Abstract
Background
Insulin resistance (IR) was reported to be associated with renal function impairment, but little is known about the gender difference. Hence, our study aimed to investigate the relationship between IR (estimated by the homeostasis model assessment of IR (HOMA-IR) index) and chronic kidney disease (CKD) in a Chinese population with metabolic syndrome (MetS) and discern whether there was any gender disparity or not.
Methods
This retrospective cross-sectional study enrolled 13,638 men and 10,450 women who received health examinations from 2013 to 2016 at Xiamen Chang Gung Hospital. Among the participants, 3,253 men (64.3%) and 1,808 women (35.7%) who had MetS and met the inclusion criteria were included for analysis. Spearman’s correlation was conducted to analyze the relationship between HOMA-IR and cardio-metabolic risk factors. Multivariable linear regression was analyzed to explore the relationship between HOMA-IR and cardio-metabolic variables. Logistic regression analysis was performed to assess the association between HOMA-IR and CKD.
Results
The median HOMA-IR and prevalence of CKD was 2.2 and 11.31%, respectively, for men and 2.09 and 15.93%, respectively, for women. In multivariable linear regression analysis, HOMA-IR was significant associated with estimated GFR, albumin/creatinine ratio in men. Multivariable logistic regression revealed a significant difference between HOMA-IR value and the prevalence of CKD in men but not in women (odds ratio in male = 1.21; 95% CI 1.14–1.28, p ≤ 0.001; odds ratio in female = 1.01; 95% CI 0.99–1.02, p = 0.38).
Conclusions
HOMA-IR was independently associated with CKD among men with MetS but not in women.
Similar content being viewed by others
Background
Chronic kidney disease (CKD) is a worldwide public problem which cause huge economic burden to healthcare systems. CKD is associated to cardiovascular disease (CVD) and an increased risk for all-cause and cardiovascular mortality [1]. The mean (95%CI) global prevalence of CKD was 13.4% (11.7–15.1%) and it increased with age [2]. Sexual dimorphism in kidney disease was noted in previous studies. Arguably, CKD was more prevalent in women than in men [2] but the progression of renal disease is faster in men than in women [3]. However, the role of sex plays in the renal physiology and pathology remains unclear.
Metabolic syndrome (MetS) is a cluster of endogenous risk factors, including atherogenic dyslipidemia, elevated blood pressure (BP), elevated plasma glucose, abdominal obesity, insulin resistance(IR), and is commonly seen in patients with CKD [4, 5]. Patients with MetS are at an increased risk of CKD, atherosclerotic cardiovascular disease and type 2 diabetes mellitus [4, 5].
IR has a strong relationship with MetS [6] and is associated with increased risk for CKD [7, 8]. IR is an early alteration associated with CKD; it is apparent when the glomerular filtration rate (GFR) is still within the normal range [9]. In nondiabetic individuals aged ≥ 20 years, the prevalence and incidence CKD progressively increased with an increase in IR [7, 8]. IR also accelerates progression toward kidney failure [10, 11] by several mechanisms, such as sodium retention, sympathetic nervous system activation, and downregulation of the natriuretic peptide system [9]. Some glucose metabolism biomarkers, such as homeostasis model assessment of IR (HOMA-IR) index, Glycated albumin and Glycated hemoglobin are found associated not only IR but also CKD [7, 12,13,14,15,16].
Therefore, this study aimed to explore the association between IR (estimated by the HOMA-IR index) and CKD, especially about the gender differences, in a relative high risk Chinese population who had MetS.
