Abstract
Background
Open-heart surgery is considered one of the primary treatments for severe coronary artery stenosis, but it comes with its own set of complications. However, these complications can be reduced through the implementation of proper cardiac rehabilitation during phase I. This study aimed to examine the impact of phase I cardiac rehabilitation training, using augmented reality, on the self-efficacy of cardiac management in patients undergoing coronary artery bypass grafting.
Methodology
This randomized clinical trial study involved 60 patients who were admitted to the Cardiac Surgery Intensive Care Unit at Ghaem Hospital in Mashhad. The software used in this study consisted of various videos and educational images demonstrating physical exercises for cardiac rehabilitation. The software was developed to train the patients in the intervention group on the rehabilitation program, starting from their admission to the Intensive Care Unit until their discharge from the hospital. The collected data were analyzed using statistical tests such as independent t-test, Mann-Whitney test, paired t-test, chi-square test, as well as descriptive indicators. Cohen’s d was also used to evaluate the magnitude of the effect size.
Results
The findings of this study revealed that the total mean score for cardiovascular management self-efficacy significantly increased during the transfer to the Intensive Care Unit and at the time of discharge. Notably, the increase observed in the intervention group was significantly greater than that of the control group (P < 0.001).
Conclusion
The results of this study indicated that implementing early rehabilitation programs, using innovative educational technology like augmented reality, enhanced the self-efficacy of patients undergoing coronary artery bypass grafting. These findings suggest that such programs can be effectively employed as educational tools throughout different stages of cardiac rehabilitation.
Trial Registration
This study was registered in the Iranian Registry of Clinical Trials (no. IRCT20200203046361N1) on 16/02/2020.
Similar content being viewed by others
Introduction
The prevalence of cardiovascular diseases has grown globally in recent years [1]. Each year, around 3.6 million men and 3.4 million women worldwide pass away due to cardiovascular disease [2]. In developing countries, this illness is the leading cause of death [3], and in Iran, it is the leading cause of death for both men and women [4,5,6].
Coronary artery disease is responsible for about 30% of all cardiovascular diseases [7, 8]. One of the effects of this disease is ischemic coronary artery [9]. Angiograms are used to confirm the diagnosis, and treatment options include angioplasty or coronary artery bypass graft surgery (CABG) [10]. Annually, over a million coronary artery graft surgeries are carried out worldwide [11], with the majority of open-heart surgeries in Iran being CABG procedures [12].
In the initial days after undergoing CABG, patients are typically hospitalized in the cardiac surgery intensive care unit [13]. For individuals with ischemic coronary artery, this surgery represents a significant milestone in their lives. However, following the procedure, these patients often encounter various physical and psychological challenges, such as restlessness, insomnia, and limitations on physical activity [14].
Research suggests that the care provided during this critical period can enhance self-efficacy and empower patients to take charge of their own well-being [15, 16]. In the context of illnesses, self-efficacy beliefs have been shown to predict health-promoting behaviors [17,18,19,20]. Specifically, in the case of heart diseases, higher levels of self-efficacy are associated with improved physical and mental performance, adherence to treatment, and greater engagement in self-care practices [21, 22].
The choice of training method significantly influences patients’ learning and their willingness to change health-related behaviors, ultimately affecting their self-efficacy [23]. Patients who require additional training in various situations should receive ongoing support.
Cardiac rehabilitation (CR) is recognized as one of the most crucial approaches for enhancing self-efficacy [24, 25]. CR is a structured program designed to improve the health and well-being of individuals who have undergone cardiac procedures, such as CABG surgery. This comprehensive rehabilitation program involves a multidisciplinary team of healthcare professionals, including cardiologists, nurses, exercise physiologists, and dietitians, who collaborate to develop personalized plans for each patient [26, 27]. CR consists of three phases [28]. Research indicates that when phase I CR is implemented effectively, patients experience improved well-being following cardiac surgery and demonstrate enhanced quality of life and self-efficacy after being discharged from the hospital [29].
Augmented reality technology is a relatively new addition to medical education and patient rehabilitation skills training. It combines text, images, and videos with real-world environments [30, 31]. By incorporating physical movements within augmented reality, viewers are encouraged to focus on their training while minimizing distractions from the outside world [18].
