Abstract
Background
To assess physical activity (PA) there is a need of objective, valid and reliable measurement methods like accelerometers. Before these devices can be used for research, they need to be calibrated and validated for specific age groups as the locomotion differs between children and adults, for instance. Therefore, the aim of the present study was the calibration and validation of the Move4 accelerometer for children aged 8–13 years.
Methods
53 normal weighted children (52% boys, 48%girls) aged 8–13 years (mean age = 10.69 ± 1.46, mean BMI = 17.93 kg/m− 2, 60th percentile), wore the Move4 sensor at four different body positions (thigh, hip, wrist and the Move4ecg including heart rate measurement at the chest). They completed nine activities that considered the four activity levels (sedentary behavior (SB), light PA (LPA), moderate PA (MPA) and vigorous PA (VPA)) within a test-retest design. Intensity values were determined using the mean amplitude deviation (MAD) as well as the movement acceleration intensity (MAI) metrics. Determination of activities and energy expenditure was validated using heart rate. After that, cut-off points were determined in Matlab by using the Classification and Regression Trees (CART) method. The agreement for the cut-off points between T1 and T2 was analyzed.
Results
MAD and MAI accelerometer values were lowest when children were lying on the floor and highest when running or doing jumping jacks. The mean correlation coefficient between acceleration values and heart rate was 0.595 (p = 0.01) for MAD metric and 0.611 (p = 0.01) for MAI metric, indicating strong correlations. Further, the MAD cut-off points for SB-LPA are 52.9 mg (hip), 62.4 mg (thigh), 86.4 mg (wrist) and 45.9 mg (chest), for LPA-MPA they are 173.3 mg (hip), 260.7 mg (thigh), 194.4 mg (wrist) and 155.7 mg (chest) and for MPA-VPA the cut-off points are 543.6 mg (hip), 674.5 mg (thigh), 623.4 mg (wrist) and 545.5 mg (chest). Test-retest comparison indicated good values (mean differences = 9.8%).
Conclusion
This is the first study investigating cut-off points for children for four different sensor positions using raw accelerometer metrics (MAD/MAI). Sensitivity and specificity revealed good values for all positions. Nevertheless, depending on the sensor position, metric values differ according to the different involvement of the body in various activities. Thus, the sensor position should be carefully chosen depending on the research question of the study.
Similar content being viewed by others
Background
The assessment of physical activity (PA) and sedentary behavior (SB) in children has gained more and more attention in recent years, as obesity and other health risks are increasingly occurring in childhood [1]. As regular PA is beneficial for the health status [2,3,4,5,6] as well as social and cognitive development in children [7], valid, reliable and feasible measurement options are essential for research examining activity behavior [8]. Activity monitoring typically is divided into two categories: subjective and objective measurement methods [9,10,11,12,13]. Valid subjective measures like surveys, activity diaries or interviews are inexpensive and therefore they are often used to assess PA behaviors in large groups of individuals [14]. Nevertheless, they often have low accuracy and depend on children’s or their parents’ recall bias [15,16,17].
In contrast, technical measurement methods, such as calorimetry, doubly labeled water, pedometers and accelerometry [9, 18, 19], allow for an objective and non-invasive assessment of PA, place less burden on study participants, and are of particular importance for younger children who show difficulties to recall or estimate their past PA, and whose intermittent activity patterns make proxy reports very difficult [20, 21].
Far less expensive and complicated than calorimetry and double labeled water are accelerometers and pedometers [8]. In addition, they eliminate recall bias and social desirability [22, 23]. These methods are commonly used for objective assessment of PA [14, 24]. Pedometers typically contain a mechanical sensor that, when moving up and down, records that movement as a step [24,25,26,27]. In contrast to pedometers, accelerometers can measure movement acceleration in multiple planes. This makes it possible to quantify the intensity, frequency and duration of an activity and not just the number of steps taken [13, 28,29,30,31]. Furthermore, accelerometers can be worn on different body positions such as hip, wrist, chest or thigh. The common use are hip worn accelerometers, that reveal accurate classification of activity type and correct classification of PA intensities [32, 33]. Nevertheless, there are advantages of wearing accelerometers on other body locations such as improved comfort [33]. In addition, measurement accuracy and compliance has consistently improved during the last years [33,34,35]. In particular, wrist accelerometers were more often used in recent studies as it has been shown to reach superior compliance in children compared to hip placement [36]. Additionally, studies with accelerometers worn on the wrist or thigh revealed that they detected more specific activities and yielded acceptably accurate assessment of energy expenditure and SB [33, 37, 38]. Due to its advantages, accelerometers are commonly used to quantify PA in adults, adolescents, and children.
For any given accelerometer, thresholds need to be developed using a calibration and validation study. So far, there exist various calibration studies concerning different age groups in children and adolescents like toddlers, elementary school children and adolescents by implementing various approaches [21, 22, 39, 40]. Nevertheless, current accelerometer studies used different accelerometers. Furthermore, these studies mostly used regression models to compute the energy expenditure from the captured raw data [41, 42]. However, to predict regression models, a reference method like indirect calorimetry is necessary. Nevertheless, this method is quite expensive as well as time-consuming. Further, calorimetry is a laboratory-study and is not useful in free living conditions and practicable for children [20, 43, 44].
