluated using a triaxial accelerometer (ActiGraph GT3X, Pensacola, FL, USA). Participants were instructed to wear it at the waist for seven days, except during sleep and water-based activities such as swimming or bathing. We chose an e-poch of 15 seconds and Evenson's equations were employed to set the intensity thresholds (counts/min) [22] to classify into four categories: light, moderate, vigorous, moderate-to-vigorous intensity, and sedentary level. A wearing period of 10 hours per day for at least 3 days was necessary for the analysis [23].
Patient-reported outcomes were evaluated using the self- and proxy-reported health-related quality of life (HRQoL) PesdQL instrument. PedsQL version 4.0, which is a generic questionnaire, has four multidimensional scales: physical functioning (eight items), emotional functioning (five items), social functioning (five items), and school functioning (five items). The three summary scores were as follows: total score (23 items), physical health summary score (eight items), and psychosocial health summary score (15 items). Each item uses a 5-point Likert scale ranging from 0 (never) to 4 (always). Items are reverse-scored and linearly transformed to a 0-100 scale, with higher scores indicating better quality of life. The psychometric properties of the PedsQL have been validated in the French Pediatric population [24].
Statistical analysis
Participants’ characteristics were presented using medians and quartiles for continuous variables and frequencies and proportions for categorical variables. The change in median differences between baseline and the end of the program was calculated using the Wilcoxon signed-rank test. The effect size was estimated using Cohen’s d measure. Statistical significance was set at 0.05, and analyses were performed using R Studio software. Given the objectives and study design of this pilot study, sample size calculation was not feasible.
Results
Feasibility, acceptability, and safety
A total of 36 patients aged between 6 and 18 years were screened for eligibility from our pediatric LQTS database. Of the 19 participants meeting the inclusion criteria, 11 declined to participate for various reasons: lack of interest (n=2), family death (n=1), transport problems (n=2), interference with the school schedule (n=4), or no answer (n=2).
Finally, eight children (seven boys and one girl) aged between 9 and 17 years (median= 11.5 years old) were enrolled in the study and participated in the baseline assessment during the initiation visit of the cardiac rehabilitation program (Fig 1), corresponding to a recruitment rate of 42%. Participants were carriers of the LQT1 (KCNQ1, n=4) or LQT2 (KCNH2, n=4) genetic mutations and were all taking beta-blockers (nadolol). The diagnosis of LQTS was made after family screening (n=4) or after a cardiac event (n=4). The corrected QT interval at baseline ECG ranged from 423 to 536 ms (mean, 474±43.5 ms). Using the Schwartz criteria for LQTS diagnosis [25], four children (50%) had a high probability (≥ 3.5 points), two had an intermediate probability (1.5 to 3 points) and two had a low probability for LQTS (≤ 1 point) (Table 1). One child had a history of refractory ventricular arrhythmias, implantable cardioverter-defibrillator, and cardiac sympathetic denervation (P5, Table 1).
After the initiation visit and baseline assessment, one adolescent dropped out of the program (participant #8 in Table 1) because of school and transport difficulties, indicating a retention rate of 88%.
Of the 114 sessions organised for the seven remaining participants, 24 sessions were not attended by the children because of interference with the school schedule (n=4), transportation issues (n=7), absence during holidays (n=8), Covid-19 infection (n=2) or hospitalisation (=3). Overall, the mean adherence rate was 79%. Two individuals fell within the 50% to 60% adherence range, while five participants had adherence levels above 75%.
Patients’ feedback about the exercise training program found that they were “very satisfied”, in terms of animation and individualized approach of the exercise physiologist, instructions understanding, and socialization during group sessions (“playing, chatting, and fun”). Participants reported being “satisfied” with the exercise session’s intensity and duration. The final questionnaire completed by patients indicated that they were “satisfied” with the intensity and duration of the exercise session, the program's ability to transform their approach to physical activity, and the perceived enhancements on mental and physical well-being. The participants rated the overall exercise training program at 9.75 over 10.
Patients’ feedback about the education program found that they were “very satisfied”, in terms of improving their understanding of the disease and medical follow-up, as well as managing their daily life. They valued the support provided by the program, the animation and individualised approach of the advanced practice nurse, and educational group sessions. Participants rated the educational program at 9.5 over 10. The most compelling feedback from parents and participants is available in Fig. 2.
