Abstract
Objective
Coronary artery calcium score and glycated hemoglobin(HbA1c) are both considered risk factors for coronary heart disease. However, the relationship between coronary artery calcium score and HbA1c is still unclear. Consequently, the present study was undertaken to explore HbA1c association with coronary artery calcium score progression in South Korea.
Methods
This study is a secondary analysis based on a retrospective cohort study in which 8151 participants received Health examination kits at the Health Promotion Center, Samsung Medical Center in Seoul, South Korea, from March 1, 2003–December 31, 2013. Cox proportional-hazards regression model was then used to evaluate the independent relationship between HbA1c and coronary artery calcium score progression.
Results
After adjusting potential confounding factors (age, sex, BMI, height, weight, SBP, DBP, TC, LDL-C, HDL-C, triglycerides, smoking status, alcohol consumption, reflux esophagitis status, hypertension, diabetes, dyslipidemia, ischemic heart disease and cerebrovascular disease), it was revealed that there was a nonlinear relationship between HbA1c and coronary artery calcium score progression, while the scoring point was 5.8%. The effect size was 2.06 to the left of the inflection point, while the 95% CI was 1.85 to 2.29. Whereas, the effect size was 1.04, on the right side of the inflection point while 95% CI was 0.99 to1.10.
Conclusion
The relationship between HbA1c and coronary artery calcium score progression is nonlinear. HbA1c is positively related to coronary artery calcium score progression when HbA1c level was less than 5.8%.
Similar content being viewed by others
Introduction
Glycated hemoglobin (HbA1c) is the core of glycemic control and management in diabetic patients and has recently been recommended as a crucial parameter for diagnosing diabetes and identifying people at risk of developing it further [1]. HbA1c has a better reliability rate when it is compared with fasting or post-load blood glucose measurements [2]. HbA1c can also effectively reflect the blood glucose control achieved in the past 2–3 months and is a recommended tool for the diagnosis and screening of diabetes [3, 4].
Coronary atherosclerotic heart disease (CHD) is a multi-factorial disease. The Framingham Heart Study originally conducted in the US established a series of risk factors for coronary heart disease, including age, gender, cholesterol, hypertension, smoking, and diabetes [5]. It is a well-known fact that chronic glucose metabolism disorders increase the risk of CHD [6,7,8,9]. However, A series of evidence regarding the association between HbA1c and cardiovascular disease event outcome yields conflict findings. Many studies reported that HbA1c was an important determinant of CHD and its severity [10,11,12,13,14]. However, studies have reported that HbA1c level was associated with future cardiovascular risk in women without diabetes, while HbA1c level was not an independent determinant of cardiovascular risk in the population including women with diabetes [15]. Multiple observational studies and randomized trials have shown inconsistent evidence of the effect of HbA1c levels below current guidelines (7.0%) on cardiovascular events and death [16,17,18,19]. Given the differences in the study population, study design, measurement of coronary artery stiffness, adjustment for covariates, and certain methodological limitations, we conducted a secondary analysis based on a retrospective cohort study to observe the correlation between HbA1c and the progression of coronary artery calcium scores (CACS) in people undergoing physical examinations at the Health Promotion Center.
Participants and methods
Study design
This study had a retrospective cohort study design. The interesting independent variable in the present work is HbA1c, whereas the dependent variable is coronary artery calcium score progression (dichotomous variable: 0 = no progression, 1 = progression).
Data source
We obtained data from the "PLOS ONE" database (https://journals.plos.org/plosone/). This website allowed users to download raw data for free. According to PLOS ONE Terms of Service, we cited PLOS ONE data package in the present study. (PLOS ONE data package: Min YW, Song BG, Kim HS, Kim K, Lee H, Min BH, Lee JH, Son HJ, Rhee PL, Kim JJ (2017) Data from: Associations between reflux esophagitis and the progression of coronary artery calcification: A cohort study. https://doi.org/10.1371/journal.pone.0184996.s001).
Study population
Since the accomplishment of the entire study was achieved by Yang Won Min et al. [20], all the steps were outlined to understand the entire research process more clearly. Those patients were enrolled in a non-selective yet consecutive manner that had undergone physical examinations at the Health Promotion Center in Samsung Medical Center, Seoul, South Korea, from March 1, 2003, to December 31, 2013. Clinical data were extracted from the hospital electronic medical record system, and the patients' identities were encoded as non-traceable codes to ensure the complete privacy of all.
