Abstract
Background
Abnormal lipid metabolism is associated with gestational diabetes mellitus (GDM) in singleton pregnancies. Data were lacking on twin pregnancies with GDM. We explored the association between serum lipid profiles in the first and second trimesters as well as their dynamic changes and GDM in twin pregnancies.
Methods
This was a retrospective cohort study of 2739 twin pregnancies that underwent a 75-g oral glucose tolerance test (OGTT) and were selected from the Beijing Birth Cohort Study from June 2013 to May 2021. Cholesterol (CHO), triglyceride (TG), high-density lipoprotein (HDL) and low-density lipoprotein (LDL) levels were measured at mean 9 and 25 weeks of gestation. We described maternal lipid levels in different tertiles that were associated with the risk of GDM stratified for age, pre-BMI, and fertilization type. GDM patients were divided into two groups according to OGTT: elevated fasting plasma glucose only (FPG group) and the rest of the GDM (non-FPG group). We estimated the relative risk of GDM with multivariable logistic regression models.
Results
In this study, we found that 599 (21.9%, 599/2739) twin pregnancies developed GDM. They had increased CHO, TG, LDL, and LDL/HDL, decreased HDL levels in the first trimester, and increased TG as well as decreased HDL in the second trimester in univariate analyses, each P < 0.05. In multivariate analysis, when TG > 1.67 mmol/l (upper tertile) in elderly individuals, nonoverweight and ART groups increased the risk of GDM by 2.7-fold, 2.3-fold and 2.2-fold, respectively, compared with TG < 0.96 mmol/l (lower tertile). This effect remained in the abovementioned groups in the second trimester. Moreover, high TGs increased the risk of GDM in the FPG group (OR = 2.076, 95% CI 1.130–3.815) and non-FPG group (OR = 2.526, 95% CI 1.739–3.67) in the first trimester when TG > 1.67 mmol/l, and the rising risk in the non-FPG group as the TG tertile increased remained in the second trimester. HDL predominantly showed a negative association with elevated FPG in the second trimester (p < 0.05).
Conclusions
Twin pregnancies with GDM have higher lipid levels. Increased TGs in the first and second trimesters are strongly associated with GDM, especially in elderly individuals, nonoverweight and ART groups. Lipid profiles varied among different GDM subtypes.
Similar content being viewed by others
Introduction
Along with changes in maternal age, the increased use of assisted reproductive technology (ART) has resulted in a higher frequency of multiple pregnancies [1,2,3]. Many studies have shown that adverse perinatal outcomes in twin pregnancies are significantly more common than those in singleton pregnancies. Gestational diabetes mellitus (GDM) is one of the most common complications of adverse outcomes of pregnancy and is diagnosed as a glucose intolerance disorder first identified during pregnancy [4]. GDM is closely associated with a plethora of complications for both mothers and babies in the short and long term, such as macrosomia, preeclampsia, caesarean section [5], long-term metabolic syndrome [6] and offspring metabolic disorders [7].
The incidence of GDM in twin pregnancies is significantly higher than that in singleton pregnancies [8], at 21.9% [9] in multiple pregnancies versus 14.8% [10] in singleton pregnancies in China. Advanced maternal age, obesity, ART, and Asian ethnicity, regarded as risk factors for GDM in twin pregnancies [11,12,13], have been widely considered. In singleton pregnancies, lipid metabolism disorder is also associated with GDM. Lipid profiles are elevated during pregnancy and fall to normal postpartum physiologically, acting as an energy supply for foetal growth, which is induced by progesterone, oestrogen, lactogen and the accumulation of fatty acids [14, 15]. Reports show that an increase in triglycerides (TGs) and a decrease in high-density lipoprotein-cholesterol (HDL) in early pregnancy are related to GDM in singleton pregnancies [14]. Our previous study suggested that TG ≥ 1.58 mmol/L significantly increased the risk of GDM in singleton pregnancies [16]. Twin pregnancies have higher TG levels than those with singleton pregnancies throughout the whole pregnancy [17]. However, there are no data on the association between maternal lipid levels and GDM in twin pregnancies.