Intervention highlights of the RYTHMO’FIT program. Legend: A- Sports activities group session led by an exercise physiologist, B- Gamification activities led by an exercise physiologist, C- Educational workshops supervised by an advanced practice nurse, the game-based learning platform used was Kahoot (Kahoot! app, https://kahoot.com/). Selected highlights of participants’ feedback: “This program would have been of great interest during the diagnosis of long QT syndrome where the world is collapsing on us, where football in competition is no longer possible, to support us finding a physical activity project behind.”, “I am truly excited to share this program with children who are dealing with the same disease.”, “This program has not only boosted my son's and my confidence, but it has also granted me the peace of mind to allow him to engage in more activities than before.”
In terms of acceptability, the healthcare professionals responsible for implementing the program were very satisfied, given that they had never supervised cardiac rehabilitation in children with LQTS. Twelve sessions were cancelled by the rehabilitation centre because of caregiver vacations or public holidays (deducted in calculating patient adherence). No logistical issues specific to the RYTHMOFIT program were identified compared with the pre-existing cardiac rehabilitation program routinely provided for children with congenital heart disease. In the final interview, the advanced practice nurse underlined the need to refine the educational content for the youngest patients (8-10 years old). The exercise physiologist also advised extending the session to include both aerobic and resistance training, spacing out interventions throughout the day, and implementing a child-friendly heart rate monitoring device, rather than ECG monitoring.
No serious adverse events were reported during the cardiac rehabilitation program. The following non-serious events associated with the exercise sessions were reported: muscle soreness (n=4, resistance training) and fatigue (n=4, aerobic training). Additional non-cardiac events unrelated to exercise sessions included muscle soreness after physical education sessions (n=2), Covid-19 and other infections (n=6), hospitalisations due to gastroenteritis (n=2), fatigue after prolonged transportation to the hospital (n=4), and sleep disorders (n=2). During the rehabilitation program, no modification of the routine cardiac follow-up of the patient was observed, and the dosage of beta-blockers remained unchanged.
Short-term efficacy
The patient characteristics remained unchanged between baseline and the end of the cardiac rehabilitation program (n=7) for anthropometric data (weight, height, and body mass index) and functional cardiac parameters at rest (ECG and echocardiography) (Table 2).
In terms of cardiorespiratory fitness, we observed a significant increase between baseline and the end of the cardiac rehabilitation program for the VAT expressed in weight-normalized values (21.7±5.2 mL/min/kg vs. 28.7±5.1 mL/min/kg, P=0.01, effect size=0.89) or percent-predicted values (48±8.6% vs. 61±11.5%, P=0.04, effect size=0.80). A significant increase in maximal systolic blood pressure during exercise was also observed (110±10.0 mmHg vs. 120±20.0, P=0.03, effect size=0.88). Between baseline and final ECG assessment, the QTc interval values at rest, peak exercise, and during recovery remained unchanged.
Muscle fitness significantly improved for upper limb grip strength (18±5.3 Kg vs. 20±4.7 Kg, P=0.02, effect size=0.90) and lower limb explosive strength (142±36.5 cm vs. 148±24 cm, P=0.02, effect size=0.90).
Actigraph quality criteria were appropriate at baseline (5±1.5 days and 12.51±1.05 hours per day) and at final assessment (5±3.5 days and 12.1±1.32 hours per day). One participant did not fulfil the valid criteria and was excluded from the analysis (n=6). No significant change in physical activity level was observed between the baseline and final assessments.
Parent-reported physical health scores of HRQoL significantly improved during the program (65.6±9.8 vs. 84.4±20.4, P=0.03, effect size=0.87). However, these improvements were no longer significant when taking into account Holm's adjustment for multiple comparisons (P=0.18).
Discussion
The RYTHMO’FIT study reported, for the first time, the implementation of a structured centre-based cardiac rehabilitation program in children with LQTS with good feasibility, acceptability, safety, and short-term efficacy.
