Abstract
Extraintestinal urinary tract infections are mainly caused by uropathogenic strains of E. coli. UPECs are a heterogeneous group of strains possessing various genes associated with virulence traits. It was demonstrated that changes in the composition of the o454-nlpD region and genetic variation in the mutS-rpoS chromosomal region in ExPEC strains are correlated with their virulence, particularly in those with the pattern III o454-nlpD region and belonging to phylogenetic group B2. In this study, we investigated the presence and distribution of the o454-nlpD genomic polymorphism in our collection of 124 uropathogenic E. coli strains, examining the correlation of o454-nlpD region types with the virulence factors studied. Our findings revealed a positive association between certain virulence factors in UPEC strains and the presence of pattern III in the o454-nlpD region. Additionally, all these strains were classified under phylogenetic group B2. We also showed that the highly pathogenic group of E. coli identified by examining the polymorphism of the o454-nlpD region coincides with the highly pathogenic group of uropathogens we identified in the averaged TRS-PCR analysis.
Similar content being viewed by others
Introduction
Extraintestinal infections due to Escherichia coli strains (ExPEC) pose a threat to public health worldwide. The broad spectrum of diseases they cause and the increasing costs associated with morbidity and mortality constitute a growing significant epidemic problem [1].
ExPEC is a highly heterogeneous group of strains with a wide spectrum of virulence factors and high flexibility in adapting to various environments, which enables and leads to the initiation of infection when an immunocompetent host is encountered [2,3,4,5,6].
Uropathogenic E. coli (UPEC) strains cause the vast majority of urinary tract infections (UTIs), classified as lower or upper and uncomplicated or complicated [7]. Moreover, UPEC are specialized bacteria owing to virulence and physiological factors that enable them to adapt to diverse environments and nutrient availability, which plays a significant role in their pathogenesis [8, 9]. Therefore, Köhler and Dobrindt [6], Foxman [7], and Mann et al. [8] proposed a classification of UPEC based on the site of isolation (urine) and the detection of two virulence-related genes typical of this pathotype. Many virulence factors may occur in different E. coli pathotypes of that species, which affects not only the virulence potential of one strain but also the mechanisms of pathogenesis [3, 10]. UPEC strains are very rich in virulence-associated factors. With their vast range of lipopolysaccharides, polysaccharide capsules, toxins, invasins, proteases, and adhesiveness features, they can enter and colonize the urinary tract and further disseminate in the human body [3, 11]. A multiplex-PCR test was created in our laboratory to identify some UPEC virulence genes [12]. Detection of six selected genes was proper to determine the distribution of UPEC-specific genes encoding S fimbriae (sfaD/sfaE), P fimbriae (papC), α-hemolysin (hlyA), cytotoxic necrotizing factor 1 (cnf1), uropathogenic-specific protein (usp), and the fimG/fimH region encoding subunits of type 1 fimbriae frequently present in many E. coli pathotypes [12]. Notably, this was a test that detected six factors among many others, such as siderophore systems—yersiniabactin (fyuA), salmochelin (iroN), aerobactin (iutA) or serine-protease autotransporter toxins—Sat (secreted autotransporter toxin), Tsh (temperature-sensitive hemagglutinin), and Pic (protease involved in colonization) [5, 8, 11, 13,14,15,16,17,18,19,20].
There is much evidence that some regions in the E. coli genome, such as the mutS-rpoS chromosomal region, may constitute a valuable marker for testing virulence potential due to its genetic variability [2, 21,22,23]. An enormous variability in the mutS-rpoS intergenic region and its flanking region revealed that it might change during evolution and HGT (horizontal gene transfer). This variability may contribute to the pathotype-specific polymorphism in this region [2, 23]. The characteristics of the mutS gene and the o454-nlpD genomic region enabled the association of its variability with some vital E. coli features, such as pathotype, virulence factors, and phylogeny [2]. The polymorphism of the o454-nlpD region and its correlation with virulence-associated genes may help analyze ExPEC strains [2, 22].