In addition, GDM defined by elevated fasting plasma glucose (FPG) appears to have different pathological processes from those defined by elevated postload glucose (PG). In nonpregnancy, lipid profiles vary from impaired fasting glucose (IFG) to impaired glucose tolerance (IGT) [18, 19]. A singleton pregnancy study found that circulating fatty acid levels were different in the FPG group and PG group [20]. Nevertheless, the effect of lipid profiles on different GDM subtypes is unknown.
Thus, the purpose of this study was to examine the association of lipid profiles in the first and second trimesters, as well as their dynamic changes with GDM in twin pregnancies with different ages, pre-BMIs and fertilization types. Moreover, we aimed to explore the relationship of lipid profiles in the first and second trimesters with the subsequent risk of different GDM subtypes.
Methods
Study subjects
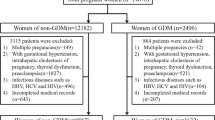
We conducted a retrospective cohort study of the Beijing Birth Cohort Study (ChiCTR220058395) in women aged 18–45 years with twin pregnancies who were followed up at Beijing Obstetrics and Gynaecology Hospital affiliated with Capital Medical University and delivered from June 2013 to May 2021. Data were obtained from the electronic medical records system. Exclusion criteria were as follows: (1) Incomplete maternal and infant information, (2) missing 75 g oral glucose tolerance test (OGTT) in 24–28 weeks, (3) presence of preexisting type 1 or type 2 diabetes mellitus, hypertension, dyslipidaemia, severe liver and kidney diseases, thyroid dysfunction, and other chronic diseases, and (4) stillbirth or reduction of 1 or both foetuses before OGTT. A total of 2739 pregnant women with twins met the above inclusion criteria, and their data were analysed (Fig. 1).
This study was conducted in Beijing Obstetrics and Gynaecology Hospital, Capital Medical University and was reviewed by the hospital's ethics committee (2018-ky-009-01). All procedures were performed in compliance with the Declaration of Helsinki.
Study design
Demographic information (age, prepregnancy height and weight, GWG, number of prior pregnancies, parity, and family history) and relevant maternal and infant outcomes, as well as laboratory data, were collected from the electronic medical record system of the hospital by trained researchers. Prepregnancy body weight was self-reported. Prepregnancy body mass index (pBMI) was calculated as prepregnancy weight in kilograms divided by the square of height in metres. Moreover, we divided all participants into several groups (young group: < 35 years old; elderly group: ≥ 35 years old; nonoverweight group: < 24 kg/m2; overweight group: ≥ 24 kg/m2; ART group: natural conception group) stratified by age, pBMI and mode of conception and estimated the risk of GDM with different tertiles of lipid concentration.
Fasting plasma glucose (FPG) was detected at 7–13 weeks, and triglyceride (TG), cholesterol (CHO), high density lipoprotein-cholesterol (HDL) and low density lipoprotein-cholesterol (LDL) were measured at 7–13 weeks (9.3 weeks on average) and 24–28 weeks (25.0 weeks on average) of gestation after fasting for at least 8–12 h. FPG in early pregnancy detected by hexokinase assay and lipid panel detection were measured by the glycerophosphate oxidase method with an automatic biochemical immunoassay system (Architect ci8200; Abbott Laboratories, Chicago, IL, USA). A 75 g oral glucose tolerance test (OGTT) was performed at 24–28 weeks. Patients were instructed to fast for 8–10 h before the OGTT test and to consume a normal diet for 3 consecutive days before the test (≥ 150 g of carbohydrates a day) [20]. FPG, 1 h-PG, and 2 h-PG were determined by the glucose oxidase method with a DxC800 automatic biochemical analyser (Beckman Coulter Company, USA).