This cardiac rehabilitation program dedicated to children with LQTS represents a new care pathway that has demonstrated positive feasibility and acceptability to patients, parents, and healthcare professionals alike. In pediatric LQTS, it is commonly difficult for caregivers and families to strike a balance between the risk of sudden death and the promotion of physical activity. The precautionary principle has long been applied, but restrictions on physical activity in patients with a genetic heart disease may lead to an increased incidence of depression, hopelessness, obesity, and suicidal ideation [26]. The 2020 ESC guidelines have initiated a positive move towards encouraging physical activity in patients with cardiovascular disease, especially by implementing the idea of shared decision-making between patients and physicians [12]. However, these guidelines are intended for the adult population, and it remains difficult to put them into practice during a routine pediatric cardiology consultation. Therefore, cardiac rehabilitation for children with LQTS, through targeted therapeutic education and supervised physical training, presents a new approach to managing these patients, consistent with the development of preventive cardiology in early childhood [27]. Interestingly, the good levels of feasibility and acceptability of the RYTHMO’FIT program are similar to those of rehabilitation programs delivered in clinical routine practice to patients with congenital heart disease [17, 28].
Furthermore, the 12-week exercise program implemented in the cardiac rehabilitation centre was found to be safe, as no adverse cardiac events were recorded, no alterations in the QTc interval were detected, and no adjustments to medical treatment were deemed necessary. This aligns with previous research on appropriately managed children with LQTS [11] and recent evidence supporting the safety of promoting physical activity in this population [11, 29]. A pilot study in asymptomatic adult patients with type 1 LQTS showed no cardiac events and unchanged QTc intervals at rest and during exercise recovery from moderate-intensity exercise programs [30]. Our research suggests that these findings might also apply to children and adolescents with both 1 and 2 LQTS genotypes. Further research on larger cohorts remains necessary to explore individualised responses to exercise based on LQTS genotype and patterns of QT interval adjustments from increased parasympathetic activity during exercise [10, 31]. The absence of cardiac events also aligns with the general principle that the benefits typically outweigh the risks for children with chronic conditions [32]. Overall, these findings may contribute to overcoming common obstacles to physical activity in LQTS, including parental overprotection, lack of motivation, and fear of cardiac events during exercise [33, 34].
In terms of short-term efficacy, this tailored cardiac rehabilitation program improved some major components of cardiorespiratory fitness, muscle fitness, and HRQoL. In terms of cardiorespiratory fitness, the extent of the ventilatory anaerobic threshold (VAT) improvement observed in this study (+24%) aligns with the most effective cardiac rehabilitation programs in children with congenital heart disease (+23%) [18]. Given that VAT is an indicator of physical fitness linked to HRQoL, improving this submaximal parameter through moderate-intensity exercise training stands as an important finding. Children with chronic conditions often experience shortness of breath after moderate exertion, which is a strong indicator of physical deconditioning, and is commonly referred to as impaired VAT. Cardiac rehabilitation programs commonly use the VAT to determine the level of exercise training, as in interval training workouts [17].
Concerning muscle fitness, the intervention also enhanced strength without notable changes to muscle architecture or mass, suggesting neuromuscular adaptations, as seen in healthy children undergoing resistance training [35]. At the end of the program, children with LQTS bridged the gap with healthy children by attaining comparable levels of strength [13, 36, 37]. These positive outcomes are of interest as poor muscle strength is associated with an increased risk of cardiometabolic diseases and impairments in neurodevelopmental and bone disorders [38].
Finally, the RYTHMO’FIT program did not change the self- and proxy-reported HRQOL. The effectiveness of cardiac rehabilitation for children has been previously assessed by measuring HRQoL as the primary outcome [39]. Interestingly, the physical health dimension showed an increase in parents' reports after the program, although not statistically significant after accounting for multiple comparisons, and despite low baseline levels compared to children's self-reports. Classically, in children with cardiac disease, parent-reported HRQoL in the physical dimension is lower than self-reported HRQoL [40] but the correlation between HRQoL scores and cardiorespiratory fitness (VO2peak) is better when assessed by parents than by children themselves [41, 42]. These results may also indicate that parents have a more unfavourable view of their child's physical health, which could underline parental overprotection. Parental overprotection could be mitigated at the end of the program to align with self-reported HRQoL.
The levels of moderate-to-vigorous physical activity in children and adolescents with long QT syndrome were not different from previously published data [13, 34] but remained lower than the general population, which typically engages in more than 50 minutes of moderate-to-vigorous physical activity per day [43, 44]. Although some physical activity programs have shown promising results in terms of improving HRQoL and physical activity level [17, 45, 46], others have failed to demonstrate significant positive changes in children with congenital heart disease [47,48,49].
