Abstract
Background
The etiology of hamstring strain injury (HSI) in American football is multi-factorial and understanding these risk factors is paramount to developing predictive models and guiding prevention and rehabilitation strategies. Many player-games are lost due to the lack of a clear understanding of risk factors and the absence of effective methods to minimize re-injury. This paper describes the protocol that will be followed to develop the HAMstring InjuRy (HAMIR) index risk prediction models for HSI and re-injury based on morphological, architectural, biomechanical and clinical factors in National Collegiate Athletic Association Division I collegiate football players.
Methods
A 3-year, prospective study will be conducted involving collegiate football student-athletes at four institutions. Enrolled participants will complete preseason assessments of eccentric hamstring strength, on-field sprinting biomechanics and muscle–tendon volumes using magnetic-resonance imaging (MRI). Athletic trainers will monitor injuries and exposure for the duration of the study. Participants who sustain an HSI will undergo a clinical assessment at the time of injury along with MRI examinations. Following completion of structured rehabilitation and return to unrestricted sport participation, clinical assessments, MRI examinations and sprinting biomechanics will be repeated. Injury recurrence will be monitored through a 6-month follow-up period. HAMIR index prediction models for index HSI injury and re-injury will be constructed.
Discussion
The most appropriate strategies for reducing risk of HSI are likely multi-factorial and depend on risk factors unique to each athlete. This study will be the largest-of-its-kind (1200 player-years) to gather detailed information on index and recurrent HSI, and will be the first study to simultaneously investigate the effect of morphological, biomechanical and clinical variables on risk of HSI in collegiate football athletes. The quantitative HAMIR index will be formulated to identify an athlete’s propensity for HSI, and more importantly, identify targets for injury mitigation, thereby reducing the global burden of HSI in high-level American football players.
Trial Registration The trial is prospectively registered on ClinicalTrials.gov (NCT05343052; April 22, 2022).
Similar content being viewed by others
Background
The incidence and burden of hamstring strain injury (HSI) is high in a number of sports involving high-speed running, including American football [1]. Understanding factors that increase the risk of HSI in football players is paramount to developing predictive models and guiding prevention strategies. The etiology of HSI is multi-factorial, with eccentric hamstring strength receiving particular attention as a primary modifiable risk factor. However, recent research suggests that eccentric hamstring strength is only weakly associated with future occurrence of HSI [2] and that the use of eccentric hamstring strength as a variable to predict future HSI is limited [3].
Hamstring strain injuries typically occur when the muscle–tendon unit (MTU) is exposed to some combination of (1) high forces; (2) lengthening action; (3) high velocity; (4) moderate-to-long length [4,5,6,7,8]. This current understanding of the injury mechanism suggests both the structure and function of the hamstrings require consideration to appropriately model an athlete’s risk of future HSI. Structurally, a larger ratio of hamstring muscle width to aponeurosis width (i.e. a large muscle relative to a smaller aponeurosis) results in higher levels of tissue strain at the muscle–tendon junction (the most common site of HSI) during running [9]. Hamstring function during running is a key element to consider when assessing HSI risk. During the second half of the swing phase, the hamstrings are active, rapidly lengthening and absorbing energy to decelerate the limb in preparation for foot contact [4]. Hamstring muscle force increases approximately 1.3-fold as running velocity increases from 80 to 100% of maximum and the greatest MTU stretch is incurred by the biceps femoris long head during high-speed running [10]. As such, “poor” running mechanics that increase MTU strain have long been considered a causative factor for HSI; however, there is limited empirical data to indicate if running mechanics influence HSI risk [11, 12].
Despite identification of important structural characteristics in the etiology of HSIs, the translation of these measures into practice has been limited due, in part, to the time and effort required to obtain them. That is, the assessment of muscle and tendon morphology requires manual segmentation of many “slices” of MRIs taken along the length of the thigh, a laborious and time-consuming process. Developing intuitive solutions to increase the adoption of measures of hamstring muscle and tendon morphology in practice is of critical importance for improving HSI prediction models. Similarly, the assessment of running mechanics is currently restricted to laboratory-based environments, which limits its practical utility. The advent of wearable sensors, such as inertial measurement units (IMUs), has the potential to allow for field-based measures of running biomechanics to assist with HSI risk determination. Developing a validated, field-based solution will lead to an increased capability to assess running mechanics and its association with future HSI.