The accelerometer Move4 (movisens GmbH) used in the present study has already been extensively validated and tested for adults in this way [45, 46]. Nevertheless, children’s PA patterns and the resulting energy expenditure differ from adults and thus, separate cut-off points for PA intensities are need. Further, two different metrics exist that give the best possible indication of the intensity of physical movements and determine cut-off points for them for classification into activity levels. Thus, the research question of the present study is the calibration of the Move4 accelerometer for children aged 8–13 years. Specifically, we defined the following three aims:
Objective 1: Validation of the selected activities for the activity levels by using heart rate.
Objective 2: Modelling and determination of cut-off points to distinguish different activity levels (SB, light PA (LPA), moderate PA (MPA), vigorous PA (VPA)).
-
a.
by using different metrics (see study description): mean amplitude deviation (MAD) [47] and movement acceleration intensity (MAI) [48].
-
b.
by differing between the four sensor positions for mapping individual movement activities representation of cut-off points per movement activity per position.
Objective 3: Determination of the test-retest agreement by using data from two survey time points to determine the test-retest reliability of the Move4 together with the respective metrics.
Materials and methods
Study design
The longitudinal study is part of the EMPADIC (Examination of methods for recording physical activity and its determinants in children aged 8–13 years) – project. The study was approved by the local Ethics Committee (Ref. No. 56_20B) and was in accordance with the 1964 Declaration of Helsinki. All participants and their legal guardians provided written informed consent for the study participation. Data collection took place from May to September 2022.
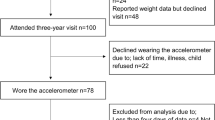
Participants and procedure
For the present study, we included children aged 8–13 years. Recruitment took place in local sports clubs and schools in Bavaria (Germany). All participants were included if they were healthy and had no known diseases that restrict them from doing sport. In school, all children were excluded who are exempt from sports lessons due to health restrictions or who are unable to participate in physical education lessons. After written informed consent of the board of directors of the sports clubs and the school director, we contacted various divisions in the sports club as well as teachers and asked, whether they would like to participate in our study. Then, parents as well as children obtained an information document and both had to give written informed consent for study participation.
For data collection, we used a test-retest design, to assess the validity of the cut-off points and the agreement between cut-off points between T1 and T1. There was a timespan of one week between the two measurement points. Data collection was pseudonymous, so at the beginning each participant received a personal code consisting of a combination of letters and numbers. Furthermore, for each child, weight and height, which was measured by a stadiometer (seca 813 and seca 213, seca GmbH & Co. KG), as well as the age, were documented. The children’s fitness status was recorded via the question “How many hours of exercise do you do per week?“ (see Supplement 1).
For the calibration of the Move4 for children, participants performed nine different activities outdoors under the guidance of the trained research team like lying, sitting, standing, running with different pace, stairs climbing, catching, and throwing a ball as well as jumping jacks. These activities consider four intensity levels: SB, LPA, MPA, and VPA. Table 1 lists the performed activities and the expected MET values. Data collection took place in a 90-minute training session (60 min test, 30 min of preparation and follow-up). Before the start of the test, the children’s verbal consent was obtained again. The sensors were applied to the children by the research team. For the present study, the children wore accelerometers at the following body positions: thigh (Move4); hip (Move4); wrist/ non-dominant hand (Move4) and chest (combination with ECG) (EcgMove4). When all sensors were properly attached, a jump was made to synchronize the sensors at each body position before the activities started. Such a jump was repeated after the activities have been performed. Subsequently, the children were instructed by the research team to perform each activity for a duration of four minutes. Average speeds for walking and running activities were estimated using defined distance and stopwatch. Further, a member of the research team guided the children through all activities and set the pace for the children for walking/running activities. This made it easier for the participants to maintain the estimated speed. During the implementation, the research team observed the participants and checked the correct performance of the activities. Between the four minutes activity there was a three-minute break to allow for transition between activities. After each activity children were instructed to stand still for 30 s to enable a separation of the activities. After completion of the nine activities the sensors were removed from the participants. Even if the rest between the activities was three minutes, we assume that the heart rate does not reach the resting heart rate after moderate and high intensity activities. As this could artefact the validation of the activities, we randomized the order of the activities for each data collection timepoint/study group.
Measurement instrument
The movisens sensor Move4 is a wearable device for measuring PA and sleep. The sensor EcgMove4 additionally records a single channel ECG and can be used to derive heart rate and heart rate variability. Both sensors have a 3-axis accelerometer and a 3-axis gyroscope for accurate detection of movements and body postures.
The sensor data is stored on an internal flash memory and can later be analyzed using the movisens Data Analyzer software [51, 52]. This software provides various analysis methods and visualization options to interpret the data and gain insights into PA, sleep and heart rate variability. Output parameters such as activity classes, body position, steps, energy expenditure and metabolic equivalents can be calculated.
The sensors are suited for use in scientific studies and interactive ambulatory assessment. They are used in a variety of applications, including sports performance analysis and rehabilitation [53,54,55,56].
The device is compact and lightweight, allowing for convenient and continuous use, and can be connected to a smartphone or other device for data transfer and analysis, e.g. to trigger questionnaires based on sensor data.
Data analysis
Descriptive statistics were calculated for study variables, mean (M) and standard deviations (SD) for continuous variables and frequency (%) for categorical variables. We conducted a test for normal distribution (Kolmogorov-Smirnov and Shapiro-Wilk) for all continuous variables. The data analysis of the accelerometer data was divided into two major steps: data preparation and data processing. During data preparation, Matlab version 2015b (TheMathWorks, Inc.) was first used to trim the sensor data to the measurements of each child. The sequence of activities was then read in so that the individual activities and the breaks in between could be marked in the sensor data. This reference annotation was used to assign the calculated PA values to the respective activity.