Numerous studies have explored the effects of cardiac rehabilitation (CR) on patients who have undergone CABG surgery [32, 33]. A systematic review conducted by de Araújo Pio (2017) examined the impact of CR on postoperative mortality, cardiovascular events, exercise capacity, and quality of life in patients with coronary heart disease, including those who underwent CABG surgery [34]. Another review by Lourens et al. (2022) evaluated the influence of CR on health-related quality of life in patients following CABG surgery. The review revealed that CR interventions were associated with significant improvements in physical function, emotional well-being, and overall quality of life among this population. Furthermore, it emphasized the importance of long-term participation in these programs to sustain positive outcomes [35].
These findings underscore the significance of integrating CR as an essential component of postoperative care for CABG patients, as it enhances their sense of self-efficacy during the recovery process [27, 36, 37].
Surprisingly, there is currently no research available on CR training based on augmented reality, despite the importance of phase I CR and its impact on self-efficacy. Therefore, this study aimed to investigate the effect of phase one CR training using augmented reality on the self-efficacy of patients after cardiac surgery.
Methods
Trial Design
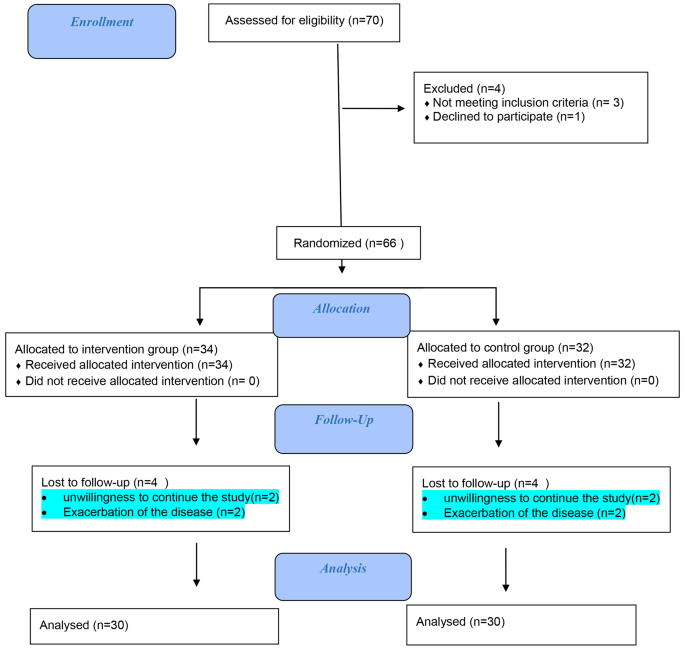
This controlled clinical trial study involved 60 patients admitted to the Ghaem Hospital of Mashhad, Iran. These patients were specifically from the cardiac surgery intensive care unit and were admitted between May 2020 and January 2021 (Fig. 1).
Participants
The study included patients who met specific inclusion criteria. These criteria required the patients to be between the ages of 18 and 60 and willing to undergo non-emergency coronary artery graft surgery. On the other hand, exclusion criteria included patients who experienced loss of consciousness until the day following surgery, those who did not have a smartphone, individuals with severe postoperative arrhythmias and hemodynamic disorders, and patients who were prohibited by their doctor from participating in rehabilitation.
Intervention
Software production
Prior to the software’s design, extensive research was conducted to prepare its content. This involved reviewing various texts, including articles, reference books, and gathering insights from experienced nurses in specialized care units. The content was then submitted to a panel of 10 specialists for validation, and their suggested revisions were incorporated.
The educational content of the software covered a range of topics, including respiratory diaphragmatic exercises, instructions on physical exercises and their proper execution, discussions and interactions with patients, and encouragement for patients to engage in routine activities. These concepts were primarily presented through instructional videos and engaging animations.
Once the content was finalized, it was handed over to the software development and information technology team for the creation of the software. After the initial software was developed, a specialized validation process was conducted by 10 IT experts to ensure its functionality and effectiveness.
