Abstract
Background
There is an increased burden of diabetes globally including in sub-Saharan Africa. The literature shows that glycaemic control among type 2 diabetes patients is poor in most countries in sub-Saharan Africa. Understanding the factors influencing glycaemic control in this region is therefore important to develop interventions to optimize glycaemic control. We carried out a systematic review to determine the prevalence and factors associated with glycaemic control in sub-Saharan Africa to inform the development of a glycaemic control framework in the Democratic Republic of the Congo.
Methods
We searched five databases (African Index Medicus, Africa-Wide Information, Global Health, PubMed, and Web of Science) using the following search terms: type-2 diabetes, glycaemic control, and sub-Saharan Africa. Only peer-reviewed articles from January 2012 to May 2022 were eligible for this review. Two reviewers, independently, selected articles, assessed their methodological quality using Joanna Briggs checklists, and extracted data. A meta-analysis was performed to estimate the prevalence of glycaemic control. Factors associated with glycaemic control were presented as a narrative synthesis due to heterogeneity as assessed by the I2.
Results
A total of 74 studies, involving 21,133 participants were included in the review. The pooled prevalence of good glycaemic control was 30% (95% CI:27.6–32.9). The glycaemic control prevalence ranged from 10–60%. Younger and older age, gender, lower income, absence of health insurance, low level of education, place of residence, family history of diabetes, longer duration of diabetes, pill burden, treatment regimen, side effects, use of statins or antihypertensives, alcohol consumption, smoking, presence of comorbidities/complications, and poor management were associated with poor glycaemic control. On the other hand, positive perceived family support, adequate coping strategies, high diabetes health literacy, dietary adherence, exercise practice, attendance to follow-up, and medication adherence were associated with good glycaemic control.
Conclusion
Suboptimal glycaemic control is pervasive among patients with type-2 diabetes in sub-Saharan Africa and poses a significant public health challenge. While urgent interventions are required to optimize glycaemic control in this region, these should consider sociodemographic, lifestyle, clinical, and treatment-related factors. This systematic review and meta-analysis protocol is registered in PROSPERO under CRD 42021237941.
Similar content being viewed by others
Background
The prevalence of type 2 diabetes mellitus has been increasing worldwide, with low and middle-income countries bearing the brunt of this growth in terms of morbidity, mortality, and economic costs [1, 2]. As such, Africa has been experiencing the greatest increase of all the World Health Organization (WHO) regions. The epidemiological transition due to the adoption of the Western lifestyle and urbanization, among other things, has played a major role in the progression of diabetes [3]. The growing burden of diabetes has been a barrier to the wellness of families and the effectiveness of the health system.
One of the main goals of diabetes mellitus management is to achieve glycaemic control to delay or prevent the onset of diabetes complications. Worldwide, only approximately 50% of patients achieve glycaemic control [4] and in sub-Saharan Africa (SSA), glycaemic control rates are generally poor. In sub-Saharan Africa, the proper management of diabetes faces numerous challenges including inadequate resources, coexisting traditional health priorities, ill-preparedness for chronic disease management and low health insurance coverage [5].
Glycaemic control represents an emergency to alleviate the burden of the disease in sub-Saharan Africa [6]. The design and implementation of effective glycaemic control strategies require accurate knowledge of the factors underlying glycaemic control to enable the identification of effective interventions. The factors associated with poor glycaemic control are numerous and vary in importance depending on the population [7, 8]. Empirical evidence suggests that higher socioeconomic status, greater dietary knowledge, and higher self-efficacy and empowerment improve glycaemic control [9]. Factors driving poor glycaemic control include patients, diabetes disease, treatment, health system, and physician-related factors [8, 10]. However, there is a paucity of literature on factors that influence glycaemic control in the sub-Saharan region. Therefore, this systematic review aims to determine the prevalence and factors associated with glycaemic control among type 2 diabetes patients in sub-Saharan Africa. The review will comprise all articles on glycaemic control among patients with type 2 diabetes from January 2012 to May 2022 to have enough studies to have a broad view of the phenomenon.
Methods
The protocol of this systematic review and meta-analysis was registered on PROSPERO with reference CRD 41021237941. The Preferred Reporting Items for Systematic reviews and Meta-Analyses (PRISMA) guidelines were used to report the entire process of this systematic review [11].
Eligibility criteria
Eligible studies were those that reported glycaemic control in persons with type 2 diabetes mellitus in sub-Saharan Africa. Only peer-reviewed articles were eligible to ensure the inclusion of valid research and avoid falsified data. Data from January 2012 to May 2022 without language restrictions were included. As we planned to estimate the prevalence and identify factors associated with glycaemic control, the following types of study designs were considered: randomized controlled trials, quasi-experimental trials, cohort studies, case–control studies, and cross-sectional studies. Only studies that reported a multivariate analysis were included in the systematic review.
Information sources
The search was conducted in five databases: African Index Medicus, Africa-Wide Information, Global Health, PubMed, and Web of Science. In addition, the reference lists of the selected articles were reviewed for any other eligible articles. The last search date was 02 May 2022.
Search strategy
The search term domains were “Type 2 diabetes mellitus”, “glycaemic control”, and “sub-Saharan Africa”. Additional file 1: Table S1 presents the search strategy at the level of the five databases.
Selection process
Two investigators (JPF and JMF) independently reviewed the studies using the eligibility criteria and selected studies for inclusion in the review. The first investigator (JPF) reviewed all articles, and the second investigator (JMF) randomly assessed 10% of the selected articles. Differences in selection were assessed by consensus. The software used for the selection and recording of decisions was EndNote 20.
Data extraction
Data from eligible studies were captured using a Microsoft Excel file. The first investigator (JPF) performed data extraction on all the articles and the second investigator (JMF) randomly assessed 10% of the extracted information. Any differences of opinion between individual judgments were resolved through consensus. For the metaanalysis of the proportions of glycaemic control, we contacted eight authors for missing information and clarification. One provided us with its study dataset, and another showed us how to access the information needed to calculate the glycaemic control.
Study variables
Main outcomes
Reported glycaemic control: pooled prevalence of samples reported to have glycaemic control.
Exposure: reported independent risk factors for glycaemic control.
Data items
The following information was extracted from the studies: the last name of the first author, study type, publication year, country, study population, total sample size, glycaemic level assessment method, glycaemic control definition, number or proportion of persons with good glycaemic control, factors associated with glycaemic control, and measure of association for glycaemic control.
Study risk of bias assessment
The assessment of the methodological quality of the selected studies was performed by two reviewers (JPF and JMF) using the Joanna Briggs Institute Critical Appraisal Tools [12]; any differences of opinion between the two reviewers were resolved by consensus. The Joanna Briggs Institute Critical Appraisal Tools were used to classify each selected study as good, moderate, or poor regarding the risk of bias. The percentage of "Yes" votes was equal to or less than 50%, 51–80%, and more than 80% for poor, moderate, or good quality respectively [13]. The assessment of an item was marked "Yes" if the description met the criteria set for the assessment, otherwise, the assessment was "No". If the description was insufficient, the assessment was "Unknown".
Synthesis methods
To estimate the overall prevalence of glycaemic control, we carried out a meta-analysis with the random-effects model of the proportions of good glycaemic control. The statistical software used was Stata 17.0 [14]. The data needed for analysis are summarized in Additional file 3: Table S3. Only 51 studies were eligible for the estimation of the prevalence of glycaemic control as randomized control trials, quasi-experimental and case–control studies were excluded. We observed high heterogeneity of the studies as shown by the I2 [15], and therefore reported the pooled prevalence estimate and the glycaemic control patterns in sub-Saharan Africa. Forest plots were used to visually display the results of individual studies and the syntheses. We explored heterogeneity by performing subgroups analysis of the prevalence by region of sub-Saharan Africa (Eastern, Western, Central, Southern), study type (case–control, cohort, cross-sectional, quasi-experimental, randomized control trial), and method (glycosylated haemoglobin, glycaemia) used to assess the control.
To assess the factors driving glycaemic control, due to the heterogeneity of the studies, we performed a narrative synthesis of reported factors. Each reported factor is presented with the studies in which it was assessed, and the measure of association —and its 95% confidence interval—with glycaemic control found in each study is reported. The factors were categorized into six groups: sociodemographic, lifestyle, clinical, treatment modalities, adherence, and interventions.