Moreover, this region can be distinguished into a few patterns. One of them—pattern III—was proposed as a marker for identifying highly virulent extraintestinal strains of E. coli [2, 24]. This region was also present in the strain designated FHI_NMBU_03, described as a hybrid of ExPEC with pathovars such as UPEC, APEC, NMEC, and IPEC—aEPEC, with virulence factors linked to ETEC [24].
Our study examined the presence and distribution of o454-nlpD region genomic polymorphisms in our collection of one hundred and twenty-four uropathogenic E. coli strains and the correlation of types of o454-nlpD regions with the studied virulence factors. Our aim was also to check whether the highly pathogenic group of E. coli identified by examining the polymorphism of the o454-nlpD region coincides with the highly pathogenic group of uropathogens identified by us in the averaged TRS-PCR analysis developed in our laboratory [12, 25, 26].
Materials and methods
Bacterial strains
The collection of 124 E. coli strains isolated from urine was used in this study. All strains were isolated from patients with urinary tract infections between June 2005 and September 2006 (various wards of Military Teaching Hospital No. 2, Medical University of Lodz, Poland). As published elsewhere, this collection of UPEC had virulence factors tested and phylogenetic affiliation specified [25,26,27]. The collection was serotyped according to the manufacturer’s protocols for E. coli (O pool and O single antisera, Statens Serum Institut SSI Diagnostica, Denmark) [26].
Bacterial growth and genomic DNA isolation
Bacterial growth and genomic DNA isolation for all E. coli strains were performed as previously published [26]. Strains from this collection were grown with agitation at 120 RPM overnight at 37 °C in LB liquid broth. A GenElute Bacterial Genomic DNA Kit (Sigma‒Aldrich, St. Louis, MO) was used according to the manufacturer’s protocol to isolate and purify DNA. The concentration and purity ratio in all the samples of the extracted DNA were measured spectrophotometrically (BioPhotometer, Eppendorf, Germany).
Amplification of the o454-nlpD genomic region of E. coli
PCR amplification was performed with primers F5 and R2 from Ewers et al. [8] to estimate the size of the o454-nlpD region within the tested UPEC collection. The PCR reactions followed the manufacturers’ guidelines for Taq polymerase (Invitrogen™, Life Technologies). Each reaction had a volume of 50 µl, containing 5 µl of 10× PCR buffer, 20 pmol of each primer (F5 and R2), 1.5 mM MgCl2, 0.2 mM of each deoxynucleoside triphosphate (dATP, dGTP, dCTP, and dTTP), 1 µl of chromosomal DNA solution (20 ng/μl), and 1 unit of Taq polymerase. The amplification was performed in a T-3000 thermocycler (Biometra, Goettingen, Germany) under customized conditions: initial denaturation for 3 min at 95 °C, 35 cycles: 1 min of denaturation at 95 °C, 1 min of annealing of the primers at 61 °C, 3 min of elongation at 72 °C, and final elongation for 8 min at 72 °C. The amplification products were separated on 1.6% agarose gels in 1× TAE buffer at room temperature until the dye (bromophenol blue) migrated 6 cm from the beginning of the gel (2.4 V/cm). Subsequently, gels were stained with ethidium bromide, photographed, normalized with 100 bp Plus DNA ladder (Fermentas, Thermo Scientific Waltham, MA, USA), and analyzed.
RFLP analysis of a pattern different A of the o454-nlpD region
Restriction digestion of the PCR amplification product containing the unusual o454-nlpD pattern (different A), which was approximately 1660 bp in length, was performed with Hae III (Thermo Scientific FastDigest Restriction Enzymes, MA, USA). The whole procedure was performed strictly according to the manufacturer’s protocol. Next, the digestion products were separated on a 1.8% agarose gel on 1× TAE buffer, stained with ethidium bromide, and photographed. The gel was normalized with regard to 1 kb and 50 bp DNA size markers (Fermentas, Thermo Scientific Waltham, Ma, USA).
