Abstract
Background
Cancer patients with diabetes are at increased risk for cardiovascular diseases due to common risk factors and well-documented drug-associated cardiotoxicity. Sodium-glucose cotransporter-2 (SGLT2) inhibitors have shown cardiovascular benefits in patients with diabetes, but their effects on cancer patients remain unclear. This study aimed to evaluate the cardiovascular outcomes associated with SGLT2 inhibitor therapy in patients with concomitant diabetes and cancer.
Methods
We conducted a systematic review and meta-analysis of cohort studies comparing cardiovascular outcomes between cancer patients with diabetes receiving SGLT2 inhibitors and those not receiving SGLT2 inhibitors. PubMed, Embase, and the Cochrane Library were searched from inception to February 29, 2024. The primary outcome was all-cause mortality, and the secondary outcomes were heart failure hospitalization, and adverse events. Random-effect models were used to calculate pooled risk ratios (RR) with 95% confidence intervals (CI). Subgroup and sensitivity analyses were conducted to identify potential sources of heterogeneity and explore the effect of SGLT2 inhibitors on mitigating cardiotoxicity.
Results
Nine cohort studies involving 82,654 patients were included. SGLT2 inhibitor use was associated with a significantly lower risk of all-cause mortality (RR 0.46, 95% CI 0.31–0.68, P < 0.0001; I2 = 98%) and heart failure hospitalization (RR 0.49, 95% CI 0.30–0.81, P = 0.006; I2 = 21%) compared to non-use. The mortality benefit remained significant in patients receiving anthracycline chemotherapy (RR 0.50, 95% CI 0.28–0.89, P = 0.02; I2 = 71%). SGLT2 inhibitor use was also associated with a lower risk of sepsis (RR 0.32, 95% CI 0.23–0.44, P < 0.00001; I2 = 0%) and no increased risk of diabetic ketoacidosis (RR 0.66, 95% CI 0.20–2.16, P = 0.49; I2 = 0%).
Conclusions
SGLT2 inhibitor therapy is associated with lower risks of all-cause mortality and heart failure hospitalization in patients with concomitant diabetes and cancer. These findings suggest that SGLT2 inhibitors may offer cardiovascular benefits in this high-risk population. Randomized controlled trials are needed to validate these findings and evaluate the safety and efficacy of SGLT2 inhibitors in specific cancer types and treatment regimens.
Similar content being viewed by others
Introduction
Cancer treatment has made remarkable progress, resulting in a growing number of cancer survivors [1]. However, cancer patients often share risk factors, such as smoking and diabetes, which increase their likelihood of experiencing cardiovascular events and reduce cancer survival [2,3,4]. Diabetes has also been shown to impede the effectiveness of certain anti-cancer drugs [5, 6]. As the population of cancer survivors expands, there is an increasing need for strategies to address the complex relationship between cancer and cardiovascular health.
Patients who have undergone cancer treatment often face cardiovascular complications, particularly chemotherapy-associated heart failure, adding complexity to their long-term health management [7]. Notably, anthracyclines are well known for their potential to cause cardiotoxicity. In addition, the combination of chemotherapy with radiotherapy or targeted therapy has been frequently reported to contribute to cardiovascular complications [8, 9].
Early diagnosis of cardiac dysfunction and prompt initiation of neurohormonal therapy have been associated with greater left ventricular ejection fraction (LVEF) recovery [10]; however, their effectiveness remains suboptimal [11, 12]. Novel therapies, including angiotensin receptor-neprilysin inhibitors (ARNI), therapies targeting apoptosis or oxidative stress, and stem cell therapy, have also been actively explored [13, 14].
Sodium-glucose co-transporter 2 (SGLT2) inhibitors are a novel class of oral diabetes drugs that block glucose reabsorption via SGLT2 in the proximal tubules of the kidneys, leading to increased glucose excretion in the urine. These drugs have demonstrated significant cardiovascular benefits, particularly in preventing heart failure in both diabetes and non-diabetes patients [15]. Recent cohort studies have suggested possible cardiovascular benefits of SGLT2 inhibitors in cancer patients [16], and animal studies and laboratory investigations have proposed mechanisms underlying this cardioprotective effect [17,18,19].