Definition
According to the 2013 American Diabetes Association (ADA) criteria, a 75‐g oral glucose tolerance test was completed at weeks 24–28 in women not previously diagnosed with overt diabetes. GDM was diagnosed if any one of the following criteria of plasma glucose was met: fasting ≥ 5.1 mmol/L, 1 h ≥ 10.0 mmol/L, or 2 h ≥ 8.5 mmol/L. According to the OGTT results, twin pregnancies were divided into 3 groups: the non-GDM group (no elevated glucose), FPG group (isolated elevated glucose level at fasting with normal glucose levels at 1 h and 2 h), and non-FPG group (excluded GDM with isolated higher FPG which including elevated PG only and patients with both high FPG and high PG). Polycystic ovarian syndrome (PCOS) was diagnosed pre‐conception according to the modified Rotterdam Criteria, which requires the presence of 2 of the following 3 criteria: ovulation or anovulation, clinical manifestations of hyperandrogen and/or hyperandrogenemia, and ultrasound findings of polycystic ovary. Patients with other diseases, such as congenital adrenal cortical hyperplasia, Cushing’s syndrome and androgen-secreting tumours, were excluded [21]. Newborns with birth weights ≥ 4000 g delivered before this pregnancy were diagnosed with a history of macrosomia.
Statistics
Student’s t test was used to compare continuous variables from the Twin‐GDM and Twin‐non‐ GDM groups, while the chi‐square test was used to analyse categorical variables. Repeated measurement data used repeated-measures ANOVA. Descriptive information was reported as the mean ± standard deviation for continuous variables. To examine the associations of maternal lipid concentrations in different stratifications with the risk of GDM and GDM subtypes, we calculated different tertiles of the lipid concentrations. A multivariate logistic regression was constructed based on univariate analyses, and we adjusted for age, prepregnancy BMI, family history of diabetes, ART, PCOS and FPG. Odds ratios (ORs) and 95% confidence intervals (CIs) were calculated in the multivariable logistic regression analyses. All statistical analyses were performed using SPSS version 26.0 (IBM Corp., Armonk, NY, USA). P < 0.05 was considered statistically significant.
Results
In this study, 599 (21.9%, 599/2739) twin pregnancies developed GDM, while 2140 (78.1%, 2140/2739) had a normal oral glucose tolerance test. Clinical characteristics are described in Table 1. Compared with the non‐GDM group, GDM women had an increased maternal age, higher pre-BMI, and were more likely to have a diabetes family history, PCOS and ART (P < 0.05). They also had increased CHO, TG, LDL, and LDL/HDL levels but lower HDL levels in the first trimester (P < 0.05). In the second trimester, except for TG and HDL, other lipid profiles converged. Concordantly, ∆CHO, ∆LDL, and ∆LDL/HDL levels of women in the non-GDM group were higher than those in the GDM group, whereas there was no significant difference in TG and HDL levels between the two groups.
We conducted two multiple logistic regression models (Tables 2 and 3), adjusted for age, prepregnancy BMI, family history of diabetes, IVF-ET, and PCOS in Model 1 and added FPG in the first trimester in Model 2. The results showed that whether we adjusted for FPG or not, higher TG levels were significantly associated with GDM in the first and second trimesters. High LDL/HDL increased the risk of GDM in Model 2 but not in Model 1 in the first trimester. Significantly, HDL showed a negative correlation with GDM in both models in the second trimester (P < 0.05).
Moreover, we divided all participants into several groups stratified by age, pBMI and fertilization type and estimated the risk of GDM with different tertiles of lipid concentration. The results are shown in Tables 4 and 5. As TGs rise, the risk of diabetes also increases significantly in the first trimester, independent of their stratification. When TG > 1.67 mmol/l in elderly individuals, nonoverweight and ART groups, the risk of GDM increased 2.7-fold, 2.3-fold and 2.2-fold, respectively, compared with TG < 0.96 mmol/l. Nevertheless, TG remained associated in the second trimester in elderly individuals, nonoverweight and ART groups. Meanwhile, the risk of GDM increased when LDL/HDL > 1.65 mmol/l, but the correlation between HDL and GDM was nonsignificant after stratification in the second trimester Additional file 1: Tables S1, S2.