Results
Study selection
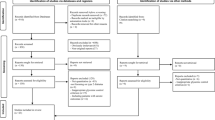
We retrieved 6656 publications from the information sources. A total of 105 publications were removed due to duplication. Of the remaining 6551 articles, 6425 were excluded after the titles and abstracts were reviewed, and 126 were retained for full-text evaluation based on the inclusion criteria. Of the 126, eighty-three articles were excluded after full-text review and 43 articles were retained. An additional search of the reference lists of selected articles yielded 2623 publications. We selected 53 publications for full-text evaluation according to the selection criteria. Of these, 22 were excluded because they did not meet inclusion criteria, and 31 articles were retained. The total number of included studies was 74 articles by both search strategies. The selection process is summarized in the PRISMA flow diagram (Fig. 1). The characteristics of the excluded studies and the reason(s) for exclusion are summarized in Additional file 2: Table S2.
General characteristics of the included studies
A total of 74 studies reporting on 21,133 patients with type 2 diabetes were included in the review. The studies were conducted in 16 sub-Saharan African countries, with Ethiopia (n = 26, 35.1%) being the most represented, followed by South Africa (n = 11, 14.9%) and Nigeria (n = 10, 13.5%). The majority of the studies (n = 51, 68.9%) were conducted in the last five years (2017-2022). Of the 74 studies selected, 55 (74.3%) were cross-sectional studies, ten (13.5%) were randomized controlled studies, four (5.4%) were quasi-experimental studies, three (4.1%) were case–control studies, and two (2.7%) were cohort studies. The general characteristics of the included studies are presented in Table 1.
Assessment of risk of bias
Of the 74 studies selected for the review, only 14 (18.9%) were assessed as being of good quality, 54 (73.0%) were of moderate quality, and six (8.1%) were of poor quality. Additional file 4: Tables S4, Additional file 5: Table S5, Additional file 6: Table S6, Additional file 7: Table S7, Additional file 8: Table S8, Additional file 9 detail the assessment of study methodological quality. Of the 55 cross-sectional studies, only four (7.3%) were able to formally identify confounding factors, while ten (1 8.2%) reported the method used to address confounding factors. In the four quasi-experimental studies, one study (25.0%) did not measure the outcomes consistently or in a reproducible way. In two of the ten randomized controlled trials (20.0%), participants and treatment providers were not blinded to treatment allocation nor were the staff members assessing outcomes blinded to treatment allocation. Moreover, for one of these two studies, the treatment groups were not similar at baseline. For two of the three case–control studies, confounding factors were not identified, and for one study, cases and controls were mismatched.
Assessment of glycaemic control
Glycaemic control was assessed by glycosylated haemoglobin in 43(58.1%) studies, fasting blood glucose in 25 (33.8%) studies and a combination of both methods in 6(8.1%) studies. The cut-off points for good glycaemic control varied across studies and were: HbA1c < 7%, HbA1c ≤ 7%, HbA1c < 8%, HbA1c < 53 mmol/mol, FBG: 70–130 mg/dL, FBG < 126 mg/dL, FBG ≤ 126 mg/dL, FBG: 70–130 mg/dL, FBG < 154 mg/dL, FBS ≤ 130 mg/dl, FPG: 100–130 mg/dL, FBG: 4–7 mmol/L, FBG ≤ 130 mg/dL or 7. 2 mmol/L.
Prevalence of glycaemic control
The estimated pooled prevalence of good glycaemic control in sub-Saharan Africa was 30.3% (95% CI: 27.6–32.9). The analysis showed considerable heterogeneity (I2: 93.9%, p < 0.001), and glycaemic control prevalence ranged from 10 to 60% (Fig. 2). The subgroup analysis by region showed that most of the studies in the Central (n = 5, 83.3%) and the Southern (n = 5, 62.5%) regions had a prevalence of glycaemic control of < 30% while most of the studies in the Eastern region had a prevalence of glycaemic control > 30% (Fig. 3).
Factors associated with glycaemic control
The reported sociodemographic, lifestyle, clinical, adherence, treatment factors, and reported glycaemic control optimization interventions factors are summarized in Tables 2, 3, 4, 5, 6, 7.
Sociodemographic characteristics
Table 2 presents the sociodemographic factors with respect to their relationship with glycaemic control. Five studies assessed the relationship between increasing age and glycaemic control [27, 31, 34, 58, 61], two found that it was negatively associated with glycosylated haemoglobin [31, 61], and one found that it was associated with good glycaemic control [57]. Older age was associated with poor glycaemic control in twelve studies [22, 29, 32, 36, 39, 65, 68, 69, 73, 77, 83, 86]. Eight studies assessed the relationship between the female gender and glycaemic control [18, 29, 34, 51, 61, 64, 65, 73], two studies found that the female gender was significantly associated with poor glycaemic control [18, 34], and one study linked it to good glycaemic control [28]. Male gender with respect to glycaemic control was assessed by eleven studies [27, 31, 39, 44, 58, 66, 75, 77, 83, 85, 87]; two studies associated it with good glycaemic control [58, 75], while two studies linked it to poor glycaemic control [27, 87]. Fifteen studies assessed the relationship between educational level and glycaemic control; in one study, primary, secondary, or tertiary education levels were associated with good glycaemic control [28]. A lack of formal education and a low level of education were associated with poor glycaemic control in three studies [39, 48, 87]. In respectively two studies, low monthly income [18, 87], absence of health insurance [47, 58], and being a farmer [25, 48] were associated with poor glycaemic control. In respectively one study, living in urban areas [49], and a high frequency of seeking traditional medicine practitioners [30] were associated with poor glycaemic control. Residing less than 100 kms from a health facility [25], residing in Guinea compared to residing in Cameroon [32], self-reporting a positive perception of family support [68], and the frequency of participating in religious activities [31] were associated with good glycaemic control in respectively one study.
Lifestyle factors
The lifestyle factors assessed were dietary adherence, the practice of exercise, smoking, and alcohol consumption (Table 3). Good dietary adherence was associated with good glycaemic control in five studies [29, 36, 40, 61, 86] while low adherence to dietary recommendations was associated with poor glycaemic control in two studies [35, 67]. Exercise was associated with good glycaemic control in two studies [29, 36]. The inadequate practice of exercise was associated with poor glycaemic control in two studies [39, 53]. In respectively one study, smoking [39], and alcohol consumption [29] were associated with poor glycaemic control.
Clinical factors
The clinical factors—history of diabetes and comorbidities—with respect to glycaemic control are summarized in Table 4. A family history of diabetes was significantly associated with poor glycaemic control in one study [80]. A long duration of diabetes was associated with poor glycaemic control in seven studies [18, 26, 27, 32, 58, 61]. As a corollary, treatment of > 10 years was associated with poor glycaemic in one study [38]. In one study, patients who always had fluctuating/unstable blood glucose levels or had blood glucose levels not improved from diagnosis were prone to poor glycaemic control [60].
Four studies found that the presence of comorbidities was associated with poor glycaemic control [53, 75, 77, 87]. The presence of hypertension led to poor glycaemic control in one study [16]. Dyslipidaemia was associated with poor glycaemic control in three studies [18, 53, 82]. Concerning body mass index (BMI), all categories, such as being underweight [60], having a normal BMI [46], or being overweight/obese [18, 34, 87] have been significantly associated with poor glycaemic control. Central obesity was associated with poor glycaemic control in four studies [16, 30, 52, 56]. In respectively one study, the presence of anaemia [17], non-alcoholic fatty liver disease [19], vitamin B12 deficiency [20], metabolic syndrome [28], cognitive impairment [32], congestive cardiac failure [46], HIV infection [46], thyroid autoimmunity [74], and hypogonadism [45] had a significant association with poor glycaemic control. The presence of peripheral neuropathy [83] or a high-level tooth mobility index [59] was associated with poor glycaemic control. Overall health-related quality of life was inversely associated with FBG [42]. The global disability burden was significantly associated with poor glycaemic control [70]. A unit reduction in the estimated glomerular filtration rate (eGFR) was also associated with HbA1c ≥ 7% [16].