Hence, certain aspects of the intervention design can be refined to enhance its efficacy for future studies involving larger sample sizes. Transforming the program into a hybrid or home-based model could provide greater flexibility and the opportunity to conduct three sessions per week, which is the most commonly used approach [50]. The recent QUALIREHAB hybrid program designed by our group showed a positive and significant change in physical activity and HRQOL [17]. Incorporating motivational and coaching sessions with an exercise physiologist and emphasizing parental involvement can enhance daily physical activity through autonomous active behaviours [51, 52]. Future studies should examine the long-term maintenance of active behaviours following the program in a larger sample to confirm these results in long QT syndrome.
The RYTHMO'FIT program presents numerous promising opportunities for the future. Exercise training programs could be a way to gradually engage children in physical activities based on individual needs to meet the WHO guidelines [17, 46]. The educational program could play a major role in understanding LQTS mechanisms and treatments. The program may support the shared decision-making process for sports participation, enabling individuals to redefine their pathways after diagnosis and consider other less intense physical activities. Future research should assess the long-term sustainability of physical activity after the program, for instance, by evaluating whether individuals join a sports club or association to maintain active behaviours.
Nevertheless, the RYTHMO’FIT program could be improved to increase its feasibility and acceptability among children and parents. First, only one girl, aged 9, with the highest QTc (536 ms), participated in the program. Previous research has suggested that female sex and the onset of puberty could trigger LQTS-related complications, such as polymorphic ventricular arrhythmia or sudden cardiac death [53]. To confirm the accuracy of our results, future exercise programs should ensure a balanced distribution of male and female participants. Additionally, gender disparities in physical activity seem to persist in the female pediatric cardiac population, affected by lower levels of physical activity, [43] early decline in cardiopulmonary fitness, [54] and, ultimately, poorer HRQoL [40]. Overall, the low recruitment rate and incomplete participation may be due to the centre-based design, which involves frequent transportation and interference with school schedules. To address these issues, transitioning to a hybrid or home-based model may be beneficial as a cost-effective alternative delivery method. Based on the QUALIREHAB hybrid cardiac rehabilitation model designed by our group, future hybrid centre- and home-based programs could pave the way for a new horizon in managing young patients with LQTS [17].
Study limitations
This pilot study enrolled a small number of patients and was not designed to assess the efficacy of the intervention. No significant increase in peak VO2, e.g., a major predictor of cardiovascular health, has been observed in this study, probably due to the moderate level of exercise training delivered by the program. Indeed, high-intensity physical activity is associated with higher cardiorespiratory fitness [55]. One potential limitation is the lack of QTc measurements during the exercise sessions, given the possible role of regular physical activity in regulating the balance between the parasympathetic and sympathetic nervous systems [56]. Effectiveness also needs to be demonstrated over the longer term. Therefore, future research relying on randomized controlled trials remains necessary to draw conclusions with a higher level of evidence.
Conclusion
In the RYTHMO’FIT pilot study, the feasibility, acceptability, and safety of a 12-week centre-based cardiac rehabilitation program tailored for children with LQTS were good. The program’s short-term efficacy was also positive in terms of cardiorespiratory fitness and muscle fitness. In line with the emergence of preventive cardiology from an early age, cardiac rehabilitation in children with LQTS opens up a new avenue in the management of these young patients and could be extended to the adult population.
Availability of data and materials
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- CPET:
-
Cardiopulmonary exercise test
- ECG:
-
Electrocardiogram
- HRQoL:
-
Health-related quality of life
- LQTS:
-
Long QT syndrome
- VAT:
-
Ventilatory anaerobic threshold
- VO2 peak :
-
Peak oxygen uptake
- WHO:
-
World health organisation
References
Kallio P, Pahkala K, Heinonen OJ, Tammelin TH, Pälve K, Hirvensalo M, et al. Physical inactivity from youth to adulthood and adult cardiometabolic risk profile. Prev Med. 2021;145:106433.
Redig L, Feter N, Dumith SC, Domingues MR, Rombaldi AJ. Physical inactivity from childhood to adolescence and incident depression. Am J Prev Med. 2022;62(2):211–8.