We further explored the association between blood lipids and GDM subtypes. Twin pregnancies were divided into 3 groups according to OGTT results (Table 6). Women with TG > 1.67 mmol/l experienced a 2.1-fold increased risk of GDM defined by elevated FPG only (95% CI 1.13–3.815) and a 2.5-fold increased risk of GDM in the non-FPG group (95% CI 1.739–3.67) compared with women who had concentrations < 0.96 mmol/l in the first trimester. In the second trimester, there was still a rising risk in the non-FPG group as the TG tertile grew up, but the risk was nonsignificant for the FPG group. Moreover, HDL predominantly showed a negative association with elevated FPG in the second trimester (p < 0.05). The findings showed that high LDL/HDL elevated FPG but was nonsignificant for LDL/HDL > 1.65 mmol/l. Other elevated lipid profiles had no significant effect on fasting and postload blood glucose levels.
Discussion
In this study, we found that the lipid profile of twin pregnancies with GDM differs from that of non-GDM women in the first and second trimester, but there is no significant result in their dynamic changes. Moreover, after stratification, adjusting for confounders, our results showed that twin pregnancies with higher TGs were at an increased risk of developing GDM in the first trimester in each subgroup. This effect remained in elderly, nonoverweight and ART-conceived women in second trimester, but the intensity decreased. The negative association of HDL appeared in the second trimester but disappeared after stratification. In addition, heterogeneity in the lipid profiles of GDM subtypes was shown in this study. Elevated TG levels in the first trimester increased FBG levels as well as PG levels. In the second trimester, TGs predominantly increased PG, whereas HDL showed a negative relationship with FBG.
During pregnancy, blood lipid levels increase due to progesterone and accumulation of fat to prepare for foetal growth [15, 22]. However, a large number of singleton pregnancy studies have confirmed that lipid metabolism disorders result in GDM, which manifests as high TGs in the first trimester [16, 23, 24]. In twin pregnancies, we found that elevated TGs in the first trimester also increased the risk of GDM, which is regarded as an important metabolic abnormality associated with insulin resistance [25]. Similar to our results, a Chinese study analysed 96 cases of twin pregnancies with 22 cases of GDM and found that TG levels in women with GDM were higher than that in women with non-GDM in the first and second trimesters. However, there was no significant difference in CHO levels in the whole pregnancy between GDM and non-GDM women, which was different from the results of our univariate analysis. However, in our multivariate analysis, there was no significant association between TC and GDM in the first and second trimesters of twin pregnancies [17]. A singleton pregnancy meta-analysis also found that high TGs remained consistent across each trimester in women with GDM in the second trimester [14]. However, high HDL and non-HDL results in the second trimester in women with GDM were inconsistent with our results [14] due to the heterogeneity of studies caused by age and prepregnancy BMI. Moreover, Bao et al. [22] also described different results in that high TGs and low HDL even showed a stronger association with GDM in the second trimester than in the first trimester in the multivariable model. In our study, the association between lipid profiles and GDM in the second trimester appeared to be mitigated, possibly due to the higher maternal costs for the growth of both foetuses. In addition, our study showed that there was no significant difference in the dynamic changes in lipid profiles between the GDM and control groups, which indicated that the absolute value of lipids in the first and second pregnancy are more noteworthy than their dynamic changes.
In recent years, an increasing number of studies have focused on the risk factors for GDM in twin pregnancies. Similar to our results, some studies found that twin pregnancies with GDM were more likely to be elderly [26], with a higher pre-BMI [27] and ART [28]. After we conducted further subgroup analyses stratified for maternal age, pre-BMI, and fertilization type, we found strong associations of increased TGs with the risk of developing GDM in each subgroup in the first trimester. This effect remained in elderly, nonoverweight and ART-conceived women in the second trimester. This suggests that more attention should be given to twin pregnancies with higher TG concentrations regardless of whether they have risk factors in the first trimester, as well as to specific populations in the second trimester. We previously conducted multiple regression analyses in singleton pregnancies [16] and indicated that high maternal TG levels was associated with an increased risk of GDM in the first trimester, independent of the mothers’ pre-BMI. Nevertheless, the negative relationship between HDL and GDM in the second trimester disappeared after stratification, indicating that this effect was caused by confounding factors.