To validate the software, both white-box and black-box testing methods were employed. In black-box testing, users with no knowledge of the software’s internal structure input their desired items and verify the recorded information. The aim is to ensure accurate data recording. White-box testing, on the other hand, requires users to have knowledge of the software’s internal structure and is typically executed by designers or experts. For instance, to assess the software’s speed, various items were selected at different speeds, and the accuracy of the selections was examined.
The next phase involved compatibility testing and security testing. Compatibility testing involved installing the application on multiple Android-based smartphones and tablets to assess its performance on each device. In security testing, a double confirmation method was implemented to ensure accurate recording of each patient’s issues. This involved the patient confirming their selected item by clicking again, reducing the possibility of accidental data entry errors.
The augmented reality software was registered and approved within the electronic services system of the Information Technology Organization of Iran.
To evaluate patient satisfaction with the augmented reality software, the Mobile Application Rating Scale (MARS) was employed.
This scale evaluates the application’s quality and performance across four dimensions: attractiveness (5 questions), functionality (4 questions), aesthetics (3 questions), information (7 questions), and subjective quality (4 questions). Each item in the scale was rated on a 5-point scale. The maximum achievable score was 115, while the minimum acceptable score was set at 23. For a detailed presentation of the results, please refer to (Table 1).
Phase I cardiac rehabilitation training based on augmented reality
After establishing the necessary agreements with officials at Ghaem Hospital in Mashhad, Iran, the first author of the study initiated the sampling process. In the intervention group, the rehabilitation program training started upon the patient’s entry into the cardiac surgery intensive care unit and continued until their discharge from the unit.
During multiple sessions, augmented reality software was utilized to train patients in physical activities, such as walking around the inpatient ward and climbing stairs. These exercises were done under the direct supervision of the researcher and were individually taught to each patient using the augmented reality software. The duration of physical activity varied based on the patient’s condition and length of hospital stay, ranging from 5 to 10 min. Throughout the rehabilitation sessions, ECG and the perceived exercise intensity were closely monitored and controlled.
In the control group, the rehabilitation training program was implemented using a routine method based on the Ministry of Health protocol. The researcher provided face-to-face training within the unit. Both the intervention and control groups completed the cardiac self-efficacy questionnaire upon admission and at the time of discharge in the special care unit of cardiac surgery.
Outcomes
In the data collection process, two demographic information questionnaires and a cardiac self-efficacy questionnaire were utilized.
The cardiac self-efficacy questionnaire used in this study was the Cardiovascular Management Self-Efficacy Questionnaire, which was developed by Estka from Italy in 2015. This questionnaire consists of 9 questions, each rated on a 5-point Likert scale, ranging from “completely confident” to “not at all confident.” The questionnaire is composed of three subscales.
The first four questions assess a person’s belief in their ability to quit smoking, maintain proper nutrition, engage in exercise, and avoid stressful situations. This subscale is referred to as self-efficacy of cardiac risk factors. Questions 5 and 6 pertain to a person’s confidence in remembering to take medications correctly, representing self-efficacy of treatment adherence. Lastly, questions 7–9 evaluate a person’s belief in their ability to identify symptoms and signs of disease exacerbation, indicating self-efficacy in symptom recognition.
Each response is assigned a score, with “not confident at all” receiving a score of one, “slightly confident” receiving a score of two, “somewhat confident” receiving a score of three, “fairly confident” receiving a score of four, and “completely confident” receiving a score of five. The total scores range from 9 to 45, with higher scores indicating greater self-efficacy in cardiovascular management [21]. Borzou et al. (2017) evaluated the validity and reliability of this tool in Iran [33]. The patients completed the Cardiovascular Management Self-Efficacy Questionnaire both before and after the intervention.
Sample size and randomization
The study involved the continuous and purposeful selection of patients who were then randomly assigned to one of two groups. After confirming that they met the inclusion criteria, eligible individuals were divided into intervention and control groups using a random sequence generated by SPSS software. This sequence was kept in a sealed envelope to maintain confidentiality. While it was challenging to blind the participants in this trial, the outcome assessors and statisticians were unaware of the type of intervention, ensuring a level of objectivity.
