Abstract
Background
This study aimed to investigate the effects of legumes in dietary approaches to stop hypertension (DASH) on blood pressure and urinary sodium and potassium in participants with type 2 diabetes. We further investigated whether changes in individual dietary food groups in the DASH diet contribute to blood pressure.
Methods
Participants were randomized to the traditional DASH diet (n = 150) or the legume-based DASH diet (n = 150). Blood pressure and urinary sodium and potassium were measured at baseline and after 16-week interventions. An intention-to-treat approach with multiple imputations of missing data was applied. The restricted cubic spline (RCS) was applied to assess the linearity and explore the shape of the relationship between the changes in food groups and systolic blood pressure (SBP) in the two intervention groups.
Results
A reduction in SBP and urinary sodium was observed at week 16 in both dietary interventions, and this reduction was more significant in the legume-based DASH diet, than in the DASH diet. In the legume-based DASH diet, SBP decreased with the legume intake of more than 95.8 g/day (P nonlinear < 0.001). The multivariable RCS analysis showed a U-shaped relationship of refined grains, an L-shaped relationship of fruits, and a linear relationship of sweet, energy, sodium and vegetables intake with SBP.
Conclusions
The DASH diet, enriched in legumes, could improve SBP in participants with type 2 diabetes. In DASH diet, the balance of consumption of refined grains and fruits along with higher vegetable consumption and lower sweet, sodium and energy intake reduced the SBP.
Trial registration: IRCT20090203001640N17.
Similar content being viewed by others
Introduction
Hypertension is a public health crisis, affecting more than one in four adults globally [1]. It is more common in type 2 diabetic patients with a prevalence of 70% [2]. Compared with non-diabetic individuals, patients with type 2 diabetes have nearly twice the incidence of hypertension [3]. The overlap between type 2 diabetes and hypertension markedly increased cardiovascular disease (CVD)-related morbidity and mortality [4]. The UK Prospective Diabetes Study showed that among type 2 diabetes patients, a 10 mg reduction in systolic blood pressure reduced the risk of CVD morbidity and mortality by 6–12% in type 2 diabetes patients [5].
Dietary modification can be effective in controlling and preventing diabetes and hypertension [6,7,8,9]. The Dietary Approaches to Stop Hypertension (DASH) diet, which is rich in healthy food groups, was developed to prevent and treatment of hypertension [10]. Also, finding from the optimal macronutrients intake (OMNI)-Heart trial which modified the DASH diet by replacing 10% of the carbohydrate with vegetable-based protein indicated a further reduction in blood pressure, compared with the original DASH diet among hypertensive patients [11]. However, replacing other animal sources of protein with red meat protein in DASH diet resulted in no more improvement in blood pressure among healthy [12], and hypertensive subjects [13].
Dietary guidelines have emphasized reducing the intake of red and processed meat and replacing these food groups with high-quality plant-based protein sources, such as legumes [14, 15]. However, it is unclear whether replacing red meat with legumes is associated with a reduced risk of hypertension [16, 17]. In addition, the majority of previous studies were conducted among healthy individuals or participants with hyperlipidemia or hypertension, and few studies investigated the effect of legumes on blood pressure among participants with type 2 diabetes; these studies showed that an 8-week consumption of legumes, 4–6 servings per week, did not have a significant effect on blood pressure among type 2 diabetes patients or individuals at risk of type 2 diabetes [18,19,20]. The low consumption rate of legumes compared to the recommended amount [17], as well as the small sample size, and the short follow-up period prevented the possible beneficial effect of legumes on blood pressure in these populations [18,19,20]. Therefore, this randomized controlled trial (RCT) aimed to investigate the effects of replacing one serving of red meat with legumes for at least 5 days per week in the DASH diet on blood pressure over 16 weeks in overweight and obese participants with type 2 diabetes. We further investigated which dietary food groups in the DASH diet were mostly contributed to the blood pressure reduction.
Methods
This RCT was registered in the Iranian Registry of Clinical Trials (IRCT) (code: IRCT20090203001640N17). The Ethics Committee of the Research Institute for Endocrine Sciences, affiliated with Shahid Beheshti University of Medical Sciences, Tehran, Iran, approved the study design (No.: IR.SBMU.ENDOCRINE.REC.1399.001) before participant recruitment. Also, all participants provided written informed consent prior to recruitment.