Despite these findings, the potential role of SGLT2 inhibitors in mitigating cardiotoxicity and protecting the cardiovascular health of cancer survivors exposed to chemotherapy remains unclear. We thus performed a comprehensive systematic review and meta-analysis of available cohort studies to evaluate the cardiovascular effects of SGLT2 inhibitors in this population. Our aim is to synthesize the available observational data and generate hypotheses for novel treatment strategies. The findings from this study may provide a foundation for future clinical trials investigating the role of SGLT2 inhibitors in protecting the cardiovascular health of cancer survivors.
Methods
Search strategy and selection criteria
The review protocol has been registered in the PROSPERO International Prospective Register of Systematic Reviews (CRD 42,023,487,280) and was written according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 statement [20].
Two reviewers (H.H.K. and H.H.C.) conducted a comprehensive search of multiple electronic databases, including PubMed, Embase (excluding Medline), and the Cochrane Library, from inception to February 29, 2024, to identify relevant retrospective cohort studies investigating the association between SGLT2 inhibitors and cardiovascular outcomes in cancer patients receiving cancer therapies. The search strategy included combinations of keywords and MeSH terms related to SGLT2 inhibitors, anthracyclines, cancer, neoplasms, malignancy, cardiotoxicity, and cardiovascular outcomes.
Studies were considered eligible if they met the following criteria: [1] retrospective or prospective cohort studies; [2] included patients with active cancer undergoing cardiotoxic therapies such as chemotherapy, immune therapy, or radiotherapy; [3] compared cardiovascular outcomes between patients receiving SGLT2 inhibitors and those not receiving SGLT2 inhibitors; and [4] reported data on at least one of the following outcomes: all-cause mortality, heart failure hospitalizations, or adverse events. Studies focusing on specific cancer types or SGLT2 inhibitor agents were also eligible. Two reviewers (H.H.K and H.H.C) independently screened the titles and abstracts and reviewed the full texts of potentially eligible studies. Disagreements were resolved by discussion with a third reviewer (L.Y.L.). Reference lists of the included studies were also manually searched for additional relevant articles.
Data extraction and quality assessment
Two reviewers (H.H.K. and H.H.C.) independently extracted data from the included studies using a pre-designed form. The extracted information included the first author, publication year, country, study period, study type, number of patients, mean age, type of cancer and chemotherapy, study outcomes, and average follow-up years. Any discrepancies were resolved by discussion with a third reviewer (L.Y.L.). The methodological quality of the included cohort studies was assessed using the Newcastle-Ottawa Scale (NOS). This scale evaluates three domains: selection of study groups, comparability of groups, and ascertainment of outcomes. Studies with scores ≥ 7 were considered to be of high quality. The quality assessment was performed independently by two reviewers (H.H.K. and H.H.C.), with disagreements resolved by consensus.
Statistical analysis and data synthesis
The primary outcome was all-cause mortality, and the secondary outcomes were heart failure hospitalization and adverse events such as sepsis and diabetic ketoacidosis (DKA). The effects of SGLT2 inhibitors on the outcomes were assessed by pooled risk ratio (RR) with 95% confidence intervals (CI). We used the random-effect method to pool the results from the included studies, accounting for variance among the studies. Heterogeneity was assessed using the Cochran’s Q test and quantified by the I2 statistic. I2 values of 25%, 50%, and 75% were considered to represent low, moderate, and high heterogeneity, respectively. To address heterogeneity, we conducted subgroup and sensitivity analyses. Subgroup analyses were performed based on the use of anthracyclines and the type of cancer, if available. In the sensitivity analyses, we omitted one study at a time to evaluate the robustness of the results.
Publication bias was assessed using funnel plots. A two-tailed P < 0.05 was considered statistically significant. All analyses were performed using the Review Manager (version 5.4.1).
Results
Study selection and characteristics
The initial literature search identified 781 articles. After removing 34 duplicates and screening titles and abstracts, 16 full-text articles were assessed for eligibility. Of these, six articles were excluded because they were not original studies or contained duplicate populations. One study did not report primary outcome data, and nine studies involving a total of 82,654 patients were included in the quantitative meta-analysis (Fig. 1).