Materials and methods
Study design and population
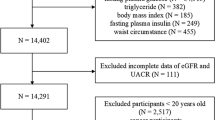
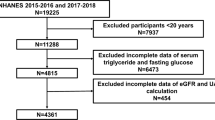
In this cross-sectional study, 13,638 men and 10,450 women (aged ≥ 18 years old) of Chinese ethnicity who received health examinations from 2013 to 2016 at Xiamen Chang Gung Hospital in Xiamen city in China were considered for enrollment. The exclusion criteria were as follows: current pregnancy, incomplete data, CKD stages 4–5, end-stage renal disease, presence of a chronic disease that may affect the metabolic status (e.g., thyroid or hypothalamic disease, chronic hepatitis, cirrhosis, malignant tumor, kidney transplants, severe urinary tract obstruction, renal cancer, and glomerulonephritis), or receiving nephrotoxic agents (e.g., nonsteroidal anti-inflammatory drugs (NSAIDs), aminoglycoside antibiotics, chemotherapeutic agents, nephrotoxic herbal medicine). Participant data were collected from their medical examination records. The study was validated by the Institutional Review Board of Xiamen Chang Gung Hospital.
Data collection and measurement
During the health checkups, well-trained nurses administered a standardized questionnaire to the participants. The questionnaire consisted of information on physiological conditions, medical history, and current medications. Detailed anthropometric measurements was performed, including waist circumference (cm) (WC), body weight (kg), body height (cm) and BP (mmHg). Body height and weight were measured using calibrated meters and scales. Body height was measured without shoes and with the participants standing erect with feet together, looking forward. Body weight was measured with participants wearing light clothing. Body weight was recorded to the 0.1 kg, and body height was measured to the 0.5 cm. Body mass index (BMI) (kg/m2) was calculated as follows: body weight/(height)2. WC was measured between the midpoint of the lowest rib and the iliac crest with feet 25–30 cm apart. BP was measured using a standardized automated sphygmomanometer placed on the participant’s right arm after at least 10 min of rest. Three consecutive measures of BP with an interval of at least 5 min were taken on the same arm. The lowest of the three measurements was collected for the analysis. Mean arterial pressure (MAP) was estimated as (2/3) × diastolic BP + (1/3) × systolic BP.
After at least 12 h of overnight fasting, patients’ venous blood samples were collected for fasting blood glucose (FBG, mmol/L), total cholesterol (TC, mmol/L), high-density lipoprotein cholesterol (HDL-C, mmol/L), low-density lipoprotein cholesterol (LDL-C, mmol/L), triglyceride (TG, mmol/L), serum creatinine (Cr, μmol/L), and insulin (mIU/L), which were determined by enzymatic, spectrophotometric, or colorimetric methods. Urine albumin and creatinine were also measured.
The estimated GFR (eGFR) based on creatinine level was calculated using the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) Equation [17]:
Scr is serum creatinine (mg/dL), κ is 0.7 for females and 0.9 for males, α is −0.329 for females and −0.411 for males, min indicates the minimum of Scr/κ or 1, and max indicates the maximum of Scr/κ or 1.
CKD was staged according to the Kidney Disease Outcomes Quality Initiative (K/DOQI) [18] on the basis of the eGFR and proteinuria measures: stage 1 (eGFR ≥ 90 mL/min/1.73 m2 with albuminuria), stage 2 (eGFR 60–89 mL/min/1.73 m2 with albuminuria), stage 3 (eGFR 30–59 mL/min/1.73 m2), stage 4 (eGFR 15–29 mL/min/1.73 m2), and stage 5 (eGFR < 15 mL/min/1.73 m2). On the basis of the recommended albumin/creatinine ratio (ACR) values, albuminuria was classified as normoalbuminuria (ACR < 30 mg/g Cr), microalbuminuria (ACR 30–299 mg/g Cr), or macroalbuminuria (ACR ≥ 300 mg/g Cr) [19].
According to the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) criteria with modification on WC cutoff for Asian population [4], MetS was defined as the presence of at least three of the following five criteria:
(1) Abdominal obesity (WC ≥ 90 cm for men and ≥ 80 cm for women), (2) high BP (a systolic BP ≥ 130 mmHg or diastolic BP ≥ 85 mmHg, taking antihypertensive drugs, or already diagnosed with hypertension), (3) hyperglycemia (FBG ≥ 5.6 mmol/L, taking antihyperglycemic agents, or diagnosed with diabetes mellitus), (4) decreased HDL-C (< 1.03 mmol/L for men and < 1.29 mmol/L for women or taking hypolipidemic agents), and (5) high serum TG (≥ 1.7 mmol/L or taking drugs used to treat hypertriglyceridemia).