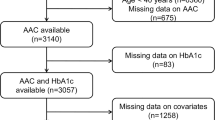
Initially, 199,375 participants were involved in this study but later on, 191,224 participants were subsequently excluded, leaving 8151 cases for the final data analysis (Fig. 1). Inclusion criteria comprised of several factors like (1) Participants over 20 years who underwent health screening examinations; (2) Participants enduring the screening esophagogastroduodenoscopy (EGD) and coronary computed tomography (CT) scanning during the same visit. Whereas, the participants who did not undergo follow-up coronary CT scans (n = 19,038), and had missing information (n = 89) as well as skipped HbA1c at the first physical examination (n = 70) were excluded. Detailed ethics and informed consent was already ensured by the author in previously published articles [20].
Variables
HbA1c
The information of HbA1c was obtained at baseline and was recorded as a continuous variable.
Coronary artery calcium score progression
Our interesting outcome variable was coronary artery calcium score progression (dichotomous variable: 0 = no progression, 1 = progression). Because there is no mutual definition for CACS progression in the literature, we used the transformed square root method of Hokanson to quantify the CACS progression recommended by John W et al. [21]. CACS progression was defined as the difference between the square root of the follow-up and baseline CAC scores ≥ 2.5. Brilliance 40 (Philips Medical Systems, Cleveland, Ohio), VCT Light Speed 64 (GE Healthcare, Milwaukee, Wisconsin), or Discovery 750HD (GE Healthcare) multidetector CT scanners were used to acquire images of CAC. The scans were analyzed using Extended Brilliance Workspace (Philips Medical Systems) or Advantage (GE Healthcare) workstations, while the CAC scores were calculated as described by Agatston et al. [22].
Covariates
In this study, the selection of covariates was based on the published literature and our accumulated clinical experience. Based on the above-mentioned principles, the following variables were used as covariates: (1) continuous variables: age, duration, body mass index (BMI), height, weight, systolic blood pressure (SBP), diastolic blood pressure (DBP), total cholesterol(TC), low-density lipoprotein cholesterol (LDL-C), high-density lipoprotein cholesterol (HDL-C), triglycerides; (2) categorical variables: sex (male, female), smoking status (never, past smoker, current smoker), alcohol consumption (never, past drinker, current drinker), reflux esophagitis status (negative, positive), hypertension (negative, positive), diabetes (negative, positive), dyslipidemia (negative, positive), ischemic heart disease (negative, positive), cerebrovascular disease (negative, positive).
Statistical analysis
Data was indicated as mean ± standard deviation (normal distribution) or median (minimum, maximum)(skewed distribution) for continuous variables and as numbers and percentages for the categorical variables. χ2 (categorical variables), student t-test (normal distribution), or Mann–Whitney U test (skewed distribution) were used to detect the differences among different CACS progression (binary variables). To examine the association between HbA1c and CACS progression, three distinct models were constructed using univariate and multivariate Cox proportional-hazards regression model, including a non-adjusted model (no covariates were adjusted), minimally-adjusted model (only sociodemographic variables were adjusted) and fully-adjusted model (covariates present in Table 1 were adjusted). Effect sizes with 95% confidence intervals were recorded. Since Cox proportional-hazards regression model-based methods are often suspected for their inability to deal with non-linear models. For that reason, nonlinearity between HbA1c and CACS progression was addressed using the Cox proportional-hazards regression model with cubic spline functions and the smooth curve fitting (penalized spline method). If nonlinearity was detected, firstly, a calculation of the inflection point using a recursive algorithm was performed, and then a two-piecewise Cox proportional-hazards regression model was constructed on both sides of the inflection point (The details were described in Additional file 1).
To test the robustness of our results, we performed a sensitivity analysis. We converted HbA1c into a categorical variable according to the quartile and calculated the p for the trend to verify the results of HbA1c as the continuous variable and to examine the possibility of nonlinearity.
To test whether the secondary prevention population would bias our results, we performed a sensitivity analysis. We excluded the secondary prevention population from the study and re-established a Cox proportional-hazards regression model to verify the stability of our results (adjustment variables were the same as fully adjused).
Modeling was performed with the statistical software packages R (http://www.R-project.org, The R Foundation) and EmpowerStats (http://www.empowerstats.com, X&Y Solutions, Inc., Boston, MA). The p-values less than 0.05 (two-sided) were considered statistically significant.