If there was an error in data acquisition for example an interruption of the activities during the measurement, for example because a child had to go to the toilet, a note was added accordingly. In line with the annotations, these sections were marked in the respective measurement and excluded from further processing. Relevant parameters were also added for further processing. These included gender, age, heart rate and the measurement time point in order to better compare the two time points. The data was processed using Matlab (TheMathWorks, Inc.) and the movisens software [51, 52]. Thereby, the PA metric values for the MAD [47] and MAI (based on Van Someren et al. [48]) metrics were determined using the movisens DataAnalyzer algorithms. For MAI, the acceleration signal was bandpass filtered (Butterworth 0.25-11 Hz, 4th order) to remove parts that are not caused by bodily movement. The three axes were fused by the Euclidean norm. The final signal output was the mean value of the output interval. Movisens uses an output interval of one minute [57]. In the literature, the MAD metric is also called Vector Magnitude Count (VMC) and makes use of the mean signal value to reduce the effect of the constant gravitational acceleration [58].
To confirm the validity of pattern-based classification of intensity, Pearson correlation coefficients were calculated between the heart rates and MAD/MAI acceleration values. In addition, Matlab was used to create boxplots representing the heart rates across activities.
Subsequently, these metric values were used to determine the cut-off points for the four different activity levels in Matlab by a decision tree using the Classification and Regression Trees (CART) method [59]. This method is based on the recursive partitioning technique and creates decision trees by recursively partitioning the data until a predefined stopping criterion (maximum depth) is reached. The goal of the CART method is to minimize the variance in the data while maximizing the information in the data.
We determined the cut-off points for the different intensity levels for each sensor position and for both measurement time points. Finally, we analyzed the sensitivity and specificity of our analysis by using one minute of each activity as a reference value.
Results
Socio-demographics
In the study participated 53 children (52% boys, 48%girls) aged 8–13 years (mean age = 10.69 ± 1.46). Overall, participants had a mean Body Mass Index (BMI) of 17.93 kg*m− 2 (SD = 2.89) ranging around the 60th percentile [60] and regularly engaged in sports for 61.26 (± 26.16) minutes per day indicating overall a good fitness-level of the children. However, as seen in the standard deviation, children varied in their amount of sports activity per day. Test of distribution of the variables indicated a normal distribution of height, all other variables (age, weight, weight status, and sports activity) were not normal distributed. Further details can be seen in Table 2.
Mean values of each activity
Table 3 shows the accelerometer values for each activity broken down for MAI and MAD metrics. Overall, MAI values were higher than MAD. Mean accelerometer values were lowest when children were lying on the floor and highest when running or doing jumping jacks with no differences between boys and girls. The accelerations in each metric increase from intensity level to intensity level with the highest values for VPA.
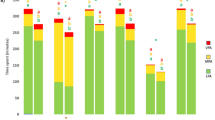
Criterion Validity
Based on the individual mean values of each activity (MAD and MAI in mg), the criterion validity was then measured by correlation between the values of the MAD/MAI metric for each activity and the heart frequency (Ecg Move4). Overall, we had no limit of heart rate and thus no termination criteria. The mean heart rate for the SB activities was 105 beats (SD = 23) per minute (bpm), 115 bpm (SD = 18) for LPA, 132 bpm (SD = 20) for MPA and highest value for VPA with 152 bpm (SD = 21). The mean correlation coefficient between acceleration values and heart rate was 0.595 (p = 0.01) for MAD metric and 0.611 (p = 0.01) for MAI metric and thus, indicated a strong correlation between these the variables [61]. Figure 1 presents each activity with the associated heart rate.
Cut-off points of intensity levels/thresholds
The nine activities considered four intensity levels (see Table 4) and validity showed a strong correlation between activities and heart rate and thus, cut-off points for SB-LPA, LPA-MPA as well as MPA-VPA could be determined. Table 4 shows the three cut-off points for the MAD and MAI metric for all four sensor positions. Overall, there were no meaningful differences in the cut-off points between boys and girls. Thus, we mention the overall cut-off points.
Overall, cut-off points differ between the two metrics with higher values for MAI across all sensor positions (see Table 4). In particular, the MAD values of the hip sensor are for SED (0-52.9 mg), LPA (53-173.3 mg), MPA (173.4-543.6 mg), VPA (> 543.6 mg).
Sensitivity and specificity
Sensitivity and specificity for classification of each PA intensity category within the MAD metrics are displayed in Table 5. For SB, the wrist worn accelerometer had highest sensitivity (98.9%), but the hip worn has highest specificity (99.1%). For LPA, MPA and VPA, sensitivity (92.0%) as well as specificity (70.8%) were highest for the chest worn accelerometer. Overall, the chest position indicated the highest sensitivity (91.1%) and specificity (82.1%) values across all intensity levels for the MAD metrics.
Sensitivity and specificity for classification of each PA intensity category within the MAI metrics are displayed in Table 6. For SB, the thigh worn accelerometer had highest sensitivity (98.2%), whereas specificity (99.7%) was highest for the chest worn accelerometer. For LPA, the thigh position indicated the highest sensitivity (93.9%) but the chest worn the highest specificity (73.6%). For MPA, sensitivity (76.8%) as well as specificity (60.1%) were highest for the chest worn accelerometer. Sensitivity (99.5%) for VPA was highest at the chest position and specificity (98.5%) at the wrist position. Overall, the hip position indicated the highest sensitivity (88.8%) and the chest position the highest specificity (81.7%) values across all intensity levels for the MAI metrics.