TRS-PCR profiling
TRS-PCR profiling was previously developed and performed for the collected E. coli strains [12, 25, 26]. For each UPEC strain, similarity dendrograms of CAC-, GTG- and CGG-PCR profiles were generated separately using Pearson correlation (1% optimization, 1% position tolerance), and clustering was performed according to the UPGMA algorithm (BioNumerics software, Applied Maths, Belgium). In this work, we generated an average dendrogram of band profile similarity, showing the grouping of the studied E. coli strains. Information regarding the o454-nlpD profile, phylotype, and virulence profile was added to the analysis.
Results
In the initial research stage, we conducted amplification (using F5 and R2 primers) of the mutS-rpoS chromosomal region to examine the presence and type of the o454-nlpD region in our E. coli collection. While performing polymorphism analyses on the o454-nlpD region, we discovered an additional pattern with a different length of 1660 bp, differing from the previously described pattern [2]. To identify complementary regions in the tested genomes, we utilized the F5 and R2 primer sequences and the online software available at http://insilico.ehu.es/PCR/. Subsequently, sequences with a length of 1660 bp (representing the atypical o454-nlpD pattern) were explicitly chosen to confirm the amplified region’s accuracy.
HaeIII restriction analysis of the 1660 bp PCR products yielded restriction fragments consistent with the predictions from in silico analysis (498, 406, 306, 172, 96, 87, 39, 36, 20 bp, Additional file 1: Fig. S1). Consequently, we verified that the newly identified mutS-rpoS chromosomal region—referred to as “Different A”—corresponds to one of the analyzed o454-nlpD patterns.
The pattern distribution of the o454-nlpD region for the 124 tested UPEC strains was determined and compared with the phylogroups, virulence factors, and TRS-PCR fingerprints.
Pattern III was overrepresented, constituting 39% (49 strains) of the tested isolates. Patterns named different A and pattern I constituted 30% (37 strains) and 21% (26 strains), respectively. Only 9% (11 strains) had pattern IV, and one strain had a different B pattern. Our collection had no strains with pattern II (Fig. 1).
The phylogenetic structure of UPEC strains for obtained o454-nlpD region patterns was tested. The results are presented in Fig. 2. The UPEC strains with pattern III all belonged to phylogenetic group B2. The phylogenetic groups D, B1, and F were represented at similar levels among strains with pattern I (31%, 31%, and 27%, respectively). Strains representing phylogenetic group A predominated among strains with a pattern different A (59%). In the case of strains with pattern IV, more than half of this group belonged to phylogenetic group B1 (55%).
Our laboratory UPEC collection of strains had the virulence factor repertoire tested as published elsewhere [12, 26]. The distribution of virulence factors in strains with particular patterns of the o454-nlpD region was determined (Table 1). Genes related to siderophore systems, such as fyuA, iutA, and iroN, were detected among all strains with the pattern I. Twenty-five of 26 strains also encoded fimG/fimH, one strain had Sat, and two had Tsh—serine-protease autotransporter toxins of Enterobacteriaceae (SPATE). Six strains from this group encoded papC, two encoded sfa, two encoded cnf1, one encoded usp, and three encoded hlyA.
The pattern III strains had at least two virulence profiles associated with uropathogenicity. Moreover, the pattern III strains had the most variable profiles of virulence genes. The gene fyuA, which is related to the siderophore system, was detected in all isolates from this group. The genes iutA, iroN, and sat were present in approximately 59%, 92%, and 29% of isolates, respectively.
Only 2% of strains with the pattern different A possessed the papC gene. Each gene, such as sfaD/sfaE, cnf1, usp, and hlyA, was present in 1% of these strains. However, genes associated with siderophore systems, such as fyuA, iutA, iroN, as well astA, were identified in approximately 32%, 24%, 35%, and 24% of isolates, respectively.
Only three strains with pattern IV encoded the astA gene, and one strain encoded the tsh gene. Most of them had iutA (approx. 73%), iroN (approx. 82%), and fyuA (approx. 45.5%).