Results
Baseline characteristics of participants
The baseline characteristics of these included participants are listed in Table 1. The average age was 53.82 ± 7.66 years, and about 90.98% of participants were male. The incidence of progression was 59.71% (4867/8151). There were statistically significant differences between the no progression group and the progression group (p-values < 0.05) for all variables except total cholesterol and cerebrovascular disease (Table 1). When compared with no progression group, HbA1c, age, sex, duration, BMI, weight, SBP, DBP, TC, LDL-C, triglycerides, smoking status, alcohol consumption, reflux esophagitis status, hypertension, diabetes, dyslipidemia, ischemic heart disease and cerebrovascular disease increased significantly in the progression group, while the opposite results were detected in covariates in terms of height and HDL-C.
The results of multivariate analyses using Cox proportional-hazards regression model
To evaluate the correlation between HbA1c and CACS progression, three different models (Cox proportional-hazards regression model) were constructed (Table 2). In the un-adjusted model, an increase of 1% of HbA1c was related to a 24% increase of CACS progression risk (HR = 1.24, 95%CI: 1.21 to 1.28), leading to a statistically significant result. In the minimally-adjusted model, adjustment of demographic variables led to an additional increase of 1% of HbA1c by 23% (HR = 1.23, 95%CI: 1.20 to 1.27). In fully-adjusted model, each additional 1% of HbA1c was accompanied by a 22% increases in CACS progression (HR = 1.22, 95%CI:1.18 to 1.26). The distribution of confidence intervals indicated that the correlation between HbA1c and CACS progression obtained by the model was reliable.
The nonlinearity addressed by Cox proportional-hazards regression model with cubic spline functions
Usage of Cox proportional-hazards regression model along with cubic spline functions and a smooth curve fitting, it was observed that the correlation between HbA1c and CACS progression was nonlinear (Fig. 2) due to which the data was adjusted proportionally to a piecewise Cox proportional-hazards regression model to fit two different slopes. Based on the sensitivity analysis, data was also arranged by standard Cox proportional-hazards regression model, and the best fit model was selected through log-likelihood ratio test (Table 3). As the p-value for the log-likelihood ratio test was less than 0.05 in our study, the two-piecewise model was utilized to fit the relationship between HbA1c and CACS progression. By using a recursive algorithm, firstly, the inflection point was discovered as 5.8, and then the effect sizes and confidence interval around the inflection point were computed through a two-piecewise Cox proportional-hazards regression model. To the left of the inflection point, the effect size was 2.06, and the 95% CI was 1.85 to 2.29, whereas the effect size was 1.04, and the 95% CI was 0.99 to1.10 on the right side of the inflection point.
Discussion
In this observational retrospective cohort study, it was concluded that HbA1c and CACS progression have a nonlinear saturated relationship. When the HbA1c level was less than 5.8%, a positive correlation was observed between HbA1c and the progression of CACS, while above 5.8%, this positive correlation gravitated towards saturated. Even if HbA1c levels increased again, the risk of CACS progression would not surge ahead. There was no significant alteration after excluding the secondary prevention population in the study (Additional file 1: Table S1).
Coronary artery calcification score is a strong predictor of cardiovascular disease events [23]. The progression of CACS has been associated with a higher risk of myocardial infarction and all-cause mortality [24,25,26]. In populations with other risk factors for cardiovascular disease events (e.g., hypertension, dyslipidemia, smoking, etc.), more aggressive control of HbA1c levels in those with HbA1c below 5.8 may have greater potential benefits. When HbA1c is higher than 5.8, the change in HbA1c level may have a scarce effect on the outcomes of cardiovascular events.
Some previous studies have shown consistent results with ours investigating correlation between HbA1c and CACS progression or coronary atherosclerosis. Reza Ajudani, in a cross-sectional study based on 411 patients without history of known diabetes mellitus, reported that HbA1c may be functioning as an independent diagnostic factor in nondiabetic patients with severe coronary atherosclerosis [27]. Besides, Wenhui Zhao et al. used African American and white diabetic patients as the study population and obtained similar results [28]. Rivera et al. reached similar conclusions in 1043 asymptomatic people without diabetes [29]. Additionally, Peter D Reaven et al., in a study comprising of veteran diabetic participants, stated that although intensive hypoglycemic therapy did not reduce cardiovascular events in the study cohort as a whole, an intensified hypoglycemic therapy could reduce cardiovascular events in people with less severe coronary atherosclerosis [30]. In a large enrollment study, the authors found that lower levels of HbA1c, systolic blood pressure and LDL were associated with a reduced risk of acute myocardial infarction and stroke. In patients with type 2 diabetes, the HbA1c level outside the target range recommended in current guidelines (7%) was a strong predictor of cardiovascular event outcomes [31]. This is closely related to our results.