Table 1 summarizes the characteristics of the included studies. Four studies were conducted in North America (the United States and Canada) [21,22,23,24], three in Asia (Taiwan and South Korea) [25,26,27], one in Israel [28], and one using a global database [29]. Study periods ranged from January 2010 to August 2022. The total number of patients in the SGLT2 inhibitor group was 19,831 compared to 62,823 in the control group. The average age ranged from 60 to 74.8 years old. Where reported, chemotherapy regimens included anthracyclines, alkylating agents, antimetabolites, platinum-based therapies, tyrosine kinase inhibitors, and immune checkpoint inhibitors. Three studies included only cancer patients receiving anthracyclines chemotherapy [21, 24, 27]. Seven of these studies included various cancer types, while the other two consisted of a single type of cancer each: non-small cell lung cancer and hepatoma, respectively [22, 23]. Average follow-up durations ranged from 1.5 to 4.8 years. Study quality assessment using the NOS indicated that all studies were of moderate to high quality (NOS score ≥ 6).
Meta-analysis of mortality
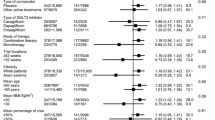
All nine studies included in the quantitative meta-analysis reported all-cause mortality as an outcome. As shown in Fig. 2a, SGLT2 inhibitor use was associated with a significantly lower risk of mortality compared to non-use (RR 0.46, 95% CI 0.31–0.68, P < 0.0001). However, high heterogeneity between studies was found in this pooled result (I2 = 98%). Subgroup analysis restricted to studies with anthracyclines chemotherapy found the mortality benefit remained significant (RR 0.50, 95% CI 0.28–0.89, P = 0.02) with moderate heterogeneity (I2 = 71%) (Fig. 2b). The all-cause mortality benefit was seen in breast cancer and lung cancer, but it was not statistically significant in hepatoma (Supplementary Fig. 1). We also conducted a sensitivity analysis by sequentially excluding one study at a time to evaluate the robustness of the results, and the pooled results remained consistent.
Meta-analysis of heart failure hospitalization
Six studies reported hospitalization due to heart failure. Patients who used SGLT2 inhibitors had a significantly lower risk for heart failure hospitalization than those without SGLT2 inhibitors (RR 0.49, 95% CI 0.30–0.81, P = 0.006). The observed heterogeneity was low (I2 = 21%) (Fig. 3). Subgroup analysis restricted to studies with anthracyclines chemotherapy showed a trend for improvement in heart failure hospitalization with low heterogeneity (RR 0.44, 95% CI 0.13–1.5, P = 0.19; I2 = 12%). One study enrolled cancer patients with prior diagnosis of cancer therapy-related cardiomyopathy or heart failure [29]. By omitting such a study in the sensitivity analysis, the risk ratio of heart failure hospitalization remained similar at 0.44 but became statistically insignificant (RR 0.44, 95% CI 0.17–1.13, P = 0.09).
Meta-analysis of adverse events
Five of the nine studies reported various adverse events associated with SGLT2 inhibitor use, including DKA, sepsis, urinary tract infection, genital infection, arrhythmia, hypoglycemia, amputation, and fournier’s gangrene. The pooled estimate for sepsis from two studies revealed a significantly lower risk in the SGLT2 inhibitor group than the non-SGLT2 inhibitor group (RR 0.32, 95% CI 0.23–0.44, P < 0.00001) (Fig. 4a). Moreover, the risk of DKA was not increased with SGLT2 inhibitor use in the pooled data (RR 0.66, 95% CI 0.20–2.16, P = 0.49) (Fig. 4b).
Publication bias
The funnel plot of mortality estimates appeared asymmetric, suggesting possible publication bias (Supplementary Fig. 2). However, sensitivity analyses using a fixed-effects model showed results consistent with the main random-effects analysis.