While much attention has focused on identifying factors associated with first-time HSI, the rates of recurrent HSI are high [13, 14]. The impact of a prior HSI on structural and functional characteristics of the hamstrings, which may subsequently predispose to recurrent injury, is largely overlooked. Long-term deficits exist in musculotendon characteristics following HSI including: biceps femoris long head atrophy with compensatory short head hypertrophy; reduced muscle quality with fatty infiltration; and an increase in tendon cross sectional area due to scar tissue rather than tendon-specific hypertrophy [15,16,17,18]. These factors contribute to an increase in muscle strain under eccentric loading adjacent to the site of the index injury [17]. Determining the relevance of these changes for modeling risk of recurrent injury is of paramount importance given that prior injury is the most consistently identified risk factor for future HSI [19].
This current study aims to combine quantitative imaging, on-field biomechanics, and computational analytics into the largest-of-its-kind study of elite collegiate football players to develop the HAMstring InjuRy (HAMIR) index that can be used to reduce the burden of HSI by identifying potential future targets for HSI risk mitigation and prophylactic approaches. This paper describes the protocol that will be followed to achieve the following specific aims:
-
1.
Develop a risk prediction model for HSI based on morphological, architectural, biomechanical and clinical factors in National Collegiate Athletic Association (NCAA) Division I (D1) collegiate football players.
-
2.
Develop a risk prediction model for recurrent HSI based on morphological, architectural, biomechanical and clinical factors (identified in Aim 1) in NCAA D1 collegiate football players.
Methods/design
Overall study design and study sites
This is a longitudinal, prospective study of NCAA D1 collegiate football student-athletes across four institutions (Fig. 1). The University of Wisconsin-Madison, Brigham Young University, and University of North Carolina-Chapel Hill will begin study enrollment in the spring of 2022 and will end data collection following the completion of the spring football season in 2025. The fourth site will be added in fall of 2022 and begin study enrollment in spring of 2023 with data collection anticipated to end following the spring football season in 2026.
The overall study flow for each year is depicted in Fig. 2. All enrolled participants will complete preseason evaluations of eccentric hamstring strength along with an IMU-based assessment of sprinting biomechanics and conventional magnetic-resonance imaging (MRI). Athletic trainers will monitor injuries as well as practice and competition participation (i.e. exposure) for the duration of the study (including in- and off-season training). Participants who sustain an HSI at any point during the study will undergo a clinical assessment at the time of injury along with MRI examinations. Following completion of structured rehabilitation and return to unrestricted sport participation, clinical assessments, MRI examinations and sprinting biomechanics will be repeated. Injury recurrence will be monitored from time of injury clearance for return to sport through a 6-month follow-up window.
Data coordinating center
The American Medical Society for Sports Medicine’s Collaborative Research Network (AMSSM CRN) will serve as the data coordinating center (DCC) for this study. The DCC is responsible for providing administrative and regulatory support to all study sites, data management, monitoring and analysis, and overseeing quality assurance of the data provided by each site. During the study planning phase, the DCC assisted in development of the centralized web data capture platform, using the Research Electronic Database Capture (REDCap) system [20, 21] and a manual of operating procedures to ensure consistency and reproducibility of study policies and procedures across study sites. The DCC will lead the training of each site on data entry into REDCap as well as study policy and protocol contained in the manual of operating procedures prior to initiating study enrollment.
The AMSSM CRN is experienced in facilitating multi-site investigations and is additionally responsible for leading communication across sites as it relates to data management and study protocol. Regular meetings between the DCC and site study coordinators will be established and regular reports will be provided from the DCC to the study sites to ensure accurate data capture. The lead biostatistician within the DCC (SAK) will also work closely with the study principal investigators to oversee all statistical analyses for the HAMIR study group.
Participant recruitment and eligibility
Prior to athlete recruitment and enrollment, the study will be approved by the Institutional Review Boards of all participating institutions with all participants providing written informed consent. All rostered members of each site’s football team will be solicited to participate during each year of the 3-year study. Primary recruitment will occur prior to the fall season of each study year, from April through August. Additional recruitment for newly enrolled athletes and those who were less than 18 years old at the last enrollment opportunity will occur prior to the spring football seasons of each study year.