However, the reduction of HbA1c level is not completely related to the occurrence and improvement of cardiovascular events. Hertzel C Gerstein et al. reported that using intensive therapy to position glycosylated hemoglobin levels below 6.0% could increase mortality, but did not significantly reduce major cardiovascular events in type 2 diabetes [32]. The inconsistency of these studies may be due to the small sample size, different study populations, different forms of outcome variables, and few cases of coronary heart disease, which may limit the statistical power.
Our study has some innate strength that is listed below. Firstly, the sample size of this study was relatively large. Secondly, all the previously cited articles that also studied HbA1c and CACS or coronary atherosclerosis did not clarify the nonlinear relationship, which we have tried to highlight in our study [27, 28, 33,34,35,36,37,38]. To the best of our knowledge, this is the first time that a nonlinear relationship has been reported, along with the determination of an inflection point exploring the correlation between HbA1c and CACS progression. Third, this study is an observational study and therefore susceptible to potential confounding, although we used strict statistical adjustment to minimize residual confounders. Lastly, we ensured the robustness of the results through sensitivity analysis (conversion of target-independent variable form and exclusion of secondary prevention population) which made our results more reliable.
Our research also has few shortcomings which need attention. Firstly, our findings can be generalized only to persons who had undergone physical examinations in South Korea. Secondly, we could not observe the correlation between HbA1c and the progression of CACS in patients with diabetes and prediabetes, which can be attributed to the limitation of the original data. Similarly, we could also not consider fasting blood glucose as a confounding factor to perceive the relationship between HbA1c and CACS progression. In addition to that, there was no differentiation between the patients whose variables were in the abnormal range without any specific intervention, either partial or complete and patients who achieved.
the observed normal levels with medication. Last but not least, we can only adjust the measurable confounding factors, but not the unmeasurable confounding factors.
Conclusion
The relationship between HbA1c and coronary artery calcium score progression is nonlinear. HbA1c is positively related to coronary artery calcium score progression when HbA1c level was lower than 5.8%.
Availability of data and materials
Data can be downloaded from the "PLOS ONE" database (https://journals.plos.org/plosone/).
Abbreviations
- HbA1c:
-
Glycated hemoglobin
- CHD:
-
Coronary heart disease
- BMI:
-
Body mass index
- SBP:
-
Systolic blood pressure
- DBP:
-
Diastolic blood pressure
- TC:
-
Total cholesterol
- LDL-C:
-
Low-density lipoprotein cholesterol
- HDL-C:
-
High-density lipoprotein cholesterol
- CACS:
-
Coronary artery calcium score progression
- EGD:
-
Esophagogastroduodenoscopy
- CT:
-
Coronary computed tomography
References
American Diabetes Association. Diagnosis and classification of diabetes mellitus. Diabetes Care. 2010;33(Suppl 1):S62–9.
Ding N, Kwak L, Ballew SH, et al. Traditional and nontraditional glycemic markers and risk of peripheral artery disease: The Atherosclerosis Risk in Communities (ARIC) study. Atherosclerosis. 2018;274:86–93.
Sacks DB, Arnold M, Bakris GL, et al. Guidelines and recommendations for laboratory analysis in the diagnosis and management of diabetes mellitus. Diabetes Care. 2011;34(6):e61-99.
Selvin E, Steffes MW, Zhu H, et al. Glycated hemoglobin, diabetes, and cardiovascular risk in nondiabetic adults. N Engl J Med. 2010;362(9):800–11.
Andersson C, Johnson AD, Benjamin EJ, et al. 70-year legacy of the Framingham Heart Study. Nat Rev Cardiol. 2019;16(11):687–98.
Go AS, Mozaffarian D, Roger VL, et al. Heart disease and stroke statistics–2014 update: a report from the American Heart Association. Circulation. 2014;129(3):e28–292.
Sarah Rosner P, Pencina MJ, Shih-Jen H, et al. Trends in cardiovascular disease risk factors in individuals with and without diabetes mellitus in the Framingham heart study. Circulation. 2009;120(3):212–20.