Discussion
This systematic review and meta-analysis of nine retrospective cohort studies provides the most up-to-date evidence that SGLT2 inhibitors have a beneficial effect on mortality and reducing cardiotoxicity in patients with cancer and type 2 diabetes mellitus undergoing cancer therapy. The pooled results involving 82,654 patients demonstrated that SGLT2 inhibitor use was associated with a significant 54% reduction in the risk of all-cause mortality (RR 0.46, 95% CI 0.31–0.68, P < 0.0001) and a 51% reduction in heart failure hospitalization (RR 0.49, 95% CI 0.30–0.81, P = 0.006) compared to patients not receiving SGLT2 inhibitors. Although the mortality analysis included a broad population of cancer patients, resulting in high heterogeneity (I2 = 98%), the significant risk reduction and consistent findings in the subgroup and sensitivity analyses strongly support the hypothesis that SGLT2 inhibitors may improve outcomes in cancer patients. Notably, the mortality benefit remained significant in the subgroup of patients receiving anthracycline chemotherapy (RR 0.50, 95% CI 0.28–0.89, P = 0.02) with moderate heterogeneity (I2 = 71%). Furthermore, SGLT2 inhibitor use was associated with a lower risk of sepsis (RR 0.32, 95% CI 0.23–0.44, P < 0.00001) and no increased risk of diabetic ketoacidosis (RR 0.66, 95% CI 0.20–2.16, P = 0.49). These findings suggest that SGLT2 inhibitors have a cardioprotective effect in mitigating anthracycline-induced cardiotoxicity without increasing the risk of serious adverse events.
The individual cohort studies included in this meta-analysis provide further insights into the potential cardioprotective effects of SGLT2 inhibitors in various cancer populations. Gongora et al. reported that SGLT2 inhibitor use was associated with fewer cardiac events, primarily driven by a reduction in heart failure admissions and new diagnoses of cardiomyopathy among patients with diabetes treated with anthracyclines [21]. Similarly, Chiang et al. observed a threefold lower rate of heart failure hospitalization and improved overall survival in SGLT2 inhibitor recipients than in non-recipients in a broader population of cancer patients treated with different types of chemotherapy drugs [25]. The effect of SGLT2 inhibitors on all-cause mortality was also observed in cancer patients treated with immune checkpoint inhibitors [28]. SGLT2 inhibitor use, in addition to guideline-directed medical therapy, reduced heart failure exacerbations, all-cause mortality, and adverse renal outcomes in patients who already had cancer therapy-related cardiac dysfunction or heart failure at baseline [29]. Major adverse cardiovascular events, a composite outcome of heart failure hospitalization, acute myocardial infarction, ischemic stroke, and death, were significantly lower in cancer patients receiving SGLT2 inhibitors [27]. Thus, SGLT2 inhibitors may offer cardiovascular benefits across different cancer types and treatment regimens.
The findings of this meta-analysis are consistent with the results of large clinical trials that have demonstrated the cardiovascular and renal benefits of SGLT2 inhibitors in patients with diabetes. The DECLARE-TIMI 58 trial demonstrated that dapagliflozin reduced the risk of hospitalization for heart failure and cardiovascular death in patients with type 2 diabetes and established cardiovascular disease or multiple risk factors [30]. Similarly, the CANVAS program found that canagliflozin reduced the risk of cardiovascular events and heart failure hospitalizations in patients with type 2 diabetes and high cardiovascular risk [31]. These trials highlight the potential of SGLT2 inhibitors to improve cardiovascular outcomes in patients with diabetes, which may extend to cancer populations with a high prevalence of diabetes and cardiovascular risk factors.
Several mechanisms have been proposed to explain the cardioprotective effects of SGLT2 inhibitors in patients with cancer and diabetes undergoing anthracycline-based chemotherapy. The potential mechanisms underlying this cardioprotection may involve the reduction of oxidative stress, inflammation, and apoptosis, as well as the improvements in mitochondrial function, fatty acid metabolism, and cardiac energy production, as suggested by preclinical studies [32,33,34,35]. SGLT2 inhibitors have been shown to increase the utilization of ketone bodies as an alternative fuel source, leading to improved cardiac efficiency and reduced oxidative stress [36]. Additionally, SGLT2 inhibitors may reduce the cardiac workload by promoting natriuresis and reducing preload and afterload [37]. These mechanisms may be particularly relevant in cancer patients, who are at increased risk of cardiovascular complications due to the direct cardiotoxic effects of cancer therapies and the high prevalence of cardiovascular risk factors [38]. Furthermore, SGLT2 inhibitors have been shown to have direct anti-tumor effects in preclinical studies, suggesting a potential dual benefit in patients with cancer [39, 40].