Study personnel at each site will meet with athletic trainers, physicians, and other key medical staff to inform them about the study. Additionally, study personnel will attend preseason meetings to recruit and consent participants. Participants will be asked to consent for the entire period of time during the study period in which they are eligible to participate. Eligibility criteria include student-athletes between the ages of 18 and 26 years of age and those rostered on the varsity football team of each participating institution during the study period. Exclusion criteria will include history of malignant disease and known contraindications to MRI.
Injury outcomes and athlete exposures
The primary outcomes for this study include index HSI and HSI re-injury. An index HSI will be defined as an acute injury to the posterior thigh that limits full, unrestricted sports participation and includes two or more of the following symptoms: palpable pain along the hamstring muscles, posterior thigh pain without radicular symptoms, weakness and/or pain with resisted knee flexion, and pain with running. HSI re-injury will be defined as an acute HSI that occurs to either limb within 6 months of an index HSI. Team athletic trainers will record daily individual HSI reports for each participant throughout the study, including in-season and off-season training. Athletic trainers will also record the occurrence and time away from sport for the following injuries: lower extremity injuries that require surgery (e.g. anterior cruciate ligament rupture; hip labral tear or femoroacetabular impingement, athletic pubalgia, tendon ruptures), other strains (e.g. gastrocsoleus complex, quadriceps, adductors) and concussions. Athletic trainers will complete weekly team reports that include the number of practice and competition exposures for each participant. An injury risk exposure will be defined as one athlete participating in one practice or competition.
MRI protocol and analysis
An MRI examination of the lumbo-pelvic region and bilateral lower extremities will be performed on all participants prior to the start of preseason (baseline). This MRI examination will be performed using 3 T scanners, a flexible surface coil, and will consist of a lumbo-pelvic and bilateral lower extremity scan to quantify muscle volumes within the entire field of view, as well as a bilateral thigh-specific scan to provide detailed contrast of the tendons and aponeuroses. The full lower extremity scan parameters were defined to create high muscle signal and low fat signal. Depending on the study site, it will consist of either an axial multi-slice 2D gradient echo fast SPGR sequence (TR/TE: 850 ms/4.5 ms, FOV 500 mm × 375 mm, 256 × 192 matrix, 5 mm thick, with fat suppression) or an axial 3D T1 DIXON sequence (TR/TE: 3.88 ms/1.1 ms and 2.2 ms, FOV 500 mm × 375 mm, 256 × 192 matrix, 5 mm thick). We have confirmed that muscle volumes calculated from each of these sequences are equivalent. Axial images will be obtained contiguously from the 12th thoracic vertebra to below the ankle joint in acquisition sets of 40 images. The tendon scan parameters were defined to highlight the contrast between tendons/aponeuroses, muscle, and fat. For all sites, it will consist of axial T1-weighted images (TR/TE: 175 ms/2.1 ms, FOV: 500 mm × 375 mm, 512 × 384 matrix, 5 mm thick, no fat suppression). The tendon scan will include axial images starting from the hamstrings’ origin on the ischium to the insertions on the tibia. MRI examinations will be repeated on those participants that sustain an HSI at the time of injury and at time of return to sport. For all sites, these examinations will include the tendon scan (as described above) as well as a fat-suppressed T2-weighted sequence (TR/TE = 7220/82.6 ms, FOV: 500 mm × 375 mm, 512 × 384 matrix, 5 mm thick) for assessment of muscle edema.
Analysis of the MR images will include quantification of all viewable muscle volumes, hamstring tendon lengths and cross-sectional areas, aponeurosis cross-sectional areas and area of attachment with muscle, scar volume and morphology, and edema volume. Automatic muscle segmentation will be performed using Springbok machine learning technology [22]. The algorithms will be updated and refined to include automatic segmentation of tendons, scar, and edema, based on training datasets that will be generated using manual segmentation. MR images obtained at time of injury will be assessed by a musculoskeletal radiologist and injury classification determined.