Design and setting of the study
This RCT was performed in the framework of the Tehran Lipid and Glucose Study (TLGS). From July 11, 2020, to March 10, 2021, in the TLGS unit, we recruited type 2 diabetes subjects (FPG level ≥ 126 mg/dl or the two-hour plasma glucose level ≥ 200 mg/dL or oral hypoglycemic medication consumption) aged 30–65 years, with BMI of 25–40 kg/m2, no weight change from three months before enrollment in the study, red meat consumption ≥ 1 serving/day, and willingness to consume legumes in the diet. Participants were excluded if they were pregnant or lactating, had a renal failure (creatinine ≥ 1.4 mg/dL in men and ≥ 1.3 mg/dL in women), or used insulin. According to the Declaration of Helsinki principles, the study procedure, objectives, and adverse events were explained to each participant.
Randomization and allocation concealment
An independent staff member of the TLGS randomly assigned the participants to the DASH diet or the legume-based DASH diet using block randomization sequences (four participants per block) generated by the randomization website (www.randomization.com).
Allocation to intervention was concealed from the principal investigators using sequentially numbered sealed opaque envelopes, which were only opened sequentially by a dietician in the presence of eligible participants at the first visit.
Dietary interventions
All participants were advised to complete a run-in period for 2 weeks, including adherence to their diet while eliminating legumes. Participants not willing to continue the study were excluded. Eligible participants were randomly allocated to the DASH diet or legume-based DASH diet over 16 weeks. The energy requirements of each participant were estimated from the initial resting energy expenditure, based on the Mifflin-St Jeor equation, multiplied by the physical activity coefficient.
Because the participants were overweight and obese, dietary interventions were designed to provide 500–700 kcal/day less than their energy requirement. Both dietary interventions provided almost 25–30% of the energy from fat, 15% from proteins, and 55–60% from carbohydrates. In the DASH diet group, the participants were instructed to follow the DASH diet (2000–3000 kcal based on energy requirement), which consisted of 8–12 servings/day of fruits and vegetables, 7–15 servings of whole grains, 2–3 servings of low-fat dairy products, two servings of red meat, one serving of nuts and seeds, and limited intake of sweets and sugar (five servings per week).
The legume-based DASH diet was similar to the traditional DASH diet, but one serving of red meat was replaced with one serving of legumes at least 5 days per week. Also, because legumes are equivalent to one serving of whole grains, one serving of bread was eliminated from the legume-based DASH diet. In both diets, the participants were advised to consume one teaspoon of salt per day (2300 mg/d) or less. All participants were asked to maintain their physical activity and not change their medications during the 16-week interventions unless prescribed by their physician. During the study, no changes in medication use were found in any participants.
Every 2 week, the dietitians called the participants to gather their dietary information using 3 day food records (2 weekdays and 1 weekend day) during the run-in period and the study period. Each phone call took between 45 and 60 min. Of 300 participants, 269 (89.6) completed 40–48 food records, and 31 (10.6) completed 30–39 food records during 16-week interventions.
Dietary intake include the mean intake of food records during 16 weeks follow-up. Dietary intake of fruits and vegetables, whole grains, refined grains, low-fat dairy products, red meat, nuts and seeds, sweets, legumes, salt intake, and energy intake were determined. To evaluate the adherence to dietary interventions, the dietitian compared participants' dietary intake with the dietary instructions, and reinforced their dietary adherence. The intake of macro- and micronutrients was also calculated using NUTRITIONIST III version 7.0 (N-Squared Computing, Salem, OR, USA), designed for Iranian food.
Measurements
Weight was measured with minimal clothing without shoes using a digital scale (Seca 707; range 0–150 kg) with an accuracy of 100 g. After a 15 min rest, blood pressure was measured using a standardized mercury sphygmomanometer on the right arm twice, at least 30 s apart. The average of the two measurements was reported as the subject’s blood pressure. Spot urine samples were obtained between 7:00 and 9:00 a.m. following overnight fasting. Urinary concentrations of sodium (mmol/dL) and potassium (mmol/dL) were measured using flame photometry (Screen Lyte, Hospitex Diagnostics, Florence, Italy).