IR was evaluated using the HOMA-IR index, which was calculated as follows: fasting insulin (mIU/L) × FBG (mmol/L)/22.5 [20].
Statistical analysis
The continuous data are shown as medians [Q1, Q3] and compared using Mann–Whitney U test. The categorical data, including albuminuria (ACR ≥ 30 mg/g Cr) and CKD, are shown as n (%) and compared using the Chi-square test. Spearman’s correlation was performed to analyze the correlation between HOMA-IR and cardio-metabolic risk factors. Multivariable linear regression was conducted to explore the relationship between HOMA-IR and cardio-metabolic risk factors (age, the waist-to-height ratio (WHtR), MAP, TG, HDL-C, eGFR, ACR). To investigate the association between cardio-metabolic risk factors which were related to metabolic syndrome (HOMA-IR, age, WC, WHtR, MAP, TG, HDL-C, FBG) and CKD prevalence, logistic regression analyses was conducted with and without covariates adjustment. We did not include WC and FBG into the multivariable logistic regression models due to the high variance inflation factor of WC and WHtR, FBG and HOMA-IR. In our study, a p < 0.05 was considered statistically significant. All statistical analyses were performed using SPSS version 19.0 (SPSS, Inc, Chicago, IL, USA).
Results
Participants’ clinicodemographic characteristics are summarized in Table 1. In all, 24,088 people (13,638 men and 10,450 women) were considered for enrollment; of them, 5,061 who had MetS and met the inclusion criteria were included for analysis. Of the study participants, 3,253 were men (64.3%) and 1,808 were women (35.7%). The median age was 47 years for men and 56 years for women. The median HOMA-IR was 2.20 and 2.09, respectively, and prevalence of CKD was 11.31% and 15.93%, respectively, for men and women. Except WHtR, FBG, TC, LDL-C, all other variables were significantly different between the sexes.
Table 2 revealed the correlation between the HOMA-IR level and cardio-metabolic risk factors. Except HDL-C, HOMA-IR was significant correlated with all the variables in men. In women, HOMA-IR was correlated with age, WC, WHtR, BMI, FBG, TG, HDL-C, insulin and ACR. Significant relationship between HOMA-IR and eGFR was only found in men.
The association of HOMA-IR and seven cardio-metabolic risk factors were shown in Table 3. HOMA-IR was significant associated with age, WHtR*10, eGFR, ACR in men. In women, HOMA-IR was only significant associated with WHtR*10.
Table 4 presented the results of univariate and multivariable logistic analysis of the association between eight risk factors and prevalence of CKD. In men with MetS, the univariate logistic regression model indicated that CKD was significantly associated with all variables The multivariable logistic regression results revealed that except HDL-C, the other five risk factors were significantly associated with the prevalence of CKD. In women with MetS, age, WHtR*10, MAP had a significant association with CKD in both the univariate and multivariable logistic regression analyses.