Interestingly, the subgroup analysis in this meta-analysis suggested that the mortality benefit of SGLT2 inhibitors may be more pronounced in patients with breast cancer and lung cancer compared to those with hepatoma. Preclinical studies have shown that SGLT2 inhibitors may have anti-cancer effects on certain tumor types. For example, in vitro studies have demonstrated that SGLT2 inhibitors can reduce the growth and proliferation of breast cancer cells by inhibiting glucose uptake and inducing apoptosis [41]. Similarly, SGLT2 inhibitors have been shown to attenuate the development of lung adenocarcinoma in mouse models by reducing glucose uptake and activating the AMPK pathway [42]. Animal experiments and cohort studies also suggest potential benefits of SGLT2 inhibitors in non-alcoholic fatty liver disease and hepatocellular carcinoma [22, 43, 44]. These findings highlight the need for further research to evaluate the potential anti-cancer effects of SGLT2 inhibitors in specific tumor types and to elucidate the underlying mechanisms.
These findings have significant clinical implications for primary care physicians, who are often involved in the long-term care of these patients and the management of their comorbidities. The results suggest that incorporating SGLT2 inhibitors into diabetes therapy for cancer patients may improve cardiovascular outcomes and overall survival without increasing the risks of DKA and sepsis.
Strengths and limitations
This meta-analysis included a large sample size of cancer patients from 9 retrospective cohort studies, increasing the power to detect significant associations. The reduction in all-cause mortality and heart failure hospitalization was significant and consistent in subgroup and sensitivity analyses, indicating the robustness of the results.
However, this study has several limitations to consider when interpreting the results. First, all included studies were observational, and thus, residual confounding due to unmeasured or inadequately measured variables cannot be excluded despite the adjustment for potential confounders in the individual studies. Furthermore, the studies relied on administrative claims data or electronic health records, which may lack detailed clinical information or have misclassification of exposures and outcomes. The duration and dosage of SGLT2 inhibitor use varied across studies, and the optimal timing and duration of treatment remain unclear. Second, the high heterogeneity observed in the mortality analysis may be due to differences in patient populations, cancer types, and treatment regimens across studies. Although efforts to account for the heterogeneity through subgroup and sensitivity analyses, the findings should be interpreted with caution. Third, the duration of follow-up varied among the included studies, ranging from 1.5 to 4.8 years, which may not be sufficient to capture long-term safety and efficacy in cancer survivors. Finally, all patients included in the cohort studies had pre-existing diabetes, and whether the benefits of SGLT2 inhibitors can be extrapolated to non-diabetic cancer patients remains to be determined.
Conclusions
This systematic review and meta-analysis suggests that SGLT2 inhibitor use may be associated with improved cardiovascular outcomes, particularly reduced mortality and heart failure hospitalization, in cancer patients with diabetes receiving cancer therapies. These findings warrant future randomized controlled trials to confirm the cardioprotective effects of SGLT2 inhibitors in cancer patients with and without diabetes and to evaluate their safety and efficacy in specific cancer types and treatment regimens. Additionally, mechanistic studies are needed to better understand the underlying pathways through which SGLT2 inhibitors exert their cardioprotective and potential anti-tumor effects on cancer therapy-induced cardiotoxicity. As the population of cancer survivors continues to grow, identifying effective strategies to mitigate the cardiovascular complications of cancer treatment becomes increasingly important. SGLT2 inhibitors may represent a promising approach to improve cardiovascular outcomes and overall survival in this vulnerable population.
Data availability
All data were extracted from publicly available sources and are included in this published article.
Abbreviations
- ARNI:
-
angiotensin receptor-neprilysin inhibitors
- CI:
-
confidence interval
- DKA:
-
diabetic ketoacidosis
- LVEF:
-
left ventricular ejection fraction
- NOS:
-
Newcastle-Ottawa Scale
- RR:
-
risk ratio
- SGLT2:
-
sodium-glucose cotransporter 2
References
Siegel RL, Miller KD, Wagle NS, Jemal A. Cancer statistics, 2023. CA Cancer J Clin. 2023;73(1):17–48.