Wu XY, Han LH, Zhang JH, Luo S, Hu JW, Sun K. The influence of physical activity, sedentary behavior on health-related quality of life among the general population of children and adolescents: A systematic review. PLoS ONE. 2017;12(11):e0187668. https://doi.org/10.1371/journal.pone.0187668.
Poitras V, Gray C, Borghese M, Carson V, Chaput J, Janssen I, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S197-239.
World Health Organization. WHO Guidelines on Physical Activity and Sedentary Behaviour. 2020; Available from: http://www.ncbi.nlm.nih.gov/books/NBK566045/.
Maggio ABR, Hofer MF, Martin XE, Marchand LM, Beghetti M, Farpour-Lambert NJ. Reduced physical activity level and cardiorespiratory fitness in children with chronic diseases. Eur J Pediatr. 2010;169(10):1187–93. https://doi.org/10.1007/s00431-010-1199-2. (Cited 2023 Aug 8).
Raghuveer G, Hartz J, Lubans D, Takken T, Wiltz J, Mietus-Snyder M, et al. Cardiorespiratory fitness in youth: an important marker of health: a scientific statement from the American Heart Association. Circulation. 2020;142(7):E101-18.
Telama R, Yang X, Leskinen E, Kankaanpää A, Hirvensalo M, Tammelin T, et al. Tracking of physical activity from early childhood through youth into adulthood. Med Sci Sports Exerc. 2014;46(5):955–62.
Saint-Maurice PF, Coughlan D, Kelly SP, Keadle SK, Cook MB, Carlson SA, et al. Association of leisure-time physical activity across the adult life course with all-cause and cause-specific mortality. JAMA Netw Open. 2019;2(3):e190355.
Harvey A, Curnier D, Dodin P, Abadir S, Jacquemet V, Caru M. The influence of exercise and postural changes on ventricular repolarization in the long QT syndrome: a systematic scoping review. Eur J Prev Cardiol. 2022;29(12):1633–77.
Chambers KD, Beausejour Ladouceur V, Alexander ME, Hylind RJ, Bevilacqua L, Mah DY, et al. Cardiac events during competitive, recreational, and daily activities in children and adolescents with long QT syndrome. J Am Heart Assoc. 2017;6(9):e005445.
Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, et al. 2020 ESC Guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42(1):17–96.
Souilla L, Avesani M, Boisson A, Requirand A, Matecki S, Vincenti M, et al. Cardiorespiratory fitness, muscle fitness, and physical activity in children with long QT syndrome: A prospective controlled study. Front Cardiovasc Med. 2023;9. Available from: https://www.frontiersin.org/articles/10.3389/fcvm.2022.1081106. Cited 2023 Mar 7.
Longmuir PE, Sampson M, Ham J, Weekes M, Patel BJ, Gow RM. The mental health of adolescents and pre-adolescents living with inherited arrhythmia syndromes: a systematic review of the literature. Cardiol Young. 2018;28(5):621–31.
Czosek RJ, Kaltman JR, Cassedy AE, Shah MJ, Vetter VL, Tanel RE, et al. Quality of life of pediatric patients with long QT syndrome. Am J Cardiol. 2016;117(4):605–10.
Giuffre RM, Gupta S, Crawford SG, Leung AKC. Fears and anxiety in children with long-QT syndrome compared to children with asthma. J Natl Med Assoc. 2008;100(4):420–4.
Amedro P, Gavotto A, Huguet H, Souilla L, Huby AC, Matecki S, et al. Early hybrid cardiac rehabilitation in congenital heart disease: the QUALIREHAB trial. Eur Heart J. 2024;ehae085. https://doi.org/10.1093/eurheartj/ehae085. Cited 2024 Mar 4.
Rhodes J, Curran TJ, Camil L, Rabideau N, Fulton DR, Gauthier NS, et al. Impact of cardiac rehabilitation on the exercise function of children with serious congenital heart disease. Pediatrics. 2005;116(6):1339–45. https://doi.org/10.1542/peds.2004-2697.
Eldridge SM, Chan CL, Campbell MJ, Bond CM, Hopewell S, Thabane L, et al. CONSORT 2010 statement: extension to randomised pilot and feasibility trials. Pilot Feasibility Stud. 2016;2(1):64. https://doi.org/10.1186/s40814-016-0105-8. (Cited 2023 Jun 4).