Discussion
In this community-based and cross-sectional study, we investigated the association between insulin resistance and CKD in a Chinese population with metabolic syndrome, especially about the gender differences. Previous studies reporting that HOMA-IR was associated with CKD and microalbuminuria prevalence [7, 8, 21]. According to NHANES III, in US middle-aged individuals without diabetes, the odds ratio of CKD prevalence increased with HOMA-IR quartiles [7]. In a cohort study including Taiwanese adults aged ≥ 65 years, those in the highest tertile of HOMA-IR had a higher prevalence of CKD compared with those in the lowest tertile (35.9% vs. 12.9%) [8]. Park et al. ‘s study demonstrated that Korean men with highest tertile of HOMA-IR had the highest risk of microalbuminuria [21]. In our multivariable linear regression analysis, HOMA-IR was significant associated with eGFR, ACR in men but not women. Our univariate and multivariable logistic regression analysis also revealed different results between men and women. In men, the prevalence of CKD was significantly associated with age, WHtR*10, MAP, TG and HOMA-IR value. In women, age, WHtR*10, MAP, but not HOMA-IR value were significantly associated with the prevalence of CKD. In the regression models of other studies, HOMA-IR value [8, 22, 23], high BP [8, 22], TG, FBG, low HDL-C level [8], and older age [22] were significantly associated with an increased odds ratio of CKD. In our study, HOMA-IR value had a significant association with eGFR, ACR and the prevalence of CKD only in men. Our result was similar to a Turkish study which showed that HOMA-IR was associated with a reduced eGFR in men, and the result was not present in women [24]. Zhao et al. performed a Mendelian randomization study and had the findings that fasting insulin was sex-specifically associated with CKD and unfavorable kidney function in men but not in women [25]. The sex-specific association of HOMA-IR and ACR was also demonstrated in studies on healthy Japanese adults and Caucasian adults with type 2 diabetes [26, 27]. We also observed that TG was significantly associated with CKD only in men. The result was similar to another Chinese study which Zhang et al. found that TG was associated with an increased risk of CKD only in male participants [28].
The sex disparity might be due to the involvement of sex hormones [29]. Estrogen has a favorable effect on insulin sensitivity; indeed, insulin sensitivity decreases after menopause and improves with hormone replacement therapy. The possible mechanisms include direct effects on insulin on glucose homeostasis, body composition, adipose tissue metabolism and distribution and proinflammatory markers. Other hormones related to IR include androgens, adiponectin, and dehydroepiandrosterone (DHEA) [29]. Sex hormones and their receptors also play a vital role in kidney injury and progression of renal disease. They have beneficial (mainly estrogens) or harmful (mainly androgens) effects through mechanisms such as oxidative stress, the renin–angiotensin system, inflammation, and fibrosis [3, 30]. Estrogen also prevents vascular injuries through direct and indirect action [31]. The aforementioned pathophysiological differences due to sex hormones may have cause the sex differences observed in our study and related studies.
Our study demonstrated that WHtR had higher OR than WC for CKD in both sexes. The result was similar with previous studies [32, 33]. WHtR is considered to be an indicator of central obesity. It corresponds to intraabdominal fat levels in computed tomography scan assessments [34]. Ashwell et al. strongly supported the use of WHtR as an index for obesity [35]. Many studies have demonstrated that WHtR had the highest association with cardiovascular disease risk factors [36]. Although obesity has been indicated to contribute to CKD and renal function decline in several studies [37,38,39], the pathophysiological mechanisms underlying this association have not been fully elucidated. Obesity has direct and indirect effects on the kidney disease. Obesity may indirectly promote CKD by increasing the risk of type 2 diabetes, hypertension, and atherosclerosis [40]. The direct pathogenesis includes renal hemodynamics change, increased inflammatory cytokines, altered adipokines, and increased growth factor [40,41,42,43,44]. Excess adiposity results in glomerular hyperfiltration, hypertrophy, and hypertension, leading to subsequent glomerulosclerosis and proteinuria. Excess adiposity also stimulates the production of proinflammatory and proatherogenic cytokines, such as Tumor Necrosis Factor -α and Interleukin-6, which are involved in CKD development. Adipose tissue secretes adipokines, including angiopoietins, vascular endothelial growth factor, cathepsins, leptin, adiponectin, and resistin. The alterations in the levels of adipokines, especially high leptin and low adiponectin levels, contribute to oxidative stress, increase sympathetic nervous system activity, cellular hypertrophy, extracellular matrix accumulation, proteinuria, and renal fibrosis.