Acquisition and processing of IMU data
Seven IMUs (MTw Awinda, Xsens Technologies B.V., The Netherlands) will be affixed on each participant (sacrum, left and right thigh, left and right shank, left and right foot) using adhesive tape and/or straps. Prior to data collection, calibration of the IMUs will be conducted via the proprietary manufacturer software (Xsens MVN, Xsens Technologies B.V., The Netherlands).
Following calibration, a static trial will be collected with the participant standing in the anatomical position to provide baseline data for sensor orientation. Once the static trial is completed, participants will then complete a maximal velocity over-ground sprinting trial from a standing start. Additional trials will be completed as needed after a minimum of two minutes of rest.
Hip, knee and ankle joint kinematic data across time will be extracted from the entirety of all the sprinting trials (including the acceleration and deceleration phases) in addition to horizontal velocity and acceleration of the center of mass.
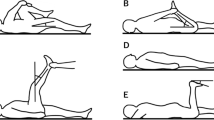
Nordbord strength testing
Eccentric hamstring strength will be measured using the NordBord Hamstring Testing System (Vald Performance, Newstead QLD, Australia) in accordance with a previously described protocol [23]. Participants will kneel on a padded platform with each ankle secured in a hook immediately superior to the lateral malleoli. Participants will be instructed to slowly lower themselves, resisting with their hamstrings, with arms across the chest and with shoulders, knees, and hips kept in a straight line. Three warm-up trials will be performed, one each at 50%, 75%, and 90% of maximal effort. Participants will then complete three trials at maximal effort with a 30 s rest after the warm-up trials and between each maximum effort trial. Trials will be accepted if the athlete maintains proper alignment during the trial, a distinct peak in maximal force output followed by a rapid decline is observed, and peaks are within 20% across the three trials. Up to two additional trials will be allowed if a distinct peak is not reached or the maximum force was more than 20% different from previous trials. Data from all trials will be recorded, and the maximum force obtained for each limb out of all trials meeting inclusion criteria will be used for subsequent analysis.
Collection of morphological, biomechanical and clinical variables
Table 1 provides an overview of the data that will be collected at baseline, within 7 days of initial HSI and within 7 days of return to sport following HSI for each year of the study. These are described in more detail below.
Baseline
At baseline, demographic and clinical characteristics including age, height, weight, playing position, prior HSI and detailed surgical history will be recorded for all participants. Additionally, participants will complete the Hamstring Outcome Score (HaOS) which is a functional patient reported outcome survey specific to their hamstring history (e.g. prior HSI) and hamstring function in training, competition and daily life [24]. Additionally, all participants will undergo baseline MRI examinations and testing of on-field sprinting biomechanics and eccentric hamstring strength. Sprinting biomechanics will be paired with MRI data to determine MTU strain. Eccentric hamstring strength of each limb will be assessed during the Nordic hamstring exercise [23, 25].
Time of injury and return to sport
Within 7 days of any diagnosed HSI, participants will undergo an additional MRI examination. A standard clinical examination will be conducted bilaterally to assess the location and extent of HSI and to evaluate the level of pain and stiffness with palpation, and hamstring range of motion and strength [26]. All participants with an HSI will undergo a post-injury rehabilitation program standardized by site [23]. Adherence to the rehabilitation program will be documented at all clinic sessions. Additionally, participants will complete the Functional Assessment Scale for Acute Hamstring Injuries (FASH) to measure the severity and impact of their symptoms on function and sports ability [27].
For participants who sustain an HSI, sprinting biomechanics and eccentric strength (as conducted at baseline) will be repeated at the return to sport time point. Determination of return to sport will be standardized by site. Within 7 days of the athlete being cleared for return to sport, the athlete will undergo another MRI examination. The same pain and clinical assessments performed at the time of injury, including the FASH, will be repeated [26].