Definition of terms
Hypertension was defined as systolic blood pressure (SBP) ≥ 140 mmHg and/or a diastolic blood pressure (DBP) of ≥ 90 mmHg or treatment with anti-hypertensive drugs [21]. Hyperlipidemia was defined as LDL-C ≥ 150 mg/dL, TC ≥ 200 mg/dL, and/or HDL-C < 40 mg/dL, and/or a triglyceride ≥ 150 mg/dL, and/or treatment with lipid lowering drugs [22].
DASH diet score calculation
We calculated a DASH diet score, based on eight dietary components, including fruits and vegetables, legumes and nuts, whole grains, low-fat dairy products, red and processed meat, sweets, fish and sodium [23].
Statistical analysis
With a two-sided α error = 0.05 and β error = 0.20 and 10 mmHg (SD = 16.6) reduction in SBP (minimal clinically important difference), and by assuming an attrition rate of 20%, total sample size was estimated to be 300 participants [20, 24] using following formula: ((Z 1-α/2 + Z1-β)2 * (S12 + S22))/\(\Delta\) 2.
All analyses were performed using Stata version 14.0 software (StataCorp LLC, TX, USA). Analyses were performed on all participants who were randomly allocated to the dietary interventions based on the intention-to-treat (ITT) principle. The Multiple imputation by chained equations (MICE) procedure was applied to impute the missing data (n = 16) for the outcomes. In multiple imputations, the predictors included all variables in Table 1, as well as dietary interventions. The baseline characteristics are presented as mean ± SD for demographic variables, dietary factors, SBP, DBP, and urine electrolytes and count (percentage) for dichotomous variables. Comparisons of food groups between interventions diets were performed using analysis of covariance (ANCOVA) adjusted for energy intake. The ANCOVA that adjusted for baseline values, oral antidiabetic medications, antihypertensive medications, and changes in physical activity levels, was also used to assess if the changes (week 16–baseline) in SBP, DBP, urinary sodium, urinary potassium, and the urinary sodium to potassium ratio were significantly different between the dietary. All statistical tests were considered statistically significant when P value was < 0.05. The restricted cubic spline (RCS) was applied to assess the linearity and explore the shape of the relationship between dietary food groups and SBP in two intervention groups.
Results
Between July 11, 2020, and March 10, 2021, a total of 563 participants were screened, of whom 307 met the inclusion criteria, and 300 were randomized to the dietary interventions (Fig. 1). Finally, 284 completed the study. The mean (SD) age and BMI were 55.4 (7.0) years and 30.4 (3.4) kg/m2, respectively. Besides, 57.1% were male, and 48.7% were obese. At baseline, the median DASH diet score was 3.0 (interquartile range 2–4) in both intervention groups. The baseline characteristics were similar between the dietary intervention groups, except for oral antidiabetic medication; in the legume-based DASH diet, the percentage of participants treated with metformin was slightly higher than in the DASH diet group (Table 1). Physical activity did not change during the study in both groups [3.5 (2.7) Met-h/week at baseline vs. 3.4 (2.7) at end of trial in DASH diet; 3.4 (2.7) at baseline vs. 3.4 (2.7) at end of trial in legume-based DASH diet].
No significant differences were observed between the intervention groups for dietary intake at baseline. Analysis of the subjects’ food records during dietary interventions showed a significant reduction in the red meat consumption (mean change difference between diets −41.0, 95% CI −63.7 to −18.5 g/day, P < 0.001), saturated fatty acid (−1.6, −1.9 to −1.2, P < 0.001), and cholesterol (−20.9, −37.3 to −4.4, P = 0.012) in the legume-based DASH diet compared to the DASH diet. Legume consumption (100.4, 96.7–104.1, P < 0.001) and fiber intake (5.1, 2.0–8.1, P = 0.001) increased significantly in the legume-based DASH diet compared to the DASH diet. No significant differences in fruit, vegetables, whole grains, refined grains, nuts and seeds, low-fat dairy products, sweets, sodium intake, DASH score, carbohydrate, protein, fat and sodium intake were found between the two groups (Table 2). Weight decreased after consumption of both hypocaloric dietary interventions [−4.0 (−5.0 to −3.0) in DASH diet and −3.7 (−7.4 to −2.7] in legume-based DASH diet); however, the difference between two dietary interventions was not significant (Table 2).