Test-retest agreement
As our study had a test-retest design, we compared the determined cut-off points for the intensity levels for all accelerometer positions between T1 and T2. Overall, for the MAD metric, the mean difference between T1 and T2 was 9.85% with greatest differences for the wrist worn accelerometer (16.3%) and lowest difference for the chest worn (6.4%). Independently of the accelerometer position, the highest deviation was seen for the SB-LPA cut and the LPA-MPA cut (see Table 7).
Similar results can be seen for the MAI metrics (see Table 7). Overall, the mean value of deviation between T1 and T2 was 8.63% with greatest differences for the wrist worn accelerometer (14.0%) and lowest difference for the chest worn (5.6%). Independently of the accelerometer position, the highest deviation was seen for the SB-LPA cut and the cut-off points for LPA-MPA and MPA-VPA had equal differences across all positions.
Discussion
The aim of the present study was the calibration of the Move4 accelerometer for children aged 8–13 years. In more detail, firstly mean values for the selected activities (in mg for MAD and MAI metric) were assessed and then these activities and the energy expenditure were validated by using the heart rate. Secondly, cut-off points were modelled and determined to distinguish different intensity levels by using two different metrics (MAD and MAI) as well as by differentiating between the four sensor positions.
Validity
First of all, the determination of activities and energy expenditure level was validated by using the heart rate measures. Overall, a strong correlation between the heart rate and the MAD values (in mg) of each activity was found. With increasing MET values, the heart rate of the activities increased. Based on this finding, it is possible to determine the cut-off points by using the MAD/MAI values of the activities. The present results are consistent with previous reports stating that heart rate is effective in detecting a variety of activity patterns [40]. Nevertheless, as we randomized the order of the activities, it was possible, that in some groups SB activities followed right after VPA activities. In that case, the three minutes rest could not have been enough time to normalize the heart rate. This could explain slightly higher heart rates of 105 bpm for SB compared to physiological studies indicating a resting heart rate of 90–95 bpm in this age range [62, 63]. In this context, it is worth mentioning that the validation of the activities was based on children with an overall good fitness level (mean activity minutes per day = 61.2) and a normal weight (overall BMI = 17.9 kg/m− 2, 60th percentile). Nevertheless, there were differences in the amount of activity and weight status between the children (see Table 2), resulting in differences in the HR while performing the activities [64]. This needs to be considered when interpreting the data. Still, as the mean value is quite good, we assume that the determined cut-off points can be used for children with a normal weight status and fitness level.
Selection of activities
In this context, the selection of the activities for the present calibration study should be discussed. First of all, a combination of locomotor activities (e.g., slow walking with 2 km/h) and other free-play activities (e.g., throwing and catching a ball) was used to better simulate the different types of activities that children engage in. These were common to children of this age group and provided both, varying intensity levels and ranges of accelerometer counts [22]. This is also a principle suggested by Welk [65] and was used in several studies so far [66,67,68,69]. Furthermore, nine activities were used which is also applied in other studies [40, 41, 65, 68, 70]. The selection and classification of the used activities is based on the Youth Compendium of Physical Activity [50]. Unfortunately, only one activity (slow walking) was selected for LPA. Thus, it is suggested that further studies should apply an equal number of activities for each of the four PA intensity levels.
Cut-off points
There is a need for using raw acceleration data instead of activity counts for measuring the intensity of PA [71,72,73]. Thus, the present study compared two different raw acceleration metrics (MAD and MAI) for the calibration of the Move4 sensor across four sensor positions in children aged 8–13 years. Within the discussion, further focus will set on the results of the MAD metrics, because, to the best of our knowledge, there is no validation and calibration study using the MAI metric so far. Nevertheless, this metric is also important as it uses a bandpass filter that ensures that accelerations that do not come from physical movements tend to be filtered out and is more and more used in studies [74, 75], so it was decided to determine the cut-off points for both MAD and MAI metrics. In comparison to Aittasalo et al. [70] who used the MAD metric for a hip worn accelerometer in children aged 13–15 years, our cut-off points differ especially in Cut 1 (SB-LPA: 52.9 vs. 26.9 mg;) and Cut 2 (LPA-MPA: 173.3 vs. 332 mg). One reason for the difference in the lower values in our study for LPA-MPA cut-off points might be the allocation of the activities to the intensities: In the present study, slow walking was the only activity for LPA and normal walking for MPA (oriented to the Youth Compendium of Physical Activity [50]), whereas Aittasalo et al. [70] allocated slow walking as well as normal walking to LPA. Another study using the MAD metric in 11 year old children indicated as the optimal cut-off points for LPA-MPA (= 3 MET) 91 mg and the MPA-VPA (= 6 MET) cut-off points was at 414 mg [47]. However, in this study participants performed a pace-conducted non-stop test on a 200 m long oval indoor track with initial speed of 0.6 m/s and it was increased by 0.4 m/s at every 2.5 min [47]. As free-living activities were also included, this could be the reason for the differences in the cut-off point from LPA to MPA (173.3 vs. 91 mg). In summary, our data show that the values respectively the cut-off points differ between the studies. This could be due to different samples, different activities and therefore it is important that for each sensor cut-off points are formed to make them usable for studies.