Sample size estimation
Sample size estimates were based on current recommended steps for calculating the minimum sample size necessary for prediction model development [28]. We anticipate enrolling approximately 100 football student-athletes at each site in their first year of data collection (with the opportunity for athletes to continue in the study during years 2 and 3). In years 2 and 3, we anticipate enrolling approximately 20 new student-athletes (primarily freshmen and transfers) at each site. This will result in an estimated enrollment of approximately 560 unique student-athletes after 3 years of data collection at each site and approximately 1200 player-years across all sites over the study period. Assuming, conservatively, an HSI prevalence of 15%, 5% attrition beyond graduation and transfer (e.g. season ending injuries), a within-subject correlation of 0.3 across study years, and an R2 (proportion of variability explained by model) of 20% we will be sufficiently powered to build an index HSI HAMIR index inclusive of approximately 10–12 candidate predictor parameters. Assuming 20% of the student-athletes who sustain an index HSI will re-injure, we conservatively estimate 180 student-athletes and 36 re-injuries will be available to develop a “re-injury” HAMIR index. Using the same modeling assumptions as for the index HSI, this will allow us to create a risk prediction model with up to 4 prediction parameters. The R package pmsampsize was used to estimate sample size requirements.
Planned statistical approach
Univariate and bivariate summary statistics and distributional plots will be examined for all candidate predictor variables to assess modeling and hypothesis testing assumptions; appropriate transformations will be considered. Candidate predictors for the prediction models will include standard demographic and clinical measures, muscle strain during sprinting (mechanical), and muscle morphology (e.g. muscle, scar and edema volume). The HAMIR index prediction models for index HSI injury and re-injury will be constructed using generalized estimating equations (GEE) for binary outcomes with a logit link, and will control for athletic-exposures. The correlation among individuals in repeated years will be accounted for using an appropriately identified correlation matrix structure. Clustering at the institution level will be considered and modeled as necessary. The mechanism for missing data will be assessed during the modeling stage and multiple imputation methods will be considered if necessary. The final risk prediction model will provide predictions of the average estimated risk of HSI (or re-injury) for an athlete given the values of model variables.
We will internally validate the models using standard internal validation criteria for the development of risk prediction models. The overall performance of the models will be assessed using the Brier score and calibration assessed using the Hosmer Lemeshow Goodness of Fit Chi-square, with a value < 20 representing sufficient calibration. We will assess discrimination with the c-statistic, with a value of 0.8 or higher indicative of excellent discrimination. Bootstrapping will be used to assess the potential optimization of the model.
Discussion
The high incidence of HSI and recurrent HSI in American football continues to burden professional leagues in regards to athlete performance and financial loss. As such, there is a need to better understand the reasons for HSI injury and re-injury in these athletes so that appropriate risk reduction strategies can be created to ultimately reduce the incidence of HSI. The most appropriate strategies for reducing risk of HSI are likely multi-factorial and depend on risk factors unique to each athlete. To our knowledge, this study will be the largest-of-its-kind (1200 player-years) to gather detailed information on index and recurrent HSI, and will be the first study to simultaneously investigate the effect of morphological, biomechanical and clinical variables on risk of HSI in elite collegiate football athletes. The quantitative HAMIR index will be formulated to identify an athlete’s propensity for HSI, and more importantly, identify targets for injury mitigation, thereby reducing the global burden of HSI in elite American football players.
Because this is strictly an observational study, we cannot guarantee the same practices will occur across all sites (e.g., rehabilitation protocols, return to sport decisions), nor can we control against major program changes such as coaching and staff turnover across the duration of the study period or differences in practice and competition schedules between sites. However, these issues represent realistic variability in clinical care and sports seasons; we intend to account for site-to-site variability and athlete exposure when developing the HAMIR index. Moreover, each site has agreed to adhere to the same protocol for detailed data collection on injury management, and all MRI and IMU data will be processed at a central location. As is common to prospective cohort studies, there is the potential that we are unable to capture all protocolized timepoints on all enrolled athletes; however, the manual of operations addresses specific policies for site coordinators to follow to minimize potential missing data. Additionally, the study analysis plan proposes to assess any missingness in data collection and will account for it, as appropriate, in the analytic phase. Our ability to create a meaningful recurrent HAMIR index is entirely dependent on the number of recurrent HSIs observed during the study period. Risk factors for re-injury are largely unknown and no objective data are available to guide practitioners on return-to-play decisions following HSI. We estimate only being able to include up to 4 predictive parameters in such an index for recurrent HSI and this may or may not be sufficient to accurately predict re-injury risk. However, this information is urgently needed by practitioners and we will minimally be able to provide a preliminary predictive model that can be further tested as more re-injury data is captured in this population.
Availability of data and materials
Not applicable.