In addition, our study revealed that TG increased FPG and PG levels in the first trimester. In the second trimester, TG predominantly impaired PG, while HDL showed a negative relationship with FPG. In recent years, scientists began to explore the subtypes of GDM, but most of them divided GDM into insulin sensitivity defects and insulin secretion defects, which were different from our subtypes. However, there is a connection between these two different classification methods. Powe noted that women in the GDM-sensitivity group had increased FPG and PG, whereas the GDM-secretion group only had increased PG [29]. Jill Layton found that TG increased in insulin sensitivity defects but not secretion defects in GDM [30]. These results suggested that TG elevated FPG and PG levels, probably by affecting insulin sensitivity. We can also find some evidence from nonpregnant studies. A European cohort showed that TG increased FPG and PG levels, which is consistent with our study [18]. TG predicts IFG better than other parameters [31] by impacting NO homeostasis and endothelial function to cause inflammation and oxidative stress [32]. Similar to our results, HDL also protects people with IFG from developing T2DM [18] by increasing plasma insulin and activating AMP-activated protein kinase in skeletal muscle [33]. In nonpregnancy, IFG and IGT have different pathological processes [34]. IFG patients predominantly present with hepatic IR and relatively normal muscle IR, while IGT patients present with the inverse condition [35, 36]. In our twin pregnancy study, the lipid profile also varied between the FPG and PG groups. Perhaps the pathological mechanism is similar to that of nonpregnant people.
To the best of our knowledge, this is the first study that compared lipid profiles of GDM women with twin pregnancies in the first and second trimesters as well as their dynamic changes with a large sample size. In addition, to exclude possible effects of confounding factors on GDM risk, we further analysed maternal lipid profiles associated with adjusted risks of GDM stratified for age, pre-BMI and fertilization type. Moreover, we first described the heterogeneity of maternal lipid levels in different GDM subtypes in twin pregnancies. However, our study still has some limitations. First, retrospective studies might have limitations due to potential confounding factors, such as educational status, alcohol consumption, and smoking status. Information on insulin is also insufficient, but we examined GDM subtypes according to FPG and PG levels. Second, potential selection bias may be present because our institution is a tertiary care centre. Although older and overweight twin pregnancies and those with ART are generally considered high-risk, women with uncomplicated pregnancies are less likely to visit a tertiary care centre. This may result in an increased incidence of GDM.
Conclusion
Our study suggested that twin pregnancies with GDM have higher lipid levels. This finding implies that special attention should be given by health care providers to twin pregnancies with higher TG concentrations regardless of whether they have other risk factors. We also noted that lipid profiles varied among women with different GDM subtypes. In addition, an increasing number of new biomarkers, such as cortisol, leptin, adiponectin and human placental lactate (hPL), have been found to be related to the incidence of insulin resistance-induced diabetes [37,38,39,40]. Individualized management of dyslipidaemia in twin pregnancies in the first trimester is needed.
Availability of data and materials
The data is available upon reasonable request to the corresponding author.
Abbreviations
- GDM:
-
Gestational diabetes mellitus
- OGTT:
-
75-G Oral glucose tolerance test
- CHO:
-
Cholesterol
- TG:
-
Triglyceride
- HDL:
-
High-density lipoprotein
- LDL:
-
Low-density lipoprotein
- FPG:
-
Fasting plasma glucose
- PG:
-
Post-load glucose
- IFG:
-
Impaired fasting glucose
- IGT:
-
Impaired glucose tolerance
- pBMI:
-
Pre-pregnancy body mass index
- ART:
-
Assisted reproductive technology
- ADA:
-
American Diabetes Association
- PCOS:
-
Polycystic ovarian syndrome
- ORs:
-
Odds ratios
- CI:
-
Confidence intervals
- hPL:
-
Human placental lactogen
References
Smith LK, et al. Trends in the incidence and mortality of multiple births by socioeconomic deprivation and maternal age in England: population-based cohort study. BMJ Open. 2014;4(4): e004514.
Buchanan TA, Xiang AH, Page KA. Gestational diabetes mellitus: risks and management during and after pregnancy. Nat Rev Endocrinol. 2012;8(11):639–49.
Adashi EY, Gutman R. Delayed childbearing as a growing, previously unrecognized contributor to the national plural birth excess. Obstet Gynecol. 2018;132(4):999–1006.
Kjos SL, Buchanan TA. Gestational diabetes mellitus. N Engl J Med. 1999;341(23):1749–56.