Adherence to treatment plans
Adherence modalities, as represented by adherence to scheduled appointments or medication adherence, are presented in Table 5. Regular attendance at scheduled appointments was associated with good glycaemic control in two studies [49, 85]. Good medication adherence was associated with good glycaemic control in two studies [40, 77], while two other studies showed no association [75, 78]. Low medication adherence had a significant association with poor glycaemic control in three studies [33, 48, 86]. Medium medication adherence was associated with poor glycaemic control in one study [48].
Treatment modalities
The findings on the treatment modalities with respect to glycaemic control are summarized in Table 6. The pill burden was associated with poor glycaemic control in one study. Combination therapy with oral hypoglycaemic agents (OHA) was associated with poor glycaemic control in two studies [48, 53] while it was linked to good glycaemic control in one study [75]. Insulin plus OHA was associated with poor glycaemic control in three studies [44, 48, 69], while it was linked to good glycaemic control in one study [75]. The use of insulin alone was associated with poor glycaemic control in two studies [53, 78]. The presence of drug-related problems was associated with poor glycaemic control as shown in one study [86]. Rwegerera et al. found that being on diet and OHA was associated with suboptimal glycaemic control [73]. A South African study found that the use of statin and antihypertensives was associated with higher glycaemic levels [50]. Non-surgical periodontal management was associated with good glycaemic control after three months in one study [82]. Diabetes information from non-health workers was significantly associated with poor glycaemic control [18], while having a high diabetes health literacy [77] was significantly associated with good glycaemic control. In one study, the absence of clarity in pharmacists’ advice was associated with poor glycaemic control [44].
Reported glycaemic control optimization interventions
The interventions retrieved from the included studies are presented along with their effect on glycaemic control in Table 7. Only one study [43] out of five reported an educational program associated with good glycaemic control. None of the self-management programs was associated with glycaemic control as found in three studies [40, 61, 62]. All exercise programs were associated with improved glycaemic control as found in four studies [37, 38, 52, 76, 84]. Adding a second OHA was associated with poor glycaemic control in one study [49]. The effectiveness of a community-based multilevel peer support intervention was associated with a significant reduction in glycosylated haemoglobin in the intervention group in one study [24].
Discussion
We sought to determine the prevalence and factors associated with glycaemic control in sub-Saharan Africa (SSA) in the past 10 years (2012–2022). Our review shows that poor glycaemic control is common in SSA with only 10–60% of patients having optimal glycaemic control. In addition, glycaemic control was associated with sociodemographic factors (younger and older age, gender, lower income, absence of health insurance, low level of education, place of residence, family support, coping strategies), lifestyle (dietary adherence, practice of exercise, smoking, alcohol consumption), clinical factors (family history of diabetes, longer duration of diabetes, presence of comorbidities/complications), adherence (adhering to follow-up appointments and medication), treatment modalities (pill burden, treatment regimen, use of statins or anti-hypertensives, drug-related problems, diabetes information from non-health workers, high diabetes health literacy, absence of clarity in pharmacists’ advice, failure to set glycaemic goals), and reported glycaemic control optimization interventions.
The assessment of glycaemic control was variable in the studies included in our review; in only 43 (58.1%) studies, glycosylated haemoglobin was used. This renders it difficult to estimate the real extent of glycaemic control, compare the results and, even in daily clinical practice, manage patients [90]. Nevertheless, our estimated prevalence of good glycaemic control in SSA is similar to the prevalence found by a meta-analysis in Ethiopia in which only one-third of patients were adequately controlled [90] and in a study in Central, East and West Africa with approximately 29% of good glycaemic control [91]. The prevalence of poor glycaemic control in sub-Saharan Africa is far lower than that found in eight European countries by The Panorama study (62.6%) [10], and in the United States of America by Fang and colleagues (55.3%) in 2015–2018 [92]. The poor glycaemic control in sub-Saharan Africa is the result of poor quality of diabetes care due, in turn, to a weak disease management framework and fragmented health systems [93]. Changes are required in the organization of healthcare systems in sub-Saharan African countries for better management of non-communicable diseases in general, with effective implementation of diabetes care into primary care [4, 93].
Several studies have reported significant associations between sociodemographic factors and glycaemic control. Advancing in age was negatively associated with poor glycaemic control, indicating the vulnerability of young patients as found by several studies [93]. Young patients are confronted with many barriers to effective self-management. Older age was associated with poor glycaemic control in our review, corroborating the findings of several studies and explained by insulin resistance and the presence of comorbidities [8, 90, 95]. Although both genders were linked to poor and good glycaemic control in our review, it is recognized that women are traditionally prone to poor glycaemic control [96]. Women with type 2 diabetes in sub-Saharan Africa have a greater risk of death due to poor access to care [97]. Thus, young, and older patients along with women represented vulnerable categories, in terms of propensity to poor glycaemic control and issues of accessing care. Caution must be taken when managing diabetes in sub-Saharan Africa to ease access to care and provide adequate responses to the needs of these categories.
Poor socioeconomic conditions (low income, poor education) have been associated with poor glycaemic control due to poor access to adequate care and poor health-seeking behaviors [18, 48, 87, 98, 99]. Increasing universal health coverage could address these problems and lead to better outcomes [100]. Factors such as food insecurity and depression have been identified as mediators in the relationship between poor living conditions and glycaemic control [98]. Family support and adequate coping strategies such as participation in religious activities were beneficial for glycaemic control and could act through these mediating factors. Management interventions to optimize glycaemic control for patients with type 2 diabetes with poor socioeconomic conditions should consider these interconnected factors.
A long distance from home to the healthcare facility has been associated with poor glycaemic control while having less distance was found to be beneficial in many studies, as the latter favors access, adherence and monitoring of care [101, 102]. However, for the nearness of health facilities to have a meaningful impact, these facilities must have adequate equipment, and trained personnel for diabetes care [32].
As expected, adherence to dietary recommendations and physical exercise have been associated with good glycaemic control [103, 104]. In our review smoking was associated with poor glycaemic control. The literature shows that smoking has a confusing relationship with poor glycaemic control [104]. Indeed, if smoking was related to poor glycaemic control due to reduced effectiveness of insulin, quitting smoking has also been linked to poorer glycaemic control [106, 107]. Nevertheless, smoking cessation is one goal of diabetes care. One study in our review linked patients who ever drunk alcohol regularly to poor glycaemic control [29], and the author did not provide details on the quantity used and the term. The literature showed that drinking moderately in the short or medium-term did not affect glycaemic control [108]. Current guidelines support moderate alcohol consumption as excessive chronic alcohol consumption or acute intoxication that adversely has detrimental effects on all organs and affects mortality and morbidity [109, 110]. In sub-Saharan Africa, careful recommendations on alcohol use need to be developed for patients with type 2 diabetes as alcohol might represent a concurrent source of expenses of the few resources available. The real nature of alcoholic beverages found in sub-Saharan Africa is not accurately known.
Several studies confirmed our findings concerning clinical factors with respect to glycaemic control. With a longer duration of diabetes, there is a deterioration of the function of the pancreas due to failure in beta cells, and the emergence of disease-related complications, which in turn can have effects on glycaemic control [8, 111]. The presence of comorbidities/complications poses a problem with respect to pill burden, adherence to treatment and cost, or as an intricate mechanism linked to beta-cell impairment or aggravation of insulin resistance [8, 94, 112,113,114,115,116,117]. In sub-Saharan Africa, there is a high proportion of undiagnosed diabetes mellitus, and the diagnosis is often delayed. At diagnosis, many patients will present with complications or comorbidities, thus complicating the management and the attainment of glycaemic targets [118]. Strategies to improve the diagnosis of diabetes mellitus must be considered by policy makers in sub-Saharan Africa for a reduction in diabetes-related complications and mortality [118].
Good medication adherence was associated with good glycaemic control. This finding is in line with that found in several studies [111, 119, 120], particularly that good adherence improves glycaemic control, leads to fewer emergency department visits, decreases hospitalizations, and lowers medical costs [121]. In sub-Saharan Africa, medication adherence is confronted by the issues of access and affordability of drugs [122]. The organization of a regular and reliable system for the supply of medicines at affordable prices, even in remote areas is essential to improve diabetes care.