Meijers WC, de Boer RA. Common risk factors for heart failure and cancer. Cardiovasc Res. 2019;115(5):844–53.
Yeh TL, Hsu MS, Hsu HY, Tsai MC, Jhuang JR, Chiang CJ, et al. Risk of cardiovascular diseases in cancer patients: a nationwide representative cohort study in Taiwan. BMC Cancer. 2022;22(1):1198.
Koene RJ, Prizment AE, Blaes A, Konety SH. Shared Risk factors in Cardiovascular Disease and Cancer. Circulation. 2016;133(11):1104–14.
Richardson LC, Pollack LA. Therapy insight: influence of type 2 diabetes on the development, treatment and outcomes of cancer. Nat Clin Pract Oncol. 2005;2(1):48–53.
Caudle AS, Kim HJ, Tepper JE, O’Neil BH, Lange LA, Goldberg RM, et al. Diabetes mellitus affects response to neoadjuvant chemoradiotherapy in the management of rectal cancer. Ann Surg Oncol. 2008;15(7):1931–6.
Yeh ET, Bickford CL. Cardiovascular complications of cancer therapy: incidence, pathogenesis, diagnosis, and management. J Am Coll Cardiol. 2009;53(24):2231–47.
Jawa Z, Perez RM, Garlie L, Singh M, Qamar R, Khandheria BK, et al. Risk factors of trastuzumab-induced cardiotoxicity in breast cancer: a meta-analysis. Med (Baltim). 2016;95(44):e5195.
Nicolazzi MA, Carnicelli A, Fuorlo M, Scaldaferri A, Masetti R, Landolfi R, et al. Anthracycline and trastuzumab-induced cardiotoxicity in breast cancer. Eur Rev Med Pharmacol Sci. 2018;22(7):2175–85.
Cardinale D, Colombo A, Bacchiani G, Tedeschi I, Meroni CA, Veglia F, et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation. 2015;131(22):1981–8.
Pituskin E, Mackey JR, Koshman S, Jassal D, Pitz M, Haykowsky MJ, et al. Multidisciplinary Approach to Novel therapies in Cardio-Oncology Research (MANTICORE 101-Breast): a Randomized Trial for the Prevention of Trastuzumab-Associated Cardiotoxicity. J Clin Oncol. 2017;35(8):870–7.
Vaduganathan M, Hirji SA, Qamar A, Bajaj N, Gupta A, Zaha V, et al. Efficacy of Neurohormonal therapies in preventing cardiotoxicity in patients with Cancer Undergoing Chemotherapy. JACC CardioOncol. 2019;1(1):54–65.
Vuong JT, Stein-Merlob AF, Cheng RK, Yang EH. Novel therapeutics for Anthracycline Induced Cardiotoxicity. Front Cardiovasc Med. 2022;9:863314.
Mecinaj A, Gulati G, Heck SL, Holte E, Fagerland MW, Larsen AI, et al. Rationale and design of the PRevention of cArdiac Dysfunction during adjuvant breast cancer therapy (PRADA II) trial: a randomized, placebo-controlled, multicenter trial. Cardiooncology. 2021;7(1):33.
Cardoso R, Graffunder FP, Ternes CMP, Fernandes A, Rocha AV, Fernandes G, et al. SGLT2 inhibitors decrease cardiovascular death and heart failure hospitalizations in patients with heart failure: a systematic review and meta-analysis. EClinicalMedicine. 2021;36:100933.
Usman MS, Siddiqi TJ, Anker SD, Bakris GL, Bhatt DL, Filippatos G, et al. Effect of SGLT2 inhibitors on Cardiovascular outcomes across various patient populations. J Am Coll Cardiol. 2023;81(25):2377–87.
Verma S, McMurray JJV. SGLT2 inhibitors and mechanisms of cardiovascular benefit: a state-of-the-art review. Diabetologia. 2018;61(10):2108–17.
Mohite P, Lokwani DK, Sakle NS. Exploring the therapeutic potential of SGLT2 inhibitors in cancer treatment: integrating in silico and in vitro investigations. Naunyn Schmiedebergs Arch Pharmacol. 2024.