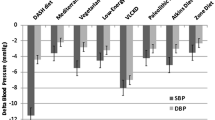
At baseline, there were no significant differences in SBP, DBP, urine electrolytes among the two intervention groups. A reduction in SBP (mean change difference between diets −3.8, 95% CI −6.2 to −1.6 mmHg, P = 0.002) and urinary sodium (−2.3, 95% CI −3.7 to −0.9 mmol/dL, P = 0.001) was found in the legume-based DASH diet compared to the DASH diet group (Table 3).
The multivariable RCS analysis showed the U-shaped association of refined grains intake (P-nonlinear < 0.001 in both intervention groups) with SBP. The greatest decrease in blood pressure was observed when reducing the intake of refined grains by −29.8 to −76.2 g/day in both intervention groups. Moreover, an L-shaped relationship was found between fruit intake and SBP in both intervention groups (P nonlinearity < 0.001 in both intervention groups). The SBP decreased with increasing fruit intake until 70.8 g/day in the DASH diet and 127.6 g/day in the legume-based DASH diet and then flattened. In the legume-based DASH diet, the SBP decreased with the legumes intake of more than 95.8 g/day (P nonlinear < 0.001). Vegetable and DASH score had a negative linear correlation with SBP. Sweet, energy, and sodium intake had a positive linear correlation with SBP in both intervention groups. No significant correlation was found between SBP and a change in the intake of whole grains, red meat, low-fat dairy products, and nuts in both intervention group (Figs. 2 and 3).
Discussion
In the current trial among obese and overweight type 2 diabetic participants, the SBP was reduced by replacing one serving of red meat with legumes in the DASH diet at least 5 days a week over 16 weeks. Further investigation of food groups in the DASH diet showed that SBP decreased with increasing vegetable intake, while it increased with increasing intake of energy, sodium, and sweets. Moreover, the lowest SBP was observed when reducing the intake of refined grains by 29.8–76.2 g/day and increasing the intake of legumes by more than 98 g/day. Additionally, when the intake of fruits exceeded certain thresholds, blood pressure did not decrease.
In the current study, adopting a traditional DASH diet improved SBP among participants with type 2 diabetes. Our findings are in line with two meta-analyses indicating that DASH diet was associated with a −4.70 mmHg (−5.76 to −3.63 mmHg) change in SBP; however, despite −3.75 mmHg (−4.53 to −2.97 mmHg) change in DBP in the meta-analysis, no reduction in DBP was observed in the current study [25, 26]. Additionally, we found that replacing a serving of total red meat with legumes significantly reduced SBP compared to the traditional DASH diet. Contradicting our findings, adopting dietary patterns such as the Mediterranean and DASH diets, independent of red meat intake, improved blood pressure among healthy, overweight and obese adults [27], and hypertensive subjects [13]. In all of these studies, however, red meat was replaced with other animal protein sources. In the current study, when we further investigated which individual dietary food groups in the DASH diet contributed to blood pressure reduction, we found that changes in the red meat intake were not associated with SBP, but the legume intake more than 98 g decreased blood pressure. In a systematic review and meta-analysis of randomized controlled trials, there was no significant effect of substituting red meat with high-quality plant protein sources on blood pressure [16], which may be because the health-promoting effects of legume consumption, as seen in the current study, are achieved by consuming more than one serving per day [17].
In the current study, SBP decreased by lowering refined grains intake from ~ 30 (1 serving/day) to ~ 80 (2.5 servings/day) g/day. Previous systematic review and meta-analyses, and long-term follow-up studies have reported that increasing the consumption of refined grains and sweets from 1 to 3 servings per day had no association with hypertension [28,29,30]. This may be because the detrimental effects of consuming refined grains on chronic diseases, as seen in the current study, are observed when the intake of refined grains exceeds 200 g/day [31]. This is in line with our study in which sweets and refined grains were consumed more than 200 g/day. However, the U-shaped effect of reducing refined grains on SBP, both in the current study and a previous study [32], aligns with recommendations that emphasize the balanced consumption of whole grains and refined grains in the diet [33]. In addition, despite meta-analysis studies that reported the consumption of whole grains as 50–100 g/day reduces the risk of chronic disease such as hypertension, type 2 diabetes, and mortality [28, 31, 34], in the current study, increasing whole grain consumption did not affect blood pressure. Further studies are needed to be clarify the type and amount of grains for preventing and managing hypertension.