Since no similar study was found that examined the efficacy of phase I cardiac rehabilitation training based on augmented reality on the self-efficacy of patients undergoing coronary artery bypass graft surgery, a sample size of 10 participants was determined for each group. The sample size was calculated using the mean comparison formula, with a confidence interval of 95% and a test power of 80% for each group, resulting in a total of 20 participants. To account for potential dropout probability, an additional 30 participants were added to each group, representing a 10% increase from the calculated values in the formula.
Statistical methods
After data collection and sampling, the collected data were analyzed using SPSS 21. Various statistical tests were employed, including independent t-test, Mann-Whitney test, paired t-test, and chi-square test. These tests were conducted with a 95% confidence level to ensure statistical significance. Descriptive indicators such as mean, standard deviation, and frequency were also used to provide a comprehensive overview of the data. Cohen’s d was also used to evaluate the magnitude of the effect size, calculated by standardized mean difference, with g > 0.2 to 0.5 = small effect size, g > 0.5 to 0.8 = medium effect size and g > 0.8 = large effect size [38].
Results
In the study, male patients accounted for 22 cases (73.3%) in both the intervention and control groups. The mean age in the intervention group was 58.2 ± 8.3 years, while in the control group it was 59.1 ± 11.7 years (Table 2).
Regarding the length of stay in the ICU for patients who underwent coronary artery surgery, the analysis of the data showed that it was 1.3 ± 0.5 days in the intervention group and 1.4 ± 0.5 days in the control group (P = 0.251) (Table 3).
The results of the current study indicated a significant improvement in the total mean (SD) score of cardiovascular management self-efficacy in the intervention group. This improvement was observed at the time of transfer to the ICU and at the time of discharge, following the implementation of the phase I cardiac rehabilitation program based on augmented reality. An independent t-test confirmed the statistical significance of this difference (P < 0.05) (Table 4).
Discussion
The results of the present study indicated that the intervention group had a higher total mean score of cardiovascular management self-efficacy compared to the control group at the time of transfer to the ICU. This difference was observed during phase I cardiac rehabilitation (CR) training, which utilized augmented reality. Furthermore, the intervention group showed a significant increase in discharge rates compared to the control group.
This finding is consistent with a study conducted by Mohebbi et al. (2018) that compared the effect of the CR training program using two multimedia and face-to-face methods on self-efficacy and spirometry indicators in patients undergoing coronary artery graft surgery. The study demonstrated that both multimedia and face-to-face training methods were effective in improving self-efficacy, with the multimedia method having a greater impact [39]. The findings of this study were in agreement with those of the present one.
One contributing factor to this consistency is the use of educational videos during phase I CR training. Augmented reality technology, as demonstrated in the current study, offers an engaging multimedia approach that can be accessed in natural settings and tailored to individual patient needs. This expands the possibilities of traditional rehabilitation methods when combined with audio or text-based training.
The findings of the study conducted by Borzou et al. (2018) were consistent with the results of our current study. Their study examined the effects of the first phase of CR training on self-efficacy among patients undergoing coronary artery bypass graft surgery. The study demonstrated that self-efficacy scores in all aspects were significantly different between the intervention group and the control group at discharge and one month after discharge [40]. One of the contributing factors to this agreement is the phase I CR training, which consisted of theoretical and practical sessions. However, this method followed a traditional rehabilitation approach, which could be slower and less effective compared to CR exercises done by patients who possessed self-care knowledge and higher motivation. In contrast, the augmented reality system allows patients to carry out the rehabilitation program with greater focus and accuracy. It also helps to control distractions that may be present in actual medical environments [41].
Furthermore, Wang et al. (2016) examined the effects of multimedia training on exercise regimens, heart rate improvement, and self-efficacy in walking. The findings of their study align with our current study, as they demonstrated that the multimedia training program resulted in increased heart rates in the multimedia group compared to the control group. Additionally, similar to our findings, an increase in self-efficacy (P = 0.002) was observed in the intervention group, and this improvement persisted for one month (P = 0.001). However, the improvement in heart rate was only observed until the time of discharge [32]. One of the reasons for these outcomes was the use of multimedia instruction specifically designed to teach sports activities. It is important to note that the self-efficacy assessed in Wang et al.’s study focused on activity-based self-efficacy, specifically walking self-efficacy. In our current study, augmented reality technology was employed for training purposes, and the patients responded very positively to it. This change in response may be attributed to the attractiveness, motivation, and therapeutic value that augmented reality technology brings to the rehabilitation process [42]. Additionally, the use of augmented reality systems has been shown to accelerate recovery, reduce costs, and have a significant impact on rehabilitation outcomes [29].