Maurea N, Canale ML, Bisceglia I, Iovine M, Paccone A, Merola A et al. Dapagliflozin reduces myocardial and renal NFkB expression in preclinical models exposed to Doxorubicin through Myd-88 and NLRP3 pathways: an Hystological Study. Circulation. 2023;148.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:n71.
Gongora CA, Drobni ZD, Quinaglia Araujo Costa Silva T, Zafar A, Gong J, Zlotoff DA, et al. Sodium-glucose co-transporter-2 inhibitors and cardiac outcomes among patients treated with anthracyclines. JACC: Heart Fail. 2022;10(8):559–67.
Hendryx M, Dong Y, Ndeke JM, Luo J. Sodium-glucose cotransporter 2 (SGLT2) inhibitor initiation and hepatocellular carcinoma prognosis. PLoS ONE. 2022;17(9):e0274519.
Luo J, Hendryx M, Dong Y. Sodium-glucose cotransporter 2 (SGLT2) inhibitors and non-small cell lung cancer survival. Br J Cancer. 2023;128(8):1541–7.
Abdel-Qadir H, Carrasco R, Austin PC, Chen Y, Zhou L, Fang J, et al. The Association of Sodium-Glucose Cotransporter 2 inhibitors with Cardiovascular outcomes in Anthracycline-treated patients with Cancer. JACC: CardioOncology. 2023;5(3):318–28.
Chiang CH, Chiang CH, Chiang CH, Ma KS, Peng CY, Hsia YP, et al. Impact of sodium-glucose cotransporter-2 inhibitors on heart failure and mortality in patients with cancer. Heart. 2023;109(6):470–7.
Huang YM, Chen WM, Jao AT, Chen M, Shia BC, Wu SY. Effects of SGLT2 inhibitors on clinical cancer survival in patients with type 2 diabetes. Diabetes Metab. 2024;50(1):101500.
Hwang HJ, Kim M, Jun JE, Yon DK. Sodium-glucose cotransporter-2 inhibitors improve clinical outcomes in patients with type 2 diabetes mellitus undergoing anthracycline-containing chemotherapy: an emulated target trial using nationwide cohort data in South Korea. Sci Rep. 2023;13(1):21756.
Perelman MG, Brzezinski RY, Waissengrin B, Leshem Y, Bainhoren O, Rubinstein TA et al. Sodium-glucose co-transporter-2 inhibitors in patients treated with immune checkpoint inhibitors. Cardio-Oncology. 2024;10(1).
Avula V, Sharma G, Kosiborod MN, Vaduganathan M, Neilan TG, Lopez T, et al. SGLT2 inhibitor use and risk of clinical events in patients with Cancer therapy–related Cardiac Dysfunction. JACC: Heart Fail. 2024;12(1):67–78.
Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and Cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019;380(4):347–57.
Neal B, Perkovic V, Mahaffey KW, de Zeeuw D, Fulcher G, Erondu N, et al. Canagliflozin and Cardiovascular and renal events in type 2 diabetes. N Engl J Med. 2017;377(7):644–57.
Kaji K, Nishimura N, Seki K, Sato S, Saikawa S, Nakanishi K, et al. Sodium glucose cotransporter 2 inhibitor canagliflozin attenuates liver cancer cell growth and angiogenic activity by inhibiting glucose uptake. Int J Cancer. 2018;142(8):1712–22.
Quagliariello V, De Laurentiis M, Rea D, Barbieri A, Monti MG, Carbone A, et al. The SGLT-2 inhibitor empagliflozin improves myocardial strain, reduces cardiac fibrosis and pro-inflammatory cytokines in non-diabetic mice treated with doxorubicin. Cardiovasc Diabetol. 2021;20(1):150.
Sabatino J, De Rosa S, Tamme L, Iaconetti C, Sorrentino S, Polimeni A, et al. Empagliflozin prevents doxorubicin-induced myocardial dysfunction. Cardiovasc Diabetol. 2020;19(1):66.
Ren C, Sun K, Zhang Y, Hu Y, Hu B, Zhao J, et al. Sodium-glucose CoTransporter-2 inhibitor Empagliflozin ameliorates Sunitinib-Induced Cardiac Dysfunction via Regulation of AMPK-mTOR Signaling pathway-mediated autophagy. Front Pharmacol. 2021;12:664181.