Our findings on the effect of increasing fruit and vegetable intake on lowering SBP are consistent with the meta-analysis of prospective cohort studies and randomized controlled trials, which concluded that fruits and vegetables were more effective in reducing SBP [25, 28, 35] and this relationship was linear for vegetables and nonlinear for fruits [28]. These findings are similar to our study, which showed that vegetable consumption was linearly related to SBP reduction, but the consumption of fruits to a certain threshold reduced SBP.
Previous clinical trials, investigating the effect of an energy restricted diet on blood pressure found that a low-energy diet reduces SBP and DBP [36, 37]. Consistently, our findings further confirm the inverse linear association between energy intake and SBP.
The strength of the current study was the interpretation of the results based on the ITT principles, low dropout rate, corrections for multiple tests, long-term nutritional intervention, and randomized trial design that allowed for controlling the confounders. Nevertheless, this study also has several limitations.
The participants were not blinded to the aim of the investigation (focused on increasing the intake of legumes), which may have affected their behaviors. Dietary interventions were recommended to participants, and no meals were prepared for them; therefore, the goal of the diet might not be fully attained. For this reason, the dietitian called the participants once a week and encouraged adherence to the dietary recommendations. We also gathered the food records of participants and assessed their adherence to dietary recommendations. However, these measures are insufficient for evaluating adherence to dietary interventions, and the assessment of the biochemical index of legume intake could be a more appropriate indicator. Also, financial constraints limited us to assessing dietary adherence accurately. Overall, adherence to a healthy diet is affected by socioeconomic status. This study was conducted in an area with a middle to high socioeconomic status, and our findings cannot be generalized to type 2 diabetic patients with a low socioeconomic status.
Conclusions
The DASH diet, enriched in legumes, could improve SBP in participants with type 2 diabetes. In DASH diet, the balance of consumption of refined grains and fruits along with higher consumption of vegetables and lower consumption of sweets, sodium and energy reduced SBP.
Availability of data and materials
The datasets generated and/or analysed during the current study are not publicly available due institution’s policy but are available from the corresponding author on reasonable request.
Abbreviations
- CVD:
-
Cardiovascular disease
- DASH:
-
Dietary approach to stop hypertension
- RCT:
-
Randomized controlled trial
- IRCT:
-
Iranian registry of clinical trials
- TLGS:
-
Tehran lipid and glucose study
- ITT:
-
Intention-to-treat
- MICE:
-
Multiple imputation by chained equations
- ANCOVA:
-
Analysis of covariance
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- RCS:
-
Restricted cubic spline
References
Olsen MH, Angell SY, Asma S, Boutouyrie P, Burger D, Chirinos JA, et al. A call to action and a lifecourse strategy to address the global burden of raised blood pressure on current and future generations: the Lancet Commission on hypertension. Lancet. 2016;388(10060):2665–712.
Lago RM, Singh PP, Nesto RW. Diabetes and hypertension. Nat Clin Pract Endocrinol Metab. 2007;3(10):667.
Klein R, Klein BE, Lee KE, Cruickshanks KJ, Moss SE. The incidence of hypertension in insulin-dependent diabetes. Arch Intern Med. 1996;156(6):622–7.
Sousa AC, Jardim TV, Costa TO, Magalhães FG, Montelo MPM, Souza WKB, et al. Hypertensive diabetic patients: incidence of cardiovascular and renal outcomes in a historical cohort over 11 years. Diabetol Metab Syndr. 2017;9:98.
Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33) UK Prospective Diabetes Study (UKPDS) Group. Lancet. 1998;352(9131):837–53.
Atefi M, Pishdad GR, Faghih S. Canola oil and olive oil impact on lipid profile and blood pressure in women with type 2 diabetes: a randomized controlled trial. Prog Nutr. 2018;20:102–9.
Ley SH, Hamdy O, Mohan V, Hu FB. Prevention and management of type 2 diabetes: dietary components and nutritional strategies. Lancet. 2014;383(9933):1999–2007.
Atefi M, Ghavami A, Hadi A, Askari G. The effect of barberry (Berberis vulgaris L.) supplementation on blood pressure: a systematic review and meta-analysis of the randomized controlled trials. Complement Ther Med. 2021;56:102608.