Oral hypoglycaemic agents (OHAs), either insulin only or combined with the former, were associated with poor glycaemic control in our review. In the included studies, the matters surrounding medication use, such as adherence, reason for prescribing one agent or a combination, were not reported. The use of statins and some antihypertensive agents (thiazide diuretics and non-selective beta-blockers) are linked to comorbidities, with hypertension being the most frequent [123] and having been linked in several studies with high levels of glycosylated haemoglobin [124,125,126]. Since many patients have comorbidities, present late and may need these adjunct treatments, these findings have implications for the management of patients with type 2 diabetes in sub-Saharan Africa. They call for the judicious use of these agents and adherence of healthcare professionals to evidence-based diabetes care in SSA.
Concerning the reported interventions, all the exercise programs, and one educational program for self-management were associated with good glycaemic control. Nevertheless, the full integration of exercise into routine healthcare in Africa is challenged by poor knowledge and attitudes of patients and healthcare providers [127]. In the same way, self-management of diabetes is poor in Africa as it faces numerous barriers [128, 129]. Peer-support interventions have been increasingly recognized worldwide, but one may note that the transferability of interventions across different cultures might be difficult [24]. Research is needed to identify effective interventions to optimize glycaemic control in the context of sub-Saharan Africa.
To the best of our knowledge, this systematic review is the first to provide a prevalence estimate of glycaemic control and an overview of factors associated with glycaemic control in patients with type 2 diabetes in SSA. The review only considered studies in which multivariate analysis was performed in the data analysis and therefore excluded factors without an uncertain link to glycaemic control. The findings of this systematic review are also as good as the quality of the studies included, more so that most (70.2%) were of moderate quality. Most of the studies were observational and one cannot ascertain causality between factors identified and glycaemic control. Glycaemic control was assessed using different methods across the studies, with only 58.1% of the included studies using the recommended glycosylated haemoglobin. There were also different thresholds for glycaemic control through studies even if the same glycaemic control assessment was used. These variations in assessment standards have the potential for errors in estimates and misclassifications.
Beyond these limitations, this systematic review is, to our knowledge, the first to provide a broad view of the extent and multifactorial drivers of glycaemic control among patients with type 2 diabetes in SSA. The review highlights the need for changes in the organization of the healthcare systems in sub-Saharan Africa while ensuring effective funding. Health providers must be trained, and health facilities equipped for adequate diabetes care. The screening of diabetes mellitus must be improved as well as access to care for vulnerable patients. While this review highlights the need for multipronged interventions to improve glycaemic control and diabetes care in this region, further studies are needed to assess their feasibility, effectiveness, affordability and acceptability.
Conclusion
Suboptimal glycaemic control is pervasive among patients with type-2 diabetes in sub-Saharan Africa and poses a significant public health challenge. While urgent interventions are required to optimize glycaemic control in this region, these should consider sociodemographic, lifestyle, clinical, and treatment-related factors.
Availability of data and materials
The dataset(s) supporting the conclusions of this article is(are) included within the article and in the supplementary files. The protocol can be accessed from request to the corresponding author.
Abbreviations
- BMI:
-
Body mass index
- EGFR:
-
Estimated Glomerular Filtration Rate
- FBG:
-
Fasting blood glucose
- FBS:
-
Fasting blood sugar
- FPG:
-
Fasting plasma glucose
- Ghb:
-
: Glycosylated haemoglobin
- GLUT2:
-
Glucose transporter 2
- HbA1c:
-
Haemoglobin A1c
- JMF:
-
Joel Msafiri Francis
- JPF:
-
Jean-Pierre FINA
- LDL-C:
-
Low-Density Lipoprotein-Cholesterol
- Mh:
-
: MesH term
- Niddm:
-
: Non insulin dependent diabetes mellitus
- OBO:
-
Olufemi Babatunde Omole
- OHA:
-
Oral Hypoglycaemic Agents
- PRISMA:
-
Preferred Reporting Items for Systematic Reviews and Meta-analyses
- SSA:
-
Sub-Saharan Africa
- T2d:
-
Type 2 diabetes mellitus
- Tw:
-
Text word
- WHO:
-
World Health Organization
References
World Health Organization. Global Report on Diabetes, vol. 978. Geneva: World Health Organization; 2016. p. 6–86.
Moucheraud C, Lenz C, Latkovic M, Wirtz VJ. The costs of diabetes treatment in low- and middle-income countries : a systematic review. BMJ Glob Health. 2019. https://doi.org/10.1136/bmjgh-2018-001258.
Giugliano D, Maiorino MI, Bellastella G, Esposito K. Glycemic control in type 2 diabetes: from medication nonadherence to residual vascular risk. Endocrine. 2018;61(1):23–7.
Pastakia S, Pekny C, Manyara S, Fischer L. Diabetes in sub-Saharan Africa—from policy to practice to progress: targeting the existing gaps for future care for diabetes. Diabetes, Metab Syndr Obes Targets Ther. 2017;10:247–63.
Kirkman MS, Mahmud H, Korytkowski MT. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes mellitus. Endocrinol Metab Clin North Am. 2018;47(1):81–96.
Jie Cheng L, Wang W, Tee Lim S, Xi WuV. Factors associated with glycaemic control in patients with diabetes mellitus: a systematic literature review. J Clin Nurs. 2019;28:1433–50.
Brown SA, García AA, Brown A, Becker BJ, Conn VS, Ramírez G, et al. Biobehavioral determinants of glycemic control in type 2 diabetes: a systematic review and meta-analysis HHS Public Access. Patient Educ Couns. 2016;99(10):1558–67.
Alramadan MJ, Afroz A, Hussain SM, Batais MA, Almigbal TH, Al-Humrani HA, et al. Patient-related determinants of glycaemic control in people with type 2 diabetes in the gulf cooperation council countries: a systematic review. J Diabetes Res. 2018. https://doi.org/10.1155/2018/9389265.
Cheng LJ, Wang W, Lim ST, Wu VX. Factors associated with glycaemic control in patients with diabetes mellitus: a systematic literature review. J Clin Nurs. 2019. https://doi.org/10.1111/jocn.14795.
de Pablos-Velasco P, Parhofer KG, Bradley C, Eschwège E, Gönder-Frederick L, Maheux P, et al. Current level of glycaemic control and its associated factors in patients with type 2 diabetes across Europe: data from the PANORAMA study. Clin Endocrinol. 2014;80(1):47–56. https://doi.org/10.1111/cen.12119.
Page MJ, Mckenzie JE, Bossuyt PM, Boutron I, Hoffmann C, Mulrow CD, et al. The PRISMA 020 statement : an updated guideline for reporting systematic reviews Systematic reviews and Meta-Analyses. Clin Endocrinol. 2021. https://doi.org/10.1111/cen.12119.
ebp - Critical Appraisal Tools | Joanna Briggs Institute [Internet]. https://joannabriggs.org/ebp/critical_appraisal_tools. Accessed 26 Apr 2020.
Benenson I, Waldron FA, Jadotte YT, Dreker MP, Holly C. Risk factors for hypertensive crisis in adult patients: a systematic review. JBI Evid Synth. 2021;19(6):1292–327. https://doi.org/10.11124/JBIES-20-00243.
StataCorp. Stata statistical software: release 17. College Station, TX: StataCorp LLC; 2021.
Higgins JP, Thompson SG, Deeks JJ, Altman DG. Measuring inconsistency in meta-analyses. BMJ. 2003;327(7414):557–60. https://doi.org/10.1136/bmj.327.7414.557.
Achila OO, Ghebretinsae M, Kidane A, Simon M, Makonen S, Rezene Y. Factors associated with poor glycemic and lipid levels in ambulatory diabetes mellitus type 2 patients in Asmara, Eritrea: a cross-sectional study. J Diabetes Res. 2020. https://doi.org/10.1155/2020/5901569.
Adejumo OA, Akinbodewa AA, Ogunleye A, Okaka EI, Lamidi O, Akinbo E. Metabolic syndrome and atherosclerotic cardiovascular risk in a population of market women in a semi-urban town. South-West Nigeria West Afr J Med. 2020;37(6):666–70.
Adeniyi OV, Yogeswaran P, Longo-Mbenza B, Ter GD, Ajayi AI, Adeniyi V. Cross-sectional study of patients with type 2 diabetes in OR Tambo district, South Africa. BMJ Open. 2016;6:10875. https://doi.org/10.1136/bmjopen-2015-010875.