Ferrannini E, Baldi S, Frascerra S, Astiarraga B, Heise T, Bizzotto R, et al. Shift to fatty substrate utilization in response to sodium-glucose cotransporter 2 inhibition in subjects without diabetes and patients with type 2 diabetes. Diabetes. 2016;65(5):1190–5.
Lytvyn Y, Bjornstad P, Udell JA, Lovshin JA, Cherney DZI. Sodium glucose Cotransporter-2 inhibition in Heart failure: potential mechanisms, clinical applications, and Summary of clinical trials. Circulation. 2017;136(17):1643–58.
Armenian SH, Lacchetti C, Barac A, Carver J, Constine LS, Denduluri N, et al. Prevention and Monitoring of Cardiac Dysfunction in survivors of adult cancers: American Society of Clinical Oncology Clinical Practice Guideline. J Clin Oncol. 2017;35(8):893–911.
Villani LA, Smith BK, Marcinko K, Ford RJ, Broadfield LA, Green AE, et al. The diabetes medication Canagliflozin reduces cancer cell proliferation by inhibiting mitochondrial complex-I supported respiration. Mol Metab. 2016;5(10):1048–56.
Nakano D, Kawaguchi T, Iwamoto H, Hayakawa M, Koga H, Torimura T. Effects of canagliflozin on growth and metabolic reprograming in hepatocellular carcinoma cells: multi-omics analysis of metabolomics and absolute quantification proteomics (iMPAQT). PLoS ONE. 2020;15(4):e0232283.
Komatsu S, Nomiyama T, Numata T, Kawanami T, Hamaguchi Y, Iwaya C, et al. SGLT2 inhibitor ipragliflozin attenuates breast cancer cell proliferation. Endocr J. 2020;67(1):99–106.
Scafoglio CR, Villegas B, Abdelhady G, Bailey ST, Liu J, Shirali AS et al. Sodium-glucose transporter 2 is a diagnostic and therapeutic target for early-stage lung adenocarcinoma. Sci Transl Med. 2018;10(468).
Arvanitakis K, Koufakis T, Kotsa K, Germanidis G. The effects of sodium-glucose cotransporter 2 inhibitors on hepatocellular carcinoma: from molecular mechanisms to potential clinical implications. Pharmacol Res. 2022;181:106261.
Krishnan A, Mukherjee D, Hutson WR, Singh S, Thakkar S, Woreta TA, INCRETIN-BASED, THERAPIES, AND SODIUMGLUCOSE COTRANSPORTER-2 INHIBITORS AND RISK OF NEWONSET NONALCOHOLIC FATTY LIVER DISEASE AND HEPATOCELLULAR CARCINOMA AMONG PATIENTS WITH TYPE 2 DIABETES IN THE UNITED STATES, et al. A NATIONWIDE REAL-WORLD LARGE POPULATION-BASED COHORT STUDY. Hepatology. 2023;78:S988–9.
Acknowledgements
Not applicable.
Funding
None.
Author information
Authors and Affiliations
Contributions
L.Y.L. conceived and designed the experiment, analyzed the data and revised the manuscript; H.H.K. and H.H.C. performed the systematic literature search, extracted and analyzed the data; K.T.W. and Z.Y.L. checked for statistical consistency and contributed to data interpretation; H.H.K. and K.T.W. drafted the manuscript; Z.Y.L. and P.L.L. critically reviewed the manuscript and contributed to the discussion. All authors reviewed the manuscript and approved the final version of this paper.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Does not involve ethical approval and consent.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Below is the link to the electronic supplementary material.

Supplementary Fig. 1.
Funnel plot of all-cause mortality.

Supplementary Fig. 2
Forest plots of all-cause mortality by cancer types. (a) Breast cancer (b) Lung cancer (c) Hepatoma.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Kuo, HH., Wang, KT., Chen, HH. et al. Cardiovascular outcomes associated with SGLT2 inhibitor therapy in patients with type 2 diabetes mellitus and cancer: a systematic review and meta-analysis. Diabetol Metab Syndr 16, 108 (2024). https://doi.org/10.1186/s13098-024-01354-4
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-024-01354-4