Bazzano LA, Green T, Harrison TN, Reynolds K. Dietary approaches to prevent hypertension. Curr Hypertens Rep. 2013;15(6):694–702.
Campbell AP. DASH eating plan: an eating pattern for diabetes management. Diabetes Spectr. 2017;30(2):76–81.
Swain JF, McCarron PB, Hamilton EF, Sacks FM, Appel LJ. Characteristics of the diet patterns tested in the optimal macronutrient intake trial to prevent heart disease (OmniHeart): options for a heart-healthy diet. J Am Diet Assoc. 2008;108(2):257–65.
Simpson EJ, Clark M, Razak AA, Salter A. The impact of reduced red and processed meat consumption on cardiovascular risk factors; an intervention trial in healthy volunteers. Food Funct. 2019;10(10):6690–8.
Sayer RD, Wright AJ, Chen N, Campbell WW. Dietary approaches to stop hypertension diet retains effectiveness to reduce blood pressure when lean pork is substituted for chicken and fish as the predominant source of protein. Am J Clin Nutr. 2015;102(2):302–8.
Qian F, Riddle MC. Red and processed meats and health risks: how strong is the evidence? Diabetes Care. 2020;43(2):265–71.
Evert AB, Dennison M, Gardner CD, Garvey WT, Lau KHK, MacLeod J, et al. Nutrition therapy for adults with diabetes or prediabetes: a consensus report. Diabetes Care. 2019;42(5):731–54.
Guasch-Ferré M, Satija A, Blondin SA, Janiszewski M, Emlen E, O’Connor LE, et al. Meta-analysis of randomized controlled trials of red meat consumption in comparison with various comparison diets on cardiovascular risk factors. Circulation. 2019;139(15):1828–45.
Ferreira H, Vasconcelos M, Gil AM, Pinto E. Benefits of pulse consumption on metabolism and health: a systematic review of randomized controlled trials. Crit Rev Food Sci Nutr. 2021;61(1):85–96.
Hassanzadeh-Rostami Z, Hemmatdar Z, Pishdad GR, Faghih S. Moderate consumption of red meat, compared to soy or non-soy legume, has no adverse effect on cardio-metabolic factors in patients with type 2 diabetes. Exp Clin Endocrinol Diabetes. 2021;129(6):429–37.
Saraf-Bank S, Esmaillzadeh A, Faghihimani E, Azadbakht L. Effects of legume-enriched diet on cardiometabolic risk factors among individuals at risk for diabetes: a crossover study. J Am Coll Nutr. 2016;35(1):31–40.
Hosseinpour-Niazi S, Mirmiran P, Hedayati M, Azizi F. Substitution of red meat with legumes in the therapeutic lifestyle change diet based on dietary advice improves cardiometabolic risk factors in overweight type 2 diabetes patients: a cross-over randomized clinical trial. Eur J Clin Nutr. 2015;69(5):592–7.
Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, et al. 2020 International society of hypertension global hypertension practice guidelines. Hypertension. 2020;75(6):1334–57.
Kuwabara M, Kuwabara R, Niwa K, Hisatome I, Smits G, Roncal-Jimenez CA, et al. Different risk for hypertension, diabetes, dyslipidemia, and hyperuricemia according to level of body mass index in Japanese and American subjects. Nutrients. 2018;10(8):1011.
Cuenca-García M, Artero EG, Sui X, Lee DC, Hebert JR, Blair SN. Dietary indices, cardiovascular risk factors and mortality in middle-aged adults: findings from the Aerobics center longitudinal study. Ann Epidemiol. 2014;24(4):297-303 e2.
Simpson SH, Majumdar SR, Tsuyuki RT, Lewanczuk RZ, Spooner R, Johnson JA. Effect of adding pharmacists to primary care teams on blood pressure control in patients with type 2 diabetes: a randomized controlled trial. Diabetes Care. 2011;34(1):20–6.
Gibbs J, Gaskin E, Ji C, Miller MA, Cappuccio FP. The effect of plant-based dietary patterns on blood pressure: a systematic review and meta-analysis of controlled intervention trials. J Hypertens. 2021;39(1):23–37.