None of the tested strains had virulence genes such as bfpB, invE, elt, escV, stx1, stx2, estIa, or estIb, and they were not included in statistical analyses associated with the o454-nlpD region.
Next, Fisher’s exact test was used to estimate the correlation between the presence of o454-nlpD patterns and the identified virulence factors. The relationship was statistically significant when P values were smaller than 0.05. Pattern I: no positive associations were detected; negative association with cnf1, hly1, sfaD/sfaE, and usp; no association with papC, fimG/fimH, fyuA, iutA, iroN, sat. Pattern III: positive association with papC, sfaD/sfaE, cnf1, usp, hly1, fyuA, and iroN; negative association with fimG/fimH and sat; no association was observed with iutA. Pattern IV: no positive and no negative associations were detected; no association with papC, sfaD/sfaE, cnf1, usp, hly1, fimG/fimH, iutA, fyuA, iroN, and sat. Pattern Different A: no positive associations were detected; negative associations with papC, sfaD/sfaE, cnf1, usp, hly1, fimG/fimH, fyuA, iutA, iroN, and sat.
For virulence factors such as tsh, astA, aggR, and pic, no association was observed with any tested pattern of the o454-nlpD region. Detailed information is gathered in Table 2.
A collective comparative analysis showing the clustering of E. coli strains in the averaged TRS-PCR analysis and the relationships between the o454-nlpD profile, phylotype, and virulence factor repertoire are presented in Fig. 3.
The cluster grouping mainly highly pathogenic phylogroup B2 and type III o454-nlpD strains is marked with a black dot. Strains with profile III o454-nlpD are marked with a blue square; pathogenicity factors with a positive correlation with the o454-nlpD profile type are marked in green; pathogenicity factors with a negative correlation to the o454-nlpD profile type are marked in red.
Discussion
Extraintestinal infections due to E. coli strains constitute an urgent public health problem even though the knowledge about such strains is widened every subsequent year. The genomic plasticity of E. coli caused by mobile genetic elements such as PAIs, transposons, phages, and plasmids, which are responsible for encoding various virulence factors, is crucial in adequately classifying this species [28]. Frequent changes in E. coli genomes, such as rearrangements, deletions, and insertions, are constantly described [28]. Due to this extreme genome plasticity, new hybrid strains of E. coli may occur [24, 28, 29]. Keeping that in mind and the presence of a wide variety of virulence factors, it is not easy to anticipate how pathogenicity might evolve in the E. coli population [29]. On the other hand, one of our studies showed that it was possible to predict how pathogenicity might develop in the E. coli population [30]. Therefore, studies examining genes related to virulence potential, monitoring the pathogenic capabilities of isolates, and improving valuable diagnostics and epidemiological methods are still of great importance [24].
Our previous research has repeatedly proven the effectiveness of the TRS-PCR test in epidemiological investigations. We demonstrated the ability of this method to detect highly pathogenic E. coli strains with multiple VFs [12, 25, 26]. In this study, we decided to compare our previous results for a collection of UPEC strains with those obtained for the same collection regarding the o454-nlpD genomic region polymorphism. As changes in the composition of the o454-nlpD region and the genetic variability of the mutS-rpoS chromosomal region in ExPEC strains are correlated with their virulence [2], we wanted to analyze what type of association for these results we would observe.
Considering statistical analyses of types of o454-nlpD region and tested virulence factors, we may state that UPEC strains with pattern IV had no association with determined virulence factors. For UPEC strains with a pattern different A or pattern I, the association with virulence factors was mainly negative, or there was none. Our study demonstrated, however, a positive association between virulence factors such as papC, sfaD/sfaF, cnf1, usp, hly1, fyuA, and iroN only for UPEC strains with pattern III. All these pattern III strains were of the B2 phylotype, following the results of Ewers et al. [2]. Moreover, we agree that screening the o454-nlpD structure may enable the selection of the most virulent strains from a tested collection of samples, especially for ExPEC and, precisely, UPEC strains [2, 24]. We also showed that the averaged TRS-PCR test (CGG-PCR, GTG-PCR, and CAC-PCR) and the o454-nlpD region polymorphism test successfully detected the most virulent E. coli strains (Fig. 3).