Sensor positions
To the best of our knowledge, this was the first study comparing four sensor positions of any accelerometer. Existing studies compared in particular hip and wrist worn accelerometer [41] or hip, wrist and thigh [68], but none compared the hip, thigh, wrist and chest position for sensor location. As the different body positions are involved differently in the nine activities, it is not surprisingly that the cut-off points differ slightly across the four sensor positions.
Regarding sensitivity and specificity of each sensor position, our results indicated overall for the hip as well as for the thigh the highest specificity (MAD hip: 88.8%; MAD chest: 82.1%) as well as sensitivity (MAD hip: 89.3%; MAD chest: 91.1%) whereas the sensitivity and specificity for the wrist indicated in MAD metrics 85.2% respectively 81.3%. In contrast, Johansson et al. [41] indicated for wrist and hip worn sensors same sensitivity (SB: 100%, MVPA: 70%) and specificity (SB: 60%, MVPA: 100%) values in preschool children. Sensitivity and specificity values for two hip worn accelerometers indicated in children aged 13–15 years almost perfect values for all cut-off values (98.6-100%) [70]. The different values of sensitivity and specificity in various studies could be explained by the selection of the activities. Depending on how far the MET values of the activities are from the MET-cutpoint (e.g., 3 MET), there are different metric cut-off points and different accuracies in the detection. In comparison, a study investigating adults found high accuracy of the thigh-worn accelerometer for predicting time spent in each PA intensity category, as seen by sensitivities and specificities > 99% for correctly classifying each PA intensity category [68]. One possible explanation for the differences between children and adults could be the inconsistent performance of activities in children whereas adults could more consequently perform activities over a certain time period [76].
Furthermore, regarding the accelerometer output (in mg) within one intensity level, there are differences according to the body position to which the sensor is attached. In particular, the MAD metrics for SB varied widely in our study: 52.9 mg for the hip placement, 62.4 mg for thigh, 86.4 mg for the wrist sensor and 45.9 mg for the chest position. The high values of wrist worn accelerometers in SB could be explained by the fact that this sensor position captures movements performed by the arms, unlike a hip worn monitor [41]. Especially younger children have problems to stand still without moving their arms [41]. Our findings are in accordance with results from other studies [36, 41, 77] which showed higher values for wrist-worn accelerometer compared with hip worn sensors, while measuring simultaneously.
Recommendations for sensor positions
We suggest to choose the sensor position depending on the research question. Overall, the sensor at the hip is really comfortable and shows good values and is already commonly used [32, 33, 78, 79]. Furthermore, the hip worn sensor indicated good sensitivity and specificity values in our study. Nevertheless other body positions should be considered while planning a study [68]. In particular, accelerometers worn on the thigh have shown high accuracy for measuring several different PA levels as well as SB and sleep [33, 38, 80,81,82,83,84]. Further, if there is an interest in the heart rate of the participants, the EcgMove4 accelerometer worn at the chest is suggested. Thus, it is easy to assess time spent in different intensity levels as well as the heart rate. The least favorable and efficient position seems to be the wrist due to low sensitivity and specificity.
Test-retest agreement
Lastly, to assess the accuracy of the Move4 sensor, a test-retest design for the agreement of the cut-off points between T1 and T2 for all sensor positions was used. Overall, agreement indicated good values with small differences between T1 and T2. Regarding the cuts, Cut 1 and 2 indicated higher deviations compared to Cut 3. This could be explained by the types of activities within one PA level allowing greater variations in the execution. Especially during the SB activities (standing and lying), some children problems to hold the position and not to move their bodies, especially their arms. In contrast, VPA activities required the whole body to move which allows less variations in execution.
Regarding the sensor positions, only the wrist worn accelerometer showed great differences especially for SB-LPA and LPA-MPA cut-off points. A problem is that the wrist worn accelerometer output is highly depending on the movements of the hands [41]. In particular, the task standing for four minutes was highly challenging for some children and variances were recognized between the children (inter-individual) and also between the two measurement points (intra-individual) in relation to the movement of the hands. This could explain the differences of 16.3% between T1 and T2 cut-off points.
Strengths and limitations
The main strength of our study is our sample size of 53 children aged 8–13 years which was numerous compared to other studies investigating between 20 and 47 participants [21, 41, 47, 70]. Furthermore, we calibrated and tested the Move4 sensor at four different body positions (hip, thigh, non-dominant wrist, and chest). Thus, the validation of the sensors was successful regarding a wide range of application possibilities. In addition, the different activities were not selected randomly, rather following the Youth Compendium of Physical Activity. Butte et al. [50] developed various activities and their resulting energy consumption in MET values. This is a meaningful list of activities and is a valuable resource. Furthermore, to ensure that the activities are performed with high accuracy, one research assistant was leading and participating in the exercise. This was highly important for the walking and running activities to lead the pace.
A limitation of this study relates to different weather conditions during the time period of the data collection. Therefore, some of the exercises were carried out indoors, which may have affected the children’s movement. Secondly, the sensors have partially fallen off during the movements. Although they were immediately reattached, a few seconds of activity had to be cut out. Further, some participants had difficulties to perform the activity the whole duration of four minutes. Thus, the data preparation contains cut outs to clean the raw data. Besides performing for four minutes, the accuracy of the execution lacked (e.g., standing). In this context, the validation of the activities and thus the determination of the cut-off points need to be slightly limited as the sample differed within the amount of activity (fitness level) and weight status, which might result in variability of the heart rate within one activity. Lastly, we only had one activity for the LPA intensity level that could be not representative for this level. Nevertheless, our data show good validity of the activities and the MET values. Further studies should consider that all intensity levels include more than one activity.