Afolabi BI, Ibitoye BO, Ikem RT, Omisore AD, Idowu BM, Soyoye DO. The relationship between glycaemic control and non-alcoholic fatty liver disease in Nigerian type 2 diabetic patients. J Natl Med Assoc. 2018;110(3):256–64. https://doi.org/10.1016/j.jnma.2017.06.001.
Akabwai GP, Kibirige D, Mugenyi L, Kaddu M, Opio C, Lalitha R, et al. Vitamin B12 deficiency among adult diabetic patients in Uganda: relation to glycaemic control and haemoglobin concentration. J Diabetes Metab Disord. 2016. https://doi.org/10.1186/s40200-016-0250-x.
Akpalu J, Yorke E, Ainuson-Quampah J, Balogun W, Yeboah K. Depression and glycaemic control among type 2 diabetes patients: a cross-sectional study in a tertiary healthcare facility in Ghana. BMC Psychiatry. 2018. https://doi.org/10.1186/s12888-018-1933-2.
Anioke IC, Ezedigboh AN, Dozie-Nwakile C, Johnpaul Chukwu I, Kalu N. Predictors of poor glycemic control in adult with type 2 diabetes in South-Eastern Nigeria. Afr Health Sci. 2019. https://doi.org/10.4314/ahs.v19i4.3.
Anyanwu AC, Fasanmade OA, Odeniyi IA, Iwuala S, Coker HB, Ohwovoriole AE. Effect of Vitamin D supplementation on glycemic control in Type 2 diabetes subjects in Lagos. Nigeria Indian J Endocrinol Metab. 2016;20(2):189–94.
Assah FK, Atanga EN, Enoru S, Sobngwi E, Mbanya JC. Community-based peer support significantly improves metabolic control in people with Type 2 diabetes in Yaoundé. Cameroon Diabet Med. 2015;32(7):886–9. https://doi.org/10.1111/(ISSN)1464-5491.
Ayele AA, Tegegn HG, Ayele TA, Ayalew MB. Medication regimen complexity and its impact on medication adherence and glycemic control among patients with type 2 diabetes mellitus in an Ethiopian general hospital. BMJ Open Diabetes Res Care. 2019. https://doi.org/10.1136/bmjdrc-2019-000685.
Belay E, Abera A, Mehari A, Gebremeskel G, Endrias A, Endris K. Achievements of diabetes goals and their determinants in type 2 diabetic patients attending outpatient diabetic clinic in Northern Ethiopia. Int J chronic Dis. 2017;2017:1–8.
BeLue R, Ndiaye K, Ndao F, Ba FNN, Diaw M. Glycemic control in a clinic-based sample of diabetics in M’Bour Senegal Airhihenbuwa CO, Ogedegbe G, editors. Heal Educ Behav. 2016;43:112S-116S.
Biadgo B, Melak T, Ambachew S, Baynes H, Andualem Limenih M, Negerie Jaleta K, et al. The prevalence of metabolic syndrome… The prevalence of metabolic syndrome and its components among type 2 diabetes mellitus patients at a tertiary hospital, Northwest Ethiopia. Ethiop J Heal Sci. 2018;28(4):645. https://doi.org/10.4314/ejhs.v28i5.16.
Biru TT. Glycemic control and its determinants among ambulatory patients with type 2 diabetes. J Diabetes Metab. 2017;8(8):2.
Blum J, Chaney M, Mudji J, Mfungwa Jaimé K, Rice T, Labhardt ND. Glycaemic control among patients with type 2 diabetes followed in a rural African primary care setting—a reality check in the Democratic Republic of Congo. Prim Care Diabetes. 2019. https://doi.org/10.1016/j.pcd.2019.08.002.
Botchway M, Davis RE, Appiah LT, Moore S, Merchant AT. The influence of religious participation and use of traditional medicine on type 2 diabetes control in Urban Ghana. J Relig Health. 2021. https://doi.org/10.1007/s10943-021-01187-9.
Camara A, Balde NM, Sobngwi-Tambekou J, Kengne AP, Diallo MM, Tchatchoua APK, et al. Poor glycemic control in type 2 diabetes in the South of the Sahara: the issue of limited access to an HbA1c test. Diabetes Res Clin Pract. 2015;108(1):187–92.
Dagnew B, Wolide AD, Mossie A. Cognitive impairment among type 2 diabetes mellitus patients at Jimma University Specialized Hospital, Southwest Ethiopia. J Public Heal Epidemiol. 2017;9(11):300–8.
Demoz GT, Gebremariam A, Yifter H, Alebachew M, Niriayo YL, Gebreslassie G, et al. Predictors of poor glycemic control among patients with type 2 diabetes on follow-up care at a tertiary healthcare setting in Ethiopia. BMC Res Notes. 2019. https://doi.org/10.1186/s13104-019-4248-6.
Doglikuu BID, Abdulai A, Yaseri M, Shakibazadeh E, Djazayery A, Mirzaei K. Association of adherence to diabetics feeding recommendation with glycaemic control and with malnutrition risk among normal weight persons with type 2 diabetes in Ghana. Malaysian J Med Sci. 2021;28(2):84–99.
Eticha T, Gebretsadik H, Kahsay G, Ali D. Factors associated with poor glycemic control in type 2 diabetic patients investigated at Ayder referral hospital, Mekelle. Ethiopia Int J Pharm Pharm Res. 2016;6(3):160–712016.
Ezema CI, Onwunali AA, Lamina S, Ezugwu UA, Amaeze AA, Nwankwo MJ. Effect of aerobic exercise training on cardiovascular parameters and CD4 cell count of people living with human immunodeficiency virus/acquired immune deficiency syndrome: a randomized controlled trial. Niger J Clin Pract. 2014;17(5):543–8.
Fayehun AF, Olowookere OO, Ogunbode AM, Adetunji AA, Esan A. Walking prescription of 10 000 steps per day in patients with type 2 diabetes mellitus: a randomised trial in Nigerian general practice. Br J Gen Pract J R Coll Gen Pract. 2018;68(667):e139–45.
Fekadu G, Bula K, Bayisa G, Turi E, Tolossa T, Kebebe H. challenges and factors associated with poor glycemic control among type 2 diabetes mellitus patients at Nekemte Referral Hospital, Western Ethiopia. J Multidiscip Healthc. 2019;12:963–74.
Fseha B. Glycemic control and it’s associated factors in type 2 diabetic patients in Suhul Hospital, Northwest Tigray Ethiopia. J Diabetes Metab. 2017;08(03):9459.
Gathu CW, Shabani J, Kunyiha N, Ratansi R. Effect of diabetes self-management education on glycaemic control among type 2 diabetic patients at a family medicine clinic in Kenya: a randomised controlled trial. African J Prim Heal care Fam Med. 2018;10(1):e1-9.
Gebremedhin T, Workicho A, Angaw DA. Health-related quality of life and its associated factors among adult patients with type II diabetes attending Mizan Tepi University Teaching Hospital, Southwest Ethiopia. BMJ Open Diabetes Res Care. 2019. https://doi.org/10.1136/bmjdrc-2018-000577.
Hailu FB, Hjortdahl P, Moen A. Nurse-Led diabetes self-management education improves clinical parameters in Ethiopia. Front Public Heal. 2018. https://doi.org/10.3389/fpubh.2018.00302.
Id SN, Birhan N, Amare F, Id GM. Rate of glycemic control and associated factors among type two diabetes mellitus patients in Ethiopia: a cross sectional study. PLoS ONE. 2021;177:1–12. https://doi.org/10.1371/journal.pone.0251506.
Inih OS, Esther YE, Adetola FO, Chinedu AA, Brenda NC, Efedaye OA. Testicular dysfunction is a common feature in men with type 2 diabetes mellitus in a Nigerian tertiary hospital. Curr Diabetes Rev. 2018;14(3):298–306.
Kalain A, Omole OB. Lifestyle advice, processes of care and glycaemic control amongst patients with type 2 diabetes in a South African primary care facility. African J Prim Heal Care Fam Med. 2020. https://doi.org/10.4102/phcfm.v12i1.2163.
Kamuhabwa AR, Charles E. Predictors of poor glycemic control in type 2 diabetic patients attending public hospitals in Dar es Salaam. Drug Healthc Patient Saf. 2014;6:155–65.