The study conducted by Sanayi et al. (2014) found that a family-centered empowerment program could improve a patient’s self-efficacy and self-esteem during coronary artery bypass surgery [43]. This aligns with our study, where augmented reality software was used to instruct patients in the first stage of cardiac rehabilitation from admission to discharge.
Warei et al. (2014) found that two sessions of peer-to-peer training significantly increased the self-efficacy of patients undergoing coronary artery bypass graft (CABG) surgery [44]. These findings are consistent with our current study, as both studies involved the same participants who received training during their hospital stay. However, it is important to note that the teaching methods and content differed between Warei et al.’s study and our own. Therefore, a direct comparison of the effectiveness of the educational methods used in the two studies cannot be made. In our study, we assessed the self-efficacy of patients using Sullivan’s CSE questionnaire (1998).
Interakamhang et al. (2013) demonstrated how a comprehensive cardiac rehabilitation (CR) program, incorporating psychological and educational interventions, could improve psychological aspects such as self-efficacy, self-management, self-care, and quality of life in patients undergoing coronary artery graft surgery [45]. These findings align with the results of our own study. In our study, the CR program was implemented early, starting from the patients’ admission to the department, which contributed to the enhancement of general health and self-efficacy in these patients [46]. However, the difference lies in the use of augmented reality software to deliver these programs in our study, and the assessment of psychological support was done using the coping quality questionnaire.
Lian et al. (2020) conducted a study focusing on comprehensive and early rehabilitation programs that included physical exercises starting from the time of patients’ hospital admission. They found that these programs led to improvements in the physical condition and self-efficacy of patients after coronary artery bypass graft (CABG) surgery [47]. These findings are consistent with the results of our present study. The increase in self-awareness and self-assurance among patients, leading to improved physical independence, may contribute to this agreement.
In a related context, a study on the use of augmented reality in wrist rehabilitation for stroke patients demonstrated that the system enhanced hand movement performance in these patients [48].
The present study demonstrated that phase I cardiac rehabilitation training utilizing augmented reality was effective in improving postoperative self-efficacy. Additionally, it was found to be a cost-effective training method for various stages of cardiac rehabilitation. However, it is important to acknowledge the limitations of this study. One limitation was the inability of some patients to do exercises. Additionally, technical issues such as problems with installing or loading the software could have hindered the smooth implementation of the training program. Patients’ dissatisfaction with illegibility or difficulties in perceiving the font or images of the augmented reality software may have also affected their experience. Furthermore, individual differences among the patients, including their cultural background, could have influenced their ability to complete the questionnaires accurately.
Conclusion
The study findings indicated that using augmented reality in phase I CR training enhanced postoperative self-efficacy by increasing patients’ engagement with the treatment plan and prioritizing the learning process. Moreover, the use of a mobile phone, even without internet connectivity, proved to be a cost-effective training approach that can be beneficial at different stages of CR.
Data Availability
The datasets generated in the present study are available from the corresponding author upon reasonable request.
Abbreviations
- CR:
-
Cardiac rehabilitation
- CABG:
-
Coronary artery bypass graft surgery
References
Alsharari AF. The needs of family members of patients admitted to the intensive care unit. Patient Prefer Adherence 2019:465–73.
Timmis A, Vardas P, Townsend N, Torbica A, Katus H, De Smedt D, Gale CP, Maggioni AP, Petersen SE, Huculeci R. European Society of Cardiology: Cardiovascular Disease statistics 2021. Eur Heart J. 2022;43(8):716–99.
Mc Namara K, Alzubaidi H, Jackson JK. Cardiovascular Disease as a leading cause of death: how are pharmacists getting involved? Integr Pharm Res Pract 2019:1–11.
Rabiee MH, Mahmoudi A, Siahsarvie R, Kryštufek B, Mostafavi E. Rodent-borne Diseases and their public health importance in Iran. PLoS Negl Trop Dis. 2018;12(4):e0006256.