Catalano PM, et al. The hyperglycemia and adverse pregnancy outcome study: associations of GDM and obesity with pregnancy outcomes. Diabetes Care. 2012;35(4):780–6.
Bellamy L, et al. Type 2 diabetes mellitus after gestational diabetes: a systematic review and meta-analysis. Lancet. 2009;373(9677):1773–9.
Hiersch L, Yogev Y. Impact of gestational hyperglycemia on maternal and child health. Curr Opin Clin Nutr Metab Care. 2014;17(3):255–60.
Rauh-Hain JA, et al. Risk for developing gestational diabetes in women with twin pregnancies. J Matern Fetal Neonatal Med. 2009;22(4):293–9.
Lin D, Fan D, Li P, et al. Perinatal outcomes among twin pregnancies with gestational diabetes mellitus: a nine-year retrospective cohort study. Front Public Health. 2022;2022(10): 946186.
Gao C, et al. Prevalence of gestational diabetes mellitus in mainland China: a systematic review and meta-analysis. J Diabetes Investig. 2019;10(1):154–62.
Ooi S, Wong VW. Twin pregnancy with gestational diabetes mellitus: a double whammy? Diabetes Care. 2018;41(2):e15–6.
Buerger O, et al. First-trimester screening for gestational diabetes mellitus in twin pregnancies. J Clin Med. 2021;10(17):3814.
Hiersch L, et al. Gestational diabetes mellitus is associated with adverse outcomes in twin pregnancies. Am J Obstet Gynecol. 2019;220(1):102-e1.
Ryckman KK, et al. Maternal lipid levels during pregnancy and gestational diabetes: a systematic review and meta-analysis. BJOG. 2015;122(5):643–51.
Wiznitzer A, et al. Association of lipid levels during gestation with preeclampsia and gestational diabetes mellitus: a population-based study. Am J Obstet Gynecol. 2009;201(5):482.e1-8.
Li G, et al. Early pregnancy maternal lipid profiles and the risk of gestational diabetes mellitus stratified for body mass index. Reprod Sci. 2015;22(6):712–7.
Lou Y, et al. Analysis of the characteristics of blood lipid metabolism in twin pregnancy. J Investig Med. 2023;71(1):53–7.
Giannini S, et al. Lipid levels in obese and nonobese subjects as predictors of fasting and postload glucose metabolism. J Clin Lipidol. 2012;6(2):132–8.
Hwang YC, et al. Association of HDL-C and apolipoprotein A-I with the risk of type 2 diabetes in subjects with impaired fasting glucose. Eur J Endocrinol. 2014;171(1):137–42.
Zhang T, et al. Complex patterns of circulating fatty acid levels in gestational diabetes mellitus subclasses across pregnancy. Clin Nutr. 2021;40(6):4140–8.
Endocrinology Subgroup and Expert Panel, Chinese Society of Obstetrics and Gyneocology, Chinese Medical Association. Chinese guideline for diagnosis and management of polycystic ovary syndrome. Chin J Obstet Gynecol. 2018;53(1):2–6.
Bao W, et al. Plasma concentrations of lipids during pregnancy and the risk of gestational diabetes mellitus: a longitudinal study. J Diabetes. 2018;10(6):487–95.
Enquobahrie DA, et al. Early pregnancy lipid concentrations and the risk of gestational diabetes mellitus. Diabetes Res Clin Pract. 2005;70(2):134–42.
Sanchez-Vera I, et al. Changes in plasma lipids and increased low-density lipoprotein susceptibility to oxidation in pregnancies complicated by gestational diabetes: consequences of obesity. Metabolism. 2007;56(11):1527–33.
Wang J, Li Z, Lin L. Maternal lipid profiles in women with and without gestational diabetes mellitus. Medicine. 2019;98(16): e15320.
Lee YJ, et al. Perinatal outcome of twin pregnancies according to maternal age. Obstet Gynecol Sci. 2019;62(2):93–102.
Lucovnik M, et al. Impact of pre-gravid body mass index and body mass index change on preeclampsia and gestational diabetes in singleton and twin pregnancies. J Matern Fetal Neonatal Med. 2014;27(18):1901–4.