Change history
19 July 2022
The HAMIR Study Group names have been added to the PDF version of this article.
Abbreviations
- HAMIR:
-
Hamstring Injury Index
- HSI:
-
Hamstring strain injury
- IMU:
-
Inertial measurement units
- MRI:
-
Magnetic resonance imaging
- MTU:
-
Muscle–tendon unit
- NCAA:
-
National Collegiate Athletic Association
- D1:
-
Division I
- REDCap:
-
Research Electronic Data Capture
- HaOS:
-
Hamstring Outcome Score
- FASH:
-
Functional Assessment Scale for Acute Hamstring Injuries
- GEE:
-
Generalized estimating equations
- DCC:
-
Data coordinating center
References
Mack CD, Kent RW, Coughlin MJ, Shiue KY, Weiss LJ, Jastifer JR, et al. Incidence of lower extremity injury in the National Football League: 2015 to 2018. Am J Sports Med. 2020;48(9):2287–94.
Opar DA, Timmins RG, Behan FP, Hickey JT, van Dyk N, Price K, et al. Is pre-season eccentric strength testing during the Nordic hamstring exercise associated with future hamstring strain injury? A systematic review and meta-analysis. Sports Med. 2021;51:1935–45.
Ruddy JD, Shield AJ, Maniar N, Williams MD, Duhig S, Timmins RG, et al. Predictive modeling of hamstring strain injuries in elite Australian footballers. Med Sci Sports Exerc. 2018;50(5):906–14.
Chumanov ES, Heiderscheit BC, Thelen DG. Hamstring musculotendon dynamics during stance and swing phases of high-speed running. Med Sci Sports Exerc. 2011;43(3):525–32.
Chumanov ES, Wille CM, Michalski MP, Heiderscheit BC. Changes in muscle activation patterns when running step rate is increased. Gait Posture. 2012;36(2):231–5.
Heiderscheit BC, Hoerth DM, Chumanov ES, Swanson SC, Thelen BJ, Thelen DG. Identifying the time of occurrence of a hamstring strain injury during treadmill running: a case study. Clin Biomech (Bristol, Avon). 2005;20(10):1072–8.
Thelen DG, Chumanov ES, Sherry MA, Heiderscheit BC. Neuromusculoskeletal models provide insights into the mechanisms and rehabilitation of hamstring strains. Exerc Sport Sci Rev. 2006;34(3):135–41.
Lenhart R, Thelen D, Heiderscheit B. Hip muscle loads during running at various step rates. J Orthop Sports Phys Ther. 2014;44(10):766–74.
Fiorentino NM, Blemker SS. Musculotendon variability influences tissue strains experienced by the biceps femoris long head muscle during high-speed running. J Biomech. 2014;47(13):3325–33.
Chumanov ES, Heiderscheit BC, Thelen DG. The effect of speed and influence of individual muscles on hamstring mechanics during the swing phase of sprinting. J Biomech. 2007;40(16):3555–62.
Kalema RN, Schache AG, Williams MD, Heiderscheit B, Siqueira Trajano G, Shield AJ. Sprinting biomechanics and hamstring injuries: Is there a link? A literature review. Sports (Basel, Switzerland). 2021;9(10):141.
Wolski L, Pappas E, Hiller C, Halaki M, Fong Yan A. Is there an association between high-speed running biomechanics and hamstring strain injury? A systematic review. Sports Biomech. 2021. https://doi.org/10.1080/14763141.2021.1960418.
Hallén A, Ekstrand J. Return to play following muscle injuries in professional footballers. J Sports Sci. 2014;32(13):1229–36.
Orchard JW, Chaker Jomaa M, Orchard JJ, Rae K, Hoffman DT, Reddin T, et al. Fifteen-week window for recurrent muscle strains in football: a prospective cohort of 3600 muscle strains over 23 years in professional Australian rules football. Br J Sports Med. 2020;54(18):1103–7.
Sanfilippo JL, Silder A, Sherry MA, Tuite MJ, Heiderscheit BC. Hamstring strength and morphology progression after return to sport from injury. Med Sci Sports Exerc. 2013;45(3):448–54.