Strengths
First, our study analyzed a large, population-based sample, which gave high credibility to the results. The result also provided epidemiological data for CKD prevalence in the South China area. Second, we used the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation to estimate GFR, which was more accurate than the Modification of Diet in Renal Disease Study (MDRD) equation [17].
Limitations
Our study had some limitations. First, this is a cross-sectional design which is unable to investigate the causal relationship. Second, we did not consider menopausal status, so the influence of female hormones on renal function could not be investigated. We could not analyze the data in premenopausal and menopausal subgroups. Third, we used the HOMA-IR value instead of the hyperinsulinemic-euglycemic glucose clamp (HEGC) technique to estimate IR. Some studies have demonstrated that the HOMA-IR was not appropriate in participants with severely impaired or absent β-cell function [45].
Conclusion
Our research adds to the growing evidence of gender differences in the associations between insulin resistance and CKD in population with metabolic syndrome. We found that HOMA-IR value was independently associated with CKD among men but not in women. These findings suggest that we should carefully evaluate the renal function progression for at-risk individuals with higher HOMA-IR value, particularly in men. Longitudinal studies in different populations and age groups are needed to prove our findings.
Availability of data and materials
The data analyzed in the present study are available from the corresponding author upon reasonable request.
References
Tonelli M, Wiebe N, Culleton B, House A, Rabbat C, Fok M, et al. Chronic kidney disease and mortality risk: a systematic review. J Am Soc Nephrol. 2006;17(7):2034–47.
Hill NR, Fatoba ST, Oke JL, Hirst JA, O’Callaghan CA, Lasserson DS, et al. Global prevalence of chronic kidney disease—a systematic review and meta-analysis. PLoS ONE. 2016;11(7):e0158765.
Neugarten J, Golestaneh L. Influence of sex on the progression of chronic kidney disease. Mayo Clin Proc. 2019;94(7):1339–56.
Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, et al. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute Scientific Statement. Circulation. 2005;112(17):2735–52.
Zhang X, Lerman LO. The metabolic syndrome and chronic kidney disease. Transl Res. 2017;183:14–25.
Roberts CK, Hevener AL, Barnard RJ. Metabolic syndrome and insulin resistance: underlying causes and modification by exercise training. Compr Physiol. 2013;3(1):1–58.
Chen J, Muntner P, Hamm LL, Fonseca V, Batuman V, Whelton PK, et al. Insulin resistance and risk of chronic kidney disease in nondiabetic US adults. J Am Soc Nephrol. 2003;14(2):469–77.
Cheng HT, Huang JW, Chiang CK, Yen CJ, Hung KY, Wu KD. Metabolic syndrome and insulin resistance as risk factors for development of chronic kidney disease and rapid decline in renal function in elderly. J Clin Endocrinol Metab. 2012;97(4):1268–76.
Spoto B, Pisano A, Zoccali C. Insulin resistance in chronic kidney disease: a systematic review. Am J Physiol Renal Physiol. 2016;311(6):F1087–108.
Caravaca F, Cerezo I, Macías R, de García VE, del Martínez VC, Villa J, et al. Insulin resistance in chronic kidney disease: its clinical characteristics and prognosis significance. Nefrologia. 2010;30(6):661–8.
Kobayashi H, Tokudome G, Hara Y, Sugano N, Endo S, Suetsugu Y, et al. Insulin resistance is a risk factor for the progression of chronic kidney disease. Clin Nephrol. 2009;71(6):643–51.
Kang SH, Jung DJ, Choi EW, Cho KH, Park JW, Do JY. HbA1c levels are associated with chronic kidney disease in a non-diabetic adult population: a nationwide survey (KNHANES 2011–2013). PLoS ONE. 2015;10(12):e0145827.
Giglio RV, Lo Sasso B, Agnello L, Bivona G, Maniscalco R, Ligi D, et al. Recent updates and advances in the use of glycated albumin for the diagnosis and monitoring of diabetes and renal, cerebro- and cardio-metabolic diseases. J Clin Med. 2020;9(11):3634.