Noticeably, our analysis of the composition of the o454-nlpD region found 38 strains with a pattern not yet described. An amplicon of 1660 base pairs was detected in 37 strains, and one strain had an amplicon of approximately six kbp. The bioinformatic analysis conducted using the appropriate primers (F5 and R2, [2]) and online software (http://insilico.ehu.es/PCR/) enabled us to find complementary regions in the tested E. coli genomes. Thanks to this and performed restriction analyses, we confirmed the atypical o454-nlpD pattern for this region with a length of approximately 1660 bp, and we named it different A. This pattern was present in 30% of our UPEC strain collection. These thirty-seven strains belonged mainly to phylogenetic groups A (59%) but also C (22%) and B1 (11%). Their virulence profiles were relatively poor, with practically no typical features for uropathogenic strains. In their study, Ewers et al. [2] stated that they observed amplicon sizes other than those described rarely and treated them as an exception.
Moreover, our study identified one strain (U 002) with a different product size than the described amplicons of the o454-nlpD region. Its length was approximately 6000 bp, and we named it a different B. This finding should be tested further to recognize the structure of its o454-nlpD region correctly and to assess whether it is an exception or potentially new pattern. Strain U 002 belonged to phylogenetic group B1 and, except FimG/H, had none of the tested virulence factors. To avoid discrepancies or misinterpretation, we did not involve this strain in the statistical calculations (Tables 1 and 2).
Conclusions
To summarize our comparative analyses, the averaged analysis of TRS-PCR band profiles grouped most uropathogenic E. coli strains possessing the type III o454-nlpD region and, consequently, strains with high pathogenicity potential.
Data availability
Not applicable.
References
Russo TA, Johnson JR. Medical and economic impact of extraintestinal infections due to Escherichia coli: focus on an increasingly important endemic problem. Microbes Infect Inst Pasteur. 2003;5:449–56.
Ewers C, Dematheis F, Singamaneni HD, Nandanwar N, Fruth A, Diehl I, Semmler T, Wieler LH. Correlation between the genomic o454-nlpD region polymorphisms, virulence gene equipment and phylogenetic group of extraintestinal Escherichia coli (ExPEC) enables pathotyping irrespective of host, disease and source of isolation. Gut Pathog. 2014;6:37. https://doi.org/10.1186/s13099-014-0037-x.
Pitout JDD. Extraintestinal pathogenic Escherichia coli: a combination of virulence with antibiotic resistance. Front Microbiol. 2012. https://doi.org/10.3389/fmicb.2012.00009.
Johnson JR, Russo TA. Extraintestinal pathogenic Escherichia coli: “the other bad E. coli”. J Lab Clin Med. 2002;139:155–62.
Kaper JB, Nataro JP, Mobley HLT. Pathogenic Escherichia coli. Nat Rev Microbiol. 2004;2:123–40.
Köhler C-D, Dobrindt U. What defines extraintestinal pathogenic Escherichia coli? Int J Med Microbiol. 2011;301:642–7. https://doi.org/10.1016/j.ijmm.2011.09.006.
Foxman B. The epidemiology of urinary tract infection. Nat Rev Urol. 2010;7:653–60. https://doi.org/10.1038/nrurol.2010.190.
Mann R, Mediati DG, Duggin IG, Harry EJ, Bottomley AL. Metabolic adaptations of uropathogenic E. coli in the urinary tract. Front Cell Infect Microbiol. 2017. https://doi.org/10.3389/fcimb.2017.00241.
Flores-Mireles AL, Walker JN, Caparon M, Hultgren SJ. Urinary tract infections: epidemiology, mechanisms of infection and treatment options. Nat Rev Microbiol. 2015;13:269–84. https://doi.org/10.1038/nrmicro3432.