Kassahun T, Eshetie T, Gesesew H. Factors associated with glycemic control among adult patients with type 2 diabetes mellitus: A cross-sectional survey in Ethiopia Endocrine Disorders. BMC Res Notes. 2016. https://doi.org/10.1186/s13104-016-1896-7.
Kefale AT, Biru TT, Addo HA. Appropriateness of insulin commencement and adequacy of glycemic control among ambulatory patients with type 2 diabetes in Ethiopia. J Diabetes Metab Disord. 2019;18(2):461–9.
Khoza SP, Crowther NJ, Bhana S. The effect of HIV infection on glycaemia and renal function in type 2 diabetic patients. Wang W, editor. PLoS ONE. 2018;13(6):e0199946. https://doi.org/10.1371/journal.pone.0199946.
Kimando MW, Otieno FCF, Ogola EN, Mutai K. Adequacy of control of cardiovascular risk factors in ambulatory patients with type 2 diabetes attending diabetes out-patients clinic at a county hospital, Kenya. BMC Endocr Disord. 2017;17(1):73.
Maharaj SS, Nuhu JM. Rebound exercise: a beneficial adjuvant for sedentary non-insulin-dependent type 2 diabetic individuals in a rural environment. Aust J Rural Health. 2016;24(2):123–9. https://doi.org/10.1111/(ISSN)1440-1584.
Mamo Y, Bekele F, Nigussie T, Zewudie A. Determinants of poor glycemic control among adult patients with type 2 diabetes mellitus in Jimma University Medical Center, Jimma zone, south west Ethiopia: a case control study. BMC Endocr Disord. 2019;19(1):1–11.
Mash R, Ugoagwu A, Vos C, Rensburg M, Erasmus R. Evaluating point-of-care testing for glycosylated haemoglobin in public sector primary care facilities in the Western Cape South Africa. South African Med J. 2016;106(12):1236–40.
Mash RJ, Rhode H, Zwarenstein M, Rollnick S, Lombard C, Steyn K, et al. Effectiveness of a group diabetes education programme in under-served communities in South Africa: a pragmatic cluster randomized controlled trial. Diabet Med. 2014;31:987–93.
Mashele TS, Mogale MA, Towobola OA, Moshesh MF, Tsakani SM, Motetelo Mogale A, et al. Central obesity is an independent risk factor of poor glycaemic control at Dr George Mukhari Academic Hospital. South African Fam Pract. 2019;61(1):18–23.
Mayet L, Naidoo SS, Naidoo SC. An evaluation of insulin therapy initiation among patients with type 2 diabetes attending a public health facility in South Africa. South African Fam Pract. 2012;54(6):525–30.
Mobula LM, Stephen F, Carson KA, Burnham G, Arthur L, Ansong D, et al. Translational metabolic syndrome research predictors of glycemic control in type-2 diabetes mellitus: evidence from a multicenter study in Ghana. Transl Metab Syndr Res. 2018;1:1–8.
Mohamed HG, Idris SB, Ahmed MF, Bøe OE, Mustafa K, Ibrahim SO, et al. Association between oral health status and type 2 diabetes mellitus among Sudanese adults: a matched case-control study. PLoS ONE. 2013;8(12):e82158.
Mohammed AS, Adem F, Tadiwos Y, Woldekidan NA, Degu A. Level of adherence to the dietary recommendation and glycemic control among patients with type 2 diabetes mellitus in Eastern Ethiopia: a cross-sectional study. Diabetes Metab Syndr Obesity-Targets Ther. 2020;13:2605–12.
Mphwanthe G, Weatherspoon D, Kalimbira A, Weatherspoon L. Non-dietary factors associated with glycemic status among adults diagnosed with type 2 diabetes mellitus in Malawi. Soc Work Public Health. 2020;00(00):1–12. https://doi.org/10.1080/19371918.2020.1785367.
Mphwanthe G, Weatherspoon D, Li W, Weatherspoon L. Dietary association with glycemic status among adults clinically diagnosed with type 2 diabetes in Malawi. J Community Health Nurs. 2020;37(4):233–43.
Muchiri JW, Gericke GJ, Rheeder P. Effect of a nutrition education programme on clinical status and dietary behaviours of adults with type 2 diabetes in a resource-limited setting in South Africa: a randomised controlled trial. Public Health Nutr. 2016;19(1):142–55.
Mwavua SM, Ndungu EK, Mutai KK, Joshi MD. A comparative study of the quality of care and glycemic control among ambulatory type 2 diabetes mellitus clients, at a Tertiary Referral Hospital and a Regional Hospital in Central Kenya. BMC Res Notes. 2016. https://doi.org/10.1186/s13104-015-1826-0.
Mwita JC, Francis JM, Omech B, Botsile E, Oyewo A, Mokgwathi M, et al. Glycaemic, blood pressure and low-density lipoprotein-cholesterol control among patients with diabetes mellitus in a specialised clinic in Botswana: a cross-sectional study. BMJ Open. 2019. https://doi.org/10.1136/bmjopen-2018-026807.
NoorSufian K, Elmadhoun WM, Bushara SO, Almobarak AO, Salim RS, Forawi SA, et al. Glycaemic control in Sudanese individuals with type 2 diabetes: population based study. Diabetes Metab Syndr. 2017;11(Suppl 1):S147–51.
Omar SM, Musa IR, Osman OE, Adam I. Assessment of glycemic control in type 2 diabetes in the eastern Sudan. BMC Res Notes. 2018. https://doi.org/10.1186/s13104-018-3480-9.
Osuji NA, Solomon Ojo O, Malomo SO, Sogunle PT, Egunjobi AO, et al. Family Medicine and Community Health Relationship between glycemic control and perceived family support among people with type 2 diabetes mellitus seen in a rich kinship network in Southwest Nigeria. Fam Med Community Heal. 2018;6(4):168–77.
Otieno CFF, Kanu JE, Karari EM, Okech-Helu V, Joshi MD, Mutai K. Glucose-lowering therapies, adequacy of metabolic control, and their relationship with comorbid depression in outpatients with type 2 diabetes in a tertiary hospital in Kenya. Diabetes Metab Syndr Obesity-Targets Ther. 2017. https://doi.org/10.2147/DMSO.S124473.
Oyewole OO, Odusan O, Ale AO. Global disability burden and its predictors among adult Nigerians living with type-2 diabetes. Ghana Med J. 2019;53(2):135–41.
Rambiritch V, Maharaj B, Naidoo P. Glibenclamide in patients with poorly controlled type 2 diabetes: a 12-week, prospective, single-center, open-label, dose-escalation study. Clin Pharmacol Adv Appl. 2014;6(1):63.
Ramkisson S, Pillay JB, Ramkisson S, Pillay BJ, Sartorius B, University of KwaZulu-Natal SA. Diabetes distress and related factors in South African adults with type 2 diabetes. J Endocrinol Metab Diabetes South Africa. 2016;21(2):35–9.
Rwegerera GM, Masaka A, Pina-Rivera Y, Moshomo T, Gaenamong M, Godman B, et al. Determinants of glycemic control among diabetes mellitus patients in a tertiary clinic in Gaborone Botswana: findings and implications. Hosp Pract. 2019;47(1):34–41.
Sarfo-Kantanka O, Sarfo FS, Ansah EO, Yorke E, Akpalu J, Nkum BC, et al. Frequency and determinants of thyroid autoimmunity in Ghanaian type 2 diabetes patients: a case-control study. BMC Endocr Disord. 2017. https://doi.org/10.1186/s12902-016-0152-4.
Shimels T, Abebaw M, Bilal AI, Tesfaye T. Treatment pattern and factors associated with blood pressure and fasting plasma glucose control among patients with type 2 diabetes mellitus in police referral hospital in Ethiopia. Ethiop J Health Sci. 2018. https://doi.org/10.4314/ejhs.v28i4.12.
Siddiqui MA, Bhana S, Daya R. The relationship between objectively measured physical activity and parameters of disease control in an African population of type 2 diabetes mellitus The relationship between objectively m. J Endocrinol Metab Diabetes South Africa. 2018;23(3):80–5.