Kang DO, Seo HS, Choi BG, et al. Absolute change in fasting plasma glucose over 12 months is associated with 2-year and 5-year major adverse cardiovascular events in patients with drug-eluting stent implants. Int J Cardiol. 2015;179:146–52.
Lin B, Koibuchi N, Hasegawa Y, et al. Glycemic control with empagliflozin, a novel selective SGLT2 inhibitor, ameliorates cardiovascular injury and cognitive dysfunction in obese and type 2 diabetic mice. Cardiovasc Diabetol. 2014;13:148.
Liu XJ, Wan ZF, Zhao N, et al. Adjustment of the GRACE score by HemoglobinA1c enables a more accurate prediction of long-term major adverse cardiac events in acute coronary syndrome without diabetes undergoing percutaneous coronary intervention. Cardiovasc Diabetol. 2015;14:110.
Ashraf H, Boroumand MA, Amirzadegan A, et al. Hemoglobin A1C in non-diabetic patients: an independent predictor of coronary artery disease and its severity. Diabetes Res Clin Pract. 2013;102(3):225–32.
Chen CL, Yen DH, Lin CS, et al. Glycated hemoglobin level is an independent predictor of major adverse cardiac events after nonfatal acute myocardial infarction in nondiabetic patients: a retrospective observational study. Medicine. 2017;96(18):e6743.
Açar B, Ozeke O, Karakurt M, et al. Association of prediabetes with higher coronary atherosclerotic burden among patients with first diagnosed acute coronary syndrome. Angiology. 2019;70(2):174–80.
Scicali R, Giral P, Gallo A, et al. HbA1c increase is associated with higher coronary and peripheral atherosclerotic burden in nondiabetic patients. Atherosclerosis. 2016;255:102–8.
Blake GJ, Pradhan AD, Manson JE, et al. Hemoglobin A1c level and future cardiovascular events among women. Arch Intern Med. 2004;164(7):757–61.
ADVANCE Collaborative Group, Patel A, MacMahon S, et al. Intensive blood glucose control and vascular outcomes in patients with type 2 diabetes. N Engl J Med. 2008;358(24):2560–72.
Holman RR, Paul SK, Bethel MA, et al. 10-year follow-up of intensive glucose control in type 2 diabetes. N Engl J Med. 2008;359(15):1577–89.
Stratton IM, Adler AI, Neil HA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321(7258):405–12.
Ismail-Beigi F, Craven T, Banerji MA, et al. Effect of intensive treatment of hyperglycaemia on microvascular outcomes in type 2 diabetes: an analysis of the ACCORD randomised trial. Lancet. 2010;376(9739):419–30.
Min YW, Song BG, Kim HS, et al. Associations between reflux esophagitis and the progression of coronary artery calcification: a cohort study. PLoS ONE. 2017;12(10):e0184996.
McEvoy JW, Blaha MJ, Defilippis AP, et al. Coronary artery calcium progression: an important clinical measurement? A review of published reports. J Am Coll Cardiol. 2010;56(20):1613–22.
Agatston AS, Janowitz WR, Hildner FJ, et al. Quantification of coronary artery calcium using ultrafast computed tomography. J Am Coll Cardiol. 1990;15(4):827–32.
Criqui MH, Denenberg JO, Ix JH, et al. Calcium density of coronary artery plaque and risk of incident cardiovascular events. JAMA. 2014;311(3):271–8.
Raggi P, Callister TQ, Shaw LJ. Progression of coronary artery calcium and risk of first myocardial infarction in patients receiving cholesterollowering therapy. Arterioscler Thromb Vasc Biol. 2004;24:1272–7.
Budoff MJ, Young R, Lopez VA, et al. Progression of coronary calcium and incident coronary heart disease events: MESA (Multi-Ethnic Study of Atherosclerosis). J Am Coll Cardiol. 2013;61:1231–9.
Budoff MJ, Hokanson JE, Nasir K, et al. Progression of coronary artery calcium predicts allcause mortality. J Am Coll Cardiol Img. 2010;3:1229–36.
Ajudani R, Rezaee-Zavareh MS, Karimi-Sari H, et al. Glycosylated haemoglobin and coronary atherosclerosis in non-diabetic patients: is it a prognostic factor? Acta Cardiol. 2017;72(5):522–8.