Wang Y, et al. Absolute risk of adverse obstetric outcomes among twin pregnancies after in vitro fertilization by maternal age. JAMA Netw Open. 2021;4(9): e2123634.
Powe CE, et al. Heterogeneous contribution of insulin sensitivity and secretion defects to gestational diabetes mellitus. Diabetes Care. 2016;39(6):1052–5.
Layton J, et al. Maternal lipid profile differs by gestational diabetes physiologic subtype. Metabolism. 2019;91:39–42.
Elizalde-Barrera CI, et al. Triglycerides and waist to height ratio are more accurate than visceral adiposity and body adiposity index to predict impaired fasting glucose. Diabetes Res Clin Pract. 2019;153:49–54.
Sottero B, et al. Postprandial dysmetabolism and oxidative stress in type 2 diabetes: pathogenetic mechanisms and therapeutic strategies. Med Res Rev. 2015;35(5):968–1031.
Drew BG, et al. High-density lipoprotein modulates glucose metabolism in patients with type 2 diabetes mellitus. Circulation. 2009;119(15):2103–11.
Ferrannini E, et al. The disposal of an oral glucose load in healthy subjects. A quantitative study. Diabetes. 1985;34(6):580–8.
Qiao Q, et al. Predictive properties of impaired glucose tolerance for cardiovascular risk are not explained by the development of overt diabetes during follow-up. Diabetes Care. 2003;26(10):2910–4.
Abdul-Ghani MA, Tripathy D, DeFronzo RA. Contributions of beta-cell dysfunction and insulin resistance to the pathogenesis of impaired glucose tolerance and impaired fasting glucose. Diabetes Care. 2006;29(5):1130–9.
Herrera E, et al. Role of lipoprotein lipase activity on lipoprotein metabolism and the fate of circulating triglycerides in pregnancy. Am J Obstet Gynecol. 1988;158(6 Pt 2):1575–83.
Rizza RA, Mandarino LJ, Gerich JE. Cortisol-induced insulin resistance in man: impaired suppression of glucose production and stimulation of glucose utilization due to a postreceptor detect of insulin action. J Clin Endocrinol Metab. 1982;54(1):131–8.
Perez-Perez A, et al. Leptin and nutrition in gestational diabetes. Nutrients. 2020;12(7):1970.
Retnakaran R, et al. Reduced adiponectin concentration in women with gestational diabetes: a potential factor in progression to type 2 diabetes. Diabetes Care. 2004;27(3):799–800.
Acknowledgements
The authors thank the participants for participating in the study and the medical staff for their work on information collection. We thank American Journal Experts (AJE) for English language editing. This manuscript was edited for English language by AJE.
Funding
This study was supported by National Natural Science Foundation of China (82171671); National Key Research and Development Program of China (2016YFC1000304); Beijing Hospitals Authority’ Ascent Plan (DFL20191402); High-level construction project of public health technical personnel in Beijing Municipal Health System (No. Lingjunrencai-02-02).
Author information
Authors and Affiliations
Contributions
All the authors contributed significantly to the manuscript. KXZ was primarily responsible for the data analysis and writing of the manuscript. WZ and XXY significantly revised the draft, interpreted the data, and involved in data analyses. RHY, YRM, WLH, JHH, KWM, PYZ, LLX, LRZ, XY, TDC and YJZ collected the information and participated in data interpretation. JW involved in the data management and draft revision. GHL was responsible for designing the study and critically revising the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Beijing Obstetrics and Gynecology Hospital (2018-ky-009-01). Written informed consent was obtained from all participants. All procedures were performed in compliance with the Declaration of Helsinki.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Logistics regression analysis of the risk of twin pregnancies GDM based on lipid stratification in the first trimester. Table S2. Logistics regression analysis of the risk of twin pregnancies GDM based on lipid stratification in second trimester.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Zhang, K., Zheng, W., Yuan, X. et al. Association between serum lipid profile during the first and second trimester of pregnancy as well as their dynamic changes and gestational diabetes mellitus in twin pregnancies: a retrospective cohort study. Diabetol Metab Syndr 15, 125 (2023). https://doi.org/10.1186/s13098-023-01095-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-023-01095-w