Mikkelsen N, Cadarso-Suárez C, Lado-Baleato O, Díaz-Louzao C, Gil CP, Reeh J, Rasmusen H, Prescott E. Improvement in VO2peak predicts readmissions for Cardiovascular Disease and mortality in patients undergoing cardiac rehabilitation. Eur J Prev Cardiol. 2020;27(8):811–9.
Miri K, Mohammadi E, Vanaki Z. Trend in the role of licensed practical nurses in health care system: a situational analysis. Nursing forum: 2021. Wiley Online Library; 2021. pp. 9–18.
Malakar AK, Choudhury D, Halder B, Paul P, Uddin A, Chakraborty S. A review on coronary artery Disease, its risk factors, and therapeutics. J Cell Physiol. 2019;234(10):16812–23.
Arta S, Mazlom SR, Amini S, Hajiabadi F. Comparing the effect of continuous and intermittent irrigation techniques on Complications of arterial catheter and partial thromboplastin time in patients following coronary artery bypass grafting Surgery. Evid Based Care. 2017;7(1):7–14.
Abdelnabi MH. Cardiovascular clinical implications of heart rate variability. Int J Cardiovasc Acad. 2019;5(2):37.
Gallo M, Blitzer D, Laforgia PL, Doulamis IP, Perrin N, Bortolussi G, Guariento A, Putzu A. Percutaneous coronary intervention versus coronary artery bypass graft for left main coronary artery Disease: a meta-analysis. J Thorac Cardiovasc Surg. 2022;163(1):94–105. e115.
Vervoort D, Swain JD, Pezzella AT, Kpodonu J. Cardiac Surgery in low-and middle-income countries: a state-of-the-art review. Ann Thorac Surg. 2021;111(4):1394–400.
Sedaghat S, Rostami S, Ebadi A, Fereidooni-Moghadam M. Stressors in open-heart Surgery patients: a qualitative study. ARYA Atherosclerosis. 2019;15(4):192.
Kao K-D, Lee S-YKC, Liu C-Y, Chou N-K. Risk factors associated with longer stays in cardiovascular surgical intensive care unit after CABG. J Formos Med Assoc. 2022;121(1):304–13.
Dehdari T, Heidarnia A, Ramezankhani A, Sadeghian S, Ghofranipour F. Effects of Progressive muscular relaxation training on quality of life in anxious patients after coronary artery bypass graft Surgery. Indian J Med Res. 2009;129(5):603–8.
Sabzmakan L. Effect ofhealth education program on the depression of patients after coronary artery bypass Surgery. J Fundamentals Mental Health. 2009;11(41):61–8.
Boroumand S, Shahriari M, Abbasi Jebeli M, Baghersad Z, Baradaranfard F, Ahmadpoori F. Determine the level of self-efficacy and its related factors in patients with Ischemic Heart Disease: a descriptive correlational study. Iran J Nurs Res. 2015;9(4):61–9.
Bandura A. Health promotion by social cognitive means. Health Educ Behav. 2004;31(2):143–64.
Gerbino M. Self-efficacy. The Wiley Encyclopedia of Personality and Individual Differences: Personality Processes and Individual Differences 2020:387–391.
Sarboozi-Hoseinabadi T, Askari M, Miri K, Namazi Nia M. Depression, anxiety, and stress of nurses’ Family members in Covid–19 pandemic; a case study of Torbat-e Heydariyeh hospitals. Iran J War Public Health. 2020;12(4):241–8.
Sabbaghi M, Miri K, Kahi R, Nia MN. Investigation of stress, anxiety, and depression levels of Pre-hospital Emergency Medicine personnel in eastern Iran during the Covid-19 pandemic. BMC Emerg Med. 2022;22(1):1–9.
Steca P, Greco A, Cappelletti E, D’addario M, Monzani D, Pancani L, Ferrari G, Politi A, Gestra R, Malfatto G. Cardiovascular management self-efficacy: psychometric properties of a new scale and its usefulness in a rehabilitation context. Ann Behav Med. 2015;49(5):660–74.