Silder A, Heiderscheit BC, Thelen DG, Enright T, Tuite MJ. MR observations of long-term musculotendon remodeling following a hamstring strain injury. Skelet Radiol. 2008;37(12):1101–9.
Silder A, Reeder SB, Thelen DG. The influence of prior hamstring injury on lengthening muscle tissue mechanics. J Biomech. 2010;43(12):2254–60.
Silder A, Sherry MA, Sanfilippo J, Tuite MJ, Hetzel SJ, Heiderscheit BC. Clinical and morphological changes following 2 rehabilitation programs for acute hamstring strain injuries: a randomized clinical trial. J Orthop Sports Phys Ther. 2013;43(5):284–99.
Green B, Bourne MN, van Dyk N, Pizzari T. Recalibrating the risk of hamstring strain injury (HSI): a 2020 systematic review and meta-analysis of risk factors for index and recurrent hamstring strain injury in sport. Br J Sports Med. 2020;54(18):1081–8.
Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap): a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–81.
Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, et al. The REDCap consortium: building an international community of software platform partners. J Biomed Inform. 2019;95:103208.
Ni R, Meyer CH, Blemker SS, Hart JM, Feng X. Automatic segmentation of all lower limb muscles from high-resolution magnetic resonance imaging using a cascaded three-dimensional deep convolutional neural network. J Med Imaging (Bellingham). 2019;6(4):044009.
Opar DA, Piatkowski T, Williams MD, Shield AJ. A novel device using the Nordic hamstring exercise to assess eccentric knee flexor strength: a reliability and retrospective injury study. J Orthop Sports Phys Ther. 2013;43(9):636–40.
Engebretsen AH, Myklebust G, Holme I, Engebretsen L, Bahr R. Prevention of injuries among male soccer players: a prospective, randomized intervention study targeting players with previous injuries or reduced function. Am J Sports Med. 2008;36(6):1052–60.
Opar DA, Williams MD, Timmins RG, Hickey J, Duhig SJ, Shield AJ. Eccentric hamstring strength and hamstring injury risk in Australian footballers. Med Sci Sports Exerc. 2015;47(4):857–65.
Askling CM, Nilsson J, Thorstensson A. A new hamstring test to complement the common clinical examination before return to sport after injury. Knee Surg Sports Traumatol Arthrosc Off J ESSKA. 2010;18(12):1798–803.
Malliaropoulos N, Korakakis V, Christodoulou D, Padhiar N, Pyne D, Giakas G, et al. Development and validation of a questionnaire (FASH–Functional Assessment Scale for Acute Hamstring Injuries): to measure the severity and impact of symptoms on function and sports ability in patients with acute hamstring injuries. Br J Sports Med. 2014;48(22):1607–12.
Riley RD, Ensor J, Snell KIE, Harrell FE, Martin GP, Reitsma JB, et al. Calculating the sample size required for developing a clinical prediction model. BMJ. 2020;368:m441.
Acknowledgements
We would like to acknowledge the critical feedback to the manuscript provided by Kenneth Kozloff, and the Sports Medicine staffs at the University of Wisconsin-Madison Division of Athletics, the Brigham Young University Athletic Department and Intermountain Healthcare, and the University of North Carolina Athletic Department for their commitment to the welfare of the student athletes and contributions to this research.
The HAMIR Study Group
1Geoffrey Baer, 1Craig Buckley, 1Kyle Costigan, 1Shauna Drew, 1Duffy Eberhardt, 1Kurrel Fabian, 1Herman Feller, 1Erin Hammer, 1Danielle Heidt, 1Kenneth Lee, 1Brian Lund, 1Jack Martin, 1Michael Moll, 1Jennifer Sanfilippo, 1Shaun Snee, 1Claire Tanaka, 1Ty Taylor, 1John Wilson, 1Devin Woodhouse, 3Yi-Chung Lin, 3Jack Hickey, 3Nirav Maniar, 3Frances Taylor, 3Ryan Timmins, 2Matthew Cousins, 2Olivia DuCharme, 2Xue Feng, 2Scott Magargee, 2Craig Meyer, 2Anthony Nguyen, 2Lara Riem, 2Robin West, 6Steven Allen, 6Dain Allred, 6Anthony Beutler, 6Dustin Bruening, 6Darren Campbell, 6A. Wayne Johnson, 6Camille Nguyen, 6Emma Remington, 6Annie A. Smedley, 6Joshua K. Sponbeck, 5David Berkoff, 5Josh Berkowitz, 5Thomas Birchmeier, 5Troy Blackburn, 5Malvika Choudhari, 5Mario Ciocca, 5Alessa Lennon, 5Caroline Lisee, 5Noah McCoy, 5David Mincberg, 5Scott Oliaro, 5Brian Pietrosimone, 5Luke Ross, 5Julie Titter, 7Sarah Sund.