Chiavaroli L, Viguiliouk E, Nishi SK, Blanco Mejia S, Rahelić D, Kahleová H, et al. DASH dietary pattern and cardiometabolic outcomes: an umbrella review of systematic reviews and meta-analyses. Nutrients. 2019;11(2):338.
O’Connor LE, Paddon-Jones D, Wright AJ, Campbell WW. A Mediterranean-style eating pattern with lean, unprocessed red meat has cardiometabolic benefits for adults who are overweight or obese in a randomized, crossover, controlled feeding trial. Am J Clin Nutr. 2018;108(1):33–40.
Schwingshackl L, Schwedhelm C, Hoffmann G, Knüppel S, Iqbal K, Andriolo V, et al. Food groups and risk of hypertension: a systematic review and dose-response meta-analysis of prospective studies. Adv Nutr. 2017;8(6):793–803.
Sawicki CM, Jacques PF, Lichtenstein AH, Rogers GT, Ma J, Saltzman E, et al. Whole- and refined-grain consumption and longitudinal changes in cardiometabolic risk factors in the framingham offspring cohort. J Nutr. 2021;151(9):2790–9.
Wang L, Gaziano JM, Liu S, Manson JE, Buring JE, Sesso HD. Whole- and refined-grain intakes and the risk of hypertension in women. Am J Clin Nutr. 2007;86(2):472–9.
Schwingshackl L, Hoffmann G, Lampousi AM, Knüppel S, Iqbal K, Schwedhelm C, et al. Food groups and risk of type 2 diabetes mellitus: a systematic review and meta-analysis of prospective studies. Eur J Epidemiol. 2017;32(5):363–75.
Liu R, Mi B, Zhao Y, Li Q, Dang S, Yan H. Gender-specific association between carbohydrate consumption and blood pressure in Chinese adults. BMJ Nutr Prev Health. 2021;4(1):80–9.
Jones JM, García CG, Braun HJ. Perspective: whole and refined grains and health-evidence supporting “Make half your grains whole.” Adv Nutr. 2020;11(3):492–506.
Schwingshackl L, Schwedhelm C, Hoffmann G, Lampousi AM, Knüppel S, Iqbal K, et al. Food groups and risk of all-cause mortality: a systematic review and meta-analysis of prospective studies. Am J Clin Nutr. 2017;105(6):1462–73.
Schwingshackl L, Hoffmann G, Iqbal K, Schwedhelm C, Boeing H. Food groups and intermediate disease markers: a systematic review and network meta-analysis of randomized trials. Am J Clin Nutr. 2018;108(3):576–86.
Velthuis-te Wierik EJ, van den Berg H, Schaafsma G, Hendriks HF, Brouwer A. Energy restriction, a useful intervention to retard human ageing? Results of a feasibility study. Eur J Clinical Nutr. 1994;48(2):138–48.
Lefevre M, Redman LM, Heilbronn LK, Smith JV, Martin CK, Rood JC, et al. Caloric restriction alone and with exercise improves CVD risk in healthy non-obese individuals. Atherosclerosis. 2009;203(1):206–13.
Acknowledgements
This study, as part of Ph.D. Thesis of Somayeh Hosseinpour-Niazi, was supported by the Research Institute for Endocrine Sciences, Shahid Beheshti University of Medical Sciences. We express our appreciation to the participants of this study for their collaboration.
Funding
This work was supported by Shahid Beheshti University of Medical Sciences, Tehran, Iran (Grant 17100).
Author information
Authors and Affiliations
Contributions
SHN, FH and PM conceptualized and designed the study. SHN and MM analyzed and interpreted the data; SHN, MM, MD, PM and FH drafted the initial manuscript; FA supervised the project. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
The study protocol was approved by the ethics committee of the Research Institute for Endocrine Sciences (RIES), Shahid Beheshti University of Medical Sciences, and written informed consent was acquired from participants prior to their inclusion in the study.
Consent for publication
Not applicable.
Competing interests
On behalf of all authors, the corresponding author hereby declares that there is no competing interest.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Hosseinpour-Niazi, S., Hadaegh, F., Mirmiran, P. et al. Effect of legumes in energy reduced dietary approaches to stop hypertension (DASH) diet on blood pressure among overweight and obese type 2 diabetic patients: a randomized controlled trial. Diabetol Metab Syndr 14, 72 (2022). https://doi.org/10.1186/s13098-022-00841-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-022-00841-w