Norozi HM, Golmohammadi Kavaki M, Hajiabadi F, Behnam Vashani H. The Effect of Motivational Abdominal Breathing device on breathing patterns and shortness of Breath in patients with Chronic Obstructive Pulmonary Disease. Evid Based Care. 2017;6(4):36–46.
Pilannejad S, Naimi SS, Okhovatian F, Attarbashi Moghadam B, Jamalian SA, Akbarzadeh Bagheban A. The effect of the first phase of cardiac rehabilitation on quality of life and functional capacity of patients with Heart Failure. Sci J Rehabilitation Med. 2017;6(2):82–90.
Raygan F, Taghadosi M, Rajabi-Moghadam H, Hoseini A, Moravveji SA. Effect of a cardiac rehabilitation program on clinical and paraclinical findings of patients with Ischemic Heart Disease. KAUMS J (FEYZ). 2013;17(2):132–8.
Babaee G, Keshavarz M, Shayegan AHM. Effect of a health education program on quality of life in patients undergoing coronary artery bypass Surgery. Acta Medica Iranica 2007:69–75.
Dalal HM, Doherty P, Taylor RS. Cardiac rehabilitation. BMJ 2015, 351.
Taylor RS, Dalal HM, McDonagh ST. The role of cardiac rehabilitation in improving cardiovascular outcomes. Nat Reviews Cardiol. 2022;19(3):180–94.
Mehra VM, Gaalema DE, Pakosh M, Grace SL. Systematic review of cardiac rehabilitation guidelines: quality and scope. Eur J Prev Cardiol. 2020;27(9):912–28.
Baniasadi T, Ayyoubzadeh SM, Mohammadzadeh N. Challenges and practical considerations in applying virtual reality in medical education and treatment. Oman Med J. 2020;35(3):e125.
Heimo OI, Kimppa KK, Helle S, Korkalainen T, Lehtonen T. Augmented reality-Towards an ethical fantasy? In: 2014 IEEE international symposium on ethics in science, technology and engineering: 2014: IEEE; 2014: 1–7.
Khodaveisi M, Azizpour B, Jadidi A, Mohammadi Y. Education based on the health belief model to improve the level of physical activity. Phys Activity Nutr. 2021;25(4):17.
Wang L-W, Ou S-H, Tsai C-S, Chang Y-C, Kao C-W. Multimedia exercise training program improves distance walked, heart rate recovery, and self-efficacy in cardiac Surgery patients. J Cardiovasc Nurs. 2016;31(4):343–9.
Borzou SR, Amiri S, Salavati M, Soltanian AR, Safarpoor G. Comparing the effects of education of the first phase of cardiac rehabilitation on self-efficacy of men and women after heart Surgery: a clinical trial study. Iran J Rehabilitation Res. 2017;4(1):52–8.
de Araújo Pio CS, Marzolini S, Pakosh M, Grace SL. Effect of cardiac rehabilitation dose on mortality and morbidity: a systematic review and meta-regression analysis. In: Mayo Clinic Proceedings: 2017: Elsevier; 2017: 1644–1659.
Lourens EC, Baker RA, Krieg BM. Quality of life following cardiac rehabilitation in cardiac Surgery patients. J Cardiothorac Surg. 2022;17(1):137.
Rashidlamir A, Dastani M, Saadatnia A, Bassami MR. Effect of cardiac rehabilitation training on ABCA1 expression in lymphocytes of patients undergoing coronary artery bypass graft operation. Zahedan J Res Med Sci 2018, 20(6).
Kanejima Y, Shimogai T, Kitamura M, Ishihara K, Izawa KP. Effect of early mobilization on physical function in patients after cardiac Surgery: a systematic review and meta-analysis. Int J Environ Res Public Health. 2020;17(19):7091.
Cohen J. Statistical power analysis for the behavioral sciences. Academic press; 2013.
Mohebbi H, Mazlom SR, Kasraei MR, Hamedi Z, Hosseinikhah H, Dehghan Moghimi H, Ebrahimi F, Malekzadeh J. Comparison of the effects of media-based and face-to-face cardiac rehabilitation training programs on self-efficacy in patients undergoing coronary artery bypass grafting. Evid Based Care. 2018;8(2):67–77.