Conclusion
This is the first calibration study using two different metrics (MAD/MAI) based on raw accelerometer data as well as determining cut-off points for four sensor positions using movisens Move4 sensor. Overall, our validation of the activities in regard to MET values by heart rate shows good correlation. Thus, the cut-off points showed good values for sensitivity and specificity. Test-retest agreement indicated good values with slightly more deviation from T1 to T2 in the wrist worn accelerometer. The optimal sensor position should be chosen depending on the research question of the study. Further calibration studies are needed for younger children, especially preschool children, as their activity patterns differ from children included in our study.
Data availability
The datasets generated during and/or analysed during the current study are available from the corresponding author on reasonable request.
References
Guthold R, et al. Global trends in insufficient physical activity among adolescents: a pooled analysis of 298 population-based surveys with 1·6 million participants. The Lancet Child & Adolescent Health. 2020;4(1):23–35.
Ekelund U, et al. Moderate to vigorous physical activity and sedentary time and cardiometabolic risk factors in children and adolescents. JAMA. 2012;307(7):704–12.
Poitras VJ, et al. Systematic review of the relationships between objectively measured physical activity and health indicators in school-aged children and youth. Appl Physiol Nutr Metab. 2016;41(6):S197–S239.
Rodriguez-Ayllon M, et al. Role of physical activity and sedentary behavior in the Mental Health of Preschoolers, children and adolescents: a systematic review and Meta-analysis. Sports Med. 2019;49(9):1383–410.
Biddle SJH, et al. Physical activity and mental health in children and adolescents: an updated review of reviews and an analysis of causality. Psychol Sport Exerc. 2019;42:146–55.
Chinapaw M, et al. Total volume versus bouts: prospective relationship of physical activity and sedentary time with cardiometabolic risk in children. Int J Obes (Lond). 2018;42(10):1733–42.
Zeng N et al. Effects of Physical Activity on Motor Skills and Cognitive Development in Early Childhood: A Systematic Review Biomed Res Int, 2017. 2017: p. 2760716.
Barkley JE, et al. The validity of the commercially-available, low-cost, wrist-worn Movband accelerometer during treadmill exercise and free-living physical activity. J Sports Sci. 2019;37(7):735–40.
Hills AP, Mokhtar N, Byrne NM. Assessment of physical activity and energy expenditure: an overview of objective measures. Front Nutr. 2014;1:5–5.
Sirard JR, Pate RR. Physical activity assessment in children and adolescents. Sports Med. 2001;31(6):439–54.
Yang Y, et al. Reliability and validity of a new accelerometer-based device for detecting physical activities and energy expenditure. PeerJ. 2018;6:e5775.
Bassett D. Validity and Reliability issues in Objective Monitoring of Physical Activity. 2015.
Ridgers N, Fairclough S. Assessing free-living physical activity using accelerometry: practical issues for researches and practitioners. Eur J Sport Sci - EUR J SPORT SCI. 2011;11:205–13.
Burchartz A, et al. Comparison of self-reported & device-based, measured physical activity among children in Germany. BMC Public Health. 2021;21(1):1081.
Prince SA, et al. A comparison of direct versus self-report measures for assessing physical activity in adults: a systematic review. Int J Behav Nutr Phys Activity. 2008;5(1):56.
Corder K, et al. Assessment of physical activity in youth. J Appl Physiol (1985). 2008;105(3):977–87.
Dowd KP et al. A systematic literature review of reviews on techniques for physical activity measurement in adults: a DEDIPAC study. Int J Behav Nutr Phys Activity, 2018. 15.
Holbrook EA, Barreira TV, Kang M. Validity and reliability of Omron pedometers for prescribed and self-paced walking. Med Sci Sports Exerc. 2009;41(3):670–4.
Trost SG, McIver KL, Pate RR. Conducting accelerometer-based activity assessments in field-based research. Volume 37. Medicine & Science in Sports & Exercise; 2005. pp. S531–43. 11.
Hager ER, et al. Toddler physical activity study: laboratory and community studies to evaluate accelerometer validity and correlates. BMC Public Health. 2016;16:936.
Van Cauwenberghe E, et al. Feasibility and validity of accelerometer measurements to assess physical activity in toddlers. Int J Behav Nutr Phys Act. 2011;8:67.
Evenson KR, et al. Calibration of two objective measures of physical activity for children. J Sports Sci. 2008;26(14):1557–65.
Pulsford RM, et al. Actigraph Accelerometer-defined boundaries for sedentary Behaviour and Physical Activity intensities in 7 Year Old Children. PLoS ONE. 2011;6(8):e21822.
Clemes SA, et al. Evaluation of a commercially available pedometer used to promote physical activity as part of a national programme. Br J Sports Med. 2010;44(16):1178–83.
Schneider PL, Crouter S, Bassett DR. Pedometer measures of free-living physical activity: comparison of 13 models. Med Sci Sports Exerc. 2004;36(2):331–5.
Bassett DR Jr., et al. Pedometer-measured physical activity and health behaviors in U.S. adults. Med Sci Sports Exerc. 2010;42(10):1819–25.