Bellia C, Cosma C, Lo Sasso B, Bivona G, Agnello L, Zaninotto M, et al. Glycated albumin as a glycaemic marker in patients with advanced chronic kidney disease and anaemia: a preliminary report. Scand J Clin Lab Invest. 2019;79(5):293–7.
Bellia C, Zaninotto M, Cosma C, Agnello L, Bivona G, Marinova M, et al. Clinical usefulness of glycated albumin in the diagnosis of diabetes: results from an Italian study. Clin Biochem. 2018;54:68–72.
Agnello L, Lo Sasso B, Scazzone C, Giglio RV, Gambino CM, Bivona G, et al. Preliminary reference intervals of glycated albumin in healthy caucasian pregnant women. Clin Chim Acta. 2021;519:227–30.
Levey AS, Stevens LA, Schmid CH, Zhang YL, Castro AF 3rd, Feldman HI, et al. A new equation to estimate glomerular filtration rate. Ann Intern Med. 2009;150(9):604–12.
Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, et al. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139(2):137–47.
Keane WF, Eknoyan G. Proteinuria, albuminuria, risk, assessment, detection, elimination (PARADE): a position paper of the National Kidney Foundation. Am J Kidney Dis. 1999;33(5):1004–10.
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC. Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia. 1985;28(7):412–9.
Park SK, Chun H, Ryoo JH, Lee SW, Lee HS, Shim KW, et al. A cohort study of incident microalbuminuria in relation to HOMA-IR in Korean men. Clin Chim Acta. 2015;446:111–6.
Gu DF, Shi YL, Chen YM, Liu HM, Ding YN, Liu XY, et al. Prevalence of chronic kidney disease and prediabetes and associated risk factors: a community-based screening in Zhuhai. Southern China Chin Med J (Engl). 2013;126(7):1213–9.
Markus MRP, Ittermann T, Baumeister SE, Huth C, Thorand B, Herder C, et al. Prediabetes is associated with microalbuminuria, reduced kidney function and chronic kidney disease in the general population: the KORA (Cooperative Health Research in the Augsburg Region) F4-Study. Nutr Metab Cardiovasc Dis. 2018;28(3):234–42.
Onat A, Hergenç G, Uyarel H, Ozhan H, Esen AM, Karabulut A, et al. Association between mild renal dysfunction and insulin resistance or metabolic syndrome in a random nondiabetic population sample. Kidney Blood Press Res. 2007;30(2):88–96.
Zhao JV, Schooling CM. Sex-specific associations of insulin resistance with chronic kidney disease and kidney function: a bi-directional Mendelian randomisation study. Diabetologia. 2020;63(8):1554–63.
De Cosmo S, Minenna A, Ludovico O, Mastroianno S, Di Giorgio A, Pirro L, et al. Increased urinary albumin excretion, insulin resistance, and related cardiovascular risk factors in patients with type 2 diabetes: evidence of a sex-specific association. Diabetes Care. 2005;28(4):910–5.
Utsunomiya K, Takamatsu K, Fukuta I, Sakamoto H, Ishizawa S, Kanazawa Y, et al. Association of urinary albumin excretion with insulin resistance in Japanese subjects: impact of gender difference on insulin resistance. Intern Med. 2009;48(18):1621–7.
Zhang L, Yuan Z, Chen W, Chen S, Liu X, Liang Y, et al. Serum lipid profiles, lipid ratios and chronic kidney disease in a Chinese population. Int J Environ Res Public Health. 2014;11(8):7622–35.
Geer EB, Shen W. Gender differences in insulin resistance, body composition, and energy balance. Gend Med. 2009;6:60–75.
Valdivielso JM, Jacobs-Cachá C, Soler MJ. Sex hormones and their influence on chronic kidney disease. Curr Opin Nephrol Hypertens. 2019;28(1):1–9.
Mendelsohn ME. Protective effects of estrogen on the cardiovascular system. Am J Cardiol. 2002;89(12a):12E-7E.