Tefera YG, Gebresillassie BM, Emiru YK, Yilma R, Hafiz F, Akalu H, et al. Diabetic health literacy and its association with glycemic control among adult patients with type 2 diabetes mellitus attending the outpatient clinic of a university hospital in Ethiopia. PLoS ONE. 2020. https://doi.org/10.1371/journal.pone.0231291.t004.
Tekalegn Y, Addissie A, Kebede T, Ayele W. Magnitude of glycemic control and its associated factors among patients with type 2 diabetes at Tikur Anbessa Specialized Hospital Addis Ababa, Ethiopia. PLoS ONE. 2018. https://doi.org/10.1371/journal.pone.0193442.
Teklay G, Hussien J, Tesfaye D. Non-adherence and associated factors among type 2 diabetic patients at Jimma University Specialized Hospital, Southwest Ethiopia. J Med Sci. 2013;13(7):578–84.
Thuita AW, Kiage BN, Onyango AN, Makokha AO. The relationship between patient characteristics and glycemic control (HbA1c) in type 2 diabetes patients attending thika level five hospital, Kenya. African J Food Agric Nutr Dev. 2019;19(4):15041–59.
Thuita AW, Kiage BN, Onyango AN, Makokha AO. Effect of a nutrition education programme on the metabolic syndrome in type 2 diabetes mellitus patients at a level 5 Hospital in Kenya: “a randomized controlled trial.” BMC Nutr. 2020. https://doi.org/10.1186/s40795-020-00355-6.
Tsobgny-Tsague NF, Lontchi-Yimagou E, Nana AR, Tankeu AT, Katte JC, Dehayem MY, et al. Effects of nonsurgical periodontal treatment on glycated haemoglobin on type 2 diabetes patients (PARODIA 1 study): a randomized controlled trial in a sub-Saharan Africa population. BMC Oral Health. 2018;18(1):28.
Alebachew Woldu M, Diriba WC. Factors associated with poor glycemic control among patients with type 2 diabetes mellitus in ambo Hospital Ambo; Ethiopia. Endocrinol Metab Syndr. 2014;03(04):2–7.
Yan H, Prista A, Ranadive SM, Damasceno A, Caupers P, Kanaley JA, et al. clinical study effect of aerobic training on glucose control and blood pressure in T2DDM East African males. ISRN Endocrinol. 2014. https://doi.org/10.1155/2014/864897.
Yigazu DM, Desse TA. Glycemic control and associated factors among type 2 diabetic patients at Shanan Gibe Hospital, Southwest Ethiopia. BMC Res Notes. 2017. https://doi.org/10.1186/s13104-017-2924-y.
Yimama M, Jarso H, Desse TA. Determinants of drug-related problems among ambulatory type 2 diabetes patients with hypertension comorbidity in Southwest Ethiopia: a prospective cross sectional study. BMC Res Notes. 2018. https://doi.org/10.1186/s13104-018-3785-8.
Yosef T, Nureye D, Tekalign E. Poor glycemic control and its contributing factors among type 2 diabetes patients at adama hospital medical college in east Ethiopia. Diabetes Metab Syndr Obes Targets Ther. 2021;14:3273–80.
Abera RG, Demesse ES, Boko WD. Evaluation of glycemic control and related factors among outpatients with type 2 diabetes at Tikur Anbessa Specialized Hospital, Addis Ababa, Ethiopia: a cross-sectional study. BMC Endocr Disord. 2022;22(1):1–11. https://doi.org/10.1186/s12902-022-00974-z.
Abebe A, Wobie Y, Kebede B, Wale A, Destaw A. Self-care practice and glycemic Control among type 2 diabetes patients on follow up in a developing country : a prospective observational study. J Diabetes Metab Disord. 2022. https://doi.org/10.1007/s40200-022-00995-42022.
Gebreyohannes EA, Netere AK, Belachew SA. Glycemic control among diabetic patients in Ethiopia: a systematic review and meta-analysis. PLoS ONE. 2019;14(8):e0221790. https://doi.org/10.1371/journal.pone.0221790.
Sobngwi E, Ndour-Mbaye M, Boateng KA, Ramaiya KL, Njenga EW, Diop SN, et al. Type 2 diabetes control and complications in specialised diabetes care centres of six sub-Saharan African countries: the Diabcare Africa study. Diabetes Res Clin Pract. 2012;95(1):30–6. https://doi.org/10.1016/j.diabres.2011.10.018.
Fang M, Wang D, Coresh J, Selvin E. Trends in diabetes treatment and control in U.S. adults, 1999–2018. N Engl J Med. 2021;384(23):2219–28.
Mercer T, Chang AC, Fischer L, Gardner A, Kerubo I, Tran DN, et al. Mitigating the burden of diabetes in sub-saharan africa through an integrated diagonal health systems approach. Diabetes Metab Syndr Obes Targets Ther. 2019;12:2261–72.
Shamshirgaran SM, Mamaghanian A, Aliasgarzadeh A, Aiminisani N, Ataie J. Age differences in diabetes-related complications and glycemic control. BMC Endocr Disord. 2017. https://doi.org/10.1186/s12902-017-0175-5.
Schernthaner G, Schernthaner-Reiter MH. Diabetes in the older patient: heterogeneity requires individualisation of therapeutic strategies. Diabetologia. 2018;61(7):1503–16. https://doi.org/10.1007/s00125-018-4547-9.
Duarte FG, Moreira S, Almeida CC, Teles CADS, Andrade CS, Reingold AL, et al. Sex differences and correlates of poor glycaemic control in type 2 diabetes : a cross-sectional study in Brazil and Venezuela. BMJ Open. 2019;9:e023401. https://doi.org/10.1136/bmjopen-2018-023401
GoedeckeJulia H, Mtintsilana A, Dlamini SN, Kengne AP. Type 2 diabetes mellitus in African women. Diabetes Res Clin Pract. 2017;123:87–96.
Seligman HK, Tschann J, Jacobs EA, Fernandez A, López A. Food insecurity and glycemic control among low-income patients with type 2 diabetes. Diabetes Care. 2012;35(2):233–8.
Houle J, Lauzier-Jobin F, Beaulieu MD, Meunier S, Coulombe S, Côté J, et al. Socioeconomic status and glycemic control in adult patients with type 2 diabetes: a mediation analysis. BMJ Open Diabetes Res Care. 2016;4(1):184.
Jackson Y, Lozano Becerra JC, Carpentier M. Quality of diabetes care and health insurance coverage: a retrospective study in an outpatient academic public hospital in Switzerland. BMC Health Serv Res. 2016;16(1):1–7. https://doi.org/10.1186/s12913-016-1801-z.
Almigbal T. Driving distance and glycemic control in patients with insulin-treated diabetes mellitus: results from the diabetes and driving study. J Nat Sci Med. 2021;26(4):244.
Kelly C, Hulme C, Farragher T, Clarke G. Are differences in travel time or distance to healthcare for adults in global north countries associated with an impact on health outcomes? A systematic review. BMJ Open. 2016;6(11):1–9.
Colberg SR, Sigal RJ, Yardley JE, Riddell MC, Dunstan DW, Dempsey PC, et al. Physical activity / exercise and diabetes: a position statement of the American diabetes association. Diabetes Care. 2016;39:2065–79.
García-Molina L, Lewis-Mikhael AM, Riquelme-Gallego B, Cano-Ibáñez N, Oliveras-López MJ, Bueno-Cavanillas A. Improving type 2 diabetes mellitus glycaemic control through lifestyle modification implementing diet intervention: a systematic review and meta-analysis. Eur J Nutr. 2020;59(4):1313–28. https://doi.org/10.1007/s00394-019-02147-6.
Campagna D, Alamo A, Di Pino A, Russo C, Calogero AE, Purrello F, et al. Smoking and diabetes: dangerous liaisons and confusing relationships. Diabetol Metab Syndr. 2019;11(1):1–12. https://doi.org/10.1186/s13098-019-0482-2.
Lycett D, Nichols L, Ryan R, Farley A, Roalfe A, Mohammed MA, et al. The association between smoking cessation and glycaemic control in patients with type 2 diabetes: a THIN database cohort study. Lancet Diabetes Endocrinol. 2015;3(6):423–30.