Rhon DI, Fritz JM, Kerns RD, McGeary DD, Coleman BC, Farrokhi S, et al. TIDieR-telehealth: precision in reporting of telehealth interventions used in clinical trials - unique considerations for the Template for the Intervention Description and Replication (TIDieR) checklist. BMC Med Res Methodol. 2022;22(1):161. https://doi.org/10.1186/s12874-022-01640-7. (Cited 2023 Jul 19).
Berger W, Gow R, Kamberi S, Cheung M, Smith K, Davis A. The QT and corrected QT interval in recovery after exercise in children. Circ-ARRHYTHMIA Electrophysiol. 2011;4(4):448-U89.
Evenson KR, Catellier DJ, Gill K, Ondrak KS, McMurray RG. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–65.
Voss C, Duncombe SL, Dean PH, de Souza AM, Harris KC. Physical Activity and Sedentary Behavior in Children With Congenital Heart Disease. J Am Heart Assoc Cardiovasc Cerebrovasc Dis. 2017;6(3):e004665. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5524004/. Cited 2022 Nov 26.
Amedro P, Huguet H, Macioce V, Dorka R, Auer A, Guillaumont S, et al. Psychometric validation of the French self and proxy versions of the PedsQLTM 4.0 generic health-related quality of life questionnaire for 8–12 year-old children. Health Qual Life Outcomes. 2021;19(1):75. https://doi.org/10.1186/s12955-021-01714-y. (Cited 2023 Aug 8).
Schwartz P, Crotti L. QTc behavior during exercise and genetic testing for the long-QT syndrome. Circulation. 2011;124(20):2181–4.
Etheridge SP, Saarel EV. Toward a long and happy life of a patient with genetic heart disease. J Am Coll Cardiol. 2021;78(6):605–7.
Raitakari O, Pahkala K, Magnussen CG. Prevention of atherosclerosis from childhood. Nat Rev Cardiol. 2022;19(8):543–54.
Duppen N, Takken T, Hopman MTE, ten Harkel ADJ, Dulfer K, Utens EMWJ, et al. Systematic review of the effects of physical exercise training programmes in children and young adults with congenital heart disease. Int J Cardiol. 2013;168(3):1779–87.
Gow RM, Borghese MM, Honeywell CR, Colley RC. Activity intensity during free-living activities in children and adolescents with inherited arrhythmia syndromes: assessment by combined accelerometer and heart rate monitor. Circ Arrhythm Electrophysiol. 2013;6(5):939–45. https://doi.org/10.1161/CIRCEP.113.000514.
Perhonen M, Haapalahti P, Kivisto S, Hekkala A, Vaananen H, Swan H, et al. Effect of physical training on ventricular repolarization in type 1 long QT syndrome: a pilot study in asymptomatic carriers of the G589D KCNQ1 mutation. Europace. 2006;8(10):894–8.
Schuit AJ, Dekker JM, de Vegt F, Verheij TC, Rijneke RD, Schouten EG. Effect of physical training on QTc interval in elderly people. J Electrocardiol. 1998;31(2):111–6.
Reid H, Ridout AJ, Tomaz SA, Kelly P, Jones N. Benefits outweigh the risks: a consensus statement on the risks of physical activity for people living with long-term conditions. Br J Sports Med. 2022;56(8):427–38. Available from: https://bjsm.bmj.com/content/56/8/427. Cited 2023 Aug 14.
Moncion K, Gardin L, Lougheed J, Adamo K, Longmuir PE. Children with Cardiomyopathy have Active Lifestyles Despite Reporting Disease-Specific Barriers to Physical Activity: A Mixed-Methods Study. Exerc Med. 2022;6. https://doi.org/10.26644/em.2022.004.
Christian S, Somerville M, Taylor S, Spence JC, Giuffre M, Atallah J. The impact of physical activity modification on the well-being of a cohort of children with an inherited arrhythmia or cardiomyopathy. Cardiol Young. 2020;30(5):692–7.
Ramsay JA, Blimkie CJ, Smith K, Garner S, MacDougall JD, Sale DG. Strength training effects in prepubescent boys. Med Sci Sports Exerc. 1990;22(5):605–14.
Castro-Piñero J, Ortega FB, Artero EG, Girela-Rejón MJ, Mora J, Sjöström M, et al. Assessing muscular strength in youth: usefulness of standing long jump as a general index of muscular fitness. J Strength Cond Res. 2010;24(7):1810–7.