He Y, Li F, Wang F, Ma X, Zhao X, Zeng Q. The association of chronic kidney disease and waist circumference and waist-to-height ratio in Chinese urban adults. Medicine (Baltimore). 2016;95(25):e3769.
Lin CH, Chou CY, Lin CC, Huang CC, Liu CS, Lai SW. Waist-to-height ratio is the best index of obesity in association with chronic kidney disease. Nutrition. 2007;23(11–12):788–93.
Ashwell M, Cole TJ, Dixon AK. Ratio of waist circumference to height is strong predictor of intra-abdominal fat. BMJ. 1996;313(7056):559–60.
Ashwell M, Hsieh SD. Six reasons why the waist-to-height ratio is a rapid and effective global indicator for health risks of obesity and how its use could simplify the international public health message on obesity. Int J Food Sci Nutr. 2005;56(5):303–7.
Browning LM, Hsieh SD, Ashwell M. A systematic review of waist-to-height ratio as a screening tool for the prediction of cardiovascular disease and diabetes: 0·5 could be a suitable global boundary value. Nutr Res Rev. 2010;23(2):247–69.
Ferris M, Hogan SL, Chin H, Shoham DA, Gipson DS, Gibson K, et al. Obesity, albuminuria, and urinalysis findings in US young adults from the Add Health Wave III study. Clin J Am Soc Nephrol. 2007;2(6):1207–14.
Ejerblad E, Fored CM, Lindblad P, Fryzek J, McLaughlin JK, Nyrén O. Obesity and risk for chronic renal failure. J Am Soc Nephrol. 2006;17(6):1695–702.
Wang Y, Chen X, Song Y, Caballero B, Cheskin LJ. Association between obesity and kidney disease: a systematic review and meta-analysis. Kidney Int. 2008;73(1):19–33.
Stenvinkel P, Zoccali C, Ikizler TA. Obesity in CKD–what should nephrologists know? J Am Soc Nephrol. 2013;24(11):1727–36.
Rhee CM, Ahmadi SF, Kalantar-Zadeh K. The dual roles of obesity in chronic kidney disease: a review of the current literature. Curr Opin Nephrol Hypertens. 2016;25(3):208–16.
Mathew AV, Okada S, Sharma K. Obesity related kidney disease. Curr Diabetes Rev. 2011;7(1):41–9.
D’Agati VD, Chagnac A, de Vries AP, Levi M, Porrini E, Herman-Edelstein M, et al. Obesity-related glomerulopathy: clinical and pathologic characteristics and pathogenesis. Nat Rev Nephrol. 2016;12(8):453–71.
Jung UJ, Choi MS. Obesity and its metabolic complications: the role of adipokines and the relationship between obesity, inflammation, insulin resistance, dyslipidemia and nonalcoholic fatty liver disease. Int J Mol Sci. 2014;15(4):6184–223.
Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008;294(1):E15-26.
Acknowledgements
The authors are deeply grateful to all study participants and the staff of Xiamen Chang Gung Hospital who assisted with this study. The study would not have been possible without their help.
Funding
The authors did not receive any specific funding for this study.
Author information
Authors and Affiliations
Contributions
Conceptualization, WCL; methodology, WCL; data collection, WY, HYH, XJX; software, JYC; validation, JYC; formal analysis, JYC; investigation, CAL and JYC; resources, JYC; data curation, CAL and JYC; writing—original draft preparation, CAL; writing—review and editing, CAL; visualization, JYC; supervision, WCL and JYC; project administration, SYL, YCC, and JYC. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study was approved by the Institutional Review Board of Xiamen Chang Gung Hospital (reference number: XMCGIRB2020003).
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Lin, CA., Li, WC., Lin, SY. et al. Gender differences in the association between insulin resistance and chronic kidney disease in a Chinese population with metabolic syndrome. Diabetol Metab Syndr 14, 184 (2022). https://doi.org/10.1186/s13098-022-00956-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00956-0