1Badger Athletic Performance Program, Department of Orthopedics and Rehabilitation, University of Wisconsin-Madison, 1685 Highland Avenue, 6136 Medical Foundation Centennial Building, Madison, WI, 53705, USA; 2Springbok Analytics, Charlottesville, VA, USA; 3Sports Performance, Recovery, Injury and New Technologies Research Centre, School of Behavioural and Health Sciences, Australian Catholic University, Fitzroy, VIC, Australia; 5University of North Carolina-Chapel Hill, Chapel Hill, NC, United States of America; 7American Medical Society for Sports Medicine Collaborative Research Network, Leawood, USA.
Funding
The National Football League (NFL). This funding source had no role in the design of this study and will not have any role during its execution, analyses, interpretation of the data, or decision to submit results.
Author information
Authors and Affiliations
Consortia
Contributions
BH, DO, SB and SK conceived the idea of the study. BH, SK and MRS-J drafted the first version of the manuscript. DO, SB, AB, JH, and BM provided critical feedback to the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
This study is approved by the Institutional Review Boards of the University of Wisconsin-Madison (Protocol ID: 2021-1420), Brigham Young University (Protocol ID: 2021-395), and University of North Carolina-Chapel Hill (Protocol ID: 21-3293). Written informed consent is obtained from all participants before inclusion. The research is performed according to the Association for the Accreditation of Human Research Protection Programs (AAHRPP) guidelines.
Consent for publication
Not applicable.
Competing interests
Bryan Heiderscheit is a paid consultant to Biocore, has ownership interest in Science of Running Medicine LLC, is an advisory board member for Springbok Analytics (stock options) and has received research funding from the National Basketball Association and GE Healthcare. David Opar is listed as a co-inventor on a patent, filed by the Queensland University of Technology (QUT), for a field-testing device of eccentric hamstring strength, which is now known commercially as the NordBord. Dr Opar has received revenue distributions from QUT based on revenue that QUT has generated through the commercialization of his intellectual property. Dr Opar is a minority shareholder in Vald Performance Pty Ltd, the company responsible for commercialization of the NordBord, among other devices. Dr Opar has received research funding from Vald Performance, for work unrelated to the current manuscript. Dr Opar is also the Chair of the Vald Performance Research Committee, a role that is unpaid. Dr Opar has family members who are minor shareholders and/or employees of Vald Performance. Silvia Blemker is co-founder and Chief Scientific Officer of Springbok Analytics and has shares in the company. Asheesh Bedi is an advisory board member for Springbok Analytics (stock options) and ViewFi (shares), and receives consulting fees and royalties from Arthrex. Joseph Hart is co-founder and Scientific Advisor of Springbok Analytics. Lara Riem is employed by Springbok Analytics and has stock options. Xue Feng is the Chief Technology Officer for Springbok Analytics and has shares in the company. Matthew Cousins is employed by Springbok Analytics. Olivia DuCharme is employed by Springbok Analytics. Anthony Nguyen is employed by Springbok Analytics. Geoff Baer has received consulting fees from Conmed. Kenneth Lee has received research and grant support from the National Basketball Association, GE Healthcare and Supersonic Imagine, and receives royalties from Elsevier. John Wilson has received research and grant support from GE Healthcare and Depuy Synthes. The remaining authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Heiderscheit, B.C., Blemker, S.S., Opar, D. et al. The development of a HAMstring InjuRy (HAMIR) index to mitigate injury risk through innovative imaging, biomechanics, and data analytics: protocol for an observational cohort study. BMC Sports Sci Med Rehabil 14, 128 (2022). https://doi.org/10.1186/s13102-022-00520-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13102-022-00520-3