Bohannon RW, Wang YC, Bubela D, Gershon RC. Handgrip strength: a population-based study of norms and age trajectories for 3- to 17-year-olds. Pediatr Phys Ther Off Publ Sect Pediatr Am Phys Ther Assoc. 2017;29(2):118–23.
Orsso CE, Tibaes JRB, Oliveira CLP, Rubin DA, Field CJ, Heymsfield SB, et al. Low muscle mass and strength in pediatrics patients: why should we care? Clin Nutr Edinb Scotl. 2019;38(5):2002–15.
Williams CA, Wadey C, Pieles G, Stuart G, Taylor RS, Long L. Physical activity interventions for people with congenital heart disease. Cochrane Database Syst Rev. 2020;10:CD013400. https://doi.org/10.1002/14651858.CD013400.pub2.
Amedro P, Dorka R, Moniotte S, Guillaumont S, Fraisse A, Kreitmann B, et al. Quality of Life of Children with Congenital Heart Diseases: A Multicenter Controlled Cross-Sectional Study. Pediatr Cardiol. 2015;36(8):1588–601. https://doi.org/10.1007/s00246-015-1201-x.
Amedro P, Picot MC, Moniotte S, Dorka R, Bertet H, Guillaumont S, et al. Correlation between cardio-pulmonary exercise test variables and health-related quality of life among children with congenital heart diseases. Int J Cardiol. 2016;15(203):1052–60.
Jacobsen RM, Ginde S, Mussatto K, Neubauer J, Earing M, Danduran M. Can a Home-based Cardiac Physical Activity Program Improve the Physical Function Quality of Life in Children with Fontan Circulation? Congenit Heart Dis. 2016;11(2):175–82. Available from: https://onlinelibrary.wiley.com/doi/abs/10.1111/chd.12330 . Cited 2024 Jun 13.
Kretschmer L, Salali GD, Andersen LB, Hallal PC, Northstone K, Sardinha LB, et al. Gender differences in the distribution of children’s physical activity: evidence from nine countries. Int J Behav Nutr Phys Act. 2023;20(1):103.
Ikeda E, Guagliano JM, Atkin AJ, Sherar LB, Ekelund U, Hansen B, et al. Cross-sectional and longitudinal associations of active travel, organised sport and physical education with accelerometer-assessed moderate-to-vigorous physical activity in young people: the International Children’s Accelerometry Database. Int J Behav Nutr Phys Act. 2022;19(1):41. https://doi.org/10.1186/s12966-022-01282-4. Cited 2023 Dec 19.
Hedlund ER, Lundell B, Söderström L, Sjöberg G. Can endurance training improve physical capacity and quality of life in young Fontan patients? Cardiol Young. 2018;28(3):438–46. https://doi.org/10.1017/S1047951117002360.
Morrison ML, Sands AJ, McCusker CG, McKeown PP, McMahon M, Gordon J, et al. Exercise training improves activity in adolescents with congenital heart disease. Heart Br Card Soc. 2013;99(15):1122–8.
Meyer M, Brudy L, Fuertes-Moure A, Hager A, Oberhoffer-Fritz R, Ewert P, Müller J. E-Health Exercise Intervention for Pediatric Patients with Congenital Heart Disease: A Randomized Controlled Trial. J Pediatr. 2021;233:163–8. https://doi.org/10.1016/j.jpeds.2021.01.058.
Klausen SH, Andersen LL, Søndergaard L, Jakobsen JC, Zoffmann V, Dideriksen K, et al. Effects of eHealth physical activity encouragement in adolescents with complex congenital heart disease: The PReVaiL randomized clinical trial. Int J Cardiol. 2016;221:1100–6. Available from: https://doi.org/10.1016/j.ijcard.2016.07.092.
Duppen N, Etnel JR, Spaans L, Takken T, van den Berg-Emons RJ, Boersma E, et al. Does exercise training improve cardiopulmonary fitness and daily physical activity in children and young adults with corrected tetralogy of Fallot or Fontan circulation? A randomized controlled trial. Am Heart J. 2015;170(3):606–14. https://doi.org/10.1016/j.ahj.2015.06.018.