Muller D, Greune L, Heusipp G, Karch H, Fruth A, Tschape H, Schmidt MA. Identification of unconventional intestinal pathogenic Escherichia coli isolates expressing intermediate virulence factor profiles by using a novel single-step multiplex PCR. Appl Environ Microbiol. 2007;73:3380–90. https://doi.org/10.1128/AEM.02855-06.
Subashchandrabose S, Mobley HLT. Virulence and fitness determinants of uropathogenic Escherichia coli. Microbiol Spectr. 2015. https://doi.org/10.1128/microbiolspec.UTI-0015-2012.
Adamus-Bialek W, Wojtasik A, Majchrzak M, Sosnowski M, Parniewski P. (CGG)4-based PCR as a novel tool for discrimination of uropathogenic Escherichia coli strains: comparison with enterobacterial repetitive intergenic consensus-PCR. J Clin Microbiol. 2009;47:3937–44. https://doi.org/10.1128/JCM.01036-09.
Terlizzi ME, Gribaudo G, Maffei ME. UroPathogenic Escherichia coli (UPEC) infections: virulence factors, bladder responses, antibiotic, and non-antibiotic antimicrobial strategies. Front Microbiol. 2017. https://doi.org/10.3389/fmicb.2017.01566.
Sabaté M, Moreno E, Pérez T, Andreu A, Prats G. Pathogenicity island markers in commensal and uropathogenic Escherichia coli isolates. Clin Microbiol Infect. 2006;12:880–6. https://doi.org/10.1111/j.1469-0691.2006.01461.x.
da Silva LC, de Mello Santos AC, Silva RM. Uropathogenic Escherichia coli pathogenicity islands and other ExPEC virulence genes may contribute to the genome variability of enteroinvasive E. coli. BMC Microbiol. 2017;17:68. https://doi.org/10.1186/s12866-017-0979-5.
Bien J, Sokolova O, Bozko P. Role of uropathogenic Escherichia coli virulence factors in development of urinary tract infection and kidney damage. Int J Nephrol. 2012. https://doi.org/10.1155/2012/681473.
Hannan TJ, Totsika M, Mansfield KJ, Moore KH, Schembri MA, Hultgren SJ. Host–pathogen checkpoints and population bottlenecks in persistent and intracellular uropathogenic Escherichia coli bladder infection. FEMS Microbiol Rev. 2012;36:616–48. https://doi.org/10.1111/j.1574-6976.2012.00339.x.
Zaw MT, Yamasaki E, Yamamoto S, Nair GB, Kawamoto K, Kurazono H. Uropathogenic specific protein-encoding gene, highly distributed in extraintestinal uropathogenic Escherichia coli, encodes a new member of H-N-H nuclease superfamily. Gut Pathog. 2013;5:13. https://doi.org/10.1186/1757-4749-5-13.
Nipič D, Podlesek Z, Budič M, Črnigoj M, Žgur-Bertok D. Escherichia coli uropathogenic-specific protein, Usp, is a bacteriocin-like genotoxin. J Infect Dis. 2013;208:1545–52. https://doi.org/10.1093/infdis/jit480.
Lüthje P, Brauner A. Virulence factors of uropathogenic E. coli and their interaction with the host. Adv Microb Physiol. 2014;65:337–72. https://doi.org/10.1016/bs.ampbs.2014.08.006.
Brzuszkiewicz E, Gottschalk G, Ron E, Hacker J, Dobrindt U. Adaptation of pathogenic E. coli to various niches: genome flexibility is the key. Microb Pathog. 2009;6:110–25. https://doi.org/10.1159/000235766.
Culham DE, Wood JM. An Escherichia coli reference collection group B2- and uropathogen-associated polymorphism in the rpoS-mutS region of the E. coli chromosome. J Bacteriol. 2000;182:6272–6.