Park W, et al. Effect of walking speed and placement position interactions in determining the accuracy of various newer pedometers. J Exerc Sci Fit. 2014;12(1):31–7.
Pate RR, O’Neill JR, Mitchell J. Measurement of physical activity in preschool children. Med Sci Sports Exerc. 2010;42(3):508–12.
Reilly JJ, et al. Objective measurement of physical activity and sedentary behaviour: review with new data. Arch Dis Child. 2008;93(7):614–9.
Sirard JR, Slater ME. Compliance with wearing physical activity accelerometers in high school students. J Phys Act Health. 2009;6(Suppl 1):S148–55.
Strath SJ, et al. Guide to the assessment of physical activity: clinical and research applications: a scientific statement from the American Heart Association. Circulation. 2013;128(20):2259–79.
Lyden K, et al. A method to estimate free-living active and sedentary behavior from an accelerometer. Med Sci Sports Exerc. 2014;46(2):386–97.
Montoye AH, et al. Energy Expenditure Prediction using raw Accelerometer data in simulated free living. Med Sci Sports Exerc. 2015;47(8):1735–46.
Preece SJ, et al. Activity identification using body-mounted sensors–a review of classification techniques. Physiol Meas. 2009;30(4):R1–33.
Attal F, et al. Physical human activity Recognition using Wearable sensors. Sensors. 2015;15(12):31314–38.
Fairclough SJ, et al. Wear compliance and activity in children wearing wrist- and hip-mounted accelerometers. Med Sci Sports Exerc. 2016;48(2):245–53.
Rowlands AV, et al. Assessing sedentary behavior with the GENEActiv: introducing the sedentary sphere. Med Sci Sports Exerc. 2014;46(6):1235–47.
Steeves JA, et al. Ability of thigh-worn ActiGraph and activPAL monitors to classify posture and motion. Med Sci Sports Exerc. 2015;47(5):952–9.
Ekblom O, et al. Validity and comparability of a wrist-worn accelerometer in children. J Phys Activity Health. 2012;9(3):389–93.
Sun DX, Schmidt G, Teo-Koh SM. Validation of the RT3 accelerometer for measuring physical activity of children in simulated free-living conditions. Pediatr Exerc Sci. 2008;20(2):181–97.
Johansson E, et al. Calibration and validation of a wrist- and hip-worn Actigraph Accelerometer in 4-Year-old children. PLoS ONE. 2016;11(9):e0162436.
Crouter SE, et al. Refined two-regression model for the ActiGraph Accelerometer. Med Sci Sports Exerc. 2010;42(5):1029–37.
Welk GJ, Corbin CB, Dale D. Measurement issues in the assessment of physical activity in children. Res Q Exerc Sport. 2000;71(2 Suppl):S59–73.
Adamo KB, et al. A comparison of indirect versus direct measures for assessing physical activity in the pediatric population: a systematic review. Int J Pediatr Obes. 2009;4(1):2–27.
Härtel S, et al. Estimation of energy expenditure using accelerometers and activity-based energy models—validation of a new device. Eur Rev Aging Phys Activity. 2011;8(2):109–14.
Anastasopoulou P, et al. Validation and comparison of two methods to assess Human Energy expenditure during free-living activities. PLoS ONE. 2014;9(2):e90606.
Vähä-Ypyä H, et al. Validation of cut-points for evaluating the intensity of physical activity with Accelerometry-Based Mean Amplitude deviation (MAD). PLoS ONE. 2015;10(8):e0134813.
Van Someren EJW, et al. Gravitational artefact in frequency spectra of movement acceleration: implications for actigraphy in young and elderly subjects. J Neurosci Methods. 1996;65(1):55–62.
Trost SG, et al. Comparison of accelerometer cut points for predicting activity intensity in youth. Med Sci Sports Exerc. 2011;43(7):1360–8.
Butte NF, et al. A Youth Compendium of Physical activities: Activity codes and metabolic intensities. Med Sci Sports Exerc. 2018;50(2):246–56.
movisens. DataAnalyzer - Sensor-Daten Analyse. 2023; Available from: https://docs.movisens.com/DataAnalyzer/.
movisens. DataAnalyzer. 2023; Available from: https://docs.movisens.com/DataAnalyzer/#welcome.
Barouni A, et al. Ambulatory sleep scoring using accelerometers—distinguishing between nonwear and sleep/wake states. PeerJ. 2020;8:e8284.
Ewert C, Hoffmann CFA, Schröder-Abé M. Stress Processing mediates the Link between momentary self-compassion and Affective Well-being. Mindfulness. 2022;13(9):2269–81.
Zhang Y, et al. Digital circadian and sleep health in individual hospital shift workers: a cross sectional telemonitoring study. eBioMedicine. 2022;81:104121.
Diel K, et al. Motivational and emotional effects of social comparison in sports. Psychol Sport Exerc. 2021;57:102048.
Karas M, et al. Accelerometry data in health research: challenges and opportunities. Stat Biosci. 2019;11(2):210–37.
movisens. Mean Amplitude Deviation (PaMetricMeanAmplitudeDeviation). 2023; Available from: https://docs.movisens.com/Algorithms/physical_activity_metrics/#mean-amplitude-deviation-pametricmeanamplitudedeviation.
Mathworks. fitctree. 2023; Available from: https://de.mathworks.com/help/stats/fitctree.html.