Meyer M, Brudy L, García-Cuenllas L, Hager A, Ewert P, Oberhoffer R, et al. Current state of home-based exercise interventions in patients with congenital heart disease: a systematic review. Heart Br Card Soc. 2020;106(5):333–41.
Callaghan S, Morrison ML, McKeown PP, Tennyson C, Sands AJ, McCrossan B, et al. Exercise prescription improves exercise tolerance in young children with CHD: a randomised clinical trial. Open Heart. 2021;8(1):e001599.
Longmuir PE, Tyrrell PN, Corey M, Faulkner G, Russell JL, McCrindle BW. Home-based rehabilitation enhances daily physical activity and motor skill in children who have undergone the Fontan procedure. Pediatr Cardiol. 2013;34(5):1130–51. https://doi.org/10.1007/s00246-012-0618-8. (Cited 2023 Jul 23).
Costa S, Saguner AM, Gasperetti A, Akdis D, Brunckhorst C, Duru F. The link between sex hormones and susceptibility to cardiac arrhythmias: from molecular basis to clinical implications. Front Cardiovasc Med. 2021;8:644279.
Amedro P, Gavotto A, Guillaumont S, Bertet H, Vincenti M, De La Villeon G, et al. Cardiopulmonary fitness in children with congenital heart diseases versus healthy children. Heart Br Card Soc. 2018;104(12):1026–36.
Burden SJ, Weedon BD, Turner A, Whaymand L, Meaney A, Dawes H, et al. Intensity and duration of physical activity and cardiorespiratory fitness. Pediatrics. 2022;150(1):e2021056003. https://doi.org/10.1542/peds.2021-056003. (Cited 2024 Mar 7).
Kuhn M, Kohlbrenner D, Sievi NA, Clarenbach CF. Increasing daily physical activity and its effects on QTc time in severe to very severe COPD: a secondary analysis of a randomised controlled trial. COPD J Chronic Obstr Pulm Dis. 2022;19(1):339–44. https://doi.org/10.1080/15412555.2022.2101992. (Cited 2024 Jun 13).
Acknowledgements
Authors are grateful to Ms. Chloe Roz, Christelle Sarran, Cloelia Boyer, Claire Sentourens, Doriane Trinquaz, Ines Juana, Thea Alary for their organizational support. The authors acknowledge the efforts of all participating patients and their parents during the program.
Funding
This study belongs to the QUALIMYORYTHM research project, dedicated to evaluating and improving the quality of life of children with inherited cardiac disorders and funded by the French Department of Health (DGOS-GIRCI-SOHO-APITHEM, www.girci-soho.fr), the French Federation of Cardiology (FFC Research Team Grant, www.fedecardio.org), and the French National Rare Cardiac Disease Network (CARDIOGEN grant, www.filiere-cardiogen.fr). Additional research funding was obtained from the Montpellier University Hospital, France (Young Researcher Award, Master’s scholarship, O.W.), the University of Montpellier, France (Doctoral fellowship, L.S.), and the Saint-Pierre Foundation (https://www.fondationsaintpierre.org/).
Author information
Authors and Affiliations
Contributions
L.S. and P.A. conceptualised and designed the study, drafted the initial manuscript, and reviewed and revised the manuscript. D.M., J-L.P., S.G, M.V, G.D.L.V, and A.A. refined the rehabilitation program during preparation meetings and reviewed the manuscript. A.R. performed CPET assessments and participated in patient screening. P.A., S.G, M.V, G.D.L.V, and J-L.P. enrolled patients. P.A. directed the study. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Informed consent was obtained from all parents or legal guardians, and oral assent was obtained from all children. This study was conducted in compliance with the Good Clinical Practice protocol and the principles of the Declaration of Helsinki. This study was approved by the Institutional Review Board of Montpellier University Hospital (IRB-MTP_2023_05_202301410) and registered at Clinicaltrials.gov (NCT05964322).
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
13102_2024_941_MOESM1_ESM.docx
Additional file 1. The CONSORT Checklist for a pilot study, CONSORT Checklist of information to include when reporting a pilot of a feasibility trial.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Souilla, L., Guillaumont, S., Auer, A. et al. Cardiac rehabilitation in children and adolescents with long QT syndrome: the RYTHMO’FIT pilot study. BMC Sports Sci Med Rehabil 16, 152 (2024). https://doi.org/10.1186/s13102-024-00941-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-024-00941-2