Saritsiri S, Panintrarux P, Kuykomoot S, Poonvutikul C. Smoking cessation and glycemic control among type 2 diabetes patients in primary care, Bangkok, Thailand. Tob Induc Dis. 2021. https://doi.org/10.1111/j.1462-8902.2004.00329.x.
Hirst JA, Aronson JK, Feakins BG, Ma C, Farmer AJ, Stevens RJ. Short- and medium-term effects of light to moderate alcohol intake on glycaemic control in diabetes mellitus: a systematic review and meta-analysis of randomized trials. Diabet Med. 2017;34(5):604–11.
Ahmed AT, Karter AJ, Warton EM, Doan JU, Weisner CM. The relationship between alcohol consumption and glycemic control among patients with diabetes: the Kaiser permanente northern California diabetes registry. J Gen Intern Med. 2008;23(3):275.
Inada S, Koga M. Alcohol consumption reduces HbA1c and glycated albumin concentrations but not 1,5-anhydroglucitol. Ann Clin Biochem. 2017;54(6):631–5. https://doi.org/10.1177/0004563216675646.
Davies MJ, Alessio DAD, Fradkin J, Kernan WN, Mathieu C, Mingrone G. Management of hyperglycemia in type 2 diabetes, 2018. A consensus report by the American diabetes association (ADA) and the European Association for the Study of Diabetes ( EASD). Diabetes Care. 2018;41:2669–701.
Chan JCN, Gagliardino JJ, Baik SH, Chantelot JM, Ferreira SRG, Hancu N, et al. Multifaceted determinants for achieving glycemic control the international diabetes management practice study (IDMPS). Diabetes Care. 2009;32(2):227–33.
Hage M, Zantout MS, Azar ST. Thyroid disorders and diabetes mellitus. J Thyroid Res. 2011. https://doi.org/10.4061/2011/439463
Pillay S, Aldous C, Mahomed F. A deadly combination—HIV and diabetes mellitus: where are we now? SAMJ. 2016;106(4):378–83.
Dedefo G, Kinde S, Mudi K, Tarekegn G, Teka S, Arba Minch University E. Hypogonadism and associated risk factors in male patients with type 2 diabetes mellitus attending the diabetic clinic of Tikur Anbessa Specialized Teaching Hospital, Addis Ababa, Ethiopia. J Endocrinol Metab Diabetes South Africa. 2019;24(1):16–22.
Urina-Jassir M, Herrera-Parra LJ, Hernández Vargas JA, Valbuena-García AM, Acuña-Merchán L, Urina-Triana M. The effect of comorbidities on glycemic control among Colombian adults with diabetes mellitus: a longitudinal approach with real-world data. BMC Endocr Disord. 2021;21(1):128. https://doi.org/10.1186/s12902-021-00791-w.
Blah AN, George CE, Mukherjee D, Norman G. Risk factors associated with poorly controlled diabetes in a rural population of Karnataka: a case-control study. Int J Res Med Sci. 2017;2(4):1530–3.
Asmelash D, Asmelash Y. The burden of undiagnosed diabetes mellitus in adult african population: a systematic review and meta-analysis. J Diabetes Res. 2019. https://doi.org/10.1155/2019/4134937.
Bagonza J, Rutebemberwa E, Bazeyo W. Adherence to anti diabetic medication among patients with diabetes in eastern Uganda; a cross sectional study. BMC Health Serv Res. 2015. https://doi.org/10.1186/s12913-015-0820-5.
Desse TA, Eshetie TC, Gudina EK. Predictors and treatment outcome of hyperglycemic emergencies at Jimma University Specialized Hospital, southwest Ethiopia. BMC Res Notes. 2015;8(1):1–8.
Capoccia K, Odegard PS, Letassy N. Medication adherence with diabetes medication: a systematic review of the literature. Diabetes Educ. 2016;42(1):34–71. https://doi.org/10.1177/0145721715619038.
Waari G, Mutai J, Gikunju J. Medication adherence and factors associated with poor adherence among type 2 diabetes mellitus patients on follow-up at Kenyatta National Hospital, Kenya. Pan Afr Med J. 2018. https://doi.org/10.11604/pamj.2018.29.82.12639.
Ekoru K, Doumatey A, Bentley AR, Chen G, Zhou J, Shriner D, et al. Type 2 diabetes complications and comorbidity in Sub-Saharan Africans. EClinicalMedicine. 2019;16:30–41. https://doi.org/10.1016/j.eclinm.2019.09.001.
Erqou S, Lee CC, Adler AI. Statins and glycaemic control in individuals with diabetes: a systematic review and meta-analysis. Diabetologia. 2014;57(12):2444–52.
Eriksson JW, Jansson P-A, Carlberg B, Hägg A, Kurland L, Svensson MK, et al. Hydrochlorothiazide, but not candesartan, aggravates insulin resistance and causes visceral and hepatic fat accumulation. Hypertension. 2008;52:1030–7.
Hirst JA, Farmer AJ, Feakins BG, Aronson JK, Stevens RJ. Quantifying the effects of diuretics and β-adrenoceptor blockers on glycaemic control in diabetes mellitus—a systematic review and meta-analysis. Br J Clin Pharmacol. 2015;79(5):733–43.
Jasper US. Diabetes and exercise in sub-Saharan Africa: challenges and way forward. J Diabetes Metab. 2014;5(4):1–3.
Stephani V, Opoku D, Beran D. Self-management of diabetes in Sub-Saharan Africa: a systematic review. BMC Public Health. 2018;18(1):1148. https://doi.org/10.1186/s12889-018-6050-0.
Letta S, Aga F, Yadeta TA, Geda B, Dessie Y. Barriers to diabetes patients’ self-care practices in Eastern Ethiopia: a qualitative study from the health care providers perspective. Diabetes Metab Syndr Obes. 2021;22(14):4335–49. https://doi.org/10.2147/DMSO.S335731.PMID:34712054;PMCID:PMC8547594.
Acknowledgements
The authors are grateful to Professor Philippe Ngwala Lukanu from the Department of Family Medicine of the Protestant University of Congo, and Professor Ernest Sumaili Kiswaya from the Department of Internal Medicine, of the University of Kinshasa for their contribution to reviewing the final draft of this manuscript. We also thank Dr Olufemi O. Oyewole from the Olabisi Onabanjo University Teaching Hospital, Nigeria for providing us with its study dataset. This systematic review is part of a PhD research in family medicine at the University of the Witwatersrand, Johannesburg.
Funding
The authors received no specific funding for this work.
Author information
Authors and Affiliations
Contributions
JPF conceived the study, conducted the literature search, selected the studies, assessed the methodological quality of the studies, synthesized the findings, and wrote the first draft of the manuscript. OBO participated in the conceptualization, analysis, synthesis of data and review of the manuscript. JMF participated in the conceptualization, selection of the studies, assessment of the methodological quality of the studies, data synthesis, and reviewed the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Table S1.
Search strategy in the included databases. A description of the strategy used for the literature search.
Additional file 2: Table S2.
General characteristics of excluded studies and reason for exclusion. A description of the excluded studies and the reason for their exclusion.
Additional file 3: Table S3.
Data for metanalysis of proportions of glycaemic control in included studies. Data extracted for metaanalysis in the individual studies.
Additional file 4: Table S4.
Assessment of methodological quality for included cross-sectional studies. Assessment of the risk of bias for cross-sectional studies with the Joanna Briggs checklist.
Additional file 5: Table S5.
Assessment of methodological quality of quasi-experimental studies. Assessment of the risk of bias for quasi-experimental studies with the Joanna Briggs checklist.
Additional file 6: Table S6.
Assessment of methodological quality for included randomized controlled trials. Assessment of the risk of bias for randomized controlled trials
Additional file 7: Table S7.
Assessment of methodological quality of case–control studies. The cross-sectional studies assessed with the Joanna Briggs checklist.
Additional file 8: Table S8.
Assessment of methodological quality of cohort study. Assessment of the risk of bias for cohort study through the Joanna Briggs checklist.
Additional file 9.
List of references of excluded studies. The list of excluded references
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Fina Lubaki, JP., Omole, O.B. & Francis, J.M. Glycaemic control among type 2 diabetes patients in sub-Saharan Africa from 2012 to 2022: a systematic review and meta-analysis. Diabetol Metab Syndr 14, 134 (2022). https://doi.org/10.1186/s13098-022-00902-0
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00902-0