Kromeyer-Hauschild K, Moss A, Wabitsch M. Referenzwerte für den Body-Mass-Index für Kinder, Jugendliche und Erwachsene in Deutschland Adipositas - Ursachen, Folgeerkrankungen, Therapie, 2015. 09(03): p. 123–127.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. 2nd edition ed. 1988, Hillsdale, N.J.: L. Erlbaum Associates.
Fernandes RA, et al. Resting heart rate is Associated with blood pressure in male children and adolescents. J Pediatr. 2011;158(4):634–7.
Koskela JK, et al. Association of resting heart rate with cardiovascular function: a cross-sectional study in 522 Finnish subjects. BMC Cardiovasc Disord. 2013;13(1):102.
Silva DAS, de Lima TR, Tremblay MS. Association between Resting Heart Rate and Health-Related Physical Fitness in Brazilian Adolescents Biomed Res Int, 2018. 2018: p. 3812197.
Welk GJ. Principles of design and analyses for the calibration of accelerometry-based activity monitors. Med Sci Sports Exerc. 2005;37(11 Suppl):S501–11.
Puyau MR, et al. Validation and calibration of physical activity monitors in children. Obes Res. 2002;10(3):150–7.
Treuth MS, et al. Defining accelerometer thresholds for activity intensities in adolescent girls. Med Sci Sports Exerc. 2004;36(7):1259–66.
Montoye AHK, et al. Validation and comparison of Accelerometers worn on the hip, thigh, and wrists for measuring physical activity and sedentary behavior. AIMS Public Health. 2016;3(2):298–312.
Heil DP. Predicting activity energy expenditure using the Actical® activity monitor. Res Q Exerc Sport. 2006;77(1):64–80.
Aittasalo M, et al. Mean amplitude deviation calculated from raw acceleration data: a novel method for classifying the intensity of adolescents’ physical activity irrespective of accelerometer brand. BMC Sports Sci Med Rehabil. 2015;7:18.
Cain KL, et al. Using accelerometers in youth physical activity studies: a review of methods. J Phys Act Health. 2013;10(3):437–50.
John D, Freedson P. ActiGraph and Actical physical activity monitors: a peek under the hood. Med Sci Sports Exerc. 2012;44(1 Suppl 1):S86–9.
Troiano RP, et al. Evolution of accelerometer methods for physical activity research. Br J Sports Med. 2014;48(13):1019–23.
Giurgiu M, et al. Sedentary behavior in everyday life relates negatively to mood: an ambulatory assessment study. Scand J Med Sci Sports. 2019;29(9):1340–51.
Kumar D et al. CACHET-CADB: a Contextualized Ambulatory Electrocardiography Arrhythmia dataset. Front Cardiovasc Med, 2022. 9.
Schuck NW, et al. Spontaneous discovery of novel task solutions in children. PLoS ONE. 2022;17(5):e0266253.
Hildebrand M, et al. Age group comparability of raw accelerometer output from wrist- and hip-worn monitors. Med Sci Sports Exerc. 2014;46(9):1816–24.
Lyden K, et al. A comprehensive evaluation of commonly used accelerometer energy expenditure and MET prediction equations. Eur J Appl Physiol. 2011;111(2):187–201.
Staudenmayer J et al. An artificial neural network to estimate physical activity energy expenditure and identify physical activity type from an accelerometer J Appl Physiol (1985), 2009. 107(4): p. 1300-7.
Dong B, et al. Energy-aware activity classification using Wearable Sensor Networks. Proc SPIE Int Soc Opt Eng. 2013;8723:87230y.
Edwardson CL, et al. Considerations when using the activPAL monitor in field-based research with adult populations. J Sport Health Sci. 2017;6(2):162–78.
Kozey-Keadle S, et al. Validation of wearable monitors for assessing sedentary behavior. Med Sci Sports Exerc. 2011;43(8):1561–7.
Lyden K, et al. Validity of two wearable monitors to estimate breaks from sedentary time. Med Sci Sports Exerc. 2012;44(11):2243–52.
Skotte J, et al. Detection of physical activity types using triaxial accelerometers. J Phys Act Health. 2014;11(1):76–84.
Acknowledgements
We would like to thank all institutions (sports club incl. departments and schools) for making the study possible. We would also like to thank all the children who participated in the study.
Funding
Open Access funding enabled and organized by Projekt DEAL. No funding was received for conducting this study.
Open Access funding enabled and organized by Projekt DEAL.
Author information
Authors and Affiliations
Contributions
Conceptualization: F.B., I.M., A.K.R.; Methodology: F.B., I.M., A.K.R.; Formal analysis and investigation: A.E., F.B.; Writing – original draft preparation: F.B.; Writing – review and editing: F.B., I.M., A.E., S.S., C.T. A.K.R.; Supervision: A.K.R.
Corresponding author
Ethics declarations
Ethics approval
The study was approved by the local Ethics Committee of the Friedrich-Alexander-Universität Erlangen-Nürnberg (Ref. No. 56_20B) and was in accordance with the 1964 Declaration of Helsinki.
Consent for publication
Not applicable.
Consent to participate
Informed consent from all participants and their legal guardians for the study participation.
Competing interests
Alina Eisenreich is an employee of the moviens GmbH. Movisens provided the sensors. All other authors declare no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Beck, F., Marzi, I., Eisenreich, A. et al. Determination of cut-off points for the Move4 accelerometer in children aged 8–13 years. BMC Sports Sci Med Rehabil 15, 163 (2023). https://doi.org/10.1186/s13102-023-00775-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-023-00775-4