Borzou SR, Amiri S, Salavati M, Soltanian AR, Safarpoor G. Effects of the first phase of cardiac rehabilitation training on self-efficacy among patients undergoing coronary artery bypass graft Surgery. J Tehran Univ Heart Cent. 2018;13(3):126.
Mousavi Hondori H, Khademi M, Dodakian L, Cramer SC, Lopes CV. A spatial augmented reality rehab system for post-stroke hand rehabilitation. Medicine meets virtual reality 20. edn.: IOS Press; 2013. pp. 279–85.
Gorman C, Gustafsson L. The use of augmented reality for rehabilitation after Stroke: a narrative review. Disabil Rehabilitation: Assist Technol. 2022;17(4):409–17.
Sanaie N, Nejati S, Zolfaghari M, Alhani F, KazemNejad A. The effect of family-centered empowerment in self efficacy and self esteem in patients undergoing coronary bypass graft Surgery. J Res Dev Nurs Midwifery. 2013;10(2):4453–3.
Varaei S, Shamsizadeh M, Cheraghi MA, Talebi M, Dehghani A, Abbasi A. Effects of a peer education on cardiac self-efficacy and readmissions in patients undergoing coronary artery bypass graft Surgery: a randomized‐controlled trial. Nurs Crit Care. 2017;22(1):19–28.
Intarakamhang P, Intarakamhang U. Effects of the comprehensive cardiac rehabilitation program on psychological factors and quality of life among coronary Heart Disease patients. Global J Health Sci. 2013;5(2):145.
Ku S-L, Ku C-H, Ma F-C. Effects of phase I cardiac rehabilitation on anxiety of patients hospitalized for coronary artery bypass graft in Taiwan. Heart & lung. 2002;31(2):133–40.
Ma L, Deng L, Yu H. The effects of a comprehensive rehabilitation and intensive education program on anxiety, depression, quality of life, and major adverse cardiac and cerebrovascular events in unprotected left main coronary artery Disease patients who underwent coronary artery bypass grafting. Ir J Med Sci (1971-). 2020;189:477–88.
Phan HL, Kim JP, Kim K, Hwang CH, Koo K. -i: wrist rehabilitation system using augmented reality for hemiplegic Stroke patient rehabilitation: a feasibility study. Appl Sci. 2019;9(14):2892.
Acknowledgements
The authors would like to thank the head, the educational supervisor, the head nurse, and the nurses working in the Cardiac Surgery Intensive Care Unit of Ghaem Hospital in Mashhad, Iran.
Funding
This study was conducted as part of a Master’s Thesis in Medical-Surgical Nursing, with project code no. 980465. Dr. Fatemeh Hajiabadi received funding from the Vice-Chancellor for Research at Mashhad University of Medical Sciences, Mashhad, Iran.
Author information
Authors and Affiliations
Contributions
All authors have read and approved the manuscript. Study design: NGM, FH, SRM; data collection and analysis: NGM, FH; manuscript preparation: NGM, MN, FH, SRM.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study received ethical approval from the Research Ethics Committees of Mashhad University of Medical Sciences, Mashhad, Iran (no. IR.MUMS.NURSE.REC.1398.077), and was registered in the Iranian Registry of Clinical Trials with the code No. IRCT20200203046361N1. Prior to the study, official permission was obtained from the hospital administrators. Informed consent was obtained from all participants, ensuring their anonymity and confidentiality through data coding. The study adhered to relevant guidelines, regulations, and the principles outlined in the Declaration of Helsinki. Participants were assured that their participation was voluntary, and they had the right to withdraw from the study at any time without facing any penalties.
Consent for publication
Not applicable.
Conflict of interest
The authors declare that there is no conflict of interest in the publication of this article.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Ghlichi Moghaddam, N., Namazinia, M., Hajiabadi, F. et al. The efficacy of phase I cardiac rehabilitation training based on augmented reality on the self-efficacy of patients undergoing coronary artery bypass graft surgery: A randomized clinical trial. BMC Sports Sci Med Rehabil 15, 156 (2023). https://doi.org/10.1186/s13102-023-00770-9
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-023-00770-9