Zhao W, Katzmarzyk PT, Horswell R, et al. HbA1c and coronary heart disease risk among diabetic patients. Diabetes Care. 2014;37(2):428–35.
Rivera JJ, Choi EK, Yoon YE, et al. Association between increasing levels of hemoglobin A1c and coronary atherosclerosis in asymptomatic individuals without diabetes mellitus. Coron Artery Dis. 2010;21(3):157–63.
Reaven PD, Moritz TE, Schwenke DC, et al. Intensive glucose-lowering therapy reduces cardiovascular disease events in veterans affairs diabetes trial participants with lower calcified coronary atherosclerosis. Diabetes. 2009;58(11):2642–8.
Rawshani A, Rawshani A, Franzén S, et al. Risk Factors, Mortality, and Cardiovascular Outcomes in Patients with Type 2 Diabetes. N Engl J Med. 2018;379(7):633–44.
Action to Control Cardiovascular Risk in Diabetes Study Group, Gerstein HC, Miller ME, et al. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med. 2008;358(24):2545–59.
Svanteson M, Holte KB, Haig Y, et al. Coronary plaque characteristics and epicardial fat tissue in long term survivors of type 1 diabetes identified by coronary computed tomography angiography. Cardiovasc Diabetol. 2019;18(1):58.
Lindholt JS, Frystyk J, Hallas J, et al. Feasibility study of advanced cardiovascular screening in middle-aged patients with diabetes. Clin Epidemiol. 2020;12:447–55.
Jung CH, Lee WY, Kim SY, et al. The relationship between coronary artery calcification score, plasma osteoprotegerin level and arterial stiffness in asymptomatic type 2 DM. Acta Diabetol. 2010;47(Suppl 1):145–52.
Yang J, Zhou Y, Zhang T, et al. Fasting blood glucose and HbA1c correlate with severity of coronary artery disease in elective PCI patients with HbA1c 5.7% to 6.4. Angiology. 2020;71(2):167–74.
Rhee EJ, Cho JH, Kwon H, et al. Association between coronary artery calcification and the hemoglobin glycation index: the Kangbuk samsung health study. J Clin Endocrinol Metab. 2017;102(12):4634–41.
Huo X, Gao L, Guo L, et al. Risk of non-fatal cardiovascular diseases in early-onset versus late-onset type 2 diabetes in China: a cross-sectional study. Lancet Diabetes Endocrinol. 2016;4(2):115–24.
Acknowledgements
The author is very grateful to the data providers of the study. They completed the entire study. They are (the rankings and institutions of these researchers were ranked according to the” reference [17]” ) Yang Won Min, Byeong Geun Song, Hyuk Lee, Byung-Hoon Min, Jun Haeng Lee, Hee Jung Son, Poong-Lyul Rhee(corresponding author), Jae J. Kim, (Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, South Korea), Hye Seung Kim and Kyunga Kim (Biostatistics and Clinical Epidemiology Center, Samsung Medical Center, Seoul, South Korea). The authors also thank Chi Chen of Yi-er College for data processing and statistical analysis.
Funding
This work is supported by the National Natural Science Foundation of China (No. 81471645, 81871333, 81760312 and 81960338), Guizhou Province 7th Thousand Innovational and Enterprising Talents (GZQ202007086), 2020 Innovation group project of Guizhou Province Educational Commission (KY [2021]017), Guizhou Province Science and Technology Project (No. Qiankehe Support [2020]4Y193 and [2020]4Y159), Guiyang Science and Technology Project (No. 2020-10-3), Key Laboratory Construction Project of Guizhou Medical University.
Author information
Authors and Affiliations
Contributions
JY contributed to the drafting of the manuscript, and analysis and interpretation of the data. BG contributed to the conception and critical revision of the manuscript, analysis and interpretation of the data and approved the final version of the submitted manuscript. Both authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Ethics approval and consent to participate
In the previously published article [17], Yang Won Min, et al. has clearly stated that: the study was conducted per the Declaration of Helsinki. Informed consent was obtained from all participants.
Consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Additional file 1: Additional methods.
Statistical analysis: the calculation method of inflection point. Table S1. The results of HR with and without secondary prevention populations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Yu, J., Gao, B. Nonlinear relationship between HbA1c and coronary artery calcium score progression: a secondary analysis based on a retrospective cohort study. Diabetol Metab Syndr 13, 136 (2021). https://doi.org/10.1186/s13098-021-00747-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s13098-021-00747-z