Brown EW, LeClerc JE, Li B, Payne WL, Cebula TA. Phylogenetic evidence for horizontal transfer of mutS alleles among naturally, occurring Escherichia coli strains. J Bacteriol. 2001;183:1631–44. https://doi.org/10.1128/JB.183.5.1631-1644.2001.
Lindstedt B-A, Finton MD, Porcellato D, Brandal LT. High frequency of hybrid Escherichia coli strains with combined intestinal pathogenic Escherichia coli (IPEC) and extraintestinal pathogenic Escherichia coli (ExPEC) virulence factors isolated from human fecal samples. BMC Infect Dis. 2018. https://doi.org/10.1186/s12879-018-3449-2.
Kubiak-Szeligowska AB, Bartnicka M, Jarych D, Majchrzak M. TRS-PCR profiling for discrimination of Escherichia coli strains isolated from children with diarrhea under 5 years of age in Lodz region, Poland. Mol Biol Rep. 2016;43:871–80. https://doi.org/10.1007/s11033-016-4031-x.
Majchrzak M, Kubiak-Szeligowska AB, Jarych D, Parniewski P. Numerical interpretation of TRS-PCR profiling results for Escherichia coli strains isolated from patients with bacteriuria in Lodz region, Poland. Mol Biol Rep. 2019;46:5543–53. https://doi.org/10.1007/s11033-019-04932-2.
Clermont O, Christenson JK, Denamur E, Gordon DM. The Clermont Escherichia coli phylo-typing method revisited: improvement of specificity and detection of new phylo-groups. Environ Microbiol Rep. 2013;5:58–65. https://doi.org/10.1111/1758-2229.12019.
Bielaszewska M, Dobrindt U, Gärtner J, Gallitz I, Hacker J, Karch H, Müller D, Schubert S, Alexander Schmidt M, Sorsa LJ, Zdziarski J. Aspects of genome plasticity in pathogenic Escherichia coli. Int J Med Microbiol. 2007;297:625–39. https://doi.org/10.1016/j.ijmm.2007.03.001.
Karch H, Denamur E, Dobrindt U, Finlay BB, Hengge R, Johannes L, Ron EZ, Tønjum T, Sansonetti PJ, Vicente M. The enemy within us: lessons from the 2011 European Escherichia coli O104:H4 outbreak. EMBO Mol Med. 2012;4:841–8. https://doi.org/10.1002/emmm.201201662.
Bartoszek K, Majchrzak M, Sakowski S, Kubiak-Szeligowska AB, Kaj I, Parniewski P. Predicting pathogenicity behavior in Escherichia coli population through a state dependent model and TRS profiling. PLOS Comput Biol. 2018;14: e1005931. https://doi.org/10.1371/journal.pcbi.1005931.
Funding
This research received no specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Contributions
AK-S, MM, and PP: substantial contributions to the conception, design of the work, data analysis. AK-S: preparation of Figs. 1 and 2, Additional file 1: Fig. S1 and all Tables. MM and PP: preparation of Fig. 3. All authors: analysis, interpretation of data, manuscript preparation and revision. PP: writing final manuscript.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
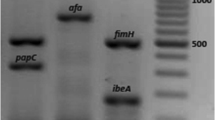
Additional file 1: Figure S1.
HaeIII restriction analysis of the 1600 bp PCR product of amplification of o454-nlpDregion for chosen UPEC strains (M1—GeneRulerTM1kb Plus DNA Ladder [Fermentas, Thermo Scientific Waltham, MA, USA); M2—GeneRulerTM50bp DNA Ladder (Fermentas, Thermo Scientific Waltham, MA, USA)].
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kubiak-Szeligowska, A.B., Majchrzak, M. & Parniewski, P. TRS-PCR profiles correlate with polymorphisms of the genomic o454-nlpD region, virulence factors repertoire, and phylogenetic groups among uropathogenic Escherichia coli strains isolated from patients from Lodz region, Poland. Gut Pathog 16, 11 (2024). https://doi.org/10.1186/s13099-024-00603-1
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13099-024-00603-1